Natural lithium traces in water were considered by John Cade in 1949 to have the potential to influence mental health. Reference Cade1 Meanwhile, the mood-stabilising effects of lithium are widely recognised by the psychiatric community Reference Altamura, Lietti, Dobrea, Benatti, Arici and Dell'osso2 and its suicide preventive properties are well documented. Reference Müller-Oerlinghausen and Lewitzka3 Although the effects of therapeutic doses of lithium are well established, little is known about the health effects of natural lithium intake.
As a natural trace element, lithium is mobilised by rain from rock and soil and dissolves in ground and drinking water. In some geographic regions, its concentrations may reach up to 5.2 mg/l, reflecting a natural daily intake of lithium of up to 10 mg/day. Reference Schrauzer4,Reference Concha, Broberg, Grandér, Cardozo, Palm and Vahter5 Although such daily doses of lithium are considerably lower than those used therapeutically, it is unknown to what extent intake of natural lithium may influence mental health or suicide mortality. Only one randomised placebo-controlled study showed favourable effects of low-dose lithium supplementation (0.4 mg daily) on mood, in a small sample of former drug users. Reference Schrauzer and de Vroey6 However, evidence from ecological studies indicates that lithium levels in drinking water may be associated with regional suicide mortality. The first study was carried out in Texas in 1990 and demonstrated that counties with higher lithium levels in municipal water supplies had lower suicide and crime rates. Reference Schrauzer and Shrestha7 A more recent report from Japan showed an inverse relationship between lithium levels in tap water and suicide mortality in Oita prefecture. Reference Ohgami, Terao, Shiotsuki, Ishii and Iwata8 However, this report has been criticised for being based on unreliable lithium measures, Reference Huthwaite and Stanley9 and for omitting socioeconomic confounders such as poverty and economic issues. Reference Chandra and Babu10 In order to replicate the report of Ohgami et al Reference Ohgami, Terao, Shiotsuki, Ishii and Iwata8 on the basis of data originating from a different country, and to address the criticisms mentioned above, we extended the design of the study by Ohgami and colleagues and used a large data source of lithium levels in drinking water. To challenge the hypothesis that lithium levels in drinking water are inversely associated with suicide mortality, we adjusted for regional socioeconomic conditions and the availability of mental health service providers. These factors were recently shown to influence suicide mortality in Austria. Reference Kapusta, Posch, Niederkrotenthaler, Fischer-Kern, Etzersdorfer and Sonneck11
Method
Statistics Austria provided the official Austrian mortality database for suicides in 17 age groups and both genders for 99 Austrian districts and for each year in the time period 2005–2009. Comprehensive data on population density, average income per capita and the proportion of Roman Catholics were obtained from the official Austrian population census 2001 (www.statistik.at). The unemployment rates were obtained from the Austrian Public Employment Service (AMS) (M. Eichinger, personal communication, 2009) and were averaged for the available years 2005–2008. All consecutive years were strongly correlated (r>0.9). The density of general practitioners (GPs) and psychiatrists per 10 000 population for each district were available for the year 2007 from the Austrian Medical Chamber (A. Sinabell, personal communication, 2009). The Austrian Institute of Health (ÖBIG)12 provided figures on the density of psychotherapists per 100 000 for the year 2005. Austria had an average population of 8 297 964 (s.d. = 65 050) during the examined time period 2005–2009. The average population per district was 83 818 (s.d. = 165 643), with a range of 1714 to 1 667 878 inhabitants (capital city Vienna). Excluding Vienna (by far the largest region) produced an average population per district of 67 654 (s.d. = 39 852).
