General practitioners (GPs) have an important role in the treatment of patients with an established diagnosis of schizophrenia (Reference Lang, Johnstone and MurrayLang et al, 1997) as well as in the identification of people in the early stages of psychosis (Reference Skeate, Jackson and BirchwoodSkeate et al, 2002). In this study, by the Swiss Early Psychosis Project (http://www.swepp.ch) among GPs in Switzerland, we investigated the following issues pertaining to patients with suspected or established schizophrenia: patient load, treatment setting, attitudes and needs, diagnostic knowledge and current treatment practice of GPs. Clear knowledge regarding these issues may advance the education of primary care professionals and thus improve the primary care of patients with chronic schizophrenia and those with early psychosis.
METHOD
Sample
The addresses of 6046 GPs who were actively practising in Switzerland as of January 2001 were obtained from the Swiss Medical Association (FMH). From these, we randomly selected 1002 French-speaking and 2995 German-speaking GPs, thus maintaining the primary language distribution among all GPs. Of these 3997 GPs, 19 were identified as clinicians with no primary care function. Thus, questionnaires were sent to 3978 GPs in a first wave in April 2001. The same questionnaire was sent 8 months later to the same GPs. Owing to retirement and the refusal to participate of some GPs, the second sample consisted of 3830 GPs. No instruction as to how GPs should fill in the questionnaire (recollection, audit figures) was given in the accompanying letter.
Questionnaire
The 23-item questionnaire (see Appendix) consisted of 4 demographic items, and 19 (partly multi-item) questions which assessed:
-
(a) patient load with individuals suffering from schizophrenia or suspected to be in the early phases of schizophrenia (2 items);
-
(b) treatment setting (4 items);
-
(c) GPs’ needs and attitudes towards current mental healthcare when treating patients with chronic schizophrenia and with suspected early psychosis (3 items);
-
(d) diagnostic knowledge (3 items);
-
(e) therapeutic knowledge and current treatment practice in early, first-episode and chronic schizophrenia (6 items);
-
(f) recent education in the field of early psychosis (1 item).
The questionnaires were anonymous. In order to match the forms of GPs who responded to both surveys, a coding system was used which conformed to the criteria of anonymity and was given oral approval by the Eidgenössisches Büro für Datenschutz, the Federal Office of Data Protection. Respondents had to provide the day and the year of birth of their mother, the day of birth of their father, as well as their own gender. Thus, the chance of a false positive match was theoretically 1 in 190 278.
Analysis
Data were analysed using the Statistical Package for the Social Sciences, version 11 for Windows. To discriminate between different levels of knowledge, we calculated a score from the two multi-item questions covering diagnostic knowledge and steps taken to corroborate a diagnosis (questions 8 and 10). The list of items in each of these questions was divided into three different score levels, ranging from 2 (highest score) to 0. In question 8, social withdrawal and functional decline scored 2, hallucinations/delusions, suicidality, depression/anxiety and bizarre behaviour scored 1 and the remaining items scored 0. In question 10, family history, information from significant others and observation over several months scored 2; personal history and neuropsychological assessment scored 1 and the remaining items scored 0. The sum of all score-2 items from these two questions constituted the core score, and the sum of all score-1 and score-2 items the total score. We based the scoring of the items on results of previous research on predictors of early schizophrenia and on considerations of what can practically be expected from GPs in detecting these predictors (see Discussion).
The core score allowed us to constitute subgroups of knowledge, ranging from a score of 0 (no score-2 item identified) to 10 (all five score-2 items identified). We analysed the frequencies of core score sub-groups as well as the frequencies with which the separate score-2 items had been identified across the core score subgroups using χ2 tests. To assess within-group profiles, we performed a χ2 test against the mean frequency with which the five items had been identified. To evaluate differences in the response profile between the different knowledge groups, we normalised the distributions using the item ‘social withdrawal’ as scaling factor. In addition, we analysed the frequencies with which score-1 items had been indicated across the core score subgroups.
Continuous variables were compared with t-tests or analyses of variance (ANOVA), categorical variables with χ2 tests. An alpha level of 0.05 was considered significant.
