Conversion disorder refers to the presence of motor and or sensory symptoms for which there are no or inadequate medical explanations.1 Typical symptoms include motor weakness, abnormal movements, non-epileptic seizures, and loss of sight, hearing and touch. The symptoms are not deliberately produced and can be associated with significant distress. Affected children can present with varying degrees of severity. The prognosis of childhood conversion disorder is poorly documented but some children are known to become very impaired, requiring prolonged hospital admission and experiencing long-term physical and psychosocial complications including psychiatric comorbidity, social isolation and educational failure.Reference Kozlowska, Nunn, Rose, Morris, Ouvrier and Varghese2-Reference Pehlivanturk and Unal4 Although cases of childhood conversion disorder have been documented in many countries, for the most part this is based on small samples of children seen in specialist units, and epidemiological data are sparse. The most robust data from a national surveillance study of Australian children under 16 years identified 194 newly diagnosed cases in the care of paediatric clinicians over 2 years, giving a yearly incidence of 2.3-4.2 per 100 000.Reference Kozlowska, Nunn, Rose, Morris, Ouvrier and Varghese2 Most were female (71%), motor symptoms were most common but half presented with multiple symptoms. Experience of separation and family conflict were the most common antecedent stressors. The majority required hospital admission and utilised extensive medical and allied resources. Accurate data on the epidemiology, clinical features, service use and prognosis of conversion disorder are important in planning services and allocating resources for affected children. In this paper we present the first national study on the clinical incidence of non-transient childhood conversion disorder in the UK and Ireland, and report 1-year outcome.
Method
We adopted similar methodology to that used in the Australian clinical surveillance incidence study of conversion disorder.Reference Kozlowska, Nunn, Rose, Morris, Ouvrier and Varghese2 Active prospective surveillance was carried out by monthly mailing of all consultant paediatricians in the UK and Ireland through the British Paediatric Surveillance Unit (BPSU, see www.rcpch.ac.uk/bpsu)Reference Verity and Preece5 from 1 October 2008 to 31 December 2009 (15 months). Given that individuals with this condition may also present to child and adolescent psychiatrists, we used a similar system, the Child and Adolescent Psychiatric Surveillance System (CAPSS, see www.rcpsych.ac.uk/quality/research/capss1.aspx), to cover consultant child and adolescent psychiatrists.Reference Lynn, Viner and Nicholls6 Jointly, the two surveillance systems represent all the consultant paediatricians and child and adolescent psychiatrists officially registered and practising in the UK and Ireland.
Clinicians were asked every month to report any cases of children seen with a new diagnosis of conversion disorder. A notification questionnaire (online supplement DS1) was sent to reporting consultants to ascertain whether the case definition was met and to obtain details of clinical data. Duplicate reports were excluded by matching on partial identification data. A panel of two consultant child and adolescent psychiatrists and a consultant paediatrician reviewed all notification questionnaires to decide by consensus whether the case definition was met. A follow-up outcome questionnaire (online supplement DS2) was sent after 1 year to all clinicians reporting confirmed cases.
The study was approved by the BPSU and CAPSS Executive Committees and by the Charing Cross Research Ethics Committee (Ref: 08/H0711/30). Section 60 exemption approval was given by the Patient Information Advisory Group (Ref: PIAG/BPSU 3-06(FT1)/2008) to allow notification of semi-anonymised data without patient and carer consent.