To account for the distributions of gender and age in each district, we calculated standardised mortality ratios (SMRs) for suicide for each district using the indirect method, by taking the gender and age composition of the general population as a standard. Although using SMR is formally more appropriate than computing with suicide rates per 100 000 in epidemiological and ecological studies, Reference Kreienbrock and Schach13 we applied both methods for each district to allow discussion of estimated effects as recently suggested. Reference Huthwaite and Stanley9
Lithium levels were obtained from AQA GmbH, an Austrian company engaged in the collection and the analysis of drinking water samples and applied scientific research. The samples were analysed by inductively coupled plasma optical emission spectrometry, a method for the determination of dissolved inorganic, organic and other compounds in water samples. Reference Stefánsson, Gunnarsson and Giroud14 The sample data were collected between 2005 and autumn 2010. In total, 6460 water samples from drinking water supplies from all 99 districts were analysed for lithium (see online Figs DS1 and DS2). The average was 65.3 samples per district (range 1–312). The lowest measurable threshold lithium level by inductively coupled plasma optical emission spectrometry was 0.0033 mg/l. Subthreshold values were found in seven districts. For the statistical calculations, lithium levels were averaged per district. The mean lithium level in Austrian drinking water was 0.0113 mg/l (s.d. = 0.027). The highest single lithium level was found in Graz-vicinity (1.3 mg/l), and the district with the highest mean level was Mistelbach (0.0823 mg/l).
To allow for comparison with the results of the Japanese study, Reference Ohgami, Terao, Shiotsuki, Ishii and Iwata8 we used similar statistical methods; although more elaborated methods for the analysis of geographical data have already been applied. Reference Kapusta, Posch, Niederkrotenthaler, Fischer-Kern, Etzersdorfer and Sonneck11 Because of the skewness of the distribution of lithium levels (skewness 4.606, kurtosis 27.134), the population density, the density of psychiatrists, psychotherapists and GPs, the variables were log-transformed to fit non-parametric tests. Prior to the log-transformation, we also applied a conservative sensitivity analysis of the crude regression model of overall suicide rates as well as SMRs for suicide and lithium levels by inspection of scatter plots and boxplots for the identification of outliers. In total, seven possible outlier districts were identified: Rust-city, Eisenstadt-vicinity, Oberwart, Bruck an der Leitha, Hollabrunn, Korneuburg and Mistelbach. However, exclusion of these outliers did not alter the direction of the association between suicide rates or SMR for suicide and lithium levels nor exceeded the significance level set at alpha 0.05 for all analyses. The same was true when districts with less than five water samples were excluded, or Vienna, the largest city, was excluded (these complementary analyses are not reported in the results). Therefore, all further regression models were based on log-transformed data of all 99 districts.
Weighted least squared (WLS) regression analyses adjusted for the size of the population per district were employed to test for the robustness of univariate and multivariate statistics. Multivariate regression models incorporated those covariates that were significantly correlated with SMR for suicide (Table 1) in correlation tests. The residuals in the regression models were inspected in plots and tested with the Kolmogorov–Smirnoff test for normality. Possible auto-regression of data was analysed using the Durbin–Watson tests. Multivariate models were tested for multicollinearity by calculating tolerance values and the condition index. Data analysis was performed on SPSS 17.0 for Windows.
Table 1 Correlation between district characteristics and standardised mortality ratios (SMR) for suicide (2005–2009)a
| Suicide SMR | ||||||
|---|---|---|---|---|---|---|
| Overall | Male | Female | ||||
| District characteristics | r | P | r | P | r | P |
| Lithium level, mean (mg/l) | –0.406 | 0.000030 | –0.364 | 0.00021 | –0.288 | 0.0038 |
| Log lithium level | –0.377 | 0.00012 | –0.326 | 0.0098 | –0.294 | 0.0032 |
| Population density (per km) | –0.213 | 0.034 | –0.223 | 0.026 | – 0.018 | 0.858 |
| Log population density | –0.291 | 0.0034 | –0.295 | 0.0030 | – 0.058 | 0.571 |
| Per capita income (in 1000 Euro) | –0.306 | 0.0021 | –0.292 | 0.0034 | – 0.143 | 0.158 |
| Proportion of Roman Catholics, % | 0.398 | 0.000045 | 0.398 | 0.000044 | 0.140 | 0.166 |
| Unemployment rate, % | – 0.143 | 0.160 | – 0.089 | 0.382 | – 0.183 | 0.071 |
| Psychiatrist density (per 10 000) | –0.284 | 0.0043 | –0.313 | 0.0016 | – 0.019 | 0.850 |
| Log psychiatrist density | 0.452 | 0.0000048 | 0.478 | 0.0000011 | – 0.066 | 0.527 |
| Psychotherapist density (per 10 000) | –0.231 | 0.021 | –0.246 | 0.014 | – 0.011 | 0.916 |
| Log psychotherapist density | –0.470 | 0.0000012 | –0.493 | 0.00000028 | – 0.063 | 0.542 |
| General practitioner density (per 10 000) | –0.244 | 0.015 | –0.240 | 0.017 | – 0.068 | 0.503 |
| Log general practitioner density | –0.223 | 0.027 | –0.215 | 0.033 | – 0.067 | 0.512 |
Results
Suicide mortality was significantly correlated with mean lithium levels per district, population density, per capita income, the proportion of Roman Catholics, as well as with the density of psychiatrists, psychotherapists and GPs. Unemployment did not correlate with suicide mortality (Table 1).
