Stillbirth after 24 weeks' gestation occurs in around 0.5% of births in England and Wales (Office of Population Censuses and Surveys, 1998). Post-traumatic stress disorder (PTSD) has been found after distressing obstetric or gynaecological procedures (Reference MenageMenage, 1993; Reference Ballard, Stanley and BrockingtonBallard et al, 1995) but has not been assessed in women who have had a stillbirth. Epidemiological data show that in the majority of cases the PTSD symptoms resolve after 2 or 3 years (Reference Yehuda and McFarlaneYehuda & McFarlane, 1995). However, because about half of the women who suffer stillbirth become pregnant within 12 months (Reference Hughes, Turton and EvansHughes et al, 1999) and it is possible that pregnancy may serve as a reactivating stressor, women could be vulnerable to experiencing symptoms during a subsequent pregnancy. This will be distressing for the woman herself and also could have implications for the child if symptoms persist after the birth, because maternal psychiatric disorders of all kinds increase the risk of disturbance in child development (Reference RutterRutter, 1989).
METHOD
Study design
This is a cohort study of a group of pregnant women whose previous pregnancy ended in stillbirth. Demographic information was gathered in the third trimester of pregnancy. Depression, anxiety and symptoms of PTSD were assessed in the third trimester and at 1 year post-partum.
Subjects
The subjects were women whose previous pregnancy (or pregnancies) had ended in spontaneous loss after 18 weeks' gestation. The mothers were over 20 years old, had a partner, had no other live children, had a singleton pregnancy and spoke enough English for interview. To minimise the confounding factors, we excluded mothers who were currently in treatment for acute physical or mental illness or if the loss had been a termination for abnormality.
Procedure
The procedure had the approval of the local ethics committee. Women were identified by screening all antenatal case records in three district general hospitals. At the time of recruitment, records were not easy to access efficiently on a computerised database so they were screened manually and a small removable marker was placed on records already reviewed so that they were not examined twice. Screening was repeated every 2 months to ensure that no woman fulfilling the criteria for the study was missed. On each visit the researcher checked with midwives and record office staff for any records kept separately from the main files. Records of potential subjects were re-checked in the third trimester to ensure that the pregnancy had not been lost, and a letter was sent to women inviting them to take part. Informed consent was obtained from all participants and initial interview took place either in the hospital out-patient department or in the participant's home.
Instruments
-
(a) Interviewer-rated demographic questionnaire.
-
(b) Edinburgh Postnatal Depression Scale (EPDS; Reference Cox, Holden and SagovskyCox et al, 1987): 10-item self-report scale developed for postnatal use, now validated for use during pregnancy (Reference Murray and CoxMurray & Cox, 1990).
-
(c) Beck Depression Inventory (BDI; Reference Beck, Ward and MendelsonBeck et al, 1961): 21-item self-report questionnaire used at 1 year post-partum.
-
(d) Spielberger State-Trait Inventory (Reference Spielberger, Gorsuch and LusheneSpielberger et al, 1970): 40-item questionnaire measuring anxiety at time of testing (state) and general tendency to anxiety (trait).
-
(e) The PTSD-I interview (Reference Watson, Juba and ManifoldWatson et al, 1991). This interview shows close correspondence with DSM-III-R (American Psychiatric Association, 1987) standards and provides binary present/absent and continuous severity/frequency outputs on each symptom and the entire syndrome. It has demonstrated substantial reliability and validity, showing very high internal consistency and test-retest reliability. The interview correlates well with the PTSD sub-scale of the Minnesota Multiphasic Personality Inventory (MMPI; Reference Keane, Malloy and FairbankKeane et al, 1984).
Statistical analysis
This study reports on the characteristics of the sample and the relationships between certain characteristics and high scores for PTSD. Exact P values are reported where possible: Mann-Whitney tests against continuous or extended variables and Fisher's tests for dichotomies. All analyses were conducted using SPSS for Windows, version 10.0.3.
RESULTS
Subjects included/lost
Approximately 30 000 case records were examined to identify subjects. Of the 96 women who met the initial criteria, 82 (86%) agreed to participate. According to data from antenatal records, women who refused did not differ in obstetric or sociodemographic factors from those who agreed to take part. Not surprisingly in this sample, 13 (14%) women delivered early, before the time arranged for the first interview, and 69 (72%) women had a third trimester interview. One was subsequently excluded owing to language problems at interview. Data from two further subjects were too incomplete for analysis, leaving baseline PTSD data on 66 women.