Case definition
The case definition was based on the DSM-IV criteria for conversion disorder,1 with an additional criterion of 7 days or longer duration to prevent reports of mild, transient cases. These were excluded as we were interested in children with problems clinically significant and burdensome enough to require assessment by consultant paediatricians and child and adolescent psychiatrists. Clinicians were asked to report any child under 16 years newly diagnosed with conversion disorder during the previous month if they had:
(a) one or more symptoms and/or signs affecting motor function (such as weakness, abnormal gait or movements, difficulty with swallowing, or loss of speech) and/or sensory function (such as loss or diminished sensation of touch, sight or hearing) and/or non-epileptic seizures (also known as pseudoseizures); and
(b) the symptoms and/or signs:
(i) could not be adequately explained by a medical condition after full investigation (according to the judgement of the treating clinician), and
(ii) there was no evidence that they have been intentionally produced, and
(iii) they caused significant distress and/or interference in daily activities such as with self-care, school attendance, play or family activities for up to 7 days or longer, and
(iv) were accompanied by psychological factors that were judged to be associated with or have contributed to the presentation.
Cases were excluded if the clinical picture was better explained by another psychiatric disorder such as somatoform disorder, depression, psychosis or tics.
Statistical analysis
Incidence of conversion disorder was calculated by dividing the number of confirmed cases with the base population of children younger than 16 years in the UK and Ireland over the 15-month surveillance period (standardised to 12 months) expressed as per 100 000 population. For the UK, the mid-year population of children younger than 16 years in 2009 was obtained from the National Office for Statistics (www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77-213645). For Ireland, similar data for 2009 were obtained from the Central Statistics Office (www.cso.ie/en/media/csoie/releasespublications/documents/population/current/popmig.pdf).
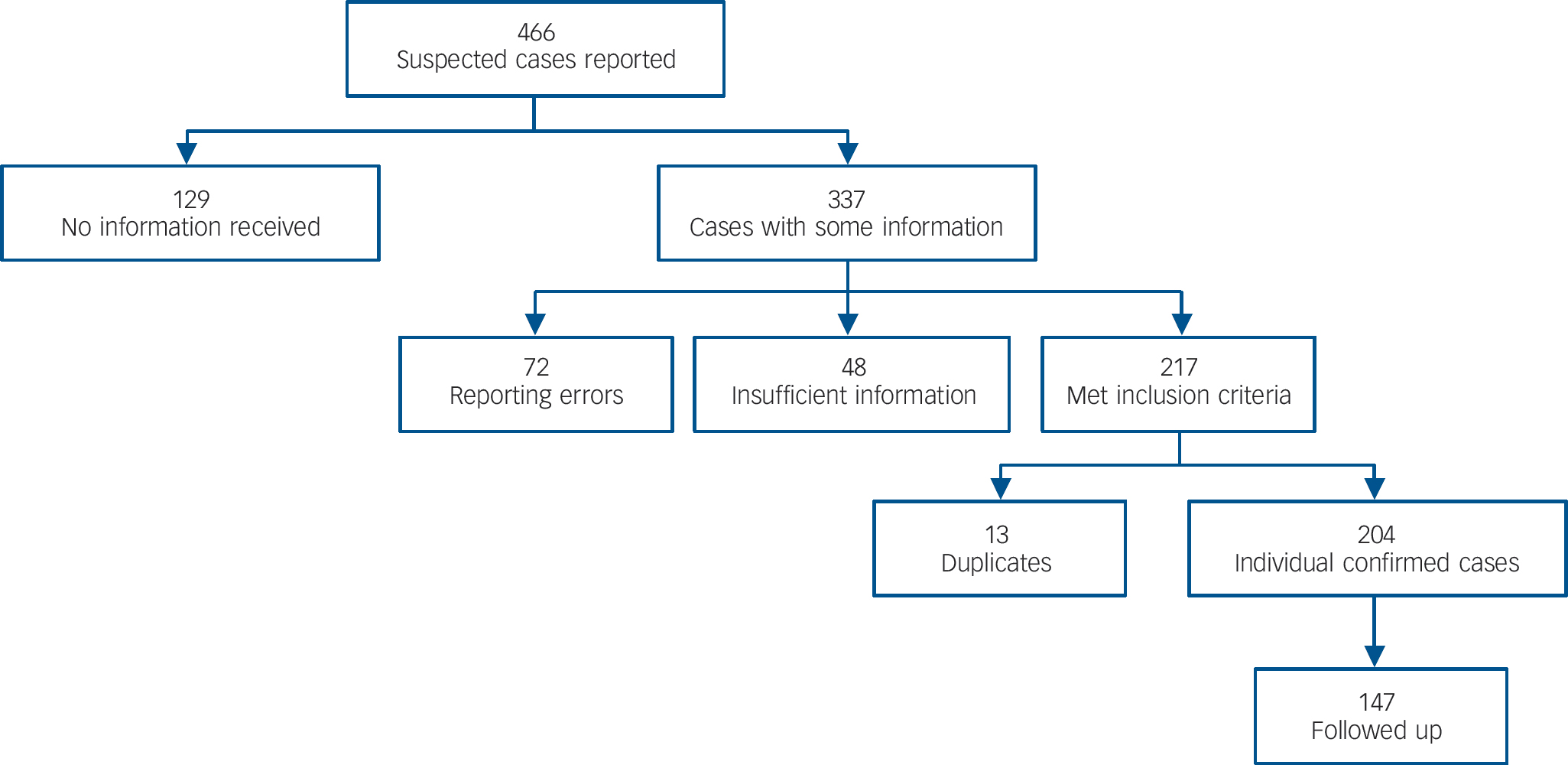
Fig. 1 Case flow.
Descriptive statistics were used for other data. Duplicate reports by different clinicians were treated summatively such that items were scored positive if so marked in either of the duplicate questionnaires. Cases have been subdivided into those in individuals under 10 years and those 10-15 years of age to enable comparison with the Australian data.Reference Kozlowska, Nunn, Rose, Morris, Ouvrier and Varghese2 As there were missing data on clinician reporting of individual clinical features, all proportions have been calculated with the denominator as number of cases with complete data for that variable.
