Young people with psychotic illness, as part of their recovery, want to complete their education and gain employment more than they want to address their mental health symptoms.Reference Ramsay, Broussard, Goulding, Cristofaro, Hall and Kaslow1 Despite this, the vocational trajectory of young people with psychosis is marked by low educational completion ratesReference Waghorn, Saha, Harvey, Morgan, Waterreus and Bush2 and rapid transition into unemployment.Reference Rinaldi, Killackey, Smith, Shepherd, Singh and Craig3 Typically, the employment needs of young people with mental illnesses are referred out from mental health services to private- or government-contracted employment providers. Young people with mental ill health often have difficulty accessing these services,Reference Scott, Fowler, McGorry, Birchwood, Killackey and Christensen4 and even where they do, employment outcomes are scandalously low.5 The individual placement and support (IPS) model was designed to assist people with chronic severe mental illness to return to mainstream employment. IPS has been very successful,Reference Bond6 even showing resilience to external economic downturns.Reference Modini, Tan, Brinchmann, Wang, Killackey and Glozier7 Most of the previous studies of IPS have been in populations of people with chronic illness. Two small trialsReference Nuechterlein, Subotnik, Turner, Ventura, Becker and Drake8, Reference Killackey, Jackson and McGorry9 in young people with first-episode psychosis (FEP) have shown very promising results. In this paper we report on a large randomised controlled trial (RCT) of IPS in a FEP population over an 18-month follow-up period (Australian and Clinical Trials Registry ACTRN12608000094370). This allows for an examination of employment outcomes at the end of the intervention as well as the duration of effects of IPS.
Method
The background and methodology of the study has been described in detail elsewhere.Reference Killackey, Allott, Cotton, Jackson, Scutella and Tseng10 Key aspects of the study methodology as well as specific details concerning the participants, interventions and analyses are briefly described here. The study received ethical approval from the Melbourne Health Mental Health Research and Ethics Committee.
Trial design
This study was a parallel single-blinded RCT comparing IPS with treatment as usual (TAU) on employment and education outcomes in young people with FEP. Sample size was determined based on the results of our pilot studyReference Killackey, Jackson and McGorry9 and calculated using SamplePower 2.0. Randomisation was undertaken by the study statistician (S.M.C.) using a computer program for blocked randomisation in random permutated blocks of four and eight with an allocation ratio of 1:1. Use of permuted blocks was in order to prevent prediction of group membership before it was assigned. The statistician was not associated with assessments and treatments and was the only person aware of the allocation sequence. Group allocation was provided to the study lead who informed the employment consultant and the participant's case manager of the participant's group allocation. All effort was taken to keep research assistants masked to study condition. Research assistants had no contact with the employment consultant, and participants were reminded at the start of each assessment that they were not to let the research assistant know whether they had been working with the employment consultant or not. Recruitment occurred over a 3-year period.
Participants
Young people with FEP who had expressed an interest in vocational recovery were approached to participate. Those who agreed to participate were required to provide written informed consent, or in the case of minors have parents/guardians provide written informed consent with the participants providing written informed assent. Participants were clients of the Early Psychosis Prevention and Intervention Centre (EPPIC) in Melbourne, Australia. EPPIC, a component programme of Orygen Youth Health Clinical Program, is a public mental health programme that treats all young people with a FEP living in a geographically defined catchment area in the west and north-west of Melbourne. The catchment has a population of approximately one million people, with approximately 250 000 in the EPPIC age range of 15–25 years. Exclusion criteria were lack of fluency in English or an inability to consent because of acute symptomatology. There were no other exclusion criteria.
Interventions
The interventions being compared were IPS and TAU. IPS has been extensively describedReference Drake, Bond and Becker11 and researched,Reference Bond6 primarily in populations of people with chronic psychotic illness. IPS was delivered by a vocational specialist who had a background working in general and disability employment. In keeping with the IPS principles the vocational specialist (G.C.) was embedded as a member of the clinical team. Participants in the IPS group received 6 months of the IPS intervention.