Univariate regression
The univariate regression parameters for the untransformed lithium levels as the independent variable were similar for the overall suicide rate per 100 000 (R2 = 0.15, β = –0.39, t = –4.14, P = 0.000073), suicide rates for males (R2 = 0.12, β = –0.35, t = –3.64, P = 0.00043) and females (R2 = 0.08; β = –0.28, t = –2.82, P = 0.0058) (online Fig. DS3). The results were comparable when SMRs were used instead of suicide rates: overall (R2 = 0.17, β = – 0.41, t = –4.38, P = 0.000030), male (R2 = 0.13; β = –0.36, t = –3.84, P = 0.00022) and female SMR (R2 = 0.08, β = – 0.29, t = –2.96, P = 0.0038) (Fig. 1).
Log-transformed regressions
All further analyses were based on log-transformed data (online Fig. DS4 andFig. 2). The univariate regression estimates of lithium as a predictor were comparable for overall (R2 = 0.14, β = –0.38, t = –4.01, P = 0.00012), male (R2 = 0.11, β = –0.33, t = –3.39, P = 0.00098) and female SMRs (R2 = 0.09; β = –0.29, t = –3.02, P = 0.0032). Weighting (WLS) for the number of inhabitants per district revealed significant associations for the overall SMR (R2 = 0.05, β = – 0.22, P = 0.029), females (R2 = 0.04, β = – 0.21, P = 0.037) and a trend for males (R2 = 0.03, β = –0.18, P = 0.083).
Multivariate regression
Lithium levels remained as a significant predictor in the unweighted multivariate model (Table 2). Lithium also remained significant in the models for females (R2 = 0.07, β = –0.25, P = 0.033) and males (R2 = 0.38, β = –0.25, P = 0.0089). In the male model the density of psychiatrists, psychotherapists and GPs was also significant (not reported). Removing lithium levels as a predictor from the unweighted multivariate model reduced the proportion of the explained variance by 7.7%.