At the 1-year follow-up three women had moved abroad and four refused an interview. Because of disability in the child or non-accidental injury, three women could not be included in a separate part of the study that concerned child development; these women were not asked to undergo further interview. Two women failed to complete the follow-up PTSD interview adequately. There was no significant difference on baseline demographic or psychiatric variables between women lost to follow-up and those who remained in the study.
Demographic characteristics of subjects (n=66)
The mean age of the subjects was 29.7 years (range 20-46). Forty-one (62%) were ethnically Caucasian, seven African—Caribbean, twelve Indian or Pakistani, four African and two ‘Other’. Of the 66 subjects, 37 (56%) had achieved at least ‘A’ levels in their education, 13 (20%) subjects were unemployed prior to maternity leave, 11 (17%) had partners who were unemployed, 15 (23%) subjects had an annual income of less than £ 10 000 and 22 (33%) complained of unsatisfactory housing.
Six (9%) subjects reported previous physical illness and six (9%) subjects reported previous mental illness; none had had hospital admission. No subject reported psychiatric treatment after the stillbirth. Six subjects reported that the stillborn infant had a congenital abnormality and the remainder were told that the infant was normal. Ten subjects with previous termination of pregnancy showed no significant differences from other subjects on baseline variables. Of the 66 subjects, 41 (62%) stillborn infants had been born in the second trimester (18-27 weeks) and 25 (38%) in the third trimester (28-42 weeks). Time between stillbirth and expected delivery date (EDD) was 10-186 months (median 19).
Results of PTSD interview analysis
Categorical classification of PTSD in DSM-III-R requires a perceived criterion A stressor and above criterion scores on all three sub-categories: trauma re-experiencing (B); persistent avoidance of stimuli associated with the trauma or numbing of general responsiveness (C); and persistent symptoms of arousal (D). The disturbance must have lasted for at least 1 month at some time period since the stressor (life-time diagnosis) and/or over the previous month (current diagnosis).
Perception of stressor
The DSM-III-R criteria define a stressor as an event that is outside the range of usual human experience that would be markedly distressing to almost anyone. Examples given include serious threats to one's physical integrity and threat or harm to one's child's life. March (Reference March1993) suggests that criteria for PTSD stressors should include the requirement that the person has experienced or witnessed an event involving an encounter with violent death or physical injury and that this induced intense fear, personal helplessness and/or horror.
It is our view that stillbirth qualifies as a criterion A stressor by all these criteria. The PTSD-I interview defines a stressor as “something so uncommon and so horrible that it would be very distressing to almost anyone”. Using this definition, 62 women identified themselves as having experienced a stressor when interviewed in pregnancy; 59 of these declared the stillbirth as their sole or main stressor, whereas only three declared a stressor other than the stillbirth. Only four women did not identify their stillbirth as a traumatic stressor and did not acknowledge having experienced any other stressor either.
For the 54 women with usable data at 1-year follow-up, one of two who previously had not acknowledged any stressor now declared that the stillbirth had been a stressor. Of 50 who at baseline had declared the stillbirth as their sole or main stressor, one now declared another trauma (whose occurrence had preceded the initial interview) and four now did not declare any stressor. Of two who had declared other events as major/sole stressors, one now reported the stillbirth as the prime stressor and the other no longer declared any stressor. The overall decline from 52 to 48 declaring a stressor is not statistically significant (McNemar test, P=0.22).
Post-traumatic stress disorder caseness
Having established that stillbirth is a traumatic stressor, it is important to look at the prevalence of case-level symptoms of PTSD. In the third trimester of the pregnancy following stillbirth, 21% of women reporting a criterion A stressor had a current diagnosis of PTSD. Current and life-time diagnosis rates for the whole group were 20% and 29%, respectively. At 1 year post-partum (birth of healthy baby) the current and life-time prevalence rates were 4% and 6%, respectively. The question then arises concerning predictive and possible protective factors in the development of PTSD.
Relationship with medical history
Examination of medical history — including history of mental illness, whether there had been previous (early) miscarriage or termination of pregnancy and the duration of the lost pregnancy (over or under 28 weeks) — showed no significant associations with PTSD.