RESULTS
Sample characteristics
With 672 (17%) GPs responding in the first survey and 417 (11%) in the second, a total of 1089 (28%) GPs responded once, which corresponds to 18% of all GPs in Switzerland; 185 GPs responded to both surveys. Characteristics of the study sample are summarised in Table 1.
Table 1 Characteristics of GPs surveyed (n=1089)
| Gender, n (%) | |
| Male | 921 (84.6) |
| Female | 168 (15.4) |
| Region of practice, n (%) | |
| Urban | 535 (49.1) |
| Rural | 542 (49.8) |
| Postgraduate education in psychiatry, n (%) | |
| Yes | 350 (32.1) |
| No | 721 (66.2) |
| Recent education in early psychosis, n (%) | |
| Yes | 186 (17.1) |
| No | 858 (78.8) |
| Treatment system, n (%) | |
| Only in GP's practice | 42 (3.9) |
| Collaboration with specialists | 841 (77.2) |
| All patients referred to specialists | 75 (6.9) |
| Time spent with patient per consultation, n (%) | |
| <10 min | 19 (2.0) |
| 10–20 min | 403 (43.2) |
| 20–30 min | 379 (40.6) |
| >30 min | 132 (14.1) |
| Time since medical school, years: mean (s.d.) | 22.6 (8.04) |
| Patient load, n: mean (s.d.) | |
| Established schizophrenia cases in treatment | 3.2 (2.7) |
| Suspected early psychosis | 1.6 (1.2) |
The mean number of patients with established schizophrenia treated by GPs was 3.2 (s.d.=2.7); the mean number of patients whom GPs see annually and suspect to be in the early phases of schizophrenia was 1.6 (s.d.=1.2) (Table 1). Respondents who did not correctly identify any of the score-2 items indicated much more often that they never see patients in whom they suspect early schizophrenia, compared with their colleagues with core scores of 2 and higher (Mann-Whitney U-test, P<0.001).
Attitudes and needs
The majority of GPs (720; 66%) expressed satisfaction with collaboration with specialists, whereas 249 (23%) did not. As Table 1 shows, the vast majority of GPs stay in collaboration with specialists (question 4: χ2=1280.00, d.f.=1, P<0.001). General practitioners with a core score of 0 preferred to refer patients to specialists compared with those with a core score of 2 or more (χ2=37.72, d.f.=2, P<0.001). A fifth of GPs (230; 21%) reported no problems when treating patients with established schizophrenia; 608 (56%) judged the patients’ behaviour to be problematic but continued care in their practice, and 144 (13%) preferred to refer patients because of their problematic behaviour. In addition, the more GPs considered the patient's behaviour to be problematic, the more often they referred them to specialists and did not seek collaboration (χ2=114.715, d.f.=10, P<0.001).
With regard to assessment of needs (question 18), a majority (732; 67%) expressed a wish for specialised low-threshold referral services, whereas only 399 GPs (37%) preferred more education in the field of early psychosis, and 173 (16%) would like a specialised mobile outreach team. These findings were independent of the practice setting (urban v. rural: χ2=3.63, d.f.=2, P<0.16), years since graduating from medical school (χ2=3.83, d.f.=6, P<0.7) and total core score level (χ2=7.42, d.f.=10, P<0.6).
Diagnostic knowledge
Ninety per cent of the responding GPs indicated that a first episode of schizophrenia was preceded by early warning signs. Frequencies of identified score-2 items (questions 8 and 10) are summarised in Table 2, and distributions of the core and total scores are shown in Figs 1 and 2. When examining the frequencies with which score-2 items had been identified across the core score subgroups, two items were significantly under-identified by GPs: these were ‘functional decline’ and ‘observation over several months’. Chi-squared tests of profiles against an even distribution were as follows: group with core score of 2, χ2=46.89; group with core score of 4, χ2=119.38; group with core score of 6, χ2=130.42; group with core score of 8, χ2=75.74; d.f.=4 for all groups; P<0.001 for all groups (Fig. 3). After normalisation of the group profiles, no between-group difference could be detected (χ2=18.17, d.f.=12, P>0.1). When examining the frequencies with which score-1 items had been indicated across the core score subgroups, two clinical features, ‘hallucinations/delusions’ (mean frequency 62%) and ‘bizarre behaviour’ (mean frequency 56%) were predominantly identified. The composite mean frequency of these two score-1 items (59%) was almost twice as high as the composite mean frequency (33%) of the two most regularly under-identified score-2 items, ‘functional decline’ and ‘observation over several months’.