Table 2 Multivariate regression estimates on overall standardised mortality ratios (SMRs) for suicide (2005-2009)a

| â | T | P | R2 | R2 adj | D–Wb | |
|---|---|---|---|---|---|---|
| Overall suicide SMR | 0.372 | 0.321 | 2.236 | |||
| Constant | 0.092 | 0.927 | ||||
| Log lithium level | – 0.309 | – 3.254 | 0.0016 | |||
| Log population density | 0.120 | 0.787 | 0.434 | |||
| Per capita income | – 0.112 | – 0.955 | 0.342 | |||
| Proportion of Roman Catholics | 0.101 | 0.858 | 0.393 | |||
| Log psychiatrist density | – 0.260 | – 1.774 | 0.080 | |||
| Log psychotherapist density | – 0.364 | – 2.199 | 0.031 | |||
| Log general practitioner density | 0.184 | 1.663 | 0.100 | |||
| Overall suicide SMR (WLS)c | 0.377 | 0.326 | 2.250 | |||
| Constant | 0.118 | 0.906 | ||||
| Log lithium level | – 0.243 | – 2.328 | 0.022 | |||
| Log population density | 0.213 | 1.167 | 0.246 | |||
| Per capita income | – 0.226 | – 1.570 | 0.120 | |||
| Proportion of Roman Catholics | 0.112 | 0.713 | 0.478 | |||
| Log psychiatrist density | – 0.335 | – 2.156 | 0.034 | |||
| Log psychotherapist density | – 0.326 | – 1.656 | 0.101 | |||
| Log general practitioner density | 0.263 | 2.308 | 0.023 |
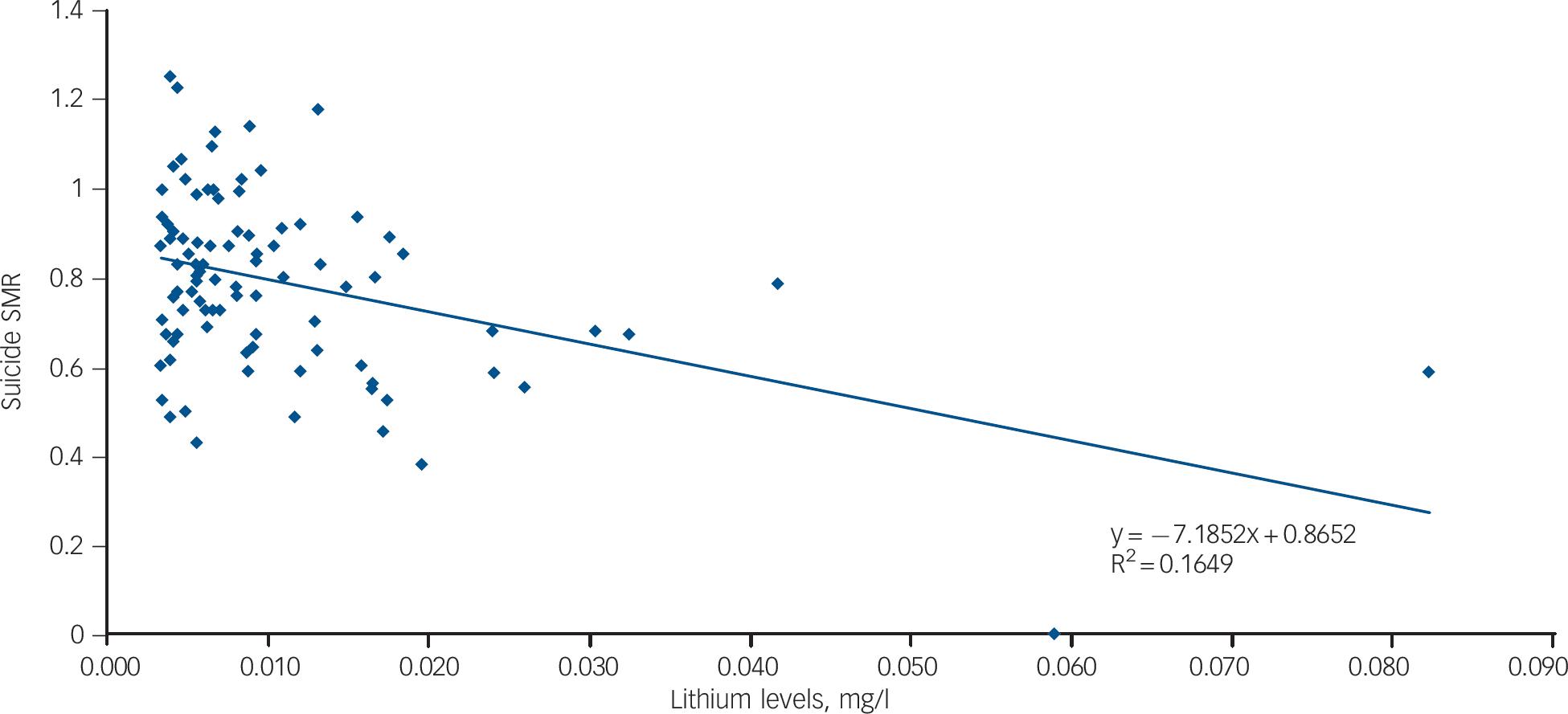
Fig. 1 Crude lithium levels and standardised mortality ratios (SMRs) for suicide (2005–2009).
