There is an ongoing debate about whether separate psychiatrists should be responsible for in- and out-patient care (functional care) or whether patients should be treated by the same psychiatrist across both settings (sectorised care).Reference Begum, Brown, Pelosi, Crabb, McTaggart and Mitchell1–Reference Omer, Priebe and Giacco4 Over the past decade, various mental health services in the National Health Service (NHS) in England have moved away from the traditional sectorised forms of care, with the majority of the 58 mental health trusts now operating a functional split. It has been argued that these changes towards functional care, which were often costly from both a financial and resource perspective, would improve in-patient care. Yet, so far, there has been no high-quality evidence supporting this claim.Reference Begum, Brown, Pelosi, Crabb, McTaggart and Mitchell1, Reference Burns2 This study aims to provide such evidence and compares two key indicators of the quality of in-patient treatment – patient satisfaction and length of stay (LoS) – in functional and sectorised care.
Method
Design
Data from the present study is taken from ‘Comparing policy framework, structure, effectiveness, and cost effectiveness of functional and integrated systems of mental health care study (COFI)’ – a European Union study being conducted across five European countries (Belgium, England, Germany, Italy and Poland) (trial registration: ISRCTN40256812). COFI is a natural experiment assessing the outcomes of different ways of organising the link between in- and out-patient care. The full protocol for the COFI study has been previously published.Reference Giacco, Bird, McCrone, Lorant, Nicaise and Pfennig5 For comparing satisfaction with in-patient care and LoS in functional and sectorised care, this paper focuses on the English site, as in England – unlike in other countries – the allocation of a patient to either functional or sectorised care is determined by location alone and not influenced by the characteristics of the patient.
Setting
A total of 23 hospitals were included in the study from 11 NHS trusts in England. In 11 hospitals run by five trusts (Camden and Islington NHS Foundation Trust, Manchester Health and Social Care Trust, North East London NHS Foundation Trust, Oxford Health NHS Foundation Trust and South Staffordshire, Shropshire and Shrewsbury NHS Foundation Trust) functional care was provided. In nine hospitals of five other trusts (East London NHS Foundation Trust, Cornwall Partnership Foundation Trust, Bradford District Care Trust, Dudley and Walsall Mental Health Partnership Trust and Pennine Care NHS Foundation Trust) sectorised care was provided. In one trust (North Essex Partnership Foundation Trust), both sectorised and functional care were routinely in operation, with functional care in two hospitals, and sectorised care in one other hospital.
Eligibility criteria
The hospitals included in the study were selected to represent a range of settings across England including urban, semi-urban and rural areas. To be included, the current form of care (i.e. sectorised or functional) needed to be in routine operation for at least 1 year and the hospital was required to have no plans to change the type of care they provided for the duration of the study. This meant that hospitals were excluded, even if run by a participating trust, if the current model of care had not been in place for at least 1 year, leading to the exclusion of three hospitals. All general adult psychiatric wards within an included hospital took part in the study, giving a total of 80 wards.
Patients were eligible if they met the following criteria: (i) a formal ICD-10 diagnosis6 (primary or secondary) of psychotic disorders (F2), affective disorders (F3) or anxiety/somatoform disorders (F4) or if they had a working diagnosis of F2–F4 as confirmed by the treating clinician; (ii) 18 years of age or older; (iii) admitted to a general adult psychiatric in-patient ward; (iv) capacity to provide informed consent; and (v) sufficient command of English to provide written informed consent and understand the questions in the research interviews. Patients with an organic brain disorder or too severe cognitive impairment to enable completion of the study measures were excluded. Additionally, patients who did not have a confirmed diagnosis at admission, and who did not go on to receive a confirmed F2–F4 diagnosis (at discharge) were excluded from the study, and no further data collected. No upper age limit was applied, providing the individual was recruited from an adult acute ward.