TAU in Australia, as well as in many other similar health systems and economies, involves referral to external government-contracted employment agencies, some focused on disability employment and others on non-disabled populations of unemployed people. Apart from the referral, there is typically little follow-up between mental health and employment agencies. The burden of navigating the different systems often falls on the individual. In many countries, and particularly in Australia, people with a mental illness are able to opt out of any welfare-related obligation to seek employment via certification of a medical condition from their medical practitioner.
In addition to trial interventions, all participants continued to receive standard EPPIC treatment, including medical management and review, out-patient case management, access to EPPIC group programme and peer and family support.
Outcomes
The primary outcome of the study was employment over the first 6 months (0–6 months) of the intervention with secondary employment outcomes between 6–12 and 12–18 months post-baseline. Consistent with previous IPS literature,Reference Killackey, Jackson and McGorry9, Reference Bejerholm, Areberg, Hofgren, Sandlund and Rinaldi12–Reference Oshima, Sono, Bond, Nishio and Ito14 employment was defined as working in a job that paid the legislated minimum wage for a minimum of 1 day in the previous 6-month period. Although this may not seem like much work, it should be remembered that Australian and international definitions of employment consider employment to be work for wages or other in-kind payment for a period of at least 1 hour in a specified period (for example a week).15 Further secondary measures assessed at the 6-month intervals were duration of employment (measured in hours), educational outcome (measured in enrolment in an educational course) and receipt or not of government benefits. No measures were made of attendance at the education course, or level of academic success.
Other secondary outcomes, not reported in this paper, were symptomatology, social and economic participation, self-reported health service usage and an evaluation of the economics of the intervention.
Data analysis
Analyses were conducted using IBM SPSS Statistics Version 22 and Stata/IC 14.1 for Windows. To determine baseline demographic and clinical differences between the IPS and TAU groups, chi-square (χ2) and independent samples t-tests were used. These same inferential statistics were used to test for differences on baseline and clinical variables between those who did and did not have post-randomisation and follow-up assessments (at 6, 12 and 18 months).
For the analysis of primary and secondary outcomes, a modified intent-to-treat method was used with all participants with at least one follow-up assessment post-randomisation included in the models.Reference Polit and Gillespie16 For the analysis of the primary outcome measure of employment over 6-month intervals (0–6, 6–12 and 12–18 months, yes/no), the ‘xtlogit’ (random-effects model) command from Stata/IC 14.1 for Windows was used. This allows for the use of panel data accrued at different time points. In the model for the primary outcome, the core predictors were treatment group (IPS v. TAU), time periods (0–6, 6–12, 12–18 months), employment at baseline assessment (yes/no, a covariate) and the interaction between group and time period. The estimated probabilities for the 0–6, 6–12 and 12–18 months are reported from this model. Sensitivity analyses were conducted using models adjusted for imbalances that might be present at baseline. This approach was also used to analyse the data for the secondary outcome variables of studying status (yes/no) and dependence on government benefits (yes/no). For the analysis of the secondary outcome of hours of work, a mixed-model repeated measures was conducted using IBM SPSS Statistics Version 22.0. Within this model, the core predictors were again treatment group and time periods, and the interaction between these two variables. The Toeplitiz covariance structure was used to model the relations between observations on different occasions.
Results
Sample characteristics
There were 171 individuals assessed for eligibility to the study. Of these 171, 25 were excluded and 146 were randomised. Of the 25 that were excluded, 23 declined to participate (5 of those began baseline assessment but declined to continue) and 2 were too unwell to participate (see Supplementary Fig. 1 available at https://doi.org/10.1192/bjp.2018.191).
The majority of the cohort were male, never married, Australian born and were not studying or working at entry into the study. Most were in receipt of government benefits (Table 1). Table 2 includes details of Axis I diagnoses. The most common psychotic disorders were schizophreniform/schizophrenia, followed by bipolar disorder and schizoaffective disorder. Comorbid substance use and anxiety disorders were common in the cohort.