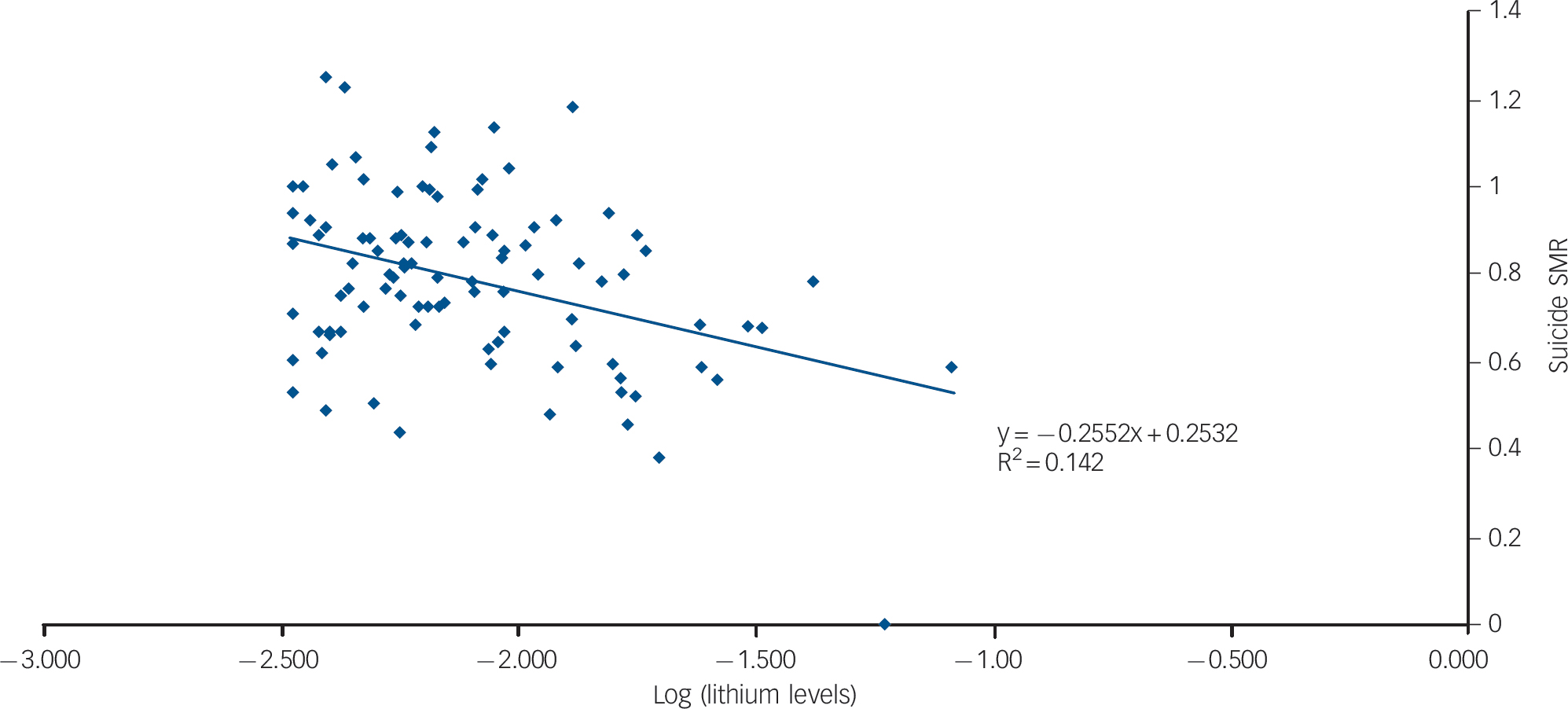
Fig. 2 Log-transformed lithium levels and standardised mortality ratios (SMRs) for suicide (2005–2009).
In the final weighted (WLS) multivariate model, lithium remained a significant predictor of SMRs (Table 2). The significance was marginal on male (R2 = 0.40, β = –0.19, P = 0.062) and female SMRs (R2 = 0.07, β = –0.22, P = 0.088). Removing lithium levels as a predictor from the WLS model reduced the proportion of the explained variance by 3.9%.
Both multivariate models (Table 2) were tested for multicollinearity. Tolerance values ranged between 0.187 and 0.811 and the highest condition index was 5.936, suggesting no multicollinearity. The Durbin–Watson test for autocorrelation revealed no autocorrelation of data.