Results
A total of 2874 consultant paediatricians are registered with the BPSU: the response rate to card surveillance was 93%. The number of consultant child and adolescent psychiatrists in the CAPSS database over the course of the study was 728 and the overall response rate to card surveillance 66.2%. Figure 1 shows the flow of reported cases on the surveillance cards. There were 466 suspected cases, 251 reported by paediatricians and 215 by psychiatrists. Scrutiny by the notification review panel of questionnaires - which were returned for 337/466 (72%) - resulted in 204 children deemed to meet the inclusion criteria after removal of duplicates. A total of 147 (72%) 1-year follow-up questionnaires were received.
Incidence
With a total estimated population of 12 542 420 children under 16 years in the UK and Ireland in 2009, the 204 confirmed cases over 15 months' surveillance provide a total 12-month incidence of 1.30/100 000 (95% CI 1.11-1.52). The incidence increased with age, being 0.26/100 000 (95% CI 0.16-0.40) among children younger than 10 years and 3.04/100 000 (CI = 2.56-3.58) for children 10-15 years old.
Demographics
The age range of the 204 confirmed cases was 7-15 years, the median 12.5 years (IQR 11-14). Three-quarters were females (153/204, 75%): the gender distribution was comparable in younger children under 10 years (i.e. 19/25, 76% female) and in the older group (i.e. 134/179, 75% female). In total, 81.2% (164/202) were White British or Irish, whereas 18.8% (38/202) were described as ‘non-White’.
Clinical features
For 166/203 individuals (82%) this was their first episode of conversion disorder. The time from appearance of first typical symptom to diagnosis ranged from less than 1 week in 15/200 children (7.5%) to over 6 months for 26 children (13%). Table 1 shows the main symptoms at first presentation. Motor weakness was the most common conversion symptom followed by abnormal movements and non-epileptic seizures. The majority (141/204; 69.1%) presented with more than one core symptom; 33/204 (16.2%) had four or more symptoms. Pain and fatigue were also commonly reported alongside the core symptoms, and La belle indifference was reported to be present in a quarter of individuals. In 46 children where laterality of symptoms was reported, 22 were right-sided and 24 left-sided.