Table 1 Baseline demographic data of the total cohort and separately for the individual placement and support (IPS) and treatment-as-usual (TAU) groups
VCE, Victorian Certificate of Education; VCAL is Victorian Certificate of Applied Learning – year 12 courses.
a. χ2−value derived from comparison of collapsed categories (studying or not studying).
b. Centrelink is the Australian national welfare agency responsible for managing welfare payments.
c. Missing = 1
d. Missing = 7
e. Missing = 2
f. Missing = 5
Table 2 Diagnostic, clinical, functioning and quality of life (QoL) characteristics of the individual placement and support (IPS) and treatment-as-usual (TAU) groups at baseline
a. Degrees of freedom were adjusted for the t-test because of violation to the assumption of homogeneity of variance.
b. Based on the sum of the global items.
c. Based on the sum of the 20 individual items.
Representativeness
Over the 3 years of recruitment the potential pool of participants was about 800. Of this pool, approximately 50% are estimated to be unemployed based on our and others’ previous work.Reference Rinaldi, Killackey, Smith, Shepherd, Singh and Craig3, Reference Killackey, Jackson, Gleeson, Hickie and McGorry17 In this population it has been shown that 53% of people with FEP expressed a desire to find employment.Reference Ramsay, Broussard, Goulding, Cristofaro, Hall and Kaslow1 In our study we approached 171 people and we believe that the recruited sample was representative of the population of individuals with FEP seeking employment.
A number of the participants were in employment at baseline (IPS 21.9%, TAU 11.0%, χ2 (1) = 3.19, P = 0.074). Previous Australian studies of FEP have found employment rates between 22 and 25%.Reference Waghorn, Saha, Harvey, Morgan, Waterreus and Bush2, Reference Cotton, Lambert, Schimmelmann, Filia, Rayner and Hides18 Before we commenced research in this area we conducted a survey of EPPIC clients. This found that 29% were in employment.Reference Killackey, Jackson, Gleeson, Hickie and McGorry17 In the present study there were 16% in employment at baseline again suggesting a representative group seeking assistance through this trial.
Baseline characteristics
The two treatment groups differed significantly with respect to gender distribution, χ 2(1) = 9.28, P = 0.002, with the IPS having twice the number of female participants compared with the TAU group (Table 1). There were no significant between-group differences with respect to psychotic symptoms, overall functioning and type of psychotic disorder; however, the TAU group were significantly more likely to have a substance use disorder at baseline, χ 2(1) = 3.99, P = 0.046 (Table 2).
The IPS group was significantly more depressed, t(143) = 2.38, P = 0.019 (Table 2), had poorer psychological quality of life (QoL, t(143) = −2.27, P = 0.025) and poorer physical health QoL (t(143) = −2.34, P = 0.021) at baseline compared with the TAU group. They had also been in the EPPIC service longer (IPS 301.97 days v. TAU 215.99 days (t(139) = 2.70, P = 0.008)).
Participant flow
There were 95 participants who had complete employment data over the 18 months. A range of missing data patterns were observed: (a) 1 participant was missing 6-month data only; (b) 5 participants had only 12-month data missing; (c) 1 participant was missing 6- and 12-months data; (d) 3 participants had missing data for 6 and 18 months; (e) 15 participants had 12- and 18- month data missing; and (f) 11 participants were missing 18-month data only. There were 15 participants who had no data for any of the follow-up data points. Therefore, post-randomisation data was available for 131 participants.
Of those with no post-randomisation data, seven had moved out of the catchment area, two withdrew participation as a result of having employment, five withdrew consent with no reasons provided, and one withdrew consent because of lack of time. The TAU group (16.4%, n = 12) was more likely to have no post-randomisation data than the IPS group (4.1%, n = 3), χ 2(1) = 6.02, P = 0.014.
