Lack of insight is a clinically important phenomenon in psychosis and has predictive value for treatment outcome (Reference Kemp and DavidKemp & David, 1996). Understanding the basis of poor insight might improve interventions. Studies of the relationship between insight and cognition have produced inconsistent results. Some have found poorer insight to be associated with lower scores on measures of executive function and IQ whereas others have not (Reference Morgan, David, Amador and DavidMorgan & David, 2004; Reference Cooke, Peters and KuipersCooke et al, 2005; Reference Aleman, Agrawal and MorganAleman et al, 2006). A curvilinear relationship between insight and cognition has also been noted (Reference StartupStartup, 1996): high cognitive ability was associated with both high and low extremes of insight. A meta-analysis also suggests that there is a modest relationship between better insight and greater depressive symptomatology (Reference Mintz, Dobson and RomneyMintz et al, 2003). However, few studies have examined the relationships between dimensions of insight and self-esteem, depression, and cognitive ability. The aim of this study was to investigate the relationships between insight and IQ, self-esteem and depression in people with psychosis.
METHOD
Sample
Sixty-seven participants (41 men, 26 women) were recruited and assessed at baseline prior to a randomised controlled trial of cognitive–behavioural therapy for psychosis. All participants were out-patients, had been stable on medication for at least 3 months and had at least one distressing positive symptom scoring three or higher on the Positive and Negative Syndrome Scale (PANSS; Reference Kay, Fiszbein and OplerKay, et al, 1987). Good insight was not required for recruitment. The mean number of previous hospital admissions was 2.6 (range 0–20), and the mean duration of illness was 8.1 years (range 0–32). The mean age was 38.1 years (range 23–62). Of the 64 participants for whom data on medication were available, 54 (84.4%) were taking an atypical antipsychotic, 7 (10.9%) a typical antipsychotic, and 3 (4.7%) were not taking any antipsychotic. The overall mean dose was 53.9% of the maximum dose.
Assessments
Insight was assessed using the self-report Insight Scale (Reference Birchwood, Smith and DruryBirchwood et al, 1994), which measures three dimensions of insight: awareness of illness (2 items), awareness of symptoms (2 items) and awareness of the need for treatment (4 items). Each sub-scale is given equal weight when calculating the total score. Item 4 (‘My stay in hospital is necessary’) was excluded because all participants were out-patients. The remaining three items from the ‘awareness of the need for treatment’ dimension were used to calculate a score for this subscale with equal weight to the other two sub-scales, allowing a total score to be calculated which has the same range (0–12) as the full Insight Scale. Higher scores indicate better insight.
The PANSS was used to assess positive, negative and general symptoms as part of the randomised controlled trial, and the PANSS G12 item was also used as an observer-rated measure of insight. Higher scores on the G12 item indicate poorer insight. Current IQ was measured using the Quick Test (Reference Ammons and AmmonsAmmons & Ammons, 1962), a picture vocabulary test consisting of 50 items. Self-esteem was assessed using the Rosenberg Self-Esteem Scale (Reference RosenbergRosenberg, 1965), a 10-item self-report questionnaire (higher scores indicate poorer self-esteem). Level of current depressive symptomatology was assessed using the Beck Depression Inventory (BDI; Reference Beck, Ward and MendelsonBeck et al, 1961), a 21-item self-report questionnaire. These measures were selected for their previous use in published studies of people with psychosis and their relatively brief administration time as part of an extensive clinical assessment.
Data analysis
Linear relationships between insight scores and other variables were examined using Pearson's correlations. Following Startup (Reference Startup1996), the possibility of quadratic relationships between insight and IQ was investigated using hierarchical regression analyses in which IQ was treated as the dependent variable and insight score (either Insight Scale or PANSS G12 item) as a predictor variable. The insight score was first entered into the regression to test for a linear relationship, followed by the square of the insight score to test for a quadratic relationship.
RESULTS
Descriptive statistics for all measures used in this study are displayed in Table 1.