Emotional support and contemporary management of the stillbirth
We explored supportive factors and presumed supportive management of the stillbirth itself. Whether a reflection of current state or indicative of a protective factor, the perceived social support (albeit retrospectively recalled) at the time of the stillbirth was statistically significantly associated with current PTSD category. Support was coded as sufficient, insufficient or uncertain. This was analysed as an ordinal variable against category. Perceived insufficient or uncertain support from partner (P=0.02) and from family (P=0.02) were related to PTSD current caseness.
Of the 66 women, 14 had not seen their stillborn infant and 47 had done so; 1/14 (7%) who had not seen the infant and 12/47 (26%) who had seen the infant had symptoms of PTSD at case level. This difference is suggestive of a relationship but not statistically significant (P=0.26). The situation was similar for having held the infant (P=0.19). Keeping some memento (such as a photograph or lock of hair) of the dead infant or having attended a funeral for him/her were not associated with PTSD (P=0.75 and 0.66, respectively).
Effect of time interval between stillbirth and current pregnancy
The overall category of current caseness on the PTSD measure was compared with the time lapse between the stillbirth and the EDD of the current pregnancy. This showed a statistically significant relationship (Fig. 1): 13 women meeting caseness criteria had a mean time gap of 23.6 months and the 49 not meeting the caseness criteria had a mean delay of 33.9 months (Mann—Whitney, P=0.011).
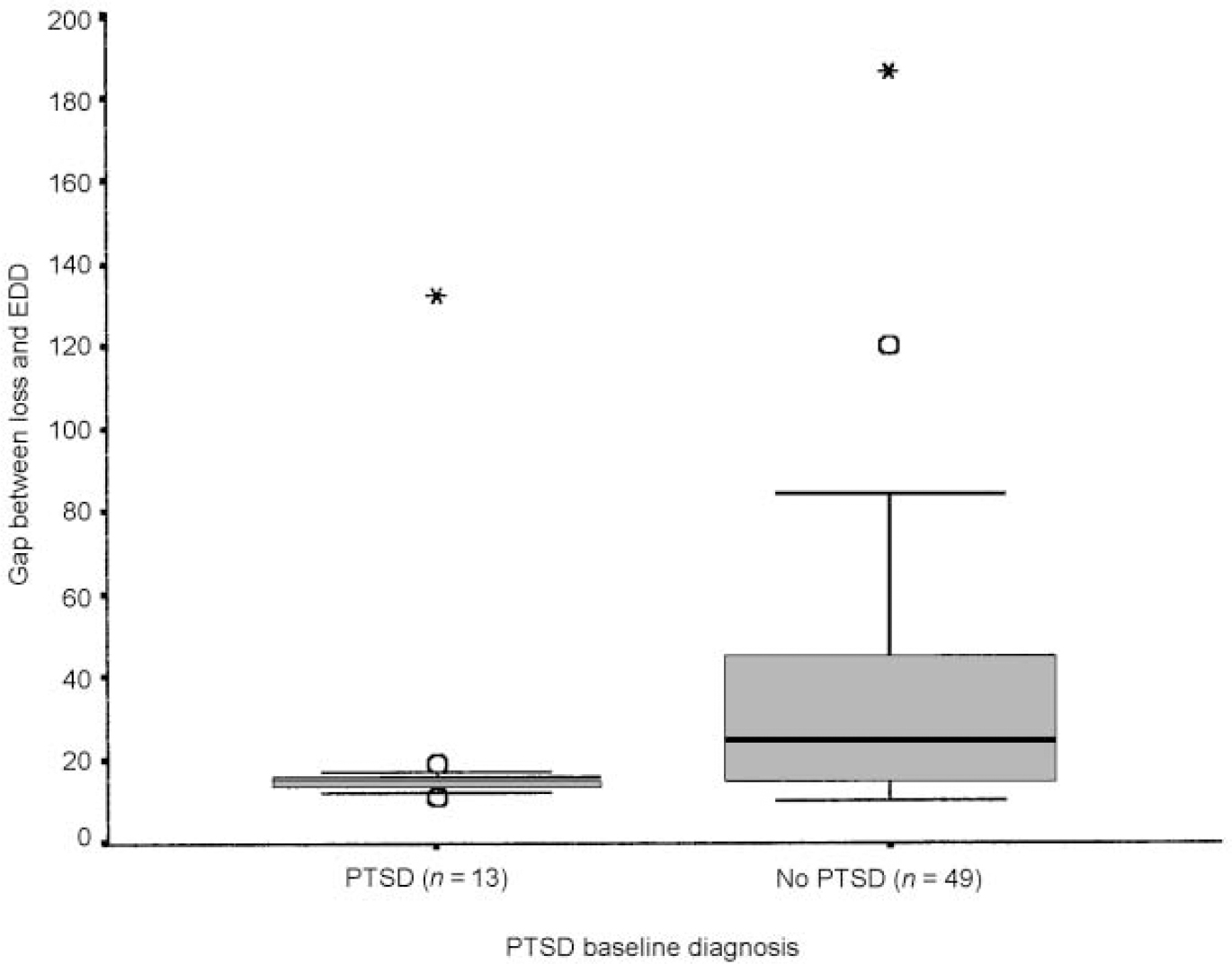
Fig. 1 Effect of time interval between stillbirth and current pregnancy. Boxes represent interquartile (25th-75th centile) ranges, with internal rules indicating group medians. The ‘whiskers’ extend to 2 s.d. either side of the mean (or to the most outlying observation for the minimum in the no-PTSD group, where this is <2 s.d. from the mean). Outliers (2-3 s.d. from the mean) are shown as circles; extremes (>3 s.d. from the mean) as asterisks. EDD, expected delivery date.
Comorbidity with depression and anxiety
In another report from this study, Hughes et al (Reference Hughes, Turton and Evans1999) have reported that women in the pregnancy after stillbirth were significantly more depressed in the third trimester than controls and had greater state-anxiety. Previous studies have shown that although ‘pure’ PTSD is found, strong associations with depression and anxiety are common. There was a strong relationship