Despite the differences in availability of post-randomisation data, there were no significant differences between the two groups with respect rates of missingness at 6 months (IPS 9.6%, n = 7; TAU 17.8%, n = 13) χ 2(1) = 2.09, P = 0.149; at 12 months (IPS 20.5%, n = 15; TAU 28.8%, n = 21) χ 2(1) = 1.33, P = 0.249; and at 18 months (IPS 23.3%, n = 17; TAU 37.0%, n = 27) χ 2(1) = 3.25, P = 0.071. There were no significant differences between those with and without data at each of these three time points in terms of baseline demographics, vocational and clinical data. Analyses were also conducted to determine whether missing data at a time point depended on vocational status at the previous time point. Those who provided data at 18 months, were significantly more likely to be studying at 12 months (59.4%, n = 57) than those individuals who were missing data at 18 months (28.6%, n = 4, χ 2(1) = 4.69, P = 0.030); however, further breakdown by treatment group was not possible because of low numbers.
IPS fidelity
As a result of resource constraints, it was not possible to engage an independent evaluator to conduct a fidelity review of our IPS intervention. However, we conducted an audit of our intervention via a self-administration of the Supported Employment Fidelity Scale.19 This audit indicated that our intervention was in the range of good fidelity.19
Primary outcome – employment status
At the end of the intervention, the IPS group had a significantly higher rate of having been employed (71.2%, 47/66) than the TAU group (48%, 29/60), odds ratio (OR) = 3.40 (95% CI 1.17-9.91, z = 2.25, P = 0.025). The greatest difference in the predicted probabilities of employment between the IPS and TAU groups was observed over the first 6 months, with minimal differences seen at later 6-month time intervals (Fig. 1). Within the primary random-effects logistic regression model the interaction between group and time period was significant, OR = 0.88 (95% CI 0.78–0.99, Wald z = −2.16, P = 0.031), even after controlling for baseline employment status. The odds ratio comparing employment between the IPS and TAU groups for the 0–6-month period was significant, OR = 3.40 (95% CI 1.17–9.91, z = 2.25, P = 0.025); however, no significant between-group differences in odds of employment were seen at 6–12 and 12–18 months (P = 0.288 and P = 0.594, respectively).
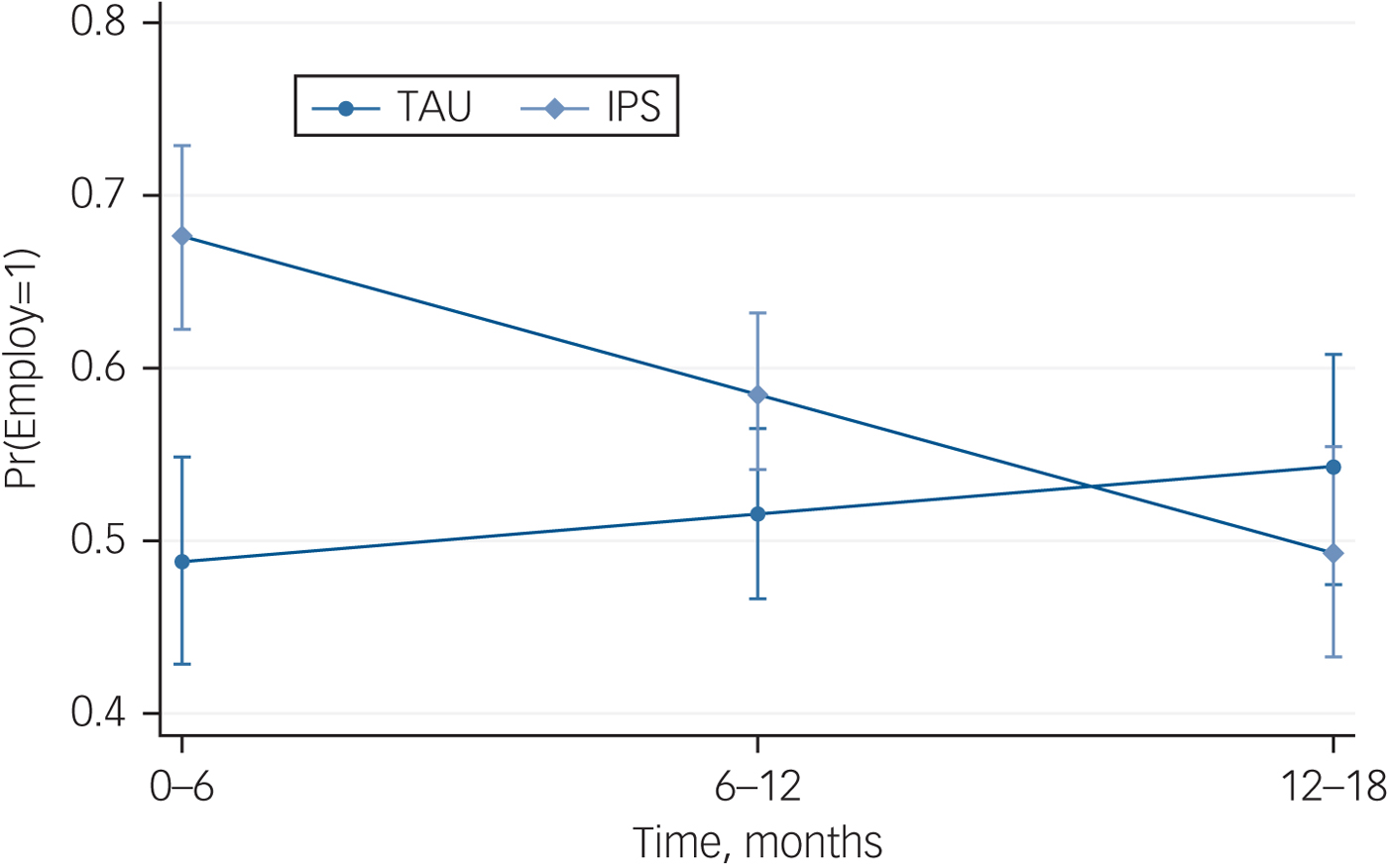
Fig. 1 Predicted probabilities (s.e.) of employment in individual placement and support (IPS) and treatment-as-usual (TAU) groups over 18 months.