Measures
Outcomes for the study were mean satisfaction scores as rated on the Client Assessment of Treatment Scale (CAT)Reference Priebe and Gruyters7 and length of hospital stay for the hospital admission for which they were included in the study. The CAT is a seven-item patient-reported outcome measure developed to assess satisfaction with in-patient care.Reference Priebe and Gruyters7 The seven items included in the measure assess satisfaction with (i) treatment received; (ii) engagement with the psychiatrist; (iii) relations with other staff members; (iv) medication; (v) other elements of treatment; (vi) feeling respected; and (vii) whether the patient feels the treatment is right for them. All seven items are rated on a Likert scale ranging from 0 (not at all/very unpleasant) to 10 (yes entirely/very pleasant) and the overall mean score per item is calculated for the measure.Reference Priebe and Gruyters7 The measure had been widely used with more than 4000 psychiatric in-patientsReference Kallert, Priebe, McCabe, Kiejna, Rymaszewska and Nawka8–Reference Priebe, Jones, McCabe, Briscoe, Wright and Sleed11 and has been demonstrated to have good internal consistencyReference Katsakou, Bowers, Amos, Morriss, Rose and Wykes10 and internal validity,Reference Priebe, Katsakou, Amos, Leese, Morriss and Rose9 as well as demonstrating factorial invariance and good factorial validity.Reference Richardson, Katsakou, Torres-González, Onchev, Kallert and Priebe12
Additionally, the following variables were collected for each patient: (i) sociodemographic characteristics; (ii) social situation including employment, accommodation, living situation, friendships, being in receipt of benefits; (iii) psychiatric and non-psychiatric diagnoses according to the ICD-10, with the primary clinical diagnosis at discharge established from the discharge summary and/or medical records; (iv) severity of illness as rated by the treating psychiatrist using the Clinical Global Impression Scale (CGI);Reference Guy13 and (v) admission details including date of admission and discharge, whether the current admission is the first one or not; and formal status at admission (involuntary/voluntary). Sociodemographic characteristics and social situation were completed by patients, and all clinical information was obtained from medical records.
Procedure
All new admissions to general adult psychiatric wards within the included hospitals were screened on every working day between 20 August 2014 and 31 December 2015. Individuals who met the inclusion criteria were initially approached by a member of the clinical team within 2 working days of admission. Where individuals did not have capacity to provide informed consent, they were re-approached in the following days. Trained researchers (from a psychology, nursing or psychiatry background) completed the assessment booklet with the participant. Medical records were used to collect clinical data such as date of admission and discharge, diagnosis at admission, primary diagnosis at discharge, legal status and additional physical health diagnoses. Following completion of the assessment, the patient's treating clinician was approached to complete the CGI measure regarding the patient's clinical status at admission. Each individual was only included in the study once, regardless of the number of admissions during the recruitment period. Patients were approached within 2 days of admission and attempts were made to assess patients within the first days to (i) avoid selection biases through early discharge; and (ii) have a consistent time frame rather than linking assessments to variable discharge dates. Ethical approval for the study was obtained from NRES Committee North East – Newcastle & North Tyneside (ref: 14/NE/1017).
Data analysis
The mean for the CAT was calculated for each person. As data was collected at the time of recruitment, missing data were minimal. Where 20% of the data or less were missing for the CAT, the means of the non-missing items were used to replace missing values. LoS was defined as the number of nights the person was admitted calculated from the date of admission and date of discharge, which were always obtained from medical records. The mean LoS was calculated to allow for us to control for the effects of clustering at the hospital level and the impact of covariates within the analysis. The first quartile, second quartile (median) and third quartile LoS were also calculated because of the non-normal distribution of the data and the potential outliners at the right end of the distribution. Additionally, Kaplan–Meier survival curves were drawn for functional and sectorised care.