Table 1 Scores on measures of insight, cognitive ability, depression and self-esteem administered to 67 people with psychosis
| Measure | Mean score | s.d. | Range |
|---|---|---|---|
| Insight Scale | |||
| Total | 8.5 | 3.3 | 0-12 |
| Awareness of symptoms 1 | 2.7 | 1.4 | 0-4 |
| Awareness of illness 1 | 2.7 | 1.4 | 0-4 |
| Awareness of the need for treatment 1 | 3.1 | 1.8 | 0-4 |
| PANSS G12 insight item | 2.7 | 1.6 | 1-6 |
| Quick Test IQ | 94.4 | 13.1 | 65-135 |
| Beck Depression Inventory | 20.6 | 11.8 | 1-54 |
| Rosenberg Self-Esteem Scale | 25.9 | 6.0 | 11-38 |
| PANSS | |||
| Positive symptoms | 17.6 | 4.9 | 11-32 |
| Negative symptoms | 12.2 | 5.0 | 7-29 |
| General symptoms | 31.8 | 7.0 | 19-50 |
| Total | 61.3 | 12.2 | 39-87 |
PANSS, Positive and Negative Syndrome Scale
1. Weighted sub-scale mean
The mean total Insight Scale score of 8.5 was comparable to that of the in-patient sample (at discharge) on which the scale was originally standardised (mean 8.1; Reference Birchwood, Smith and DruryBirchwood et al, 1994). Splitting our sample according to the cut-off score of 9 for good insight which was recommended in the original study (Reference Birchwood, Smith and DruryBirchwood et al, 1994), 30 individuals (44.8%) would be classified as having poor insight, whereas 37 (55.2%) would be classified as having good insight. This suggests that in our sample insight was slightly lower than in a recent neuropsychological study which utilised the Insight Scale (30% with poor insight; Reference Donohoe, Corvin and RobertsonDonohoe et al, 2005). As expected, the total Insight Scale and PANSS G12 measures, which are scored in opposite directions, were highly negatively correlated (r=-0.646, P<0.001).
Self-reported insight
Total Insight Scale score was correlated with higher IQ (r=0.264, P<0.05) and poorer self-esteem (r=0.382, P=0.001), but not depression (r=0.189, P>0.05). The relationship between insight and self-esteem remained significant after controlling for depression (r=0.342, P<0.005), as did that between insight and IQ (r=0.31, P=0.01). IQ and self-esteem were not related (r=0.12, P=0.3).
In the regression analysis, the linear Insight Scale component was significant (R 2 change 0.070, F change (1,65) 4.86, P<0.05), reflecting an association between higher Insight Scale score and higher IQ. The quadratic Insight Scale component was also highly significant (R2 change 0.127, F change (1,64) 10.11, P<0.005). The full model accounted for 19.6% of the variance, with an adjusted R2 of 0.17 (F (2,65) = 7.82, P<0.001). The quadratic Insight Scale component of the model remained significant when positive, negative and general PANSS sub-scale scores, as well as BDI scores, were entered into the model at the first step (R2 change 0.163, F change (1,60) 14.63, P<0.001). There was one IQ outlier more than 1.5 times the interquartile range above the upper quartile, and no Insight Scale outliers. When the analysis was run again excluding this outlier, the quadratic component of the regression remained significant.
Separate regressions for the three dimensions of the Insight Scale indicated that it was the ‘awareness of illness’ dimension which was driving the curvilinear relationship between total Insight Scale score and IQ (Fig. 1), as this was the only dimension for which the quadratic component was significant (R2 change 0.181, F change (1,64) 7.763, P<0.005). Better insight in all three dimensions was significantly associated with poorer self-esteem (P<0.015 for all), but there were no significant correlations with depression.
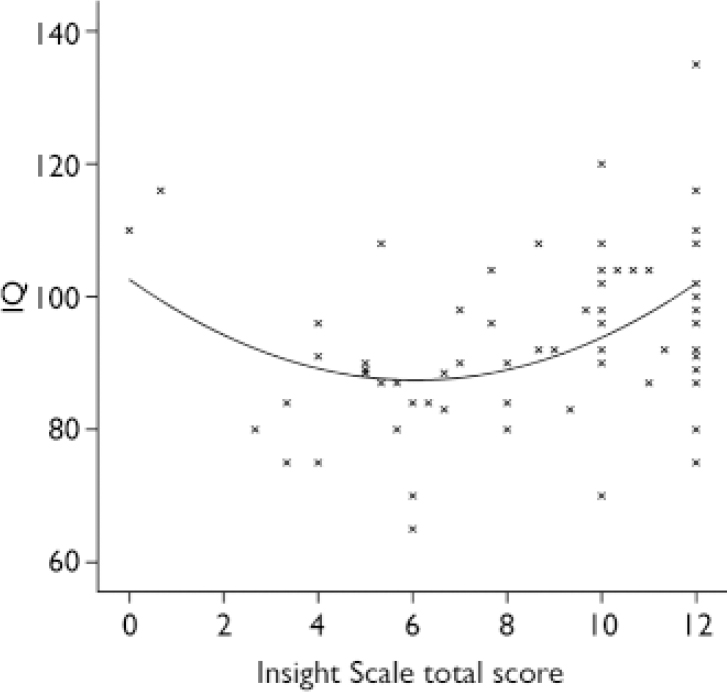
Fig. 1 Scatterplot of IQ against Insight Scale scores with fitted quadratic regression curve.
Observer-rated insight
The PANSS G12 score was not significantly correlated with IQ, self-esteem or depression. Neither the linear nor the quadratic component of the PANSS G12 regression was significant.