The percent change in estimate odds was calculated for the two groups.Reference Rabe-Hesketh and Skrondal20 The conditional odds of employment increased by 2.8% per 6-month time period in the TAU group whereas there was a decrease by 9.5% per 6-month period in the IPS group. An adjusted model was also run controlling for baseline employment status, gender and baseline depressive symptoms. QoL was not included in this model because of the overlap with depressive symptoms. For this adjusted model the interaction between group and time remained significant, OR = 0.88 (95% CI 0.78–0.99, Wald z = −2.26, P = 0.024). The odds ratio comparing groups at 0–6 months also remained significant, OR = 3.57 (95% CI 1.19–10.70, z = 2.28, P = 0.023) whereas group comparisons at 6–12 and 12–18 months were non-significant (P = 0.293 and P = 0.576, respectively).
Secondary outcomes – hours worked, studying and Government pensions
The average hours worked over the three time periods for the two groups is displayed in Supplementary Fig. 2. Note that information regarding hours worked in the 6-month period prior to randomisation was not collected so there were no covariates in this model. The interaction between treatment group and time was not significant, F(2, 148.4) = 0.95, P = 0.390. Furthermore, the main effects for time, F(2, 148.4) = 0.50, P = 0.608 and for group, F(1,112.9) = 0.20, P = 0.652, were not significant.
The predicted probability of the two groups studying over the 18 months are displayed in Supplementary Fig. 3. Notably, the IPS group was more likely to be studying at each of the follow-up 6-month time intervals. There was a significant interaction between group and time with respect to studying status, OR = 0.87 (95% CI 0.77–0.97, Wald z = −2.37, P = 0.018), after controlling for baseline study status. The odds ratio comparing studying status between the IPS and TAU groups at the 0–6-month time interval was significant, OR = 3.04 (95% CI 1.01–9.17, Wald z = 1.97, P = 0.049. No between-group differences were observed at 6–12 and 12–18 months (P = 0.584 and P = 0.300, respectively). The conditional odds of studying increased by 7.6% per 6-month time period in the TAU group whereas there was a decrease by 6.9% per 6-month period in the IPS group. The model was re-run controlling for baseline studying status, gender and baseline depressive symptoms; the interaction remained significant, OR = 0.86 (95% CI 0.77–0.97, z = −2.40, P = 0.016). Controlling for these three variables; however, the point-estimate for difference between the groups in the 0–6 months interval was no longer significant (P = 0.084).