Discussion
The results of this study indicate that lithium levels in drinking water are inversely associated with suicide rates and SMRs for suicide. We improved Ohgami et al's model and replicated their findings of inverse association between suicide mortality and lithium levels in Oita prefecture on the basis of Austrian data. A strength of our study is that data on lithium concentrations were based on 6460 water measurements in comparison to 79. Reference Ohgami, Terao, Shiotsuki, Ishii and Iwata8 Together with suicide SMRs, they were aggregated to 99 data-pairs – in contrast to 27 and 18 in previous studies. Reference Schrauzer and Shrestha7,Reference Ohgami, Terao, Shiotsuki, Ishii and Iwata8 Sensitivity analyses of the univariate models did not challenge the robustness of the findings. Also, adjustment for well-known socioeconomic confounders, which previously have been shown to be important predictors of suicide mortality in Austria, Reference Kapusta, Posch, Niederkrotenthaler, Fischer-Kern, Etzersdorfer and Sonneck11 did not affect the association with lithium concentrations in drinking water. The WLS procedure produced distortions of regression estimates especially in the separate gender analyses. The effects of lithium in drinking water on males and females were marginally significant. It has to be noted that the variables such as lithium levels, per capita income, proportion of Roman Catholics and the availability of mental health providers could not be stratified by gender for separate analyses, thus the estimates for both genders in our study and also in the Japanese study Reference Ohgami, Terao, Shiotsuki, Ishii and Iwata8 are likely to be biased. Therefore marginal significance may be considered as a sign of robustness. Also, a further stratification of the data, for example by age groups, would lead to a further collapse of the power of the analysis due to decreasing cell counts per stratum.
Sources of lithium intake
Although it can be assumed that lithium in drinking water explains a part of the variance in suicide mortality, other possible lithium sources should be mentioned. Ohgami and colleagues Reference Ohgami, Terao, Shiotsuki, Ishii and Iwata8 were criticised for having omitted consideration of individuals’ intake of bottled mineral water, Reference Huthwaite and Stanley9 which may contain high levels of lithium. Reference Krachler and Shotyk15 They were also criticised for not having accounted for the consumption of vegetables, Reference Desai and Chaturvedi16 which absorb lithium from the soil and may be a complimentary lithium source. Reference Schrauzer4 For obvious reasons, data for both of these factors are not available at aggregate levels; hence we were unable to consider these factors. It has also been considered that lithium could play a role during the cooking process. Reference Krachler and Shotyk15 Indeed, lithium as a salt is likely to be taken up from drinking water into vegetables and animal-derived food and vice versa during osmotic processes. Lithium levels in food would then regress to the levels of local cooking/drinking water. A further source of lithium intake has not been mentioned in this discussion. It has not been considered before that tap water is also used for personal hygiene and it is known that lithium may be taken up percutaneously. Reference Sparsa and Bonnetblanc17 Therefore it needs to be considered whether the large water volumes used during bathing and showering could be an additional source of natural lithium. It is likely that transdermal and per os intake of lithium reflects local water lithium levels in Austria.
Lithium intake and excretion
It has been demonstrated that urinary excretion of lithium correlates with rainfall, due to a dilution effect of rainfall on ground water Reference Dawson, Moore and McGanity18 and that urinary lithium levels correlate with lithium levels in drinking water and the amount of water consumed per day. Reference Concha, Broberg, Grandér, Cardozo, Palm and Vahter5 Lithium is absorbed via sodium channels in the small intestine and uniformly distributed in body water, although others have found differences in lithium levels between tissues Reference Schrauzer4 and plasma and brain concentrations. Reference Soares, Boada, Spencer, Mallinger, Dippold and Wells19 Because renal clearance is not dependent on plasma lithium levels, plasma levels are proportional to daily intake. Reference Price and Heninger20 Although excreted mainly by the kidney, approximately 80% of lithium is reabsorbed by the proximal renal tubule. Reference Jermain, Crismon and Martin21 Excretion of lithium is dependent on the glomerular filtration rate and therefore affected by renal diseases and age, conditions in which plasma lithium increases. On the other hand, dehydration (and loss of salt) decreases the clearance of lithium. Reference Soares, Boada, Spencer, Mallinger, Dippold and Wells19 These considerations suggest that water intake has at least a twofold effect on plasma lithium levels, and that lithium retention is probable when intake of water is reduced.