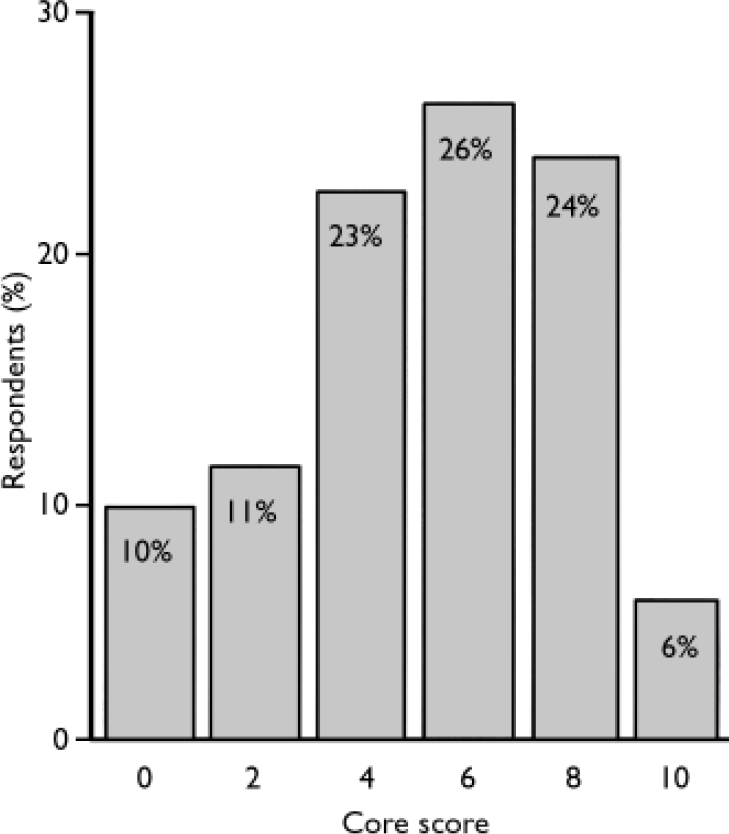
Fig. 1 Distribution of core scores (mean 5.2, s.d.=2.7).
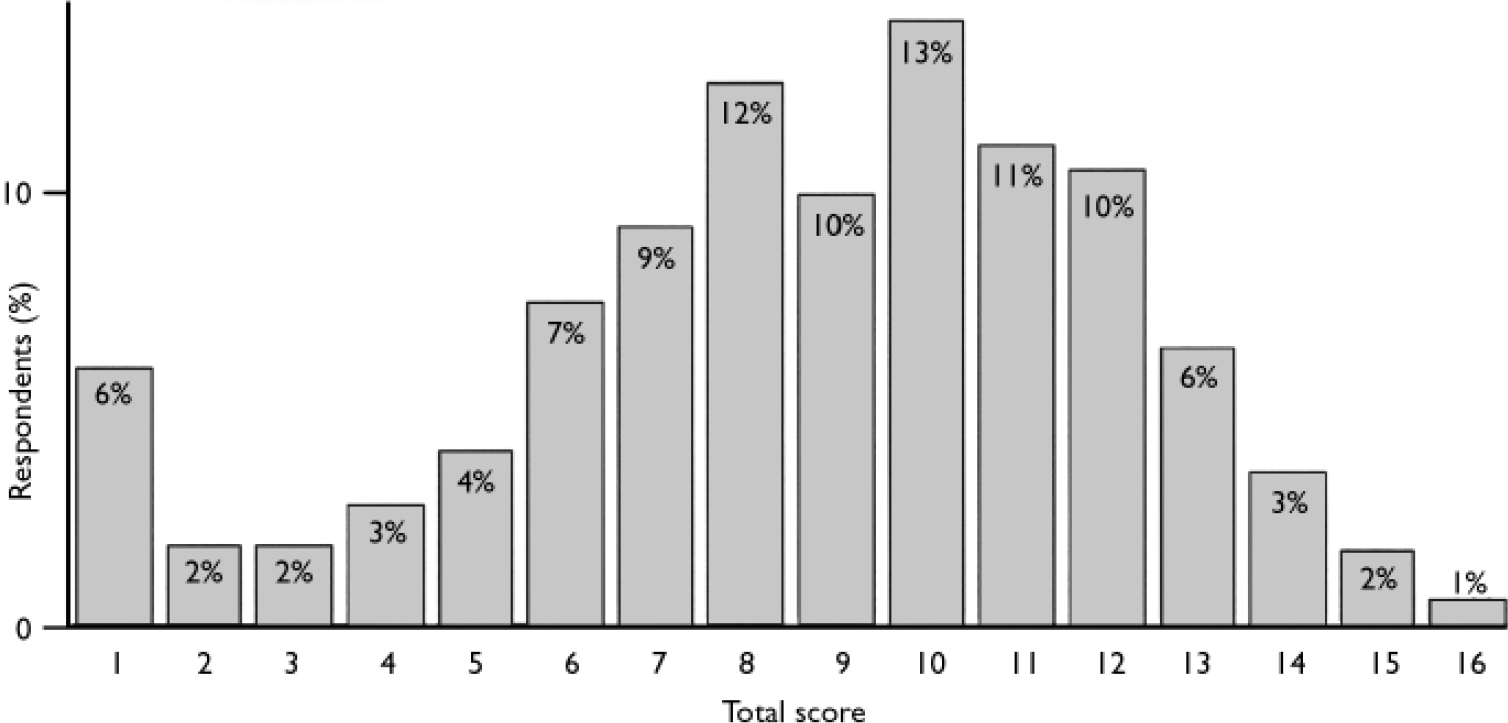
Fig. 2 Distribution of total scores (mean 7.7, s.d.=3.4).
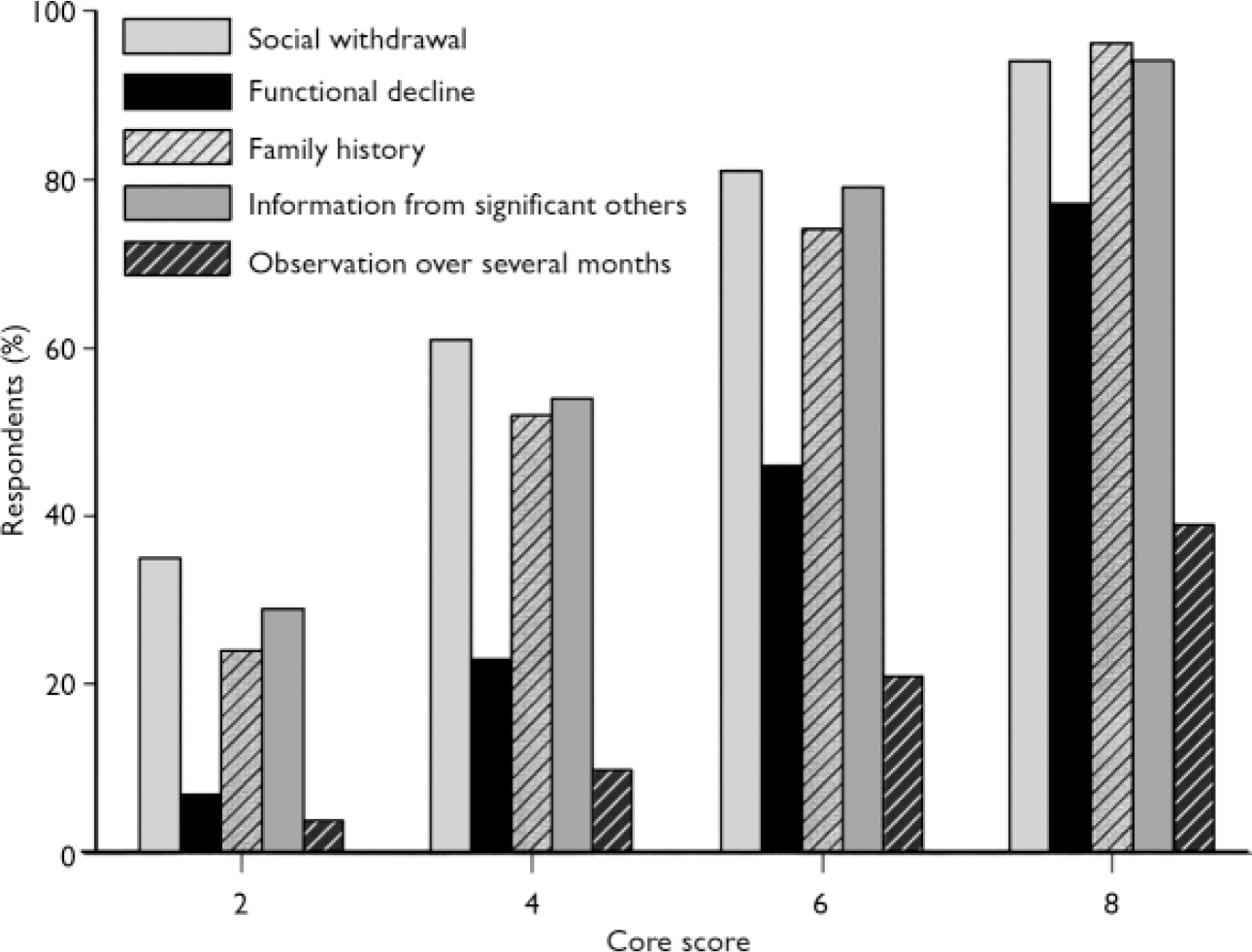
Fig. 3 Percentage of general practitioners who correctly identified the five score-2 items in groups defined by their core score, from 2 (one item identified) to 8 (four items identified). Across all groups the items ‘functional decline’ and ‘observation over several months’ were identified significantly less often than the other items.
Table 2 Percentage of general practitioners identifying the five core items
| Item | % |
|---|---|
| Social withdrawal | 68 |
| Functional decline | 43 |
| Family history | 63 |
| Information from significant others | 65 |