Table 1 Type of symptoms at presentation
| Symptoms | n/N (%)Footnote a | Median (IQR) |
|---|---|---|
| Core conversion symptoms | ||
| Motor weakness | 114/180 (63.3) | |
| Abnormal movement | 73/169 (43.2) | |
| Non-epileptic seizures | 66/165 (40.0) | |
| Anaesthesia/paraesthesia | 56/173 (32.4) | |
| Diminished consciousness | 47/162 (29.0) | |
| Visual loss | 37/161 (23.0) | |
| Limb paralysis | 34/157 (21.7) | |
| Loss of speech | 30/155 (19.4) | |
| Hearing loss | 12/155 (7.7) | |
| Total number of core symptoms (range 1–9) | 2 (1–3) | |
| Associated non-core symptoms | ||
| Pain | 96/175 (54.9) | |
| Fatigue | 55/162 (34.0) | |
| La belle indifference | 45/166 (27.1) | |
| Total number of symptoms (both core and non-core) (range 1–13) | 3 (2–4.8) |
a. The denominators refer to the number of clinicians answering ‘Yes’ or ‘No’ to the question on whether a child had a particular symptom. Blank or ‘not known’ answers were treated as missing data.
Table 2 Antecedent stressors, psychiatric and medical histories
| n/N (%)Footnote a | |
|---|---|
| Antecedent stressors | |
| Bullying requiring school action | 44/185 (23.8) |
| Parental separation | 35/184 (19.0) |
| Death of a relative or friend | 31/186 (16.7) |
| Hospital admission of a parent or sibling | 22/182 (12.1) |
| School examination | 21/180 (11.7) |
| Break up with a best friend | 16/181 (8.8) |
| Abuse requiring social services referral | 12/181 (6.6) |
| Psychiatric disorder coexisting with conversion disorder | |
| Anxiety disorder | 36/198 (18.2) |
| School phobia | 16/191 (8.4) |
| Depressive disorder | 17/193 (8.8) |
| Conduct disorder | 5/189 (2.6) |
| Post-traumatic stress disorder | 5/188 (2.7) |
| Autism spectrum disorder | 3/188 (1.6) |
| Attention-deficit hyperactivity disorder | 1/188 (0.5) |
| The six most commonly reported medical problems/symptoms in the year leading up to diagnosis of conversion disorderFootnote b | |
| Non-epileptic neurological conditions (e.g. cerebral palsy, hydrocephalus) | 11 (10.5) |
| Abdominal pain | 10 (9.5) |
| Epilepsy/seizures | 9 (8.6) |
| Cardiac symptom | 5 (4.8) |
| Headache | 5 (4.8) |
| Chest pain | 4 (3.8) |
a. The denominators refer to the number of clinicians answering ‘Yes’ or ‘No’ to the question on whether the particular item applied to the child. Blank or ‘not known’ answers were treated as missing data.
b. N = 105 but only 44 individuals had symptoms that could be grouped.
There were no significant differences in frequency of conversion disorder symptoms between the two age groups (under 10 years and 10-15 years). Females were more likely to present with loss of consciousness compared with males (41/122 (34%) v. 6/37 (16%)) (χ2 = 4.1, d.f. = 1, P = 0.042). No other symptom showed a gender difference.
Antecedent stressors
Antecedent stressors were sought with the question: ‘Has the child experienced any of the following life stresses [seven stresses were listed] within a year to the onset of this episode of conversion disorder?’ Results are detailed in Table 2. Any type of antecedent stressor was reported in 161/199 (80.9%) of cases. Out of the possible stressors listed, experience of bullying or victimisation was most common, reported for a quarter. Other comparatively common antecedents were parental separation and death of a relative or friend. There were no differences in frequency of stressors between younger (less than 10 years) and older children (10-15 years) or across gender. Table 2 also gives details of comorbid past and concurrent psychiatric and medical problems.