between the PTSD category and EPDS score and both the state and trait scores from the Spielberger questionnaire (Mann—Whitney, P<0.0005, P=0.001 and P=0.001, respectively). The association between PTSD category and depression category on the EPDS was also considered. As recommended by Murray & Cox (Reference Murray and Cox1990), the 14/15 cut-off on the EPDS was used because of the high levels of dysphoria in pregnancy. Sixty-three women had complete scores on both measures: eight were above the criterion on both; forty-one were below on both, nine were above the criterion on the EPDS but not for PTSD; and five were below the criterion on the EPDS and above for PTSD. The overall κ value was 0.39; P=0.004.
DISCUSSION
Prevalence
Epidemiological studies report widely varying rates of PTSD in the general population. For example, estimates of the prevalence of PTSD among those exposed to a criterion A stressor range from 3% to 58% (Reference Yehuda and McFarlaneYehuda & McFarlane, 1995). Davidson et al's (Reference Davidson, Hughes and Blazer1991) study of a community sample found lifetime and past-6-month prevalence rates of 1.3% and 0.44%, respectively. Resnick et al (Reference Resnick, Kilpatrick and Dansky1993) report the overall prevalence of PTSD in a representative sample of US adult women as 12.3% (life time) and 4.6% (past 6 months). This study has demonstrated that stillbirth is a major stressor associated with PTSD prevalence rates of 29% (life time) and 20% (current) in the subsequent pregnancy.
The wide variation in reported incidence and prevalence rates highlights the methodological difficulty dogging studies of PTSD generally. Part of the difficulty lies in the diverse nature of traumatic stressors and variations in the severity, duration and sequelae of the traumatic event. Other variations in reported prevalence rates following a particular type of stressor may be accounted for by pre-trauma vulnerability factors: genetic and biological risk factors, including family history, mental health and personality; and socio-economic factors, such as history of trauma and rearing environment (Reference ShalevShalev, 1996). Symptoms also may vary with time since the trauma. Post-traumatic stress disorder encompasses different clusters of symptoms and there is some evidence that these may ‘kick in’ at different times, with avoidance phenomena following those of hyperarousal or intrusive symptoms (Reference Karlehage, Malt and HoffKarlehage et al, 1993). Thus, the time interval between stressor and assessment may be another important variable.