DISCUSSION
Main findings
This study found significant linear correlations between better self-reported insight and both higher IQ and poorer self-esteem, but not depression, in a sample of individuals with psychosis. A curvilinear (quadratic) relationship between self-reported insight and IQ was also found, and survived correction for symptom variables. This relationship was driven by the ‘insight into illness’ dimension. Despite a high concordance between the scales, no correlations with observer-rated insight were found.
It has previously been suggested that the association between insight and IQ reflects the inability of people with low IQs to communicate the presence of insight to the satisfaction of an interviewer (Reference LewisLewis, 1934; Reference Rossell, Coakes and ShapleskeRossell et al, 2003). This hypothesis is not supported by the present study, which did not find an association between observer-rated insight and IQ.
However, the linear association between total Insight Scale score and IQ is consistent with the findings of a number of previous studies (for a review see Reference Cooke, Peters and KuipersCooke et al, 2005), as well as a recent study which utilised the Insight Scale (Reference Donohoe, Corvin and RobertsonDonohoe et al, 2005). The significant curvilinear relationship between total Insight Scale score and IQ also supports the hypothesis of Green et al (Reference Green, Kern, Robertson, Sharma and Harvey2000) that there may be two influences on insight. First, high cognitive ability is conducive to, but in itself not sufficient for, having good insight. Second, some individuals may cope with psychosis in a way that promotes their own positive self-evaluation and thus manifest poor insight. The association found in this study between higher Insight Scale scores and poorer self-esteem is consistent with this, and suggests a further psychological mechanism whereby self-esteem is increased at the expense of insight, which may apply to all individuals across the IQ range. The combination of these two factors might explain why some people with high cognitive ability display good insight and others display poor insight, particularly in the ‘awareness of illness’ dimension.
In the only previous study to find a curvilinear relationship between insight and cognitive ability, Startup (Reference Startup1996) found that a composite ‘cognitive deficits’ score derived from factor analysis of neuropsychological test scores explained 56% of the variance in insight. No linear relationship with cognitive ability was found. Although we employed similar statistical methods to Startup (Reference Startup1996), our use of a single cognitive measure and a different insight scale might explain why the amount of variance accounted for by the regression model in this study was modest (20%), and why a linear as well as a curvilinear relationship, was found. Furthermore, although the Quick Test has been used in a number of studies of people with psychosis (e.g. Reference Kondel, Mortimer and LeesonKondel et al, 2003), some evidence (Reference Mortimer and BowenMortimer & Bowen, 1999) suggests that it overestimates IQ in this population. This may have influenced the results, particularly the high IQ outliers. Nevertheless, these data support the curvilinear relationship between cognitive ability and insight in a sample of out-patients with psychosis and complement the results from a sample of in-patients investigated by Startup (Reference Startup1996). The findings support the view that the relationship between insight and cognition may be complex, and may reflect an interaction between cognitive abilities and other factors, such as the way a person copes with psychosis. Poor insight, especially in people with good intellectual function, may be adaptive and serve to protect against low self-esteem.
Implications
Self-report measures of insight may be more sensitive to associations with variables relevant to the aetiology of insight than single items from general symptom rating scales. Different dimensions of insight may have different psychological and cognitive correlates.
The finding that better insight is associated with poorer self-esteem, but not greater depression, suggests that insight might be more strongly related to stable, core beliefs about self-worth in people with psychosis than their current level of depressive symptomatology, which may be a result of a number of other factors, such as current social situation. If a person believes that they are mentally well despite disagreements with clinicians (‘poor insight’), this might help to maintain positive core beliefs about the self and promote good self-esteem. Therefore poor insight could be viewed as an adaptive response to a diagnosis of a serious mental illness with respect to psychological well-being, although it can have maladaptive effects on other areas of functioning, such as engagement with services and taking medication.
Limitations
There are limitations to the generalisability of this study's sample, since it was composed of out-patients who were recruited to a trial of cognitive–behavioural therapy for psychosis. Although the mean level of insight was comparable with samples reported in other studies using the Insight Scale (Reference Birchwood, Smith and DruryBirchwood et al, 1994; Reference Donohoe, Corvin and RobertsonDonohoe et al, 2005), our participants might not have been representative in other ways, such as being more engaged with services, more motivated and less cognitively impaired. Detailed information on the psychiatric diagnosis was not available. Moreover, the curvilinear relationship between self-reported insight and cognitive ability was modest and requires replication.
Acknowledgements
M.C. was supported by a Wellcome Trust Prize Studentship (072298/z/03/z). V.K. is supported by a Wellcome Trust Senior Research Fellowship (067427/z/02/z).





eLetters
No eLetters have been published for this article.