Personal psychiatric and medical history
A total of 78% (160/204) of individuals with data on psychiatric history had had no mental disorder prior to the episode of conversion disorder. Of those with a premorbid psychiatric diagnosis, anxiety disorder was reported in 21/200 (11%) and depressive disorder in 10/194 (5%). Similarly, more children presented with concurrent anxiety disorders than depressive disorder (Table 2).
About half (93/192, 48%) of the individuals with data on medical history had required paediatric in-patient and/or out-patient consultation in the 1 year to onset of conversion disorder symptoms. These were reported as still active at the time of diagnosis of conversion disorder in 46/91 (50.5%). In total, 105 of the 192 individuals with data on medical history had a specific condition or symptom reported. A wide variety of problems were reported and the most common are detailed in Table 2.
Family history of psychiatric and medical conditions
In total, 26% (52/201) of individuals with data on family history of mental illness had a family member diagnosed with a psychiatric disorder in the 1 year preceding onset of conversion disorder. The most common conditions were depressive (30/191, 16%) and anxiety disorders (17/189, 9%); a family history of conversion disorder was reported in 6/186 (3%). For 45/195 (23%) there was a family member diagnosed with a medical condition in the 1 year to the onset of the child's conversion disorder. The most common diagnoses were neurological conditions (excluding epilepsy), which were reported in 14/184 (7.6%), epilepsy noted in 6/180 (3.3%) and cancer reported in 6/181 (3.3%). Non-epileptic seizures were not significantly more common in children with a family history of seizures (3/5, 60% v. 43/99, 43%, Fishers Exact Test, P = 0.65).
Medical investigations and management
The case management was resource intensive. In total 161/204 (79%) individuals with complete data about admission required in-patient admission. For the 125 children who had been discharged at the time of reporting, the median duration of admission was 7 days (range 1-217, IQR 3-14). However, for the 12 individuals who were still in-patients at the time of reporting, the median duration of admission to date was 50 days (range 5-140, IQR 28-111). There was no significant difference between younger (less than 10 years) and older children (10-15 years) in their likelihood of being admitted.
The children had extensive medical investigations (Table 3), most commonly magnetic resonance imaging, electroencephalograms and computed tomography scans. The median number of investigations was 2 (range 0-17, IQR 1-3). They were supported by a wide range of professionals (Table 3). The median number of professionals involved was 4 (range 1-10, IQR 3-5). Psychotropic medications, mainly antidepressants, were prescribed for 27/204 (13.2%) in the course of the study.
Table 3 Medical investigations and professionals involved in the management of conversion disorder
| n/N (%)Footnote a | |
|---|---|
| Investigations | |
| Magnetic resonance imaging | 125/188 (66.5) |
| Electroencephalogram | 95/186 (51.1) |
| Computed tomography scan | 47/171 (27.5) |
| X-ray | 40/171 (23.4) |
| Nerve conduction | 14/166 (8.4) |
| Electromyography | 12/165 (7.3) |
| Video telemetry | 11/164 (6.7) |
| Professionals | |
| Medical practitioners | |
| General paediatrician | 175/192 (91.1) |
| Child and adolescent psychiatrist | 129/187 (69.0) |
| Paediatric neurologist | 104/170 (61.2) |
| Other professionals | |
| Education staff (e.g. teachers) | 110/165 (66.7) |
| Clinical psychologist | 79/164 (48.2) |
| Physiotherapist | 83/161 (51.6) |
| Occupational therapist | 32/149 (21.5) |
| Social worker | 29/147 (19.7) |
| Educational psychologist | 11/140 (7.9) |
a. The denominators refer to the number of clinicians answering ‘Yes’ or ‘No’ to the question on whether the particular item applied to the child. Blank or ‘not known’ answers were treated as missing data.