Descriptive statistics for all sociodemographic, social and clinical variables were tabulated for the two forms of care and any differences between them assessed using t-tests (for continuous data) or chi-squared tests (for categorical data). Descriptive statistics were also calculated for the seven individual items on the CAT; however, we did not test for any significant differences between functional and sectorised care at the item level as the individual item scores as such have not been developed for this purpose.Reference Priebe and Gruyters7
Mixed-effects linear regression with unstructured variance matrix was used to test for the impact of model of care (i.e. specialisation or functional) on the CAT. As per protocol, within the models, hospital was added as a random effect to adjust for clustering, whereby individuals recruited and receiving treatment from the same hospital were clustered together. The following covariates that were pre-specified in the data analysis plan were included as fixed effects: age, gender, severity of illness, first or repeat admission and legal status. Any variables shown to significantly differ at baseline between the two systems were included in the model. Given that LoS was not normally distributed, we conducted a quantile regression to test for significant differences in the first, second or third quartiles for LoS. The quantile regression used clustered standard error and the same covariates as applied within the regression model. Additionally, because of the large sample size, mixed-effects linear regression with unstructured matrix was used to confirm the findings of the quantile regression. As LoS represents duration data, a sensitivity analysis was conducted to analyse the data using a multilevel generalized linear model (GLM) with gamma distribution.
Results
A total of 8771 participants were screened within the study period. Of these, 6224 were eligible for inclusion and 3021 recruited, giving an opt-in rate of 48.5% (Fig. 1). Of the recruited participants, 312 individuals (10.3%) were retrospectively excluded at the point of discharge as the working diagnosis of F2–F4 was not confirmed. In total, 2709 eligible individuals were recruited and included in the analysis, of which 1612 received functional and 1097 sectorised care.
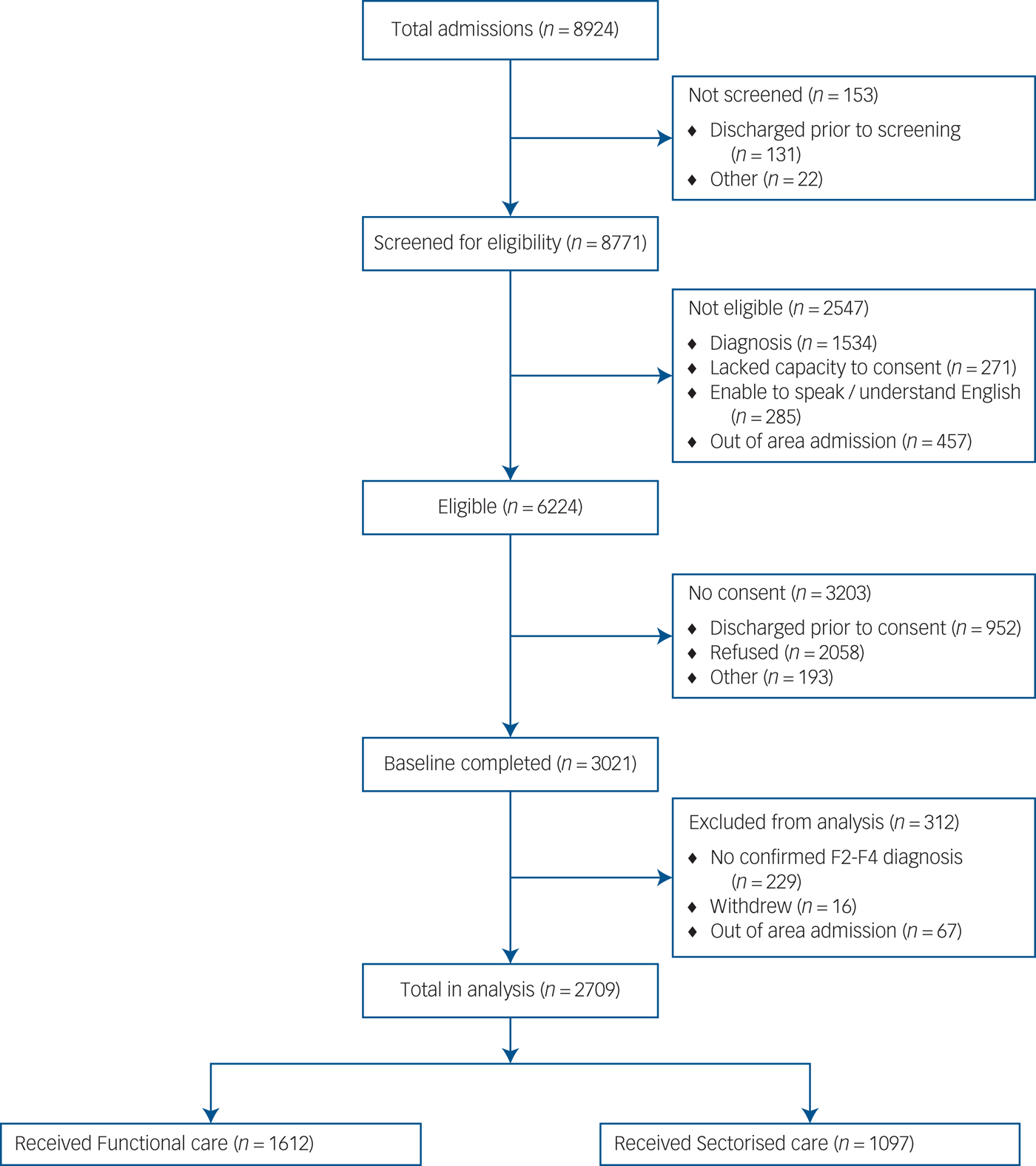
Fig. 1 Flow chart of participants through the study.