The interaction between group and time period for dependence on pensions was not significant, OR = 0.98 (95% CI 0.84–1.13, z = −0.31, P = 0.757), after controlling for baseline dependence on government pensions. This result remained non-significant after controlling for gender, baseline government pension status and baseline depressive symptoms.
Discussion
Key findings and comparison with findings from other studies
This is the largest trial to our knowledge on the efficacy of IPS in FEP. It is also one of the only trials in FEP to examine the duration of employment past the intervention stage. The key findings were that IPS was superior to TAU in rates of employment over 6 months, but this finding was not sustained after the intervention period at 12- and 18-month follow-up. Duration of employment and educational engagement did not differ between groups at any time point.
In previous trials of IPS in FEP populations, IPS has produced favourable employment outcomes compared with comparison conditions.Reference Bond, Drake and Luciano21 This finding has been replicated here, at least at the end of 6 months of intervention. However, the benefit of IPS in the present study is seen to disappear relative to the control group over the follow-up period. This contrasts with studies of IPS in populations with chronic illness in which the benefit of IPS persists over time.Reference Modini, Tan, Brinchmann, Wang, Killackey and Glozier7, Reference Drake, Bond and Becker22, Reference Hoffmann, Jäckel, Glauser, Mueser and Kupper23 However, the result in the present study seems to be as much about the higher than expected performance of the control group as it is about the failure of the IPS group to maintain its initial significant benefit.
In a previous, albeit smaller (n = 41) RCT of IPS conducted in the same clinic, the control group achieved only a 9.5% employment outcome at the end of the 6-month intervention.Reference Killackey, Jackson and McGorry9 However, in the current study the control group employment rate was 48% at the 6-month time point. In comparison, the IPS group in our initial studyReference Killackey, Jackson and McGorry9 had a 65% employment rate that is similar to the 71% achieved in the present study. This raises the question of what could account for this type of improvement in the control group results.
Possible reasons for our findings concerning the control group
We believe that there are three possible explanations for the improvement in the control group results. The first possible reason is that the external, government-contracted employment agencies that are current best practice have improved their performance in relation to facilitating the employment of young people with psychosis, but this seems unlikely. During the time period of the current study the government department responsible for employment services in Australia conducted a review of performance of the system. That review found that in relation to outcomes for people with psychiatric and psychological disabilities that the highest level of support provided only resulted in 14% of people obtaining employment lasting 13 weeks.5 Although there was at that time also a payment for agencies that assisted people to access 26 weeks of employment, no data was reported for the percentage that made it to 26 weeks. One possible interpretation was that the number who did so was so small as to not be worth reporting. In a system that is performing so poorly at a national level it is possible but less likely that our local employment services were producing results that would be sufficiently better than the rest of the national system to explain our outcomes.
The second possible explanation of the results of the control group is speculation that there was a change in the clinical culture in relation to vocational outcomes in the EPPIC clinic where the study was conducted. As mentioned, EPPIC was also the site at which we conducted a previous RCT of IPS in FEP.Reference Killackey, Jackson and McGorry9 That first RCT was the first time that IPS had been introduced to the EPPIC clinic. Initially, when we introduced IPS there was scepticism from clinicians that young people with IPS would be able to enter or return to employment in significant proportions. However, as they witnessed the success of the young people with psychosis in that trial in returning to and successfully engaging with employment, much of their scepticism translated to enthusiasm for exploring the vocational ambitions of their clients.