Table 4 Outcome of conversion disorder symptoms at 12-month follow-up
| n | Outcome, n (%) | ||||
|---|---|---|---|---|---|
| Symptom | Reported originally | Known outcomeFootnote a | Improved | Not improved | Worse |
| Core conversion symptoms | |||||
| Non-epileptic seizures | 66 | 38 | 35 (92.1) | 2 (5.3) | 1 (2.6) |
| Motor weakness | 114 | 63 | 58 (92.1) | 4 (6.3) | 1 (1.6) |
| Paralysis | 34 | 29 | 29 (100) | 0 (0) | 0 (0) |
| Abnormal movement | 73 | 31 | 28 (90.3) | 2 (6.5) | 1 (3.2) |
| Hearing loss | 12 | 9 | 7 (77.8) | 1 (11.1) | 1 (11.1) |
| Visual loss | 37 | 20 | 16 (80.0) | 3 (15.0) | 1 (5.0) |
| Loss of speech | 30 | 12 | 9 (75.0) | 2 (16.7) | 1 (8.3) |
| Diminished consciousness | 47 | 18 | 17 (94.4) | 1 (5.6) | 0 (0) |
| Anaesthesia/paraesthesia | 56 | 20 | 18 (90.0) | 2 (10.0) | 0 (0) |
| Associated non-core symptoms | |||||
| Pain | 96 | 42 | 37 (88.1) | 5 (11.9) | 0 (0) |
| Fatigue | 55 | 27 | 22 (81.5) | 4 (14.8) | 1 (3.7) |
| La belle indifference | 45 | 30 | 21 (70.0) | 9 (30.4) | 0 (0) |
a. Denominator = n (number of cases with known outcome).
1-year outcome
Follow-up data were available for 147/204 confirmed cases (72.1%), more so for boys than girls (43/51 (84%) v. 104/153 (68%), χ2 = 5.1, d.f. = 1, P = 0.017). Individuals for whom there were follow-up data did not differ significantly from those without follow-up data on age, core symptoms, duration of admission or median number of investigations. The median duration of out-patient treatment was 24 days (range 0-156, IQR 8-52). Table 4 shows that most symptoms were reported as improved.
A total of 32/115 (28%) individuals with completed data were diagnosed with a new psychiatric disorder during the follow-up period. The three most common diagnoses were anxiety disorder (15/105, 14%), depressive disorder (14/105, 13%) and school phobia (9/101, 9%).
Clinicians offered the children's families a non-medical explanation for the conversion disorder symptoms in the vast majority of cases (116/124, 94%). For the children with complete data for this analysis most families accepted the non-medical explanation either fully 69/120 (58%) or partially 39 (33%): thus over 90% of families had some level of acceptance for a non-organic explanation.
The psychological interventions offered and accepted by families were: psychoeducation (49/89, 55%), supportive counselling (41/80, 51%), anxiety management such as relaxation training (34/69, 49%), family therapy (26/68, 38%) and cognitive-behavioural therapy (15/53, 28%).
Discussion
This is the first study to prospectively investigate the incidence of conversion disorder in children in a European population. With 204 cases, this is the largest cohort of incident cases of non-transient childhood conversion disorder reported in the medical literature. The incidence was low but increased with age. The cases were often complex as comorbid medical symptoms and psychiatric disorders were commonly reported. Most conversion symptoms improved over the 12 months of follow-up but there was high use of health and other professional services.
Incidence
The total yearly incidence of 1.30/100 000 (95% CI 1.11-1.52) is about half that reported from Australia (2.3-4.2/100 000) in a study that used a similar methodology.Reference Kozlowska, Nunn, Rose, Morris, Ouvrier and Varghese2 This may be explained by our study using a case definition that excluded transient (under 7 days) symptom duration unlike the previous study that did not specify duration. Another possible explanation is underreporting of cases: whereas the BPSU reporting system is well established with return rates of 93%, the CAPSS system is still in an early phase of development and the card return rate during the study was 66%. This compares with an overall 96% return rate in the Australian study. Data for 129 reports were not returned in our study. Given that the rate of verified case reports was 61% (204/337), this extrapolates to a potential 79 additional cases, which would raise the incidence to 1.8/100 000.