It appears from this study that having good emotional support after the stillbirth may be a protective factor. Furthermore, although not reaching significance, the findings suggest that the current practice of encouraging women to see and hold the dead infant may increase the risk of PTSD.
Did the pregnant state activate symptoms?
Boyle et al (Reference Boyle, Vance and Nejman1996) found that the majority of women bereaved by stillbirth, neonatal death or sudden infant death did not develop serious psychological problems, and in those that did the psychological impairment was self-limiting. We also found that most women who had case-level symptoms at baseline experienced remission during the 15 months between the two assessments. Boyle et al additionally reported, however, that women who remained distressed 8 months after the loss were likely still to be distressed at 30 months. All the women in our study were more than 8 months post-bereavement at the time of initial assessment. The elevated incidence of case-level PTSD that we found during pregnancy and the marked improvement at the post-partum assessment would suggest, therefore, that for many women pregnancy was a re-activating but self-limiting stressor. Alternatively, the birth of a healthy baby after the next pregnancy had a ‘curative’ effect.
Relationship with time since loss
The interaction between time since trauma and re-activating stressors is complex. An earlier paper from this study (Reference Hughes, Turton and EvansHughes et al, 1999) has reported that the significantly higher levels of depression and state-anxiety found in women in the pregnancy after stillbirth were accounted for by those women whose loss was less than 12 months before conception. Women more recently bereaved improved post-partum, but had increased depression at 1 year. The statistically significant relationship between time since traumatic loss and PTSD caseness in the third trimester of the next pregnancy adds to this finding. Although it is important to recognise that parents have various and individual reasons for timing the next pregnancy, it appears that there may be an advantage in delaying conception for at least a year, if only to reduce the likelihood of additional distressing symptoms in the next pregnancy.
Comorbidity
Exposure to traumatic events is associated with the development of multiple forms of comorbid psychopathology (Reference TurnbullTurnbull, 1997). Yehuda & McFarlane (Reference Yehuda and McFarlane1995) note the relative rareness of ‘pure PTSD’ as a syndrome uncomplicated by the presence of symptoms of other psychiatric disorders. Our finding that PTSD in the pregnancy following stillbirth was associated with heightened symptoms of depression and state-anxiety is in line with previous research on comorbidity (Reference Sierles and ChenSierles & Chen, 1986).
Therapeutic intervention
This study has shown that women who in stillbirth have suffered the double psychological burdens of trauma and bereavement are vulnerable to case-level symptoms of PTSD in the next pregnancy. Given the potential deleterious effects of maternal mental ill health on the mother's self-care and the infant's emotional and cognitive development (Reference MurrayMurray, 1992), there is a potential case for offering therapeutic intervention in the interests of both mother and infant. Timely intervention also may reduce the likelihood of the re-emergence of symptoms in subsequent pregnancies. Women are likely to be motivated to accept psychological help in pregnancy, partly because they are in contact with clinical services and partly out of concern for their unborn child.
If, however, the pregnant state was a reactivation of a self-limiting stressor, intervention would be better targeted at those women who develop chronic PTSD. This problem requires further research.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Twenty-one per cent of women reporting stillbirth as a criterion A stressor had post-traumatic stress disorder (PTSD) symptoms at caseness levels in the third trimester of the next pregnancy.
-
▪ Significant risk factors are conceiving within I year of loss and a felt lack of social support at the time of the loss. Although not reaching significance, the findings also suggest that seeing and holding the dead infant may increase the risk of PTSD.
-
▪ For nearly all women, PTSD symptoms remit by I year post-partum. However, because a small proportion of women continue to suffer chronic symptoms, the possibility of this diagnosis should be recognised.
LIMITATIONS
-
▪ It would be useful to have data from a group of non-pregnant women who had had a stillbirth, matched (including time since loss) with the pregnant stillbirth group.
-
▪ Further longitudinal research is needed to monitor remission and recurrence of symptoms, particularly in subsequent pregnancies.
-
▪ A larger cohort would permit the evaluation of risk factors not reaching significance in this study.
ACKNOWLEDGEMENTS
Our thanks go to Liz Hopper and Gill McGauley, who contributed to the data collection, to the obstetricians and midwives at St George's, St Helier's and Kingston Hospitals and particularly to the patients who allowed us to interview them.




eLetters
No eLetters have been published for this article.