Characteristics of the participants are shown in Table 1. The average age of participants was 40.6 years and 58.5% were male. There was a statistically significant difference in the level of education, with a lower proportion of individuals within sectorised sites having completed tertiary education and a greater proportion completing primary or secondary education compared with functional care. Additionally, the proportion of people born in the UK differed between patients in the two systems. All other sociodemographic variables did not differ. In total, 1155 patients (42.6%) had a diagnosis of a psychotic disorder (F2), 1371 (50.6%) a diagnosis of an affective disorder (F3) and 427 (15.8%) had an anxiety/somatoform disorder (F4). There were no significant differences in the proportion of participants with psychotic or affective disorders between the two groups; however, the proportion of patients with a diagnosis of anxiety disorder was higher for those receiving sectorised care. Finally, more individuals receiving functional care were admitted involuntarily (45.5% v. 38.2%).
Table 1 Participant characteristicsa
a. In all cases, n, % may be slightly less than 100% due to missing data.
b. Overall percentage is greater than 100% as figures represent any confirmed diagnosis (including comorbid diagnoses).
*Difference between groups P<0.05; **difference between groups P<0.01.
Satisfaction with care
On average patients were interviewed 5.9 days following admission (median 3 days, range 0–87 days; working days mean 4.1, median 2). The overall mean score for patient satisfaction with care across the CAT for the whole sample was 6.7 (s.d. = 2.5). Mean satisfaction with care was 6.6 (s.d. = 2.5) for functional and 7.1 (s.d. = 2.3) for sectorised care. At an individual-item level the mean difference between satisfactions scores for functional and sectorised care ranged from 0.4 to 0.8, and was always favouring sectorised care.
Satisfaction with care was significantly greater for patients receiving sectorised care (β = 0.54, 95% CI 0.35–0.73, P<0.001). This difference remained significantly higher when adjusting for clustering at the hospital level (β = 0.50, 95% CI 0.17–0.82, P = 0.003) and all other covariates (β = 0.40, 95% CI 0.06–0.74, P = 0.020). This represented a small effect size always favouring sectorised care (d = 0.12, 0.09 and 0.07 unadjusted, adjusted for clustering and fully adjusted model, respectively).