Our study indicates that conversion disorder is less common in children than in adults where incidence rates of 5-12 per 100 000 have been reported.Reference Akagi and House7 The higher incidence in adults could be related to the role of trauma in the pathogenesis of conversation disorder,Reference Roelofs, Keijsers, Hoogduin, Naring and Moene8 such that the cumulative effect of trauma in the journey from childhood to adulthood would increase the risk. It might also be related to developmental immaturity, since we, as in previous studies,Reference Kozlowska, Nunn, Rose, Morris, Ouvrier and Varghese2 found the incidence to be lower in the younger children.
Demographics
The median age of the children in our study (12.5 years) is similar to the Australian survey's (11.8 years).Reference Kozlowska, Nunn, Rose, Morris, Ouvrier and Varghese2 Both studies showed a preponderance of females (over 70%), and in ours this was as marked in the younger as in the older age group. This may be linked to the high representation of non-epileptic seizures in our study, a symptom where female gender is especially overrepresented.Reference Bass, Gelder, Andreasen, Lopez-Ibor and Geddes9
Consistent with other studies,Reference Kozlowska, Nunn, Rose, Morris, Ouvrier and Varghese2,Reference Grattan-Smith, Fairley and Procopis3,Reference Kotagal, Costa, Wyllie and Wolgamuth10 we found the incidence of conversion disorder to increase with age: in fact no children reported were below the age of 7. This has been attributed to immaturity in young children in the development of the social skills and ability to see themselves from another person's perspective,Reference Hetherington and Parke11 which is necessary for the display of the range of interpersonal behaviours that are an integral part of somatising syndromes in children.Reference Taylor12,Reference Garralda13
Clinical presentation
Children presented with a wide range of clinical features: as in previous reports,Reference Kozlowska, Nunn, Rose, Morris, Ouvrier and Varghese2,Reference Pehlivanturk and Unal4 motor symptoms and non-epileptic seizures were most commonly reported and multisymptomatic presentations common. Antecedent stressful events were reported for 80.8% of individuals. This again is comparable to the results of the Australian surveillance study and confirms the perceived significance of stress.
The main stresses in our sample were related to bullying requiring school action, although examinations and break up with friends were also mentioned, as were parental separation, illness and losses. The findings are generally in line with previous reports.Reference Kozlowska, Nunn, Rose, Morris, Ouvrier and Varghese2,Reference Pehlivanturk and Unal4 Taken together these findings highlight the importance of stressors involving school and relationships, rather than major breakdowns in family relationships and boundaries such as in child abuse as reported in the adult literature.Reference Roelofs, Keijsers, Hoogduin, Naring and Moene8,Reference Sar, Akyüz, Kundakçi, Kiziltan and Dogan14 This may be accounted for by retrospective overreporting of child abuse by adult patients or underreporting in childhood studies like ours. The exact nature and causal importance of the reported antecedent stressors is not determinable by our study.
Past or current psychiatric comorbidity (usually anxiety and depressive disorders) was reported for about a quarter of individuals, in line with previous reports from both clinical surveillance and psychiatric clinical samples.Reference Pehlivanturk and Unal4 Management frequently involved paediatric in-patient admission, performance of special investigations and contact with a large number of health and educational professionals, and we identified a small number of children with prolonged hospital admissions as part of the assessment procedure. This reflects the diagnostic difficulties and concerns about the possibility of organic illness before a final diagnosis is reached, and illustrates the cost of these problems and the requirement for paediatric and psychiatric expertise.