Estimated effects
Lithium concentrations in drinking water vary considerably by geographic region Reference Schrauzer4,Reference Concha, Broberg, Grandér, Cardozo, Palm and Vahter5 and correlate with natural lithium resources. In northern Chile, a region with one of the largest lithium resources in the world located in the Salar de Atacama, Reference Kampf, Tyler, Ortiz, Muñoz and Adkins22 the natural concentrations of lithium in ground water may reach up to 5.2 mg/l, leading to a natural daily intake of lithium of up to 10 mg/day. Reference Schrauzer4,Reference Concha, Broberg, Grandér, Cardozo, Palm and Vahter5 This is relatively high in comparison to the highest level of 1.3 mg/l measured in Austria. In our study, regional lithium concentrations explained only one part of the suicide mortality variance, namely up to 17% in the crude model and 3.9% in the adjusted and weighted model. Although the direction of the association and the significance of the statistical models were robust after sensitivity analyses and adjustment for confounders, the explained variance varied between the models. Adding variables to the multivariate models increased the total variance explained and suppressed the variance explained by lithium, although multicollinearity was absent. Finally, there is still considerable unexplained variance that is unaccounted for. It has to be noted that ecological studies per se are designed to establish hypotheses rather then proving cause, and their results are not applicable to individual cases (ecological fallacy). Thus, although informative, the estimates should be interpreted with caution due to the aggregated nature of data. In the crude model (online Fig. DS3), an increase of lithium concentration in drinking water by 0.01 mg/l was associated with a decrease in the suicide rate of 1.4 per 100 000 or a 7.2% reduction in the SMR for suicide. This would correspond to one conventional lithium pill (75 mg) in 7400 l (1955 gallons) of drinking water. Despite evolving evidence, the debate on whether continuous low-level lithium intake has protective effects on mental health and suicide risk should be further pursued. Although national suicide prevention programmes are increasingly implemented by politicians in many countries and researchers are seeking for effective preventive interventions, Reference Doessel and Williams23 it is a highly controversial question whether adding lithium to tap water would reduce suicide mortality as previously suggested. Reference Terao, Goto, Inagaki and Okamoto24 It has to be noted that lithium concentrations increase in the brain during the first trimester of gestation Reference Schrauzer4 and early exposure to lithium may cause damage in human brain neurodevelopment. Reference Gentile25 Lithium acts on mood and suicidality via complex interactions with the serotoninergic system Reference Hughes, Dunne and Young26 and more recent studies suggest that lithium has stimulating effects on neurogenesis, Reference Wada27 which could explain both toxicity during neurodevelopment as well as antidepressive/antisuicidal effects. Therefore, currently, not enough is known about the effects of natural lithium on the prevalence of neurodevelopmental disorders to consider artificially increasing its levels in drinking water as a method of universal prevention.
Implications
Owing to the sizeable magnitude of our finding, we provide conclusive evidence that lithium concentrations in drinking water are inversely correlated with suicide rates. Starting with anecdotic reports about the beneficial effects of lithium in drinking water on mental health in 1949 and earlier, Reference Cade1 there is increasing evidence from three independent countries and continents that lithium in drinking water is associated with reduced mortality from suicide. In Texas, USA, lithium levels in drinking water were shown to be inversely associated with admissions and readmissions for psychoses, neuroses and personality disorders in state mental hospitals, as well as with homicide rates, Reference Dawson, Moore and McGanity18,Reference Dawson, Moore and McGanity28 suicide and crime rates. Reference Schrauzer and Shrestha7 In Oita prefecture in Japan, lithium levels in tap water supplies were recently shown to be inversely associated with suicide mortality. Reference Ohgami, Terao, Shiotsuki, Ishii and Iwata8 Of note, in 1969, lithium in drinking water was widely discussed as possibly having an impact on atherosclerotic heart disease Reference Voors29,Reference Voors30 but this has not led to preventive supplementation of lithium in drinking water. Certainly, with these findings in mind, the true effects of chronic low-lithium intake on health and suicide should be investigated further. Reference Young31







eLetters
No eLetters have been published for this article.