LoS
The mean LoS across the sample was 46.4 days (s.d. = 63.5). The mean LoS for functional care was 49.1 days (s.d. = 67.3), whereas for sectorised care it was 42.3 days (s.d. = 57.3). Across the whole sample, the first, second (median) and third quartiles were 11, 25 and 52 days. In functional care they were 12, 26 and 55 days, and in sectorised care 10, 24 and 49 days, respectively. Quantile regression (QR) indicated that patients receiving sectorised care had significantly shorter stays at all quartiles compared with those admitted in hospitals providing functional care (1st quartile QR coefficient −2, 95% CI −3.17 to −0.28, P = 0.023, 2nd quartile QR coefficient −2, 95% CI −4.01 to −0.01, P = 0.051 and 3rd quartile QR coefficient −6, 95% CI −12.14 to −0.01, P = 0.052). However, the difference was no longer statistically significant when clustering at the hospital level was accounted for (1st quartile QR coefficient −2, 95%CI −6.29 to 2.28, P = 0.361, 2nd quartile QR coefficient −2, 95% CI −6.99 to 2.99, P = 0.432 and 3rd quartile QR coefficient −6, 95%CI −14.8 to 2.80, P = 0.182) and after adjusting for clustering and covariates (1st QR coefficient −0.75, 95% CI −5.18 to 3.68, P = 0.740, 2nd QR coefficient −0.40, 95% CI −5.33 to 4.53, P = 0.847 and 3rd QR coefficient −0.29, 95% CI −10.41 to 9.83, P = 0.955). A Kaplan–Meier curve visually representing LoS for functional and sectorised care is shown in Supplementary Fig. 1 (available online at http://dx.doi.org/10.1192/bjp.2017.20).
To test the robustness of the quartile regression two sensitivity analyses were conducted, first because of the large sample size a mixed-effect linear regression was conducted using the means. Consistent with the above, patients receiving sectorised care had a significantly shorter admission by approximately 7 days compared with those admitted in hospitals providing functional care (β = −6.89, 95% CI −11.76 to −2.02, P<0.001). However, when adjusting for clustering, this difference was no longer statistically significant, and the number of days explained by the system of care was reduced to 4.9 days (β = −4.89, 95% CI −13.34 to 3.56, P = 0.257). The number of days difference accounted for by the system of care was further reduced to 2 days when other covariates were added to the model (β = −2.44, 95% CI −10.22 to 5.34, P = 0.539).
Second, as LoS data had a non-normal distribution, a further sensitivity analysis was conducted using a multilevel GLM with gamma distribution. As before, the results indicated a significant difference between functional and sectorised care (coefficient −0.15, 95% CI −0.26 to −0.05, P = 0.004), which was no longer significant when adjusting for clustering at the hospital level (coefficient −0.10, 95% CI −0.29 to 0.09, P = 0.292) and other covariates (coefficient −0.09, 95% CI −0.28 to 0.10, P = 0.335).
Discussion
Main findings
Patients who receive sectorised mental healthcare are significantly more satisfied with their in-patient care compared with patients who receive functional care. This higher patient satisfaction was found in the first week after admission. The difference remained significant when the findings were adjusted for the influence of other factors such as locality of services, legal status, first or repeat admission and illness severity. Although patients in sectorised care stayed on average 7 days fewer than those in functional care, this difference was no longer significant once clustering by the hospital had been accounted for, suggesting factors aside from the organisation of care and patient characteristics have an impact on LoS.