| Observation over several months | 24 |
With regard to diagnostic knowledge, GPs who did not correctly identify any of the score-2 items indicated much more often that they never saw patients in whom they suspected the onset of schizophrenia, compared with their colleagues with core scores of 2 and higher (Mann-Whitney U-test, P<0.001). Interestingly, although GPs with psychiatric training had a higher mean core score than those without such training - 5.85 (s.d.=2.56) v. 4.98 (s.d.=2.76) - the profiles of identified score-2 items for these two groups were similar: χ2=4.08, d.f.=4, NS. Similarly, recent education in the field of early psychosis had no significant influence on score-2 item profile: χ2=1.10, d.f.=4, NS.
Treatment of first-episode and chronic schizophrenia
Question 12, concerning the form of therapy the respondent would recommend for a patient with a suspected first episode of schizophrenia, was answered by 1026 GPs (94%). Four choices were given: psychotherapy, pharmacotherapy, family therapy and ‘observe and wait’. Multiple responses were permitted. Pharmacotherapy, alone or in possible combination with other types of therapy, was selected by 88% of GPs. Psychotherapy alone or in combination was recommended by 47%, but only 1% recommended psychotherapy alone. Family therapy alone or in combination was recommended by 30%, but only 0.2% recommended family therapy alone. The 122 GPs (11%) who did not include pharmacotherapy in their recommendations demonstrated significantly worse diagnostic knowledge: mean core score 2.7 (s.d.=3.2) v. 5.5 (s.d.=2.5), t=–11.46, d.f.=1087, P<0.001.