Further, there was a 2-year window between the end of the first study and commencement of the second. During this time, demand for IPS services outstripped the resources that were available to supply IPS. In order to assist, a number of workshops were conducted with clinical staff about how to engage in assisting their clients to obtain employment or return to school. As a consequence, the clinical staff were upskilled around employment. Some evidence that may support this supposition comes from a file audit study of a cohort of EPPIC clients conducted before the current trial.Reference Cotton, Lambert, Schimmelmann, Filia, Rayner and Hides24 The file audit showed that at discharge from EPPIC, the majority of clients were unemployed and not studying. Further evidence of the acceptance of the possibility and importance of vocational recovery among the clinical staff and management of EPPIC was that during this time one clinical position was converted to an IPS position. In a cash-strapped public mental health service, this is a strong indication of the perceived value of an intervention. The positive impact of changed staff attitudes on employment outcomes for people with FEP has previously been demonstrated by Craig et al,Reference Craig, Shepherd, Rinaldi, Smith, Carr and Preston25 providing some tentative support for this hypothesis. Nevertheless, this possible explanation is speculative as there was no systematic measurement of clinical staff attitudes and skills in relation to vocational recovery. If there is an acceptance of the possibility that this cultural change explains elements of the results, there are a number of positive conclusions to be drawn.
Too often in the past clinicians and others involved in care have ‘protected’ young people with psychosis from the possible stressors that exist in pursuing vocational recovery.Reference Rinaldi, Killackey, Smith, Shepherd, Singh and Craig3 This is a classic example, although often well motivated, of the ‘soft bigotry of low expectations’. Where it leads to failure to realise educational potential, abandonment of vocational dreams, lifelong unemployment and social exclusion, this form of protection is no protection at all. It is therefore hopeful that the vocational expectations clinicians hold may be adjusted in light of new evidence. In this case, that young people with psychosis can and should obtain and retain employment.
That end-of-intervention outcomes were significantly better for IPS suggests that the expertise of a specialist IPS worker has something to offer over the skill of a mental health clinician. As IPS is still largely a research intervention in many parts of the world, there is not a ready workforce to conduct IPS in mental health services. If it is possible to upskill existing mental health workforces to address this much-desired element of recovery it may be possible to deliver a more stepped vocational recovery model. For those with better employment or educational prospects, the assistance of their mental health clinician who has done further training might be sufficient. For those with poorer vocational prognoses, or who have not achieved the vocational outcomes they sought with their mental health clinician, referral to an IPS specialist would be indicated.
Importantly, irrespective of which level of vocational intensity was accessed, our findings suggest that strategies to promote long-term maintenance of vocational functioning should be implemented. Although IPS was effective while being implemented, in common with many psychosocial interventions, the benefit of IPS in this study was reduced over time. This suggests a need to focus in future on mechanisms to extend this positive benefit, which can be scalable over time and are not excessively resource intensive. Examining the ways in which technology can be of assistance in this area may be worthwhile.Reference Alvarez-Jimenez, Bendall, Lederman, Wadley, Chinnery and Vargas26
A third possible explanation that is not mutually exclusive from the others is a change in government policy in relation to young people, employment, education and welfare that may have had an impact on the results of the control group. Such a change in policy did occur during the course of the study. The effect of this policy change was that to remain eligible for welfare payments, young people who had not completed high school or an equivalent had to be enrolled in an educational course of some kind. Although this may explain why there was no difference in the level of educational outcomes in the study, it does not explain the high rates of employment seen in the control group.
Implications of findings regarding educational outcomes
Given the age range of people typically attending FEP services, a focus on education as part of vocational recovery is important. However, the treatment groups did not differ on educational outcomes at any time point. This is consistent with other IPS study resultsReference Bond, Drake and Campbell13 and indicates that IPS as currently practised may require adaptation for enhanced education outcomes. There is no reference to education in the IPS fidelity scale which in turn comes from IPS being an intervention primarily developed in adults with severe mental illness and with a sole focus on employment. In addition to this it suggests an addition education focused skill-set may be needed for IPS workers to successfully address educational vocational recovery in young people. Recent evidence tentatively suggests that adapting IPS to a specific focus on education, with an IPS worker with expertise in working in the education sector can achieve good educational outcomes.Reference Killackey, Allott, Woodhead, Connor, Dragon and Ring27 However, this is an area in need of more and controlled research.