Strengths and limitations
The data for the present study were collected in a natural experiment where the exposure of patients to either sectorised or functional care was outside the control of the investigators.Reference Giacco, Bird, McCrone, Lorant, Nicaise and Pfennig5 A key limitation of existing studies is that they often assessed the effectiveness of a new system, where initial enthusiasm for newly introduced changes may influence the results. A previous review identified such a novelty effect.Reference Omer, Priebe and Giacco4 Consequently, a major strength of the present study is that we did not introduce a new system. Instead, sectorised or functional care was in routine practice for at least 1 year prior to the study. Thus, any systematic bias introduced by novelty effects was minimised. Within each site, allocation to sectorised or functional care was determined by geography and not influenced by the characteristics of the patient. Additionally, the study is one of the largest ever conducted with psychiatric in-patients within the UK. The large sample size, which is more than ten times larger than other studies directly comparing sectorised and functional care, enabled us to test for small differences, which at a national level may have wide implications. Finally, the study aimed to approach all potentially eligible participants within 2 working days after admission, with interviews conducted on average 6 days following admission. Often in-patient studies have assessed patients at least 1 or more weeks following admission, at the point of discharge or have collected satisfaction data retrospectively. This may bias the included sample, as individuals with a short admission may not be included. Research has also indicated that the appraisal of care changes during hospital admission.Reference Katsakou, Bowers, Amos, Morriss, Rose and Wykes10
There are also a number of limitations. Most notably, this was not a randomised controlled trial (RCT), therefore, there may be non-random differences between the groups because of locality and the clinical and participant characteristics of the local area. Within the present study any patient characteristics shown to differ between the two systems were adjusted for. Furthermore, aside from the methodological problem of implementing a new system, one may argue that it would be practically impossible to randomly allocate a sufficient number of hospitals to sectorised and functional systems to conduct a formal RCT. Hospitals also varied in the types of acute wards provided. For instance, several hospitals included a triage or assessment ward, which impose a maximum stay before the patient is either discharged or transferred. However, existing evidence has suggested that the overall LoS for the hospital admission is not reduced by the use of these wards.Reference Williams, Csipke, Rose, Koeser, McCrone and Tulloch14 Finally, the opt-in rate of 48.5% may make generalisability to all patients difficult, particularly if more unwell patients refused participation. However, there were no differences between the two types of care in the opt-in rates or various patient characteristics including illness severity, suggesting selection bias is unlikely to explain the results.
Links with the existing evidence
Qualitative studies assessing the experience of patients and clinicians have highlighted the benefits of both models of care, whereas quantitative studies directly addressing patient satisfaction tend to favour sectorised care.Reference Omer, Priebe and Giacco4 However, the majority of studies have investigated whether patients have a general preference for the same or different psychiatrists across settings, rather than investigating their actual experience.Reference Begum, Brown, Pelosi, Crabb, McTaggart and Mitchell1 Additionally, studies have been limited by a number of factors including the implementation of a new system of care usually as part of the study,Reference Lambert, Bock, Schottle, Golks, Meister and Rietschel15 only focusing on patient satisfaction with the psychiatrist,Reference Laugharne and Pant16 and/or including only a small number of patients ranging from 41Reference Le Bas, King and Block17 to 255.Reference Begum, Brown, Pelosi, Crabb, McTaggart and Mitchell1 The present study overcomes each of these limitations to provide more robust evidence.
One suggestion for the higher satisfaction of patients found in sectorised care is the impact of personal continuity. Participants in previous studies have highlighted how developing a positive therapeutic relationshipReference Poremski, Harris, Kahan, Pauly, Leszcz and O'Campo18 and building trustReference Shan, Li, Ding, Wu, Liu and Jiao19 may be harder to achieve if different clinicians are seen across settings. For instance, although not specific to psychiatrists, a higher turnover of mental health staff is associated with poorer patient outcomesReference Puntis, Rugkasa and Burns20 and lower levels of satisfaction.Reference Sanatinia, Cowan, Barnicot, Zalewska, Shiers and Cooper21 Alternatively, the difference in satisfaction may be because of the attitude and behaviour of staff working in the different services. For example, there is some evidence to suggest that staff prefer the sectorised model of care.Reference Omer, Priebe and Giacco4 This preference and awareness of longer-term responsibility by the clinicians may influence their behaviour and hence have an impact on patient experience. However, the present study did not assess such potentially mediating factors. Future research should explore in depth the processes that mediate the impact of service organisations on patient satisfaction. This may include detailed organisational procedures, staff attitudes and behaviours as well as actual patient–clinician interactions during the in-patient admission.