Two-thirds of respondents (n=732) indicated what kind of medication they would prescribe for the treatment of a first episode of schizophrenia. At most four drugs could be mentioned. We analysed only the frequency with which medication groups were recommended. Of the total of 1542 recommendations, 98.5% were for antipsychotics: 58.7% for atypical and 40.7% for typical antipsychotics. However, 84% of all GPs providing drug treatment recommendations mentioned an atypical antipsychotic at least once. Among the GPs who mentioned only one antipsychotic, 69% recommended an atypical agent. Higher levels of diagnostic knowledge were associated with a significantly higher percentage of atypicals prescribed (median split on total score: 64% v. 58%, t=–2.25, d.f.=728, P<0.05).
Estimates of relapse rate and duration of maintenance treatment
An estimate of the relapse risk of untreated patients in the first year after a first episode was given by 877 GPs (81%); the mean figure was 52% (s.d.=22). An estimate of 60-90% was considered correct and was given by 32% of respondents. Two-thirds (68%) estimated the relapse risk as less than 60%. Eight out of ten GPs estimated the course after a first episode as being favourable (one or several episodes with possible maintenance of social functioning).
In response to question 14, 930 GPs (85%) indicated how long they would maintain antipsychotic treatment after a first episode of schizophrenia, and 919 (84%) how long they would do so in patients with multi-episode schizophrenia. We considered a treatment period after a first episode of schizophrenia of less than 6 months as insufficient, a treatment period of 6-12 months as acceptable and treatment for more than 12 months as meeting international treatment recommendations (Work Group on Schizophrenia, 1977). Thus, 32% of all respondent GPs would recommend an insufficient duration of treatment, 38% an acceptable duration and 30% a duration in accordance with international recommendations. We considered treatment of a patient with multi-episode schizophrenia for less than 3 years as insufficient, and treatment for more than 3 years as meeting international treatment recommendations (Work Group on Schizophrenia, 1977). Thus, 52% of respondents to this question (44% of the total sample) would provide maintenance treatment in patients with chronic illness according to international guidelines. To assess associations of treatment strategies with diagnostic knowledge, we divided all GPs into two groups with high and low levels of diagnostic knowledge, respectively, using the median split of the total score. There was no significant difference with regard to maintenance treatment after a first episode or in multi-episode schizophrenia between the two knowledge groups. Significantly more GPs with correct estimates of relapse rates after a first episode would provide maintenance treatment in first-episode patients according to international recommendations (χ2=13.01, d.f.=2, P=0.001). Also, GPs providing acceptable or correct maintenance treatment recommended atypical antipsychotics significantly more often than the other GPs (67% and 65%, respectively, v. 50%; ANOVA F 2,707=15.48, P<0.001; post hoc tests P<0.001 for both comparisons).
Among GPs with former psychiatric training, 58% would provide maintenance treatment according to international guidelines, whereas only 49% without former psychiatric training would do so (χ2=7.80, d.f.=1, P=0.005). Treatment strategies in first-episode schizophrenia were highly associated with treatment strategies in multi-episode illness (χ2=121.76, d.f.=2, P<0.001. When considering the number of patients treated by each GP, the percentages of GPs recommending acceptable maintenance treatment in patients with multi-episode schizophrenia translate into 54% of all patients with chronic schizophrenia receiving internationally recommended maintenance treatment.
DISCUSSION
Weaknesses and strengths of this study
Before interpreting these results, the weaknesses and strengths of this survey should be acknowledged. First, this study, like any research on attitudes, is limited by the tendency to include cooperative respondents. Second, the answers given may not assess actual behaviour, but should be considered more of a proxy measure of intended behaviour (Reference Penn and CorriganPenn & Corrigan, 2002). Third, compared with telephone or personal interviewing, postal surveys are considered to be inferior in terms of cooperation, interview administration (e.g. rapport and confidence), confidentiality and social desirability (Reference FowlerFowler, 2002). Finally, the training and role of GPs in the healthcare system may vary internationally; thus, the findings of our study may not be generalisable to other settings. However, preliminary results of an international multicentre survey of GPs using identical questions demonstrate findings comparable to the results of this study (Reference Simon and UmbrichtSimon et al, 2004). Nevertheless, the response rate of 28% is reasonably high given the fact that we used no pre-mailing, follow-up contacts or incentives, and the sample included a representative sample of Swiss GPs in terms of age, gender and geographic coverage. To the best of our knowledge, this is the first survey worldwide to make a comprehensive assessment of patient load, treatment setting, attitudes and needs, and diagnostic and treatment knowledge of GPs with regard to their work with patients with chronic schizophrenia and patients in whom they suspect an early psychosis.