Strengths and limitations
The strengths of this study include that it was adequately powered to explore the effect of IPS on employment rates of young people with FEP. Further, only four participants did not complete the intervention, and there was low attrition across the 18 months of the study with 87% included in the final analysis. The study also reflected real-world practice in having few exclusion criteria. This is important in considering translation of IPS into routine practice in FEP services.
The study had some limitations that should be considered. It was conducted in Australia and results may be limited in their generalisability by the economic, welfare and labour market context that the study occurred within. The intervention period was only 6 months. This is short by contrast with other international IPS trials. For pragmatic reasons and based on our earlier pilot study,Reference Killackey, Jackson and McGorry9 we provided 6 months of intervention. Many other trials provide 9 or more months. It is possible that initial gains may have been better maintained with a longer intervention or top-up sessions. One way we are currently addressing this in our clinic is employing peer workers to work alongside IPS workers and to provide more support than the IPS worker alone is able to provide.
Resource limitations meant that this study had a single IPS worker rather than a team of IPS workers. This may have limited the capacity for thorough follow-along support that in turn may have had an impact on the duration of employment. Primary outcome measurement is an issue in the IPS literature with no set standard. Some studies use obtainment of employment with no measure of duration, some use a day, a week or a number of hours per week as a threshold. Our study used at least 1 day of work in the previous 6 months. It is possible that using a different definition would have led to different results. However, our definition is consistent with some IPS literature and our own previously published work in this area. Measurement of education is important in this cohort, some of whom are younger than the legal working age. There are currently few good measures of educational outcomes for people with mental illness and this is an area that requires attention. Another limitation is that there was likely to be less post-randomisation data in the TAU group. This is mitigated somewhat by there being no differences between the groups in terms of missingness, and baseline vocational, clinical and demographic data. Finally, although there was an initial benefit of IPS for education at the 6-month time point, this is seen to disappear when baseline variables are considered.
In conclusion, IPS is effective at supporting young people with FEP to return to work. However, this benefit was not maintained compared with usual treatment in a clinic in which clinical staff are optimistic about, and have been upskilled around, the provision of vocational recovery. This suggests that specialist vocational recovery services may be most usefully deployed for people who have failed to make an initial vocational recovery during their usual treatment. Further, this study along with others has not demonstrated that a general approach to vocational recovery using IPS leads to superior educational outcomes. A more specific and targeted approach to education may be needed.
Funding
This work was supported by the following grants: Australian Research Council LP0883237; Australian Rotary Health Mental Health Grant, and; National Health and Medical Research Council CCRE 264611. The following fellowships were held by authors related to this project: E.K – Ronald Philip Griffith Fellowship Faculty of Medicine Dentistry and Health Sciences, The University of Melbourne; NHMRC CDF II Fellowship APP1051891; BB & A Miller Foundation Fellowship; K.A. – Ronald Philip Griffiths Fellowship Faculty of Medicine Dentistry and Health Sciences, The University of Melbourne; S.M.C. – Ronald Philip Griffith Fellowship Faculty of Medicine Dentistry and Health Sciences, The University of Melbourne; NHMRC CDF Level II Fellowship APP1061998 and NHMR Senior Research Fellowship APP1136344; M.A.-J. – CR Roper Fellowship Faculty of Medicine Dentistry and Health Sciences, The University of Melbourne; NHMRC Career Development Fellowship APP1082934; and F.K.-L. – NHMRC CDF Level I Fellowship APP1008972 and NHMRC Senior Research Fellowship APP1110371.
Acknowledgements
We wish to express our deep appreciation for all the participants of this trial who contributed their time and lived experience to our research. The authors acknowledge the dedication and hard work of the research assistants who worked on this trial, and the EPPIC Clinical programme for facilitating this research.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2018.191






eLetters
No eLetters have been published for this article.