Although the results show a clear finding regarding patient satisfaction, the comparison of LoS was not so clear-cut. The admission for patients receiving sectorised care was on average 7 days shorter than for those receiving functional care. The differences for the mean and median were not statistically significant once adjusting for other factors, including the hospital. This lack of statistical significance – despite the large sample size – reflected the large amount of variability in LoS. It is likely that LoS is influenced by a complex mix of factors above and beyond the model of care provided, including variables at the hospital level such as bed pressure, treatment practices, local clinical governance procedures and characteristics of the local area, as well as patient characteristics. In any case, one may conclude from the findings that functional care was not associated with shorter LoS.
The lack of an association of care organisation with LoS may be seen as consistent with previous research. Patient characteristics such as severity and chronicity of illnessReference Nakanishi, Niimura, Tanoue, Yamamura, Hirata and Asukai22, Reference Zhang, Harvey and Andrew23 and a lack of social supportReference Zhang, Harvey and Andrew23, Reference Gigantesco, de Girolamo, Santone, Miglio and Picardi24 are all linked to longer LoS. Yet, good clinical care and the quality of services provided does not always result in reduced LoS once patient characteristics have been controlled for.Reference Zhang, Harvey and Andrew23 Further research is needed to explore the individual patient factors and hospital factors, including the attitudes and behaviours of clinicians, which may be linked to shorter hospital admissions.
Implications
The study findings provide evidence for the ongoing debate about the pros and cons of a functional split of psychiatrist responsibility between in- and out-patient care.Reference Burns and Baggaley3 Despite the central importance of this question for patients and clinicians alike, decisions to change from one system to another – in England mostly from a sectorised to a functional one – have been made in the absence of any high-quality evidence.
In their debate article, Burns & Baggeley outline the potential benefits of both sectorised care and a functional split in psychiatrist responsibility.Reference Burns and Baggaley3 Arguments for reconfiguring services have frequently included the stressful nature of in-patient wards, improving ward throughput, reducing bed occupancy and making the workload of the consultant psychiatrist more manageable.Reference Burns and Baggaley3 It has therefore been suggested that a functional split facilitates the management of in-patient wards and improves the quality of in-patient care.Reference Tulloch, Soper, Gorzig, Pettit and Koeser25 However, counterarguments for sectorised care point to the increased fragmentation within functional services and to increased patient and clinician satisfaction potentially as a result of the higher chance of developing a positive therapeutic relationship in sectorised systems. The present study provides the first sound evidence that patient satisfaction with in-patient treatment is greater in sectorised care. Thus, arguments for improved quality of care following a functional split are not supported. On the contrary one might argue that if patient satisfaction is a key indicator of quality of care, trusts may consider a transition back to a sectorised model – which has been the case in one of the trusts (Bradford District Care Trust) included in the study.
The Francis inquiry report examining causes of the failings in care provided by Mid Staffordshire NHS Foundation Trust between 2005 and 2009, highlighted the importance of patient satisfaction to health service providers.Reference Francis26 Higher patient satisfaction with in-patient treatment is an important outcome in its own right, especially since satisfaction with in-patient care has deteriorated in recent years.Reference Csipke, Williams, Rose, Koeser, McCrone and Wykes27 Satisfaction is also an indicator for longer-term clinical outcomes. When assessing the outcomes of involuntary hospital admission, patient satisfaction with in-patient treatment was the only factor associated with both objective and subjective outcomes at 1 year follow up. In particular, higher initial treatment satisfaction was associated with lower rates of involuntary readmission and with a more positive appraisal of the admission retrospectively.Reference Priebe, Katsakou, Amos, Leese, Morriss and Rose9
In summary, the present study suggests that the current trend in the NHS of transforming services to functional care needs reconsidering. Sectorised care appears preferable in the interest of higher patient satisfaction with in-patient treatment.
Funding
This study was funded by the European Commission seventh Framework Programme. Grant agreement number is 602645. The views expressed in this publication are those of the authors and not necessarily those of the National Health Service, European Commission or Queen Mary University.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2017.20.
Acknowledgements
The authors would like to grateful acknowledge the support of the funders, participants and wider COFI study group.





eLetters
No eLetters have been published for this article.