1-year outcome
The follow-up findings confirm previous reports of improvement over time for many children.Reference Pehlivanturk and Unal4 Nevertheless, some symptoms persisted, and a quarter of the children developed a new psychiatric disorder during follow-up, especially anxiety and depressive disorders, possibly representing progress away from somatic to emotional expression of distress in some children.
The rate of improvement in core conversion disorder symptoms in our study (75-100%) is higher than that reported for adult patients. For example, Crimlisk and colleaguesReference Crimlisk, Bhatia, Cope, David, Marsden and Ron15 reported resolution or improvement in 58% of individuals in a 6-year follow-up of adult patients from a national centre. Adult patients in that study would have had more severe index episodes; hence their referral to a specialist neurology hospital. However, our follow-up period was shorter and it is possible that individuals with no follow-up data showed less improvement, leading to overestimation of overall positive outcomes.
The follow-up data indicate that most families displayed some degree of acceptance of the non-medical explanation for the symptoms, and about a half received psychological treatments, confirming the feasibility of helping many families move from a medical to a mental health perspective and of putting into place psychosocial interventions.Reference Leslie16 Nevertheless, a small percentage failed to accept a non-medical framework for understanding the problems, and therefore are likely to remain a challenge for clinicians.
As a result of the relatively short duration of follow-up, we do not know whether the reported improvements were maintained or whether a proportion of the children subsequently developed other psychosocial difficulties. Data from follow-up of adult patients attending specialist centres suggest increased levels of psychiatric diagnoses long term.Reference Crimlisk, Bhatia, Cope, David, Marsden and Ron15
Strengths and limitations
The main strengths are the high ascertainment of cases from a complete national population. This was made possible by the dual surveillance strategy that enabled reports by paediatricians and child and adolescent psychiatrists.
The first limitation is that surveillance methodology only identifies individuals whose cases are severe enough to present to secondary care and to the attention of consultant paediatricians and child and adolescent psychiatrists. This is underscored by our focus on non-transient cases. Moreover, we might have missed children seen by adult neurology, ophthalmology or psychiatric services who side-stepped paediatric services, although this seems unlikely given service organisation in the UK and Ireland. Second, we were unable to confirm the eligibility of a quarter of reported cases due to clinicians not returning the initial questionnaires despite several reminders, and the lower card-return rate for CAPSS was also a limitation, suggesting that our incidence may be an underestimate. Third, and as already stated, follow-up data on individual symptom change were only available for a proportion of cases and this finding should therefore be regarded with caution. Finally, although most families for which this information was available showed some level of acceptance of a non-medical explanation, we had no data on the children's own understanding or acceptance of this formulation
Clinical implications
Although uncommon, conversion disorder presents a diagnostic challenge to clinicians and consumes considerable diagnostic and clinical resources. Rare conditions such as non-transient conversion disorder lack coherent national plans for assessment and treatment. Its rarity, complexity and the commonly reported associated psychiatric and psychosocial factors point to the importance of the availability of specialist services with expertise in both biological and psychiatric aspects. These services may be in the best position to provide the breadth of experience and expertise necessary to confidently manage the disorder or to advise other clinicians.
Uncommon disorders often lack the robust evidence base to guide treatment as the numbers required for randomised trials are often too difficult to obtain. This study provides epidemiological evidence about incidence, duration and severity in order to inform the development of possible future intervention studies.
Funding
The project was funded by the BUPA Foundation.
Acknowledgements
We would like to thank Vasanthi James for running the administration of the study, and Nicole Hickey for additional administrative support. We thank the executive committees of BPSU and CAPSS for facilitating the study. We thank the thousands of consultant paediatricians and child and adolescent psychiatrists who returned the study notification cards. Finally, we thank BUPA foundation for funding the project. We acknowledge the BPSU, supported by the Department of Health, for facilitating the data collection and the reporting clinicians, particularly those who completed the questionnaires.








eLetters
No eLetters have been published for this article.