Importance of GPs in the treatment of chronic schizophrenia
Our survey indicated that a single GP treats on average about three patients with established schizophrenia annually, which is consistent with the results of previous studies (Reference Lewin and CarrLewin & Carr, 1998). Assuming that this number represents the average number of patients seen by all Swiss GPs, one can extrapolate that about 19 000 patients with established schizophrenia are treated by GPs alone or in collaboration with specialists. Based on a lifetime risk of schizophrenia of 1% (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992) and a total population in Switzerland of approximately 7 million inhabitants, the expected prevalence rate for Switzerland amounts to 70 000 patients with established schizophrenia. Thus, more than a quarter of all patients with schizophrenia are treated by GPs in Switzerland (the number of patients who are seen by GPs but referred for all treatment to a specialist amounts to only 3% of all patients seen). Our results suggest that GPs in Switzerland are involved in the treatment of approximately a quarter of patients with chronic schizophrenia. Therefore, for a considerable number of patients with chronic schizophrenia, GPs in Switzerland have an important role. In the Swiss healthcare system a minority of patients participate in gatekeeper models. Thus, it is questionable to which extent these results can be generalised to the UK and other countries with nationalised gatekeeper systems. However, in studies conducted in the UK it was found that up to a quarter of patients with long-term mental illness depend solely on GPs for their care (Reference Johnstone, Owens and GoldJohnstone et al, 1984; Reference Kendrick, Burns and FreelingKendrick et al, 1994), suggesting that the results obtained in our survey may also apply to other healthcare systems. Furthermore, preliminary results of an international multicentre survey of GPs indicate that the mean numbers of patients with chronic schizophrenia seen by GPs are similar across many countries and healthcare systems (Reference Simon and UmbrichtSimon et al, 2004).
Early psychosis is a low-prevalence disorder in general practice
Considering the overall number of GPs in Switzerland (n=6046) and the mean annual number of patients seen by GPs and suspected to be in an early phase of psychosis (1.6), the total number of such patients can be extrapolated to approximately 10 000 cases per year. Using the incidence values of the World Health Organization ten-country study (Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992) for Aarhus and Nottingham (21 per 100 000), approximately 1500 new cases of schizophrenia per year can be expected in Switzerland. Our results suggest, on the one hand, that a substantial proportion of patients with emerging schizophrenia are seen at some point along their help-seeking pathway to care by a GP, even if emerging schizophrenia is a low-prevalence disorder in the individual general practice. However, compared with the estimated annual incidence rate of 1500 new cases of schizophrenia in Switzerland, GPs may suspect the onset of schizophrenia in a large number of cases in which the disorder will never develop. The fact that GPs with a higher knowledge level reported seeing more patients in whom they suspected early-onset schizophrenia suggests that they may be too quick to develop this suspicion when they identify a possible prodromal symptom, but fail to conduct a thorough assessment that could corroborate or refute their suspicion. Interestingly, this did not apply for GPs with a low knowledge score, who more often seemed to overlook a first episode of schizophrenia.
To our knowledge, no previous study has investigated the prevalence of suspected early schizophrenia among patients in general practice. However, preliminary analyses of the international survey among GPs cited above found that GPs see about 1.4 patients a year in whom they suspect emerging schizophrenia (Reference Simon and UmbrichtSimon et al, 2004).
Definition of score-2 items
With regard to the definition of score-2 items, all of them were either potential precursors of a first episode of schizophrenia or important aspects in the assessment of such patients. However, our choice was guided by two considerations: first, the reported results of studies on early phases of schizophrenia, and second, consideration of what can be practically expected from GPs in terms of recognition of precursors and diagnostic steps. Two of the score-2 items, ‘social withdrawal’ and ‘functional decline’, have frequently been reported in the prodromal phase of schizophrenia (Reference Hafner, Loffler and MaurerHafner et al, 1999). Indeed, in a retrospective study of 200 patients with a first onset of functional psychosis, McGorry et al (Reference McGorry, McKenzie and Jackson2000) reported that a prolonged functional deterioration was likely to predict a diagnosis of schizophrenia. Social withdrawal has been carefully described in a study of the subjective experiences of patients with early psychosis (Reference Moller and HusbyMoller & Husby, 2000). Both social withdrawal and functional decline are often ‘sealed over’ (Reference Birchwood, Todd and JacksonBirchwood et al, 1998) by such patients. Therefore, ‘information from significant others’ (another score-2 item) is an indispensable tool for GPs in their assessment of social withdrawal and functional decline.
High prevalence rates in the prodromal phase of schizophrenia have been found for depression and anxiety (Reference Hafner, Loffler and MaurerHafner et al, 1999), drug misuse (Reference Hambrecht and HafnerHambrecht & Hafner, 1996) and, to a lesser extent, suicidality (Reference Verdoux, Liraud and GonzalesVerdoux et al, 2001). Typically, these findings stem from first-episode studies, i.e. from patients who already have a clinical manifestation of a first episode of schizophrenia. The only prospective study that controlled for the diagnostic efficiency of initial prodromal symptoms (Reference Klosterkótter, Hellmich and SteinmeyerKlosterkötter et al, 2001) showed that, using the Bonn Scale for the Assessment of Basic Symptoms (Reference Gross, Huber and KlosterkotterGross et al, 1997), the cluster containing affective disorders had the highest sensitivity, but comparatively low specificity and predictive power. Suicidality is a serious phenomenon in adolescents and young adults, particularly in the prepsychotic phase (Reference Mortensen and JuelMortensen & Juel, 1993), but psychosis does not feature in the primary pathology in most studies of suicidal adolescents. These findings and reflections led us to define ‘depression/anxiety’ and ‘suicidality’ as score-1 items. Another example that illustrates our procedure in defining item scores is drug misuse. Drug misuse, in particular misuse of cannabis, is a frequent finding in early psychosis (Reference Hambrecht and HafnerHambrecht & Hafner, 1996); however, the use of cannabis is steadily growing in society, particularly among adolescents and young adults, and we therefore rated drug misuse as a score-0 item. Hallucinations and delusions (a score-1 item) often require information from significant others for their detection, yet their presence indicates that these patients have already converted from prodromal stages to frank psychosis.
A positive family history is associated with an increased risk of schizophrenia, but the vast majority of people with schizophrenia have no positive family history (Reference GottesmanGottesman, 1991). None the less, in our analysis we defined the assessment of family history as a score-2 item, since it is an easily applicable tool and may, in the case of positive findings, provide important information. Personal history is of no lesser importance, but we supposed this to be a basic part of any medical assessment.
The ‘forgotten’ insidious features of early psychosis
Although the majority of GPs believed in the existence of early warning signs prior to a first episode of schizophrenia, their diagnostic knowledge showed inconsistencies. Two score-2 items, ‘functional decline’ and ‘observation over several months’, i.e. sustained functional deterioration, were regularly under-identified across all knowledge subgroups. In contrast, GPs were more likely to look out for frank psychotic symptoms such as hallucinations and delusions as well as bizarre behaviour.
These findings highlight the importance that future educational programmes for GPs should put more emphasis on these ‘hidden’ features and on careful history-taking. However, given that in our study the vast majority of GPs expressed a wish for collaboration with secondary care services and preferred low-threshold referral services to educational programmes, the value of the latter must be questioned. Indeed, knowledge profiles did not differ between GPs with and without former psychiatric training and between GPs who had attended educational programmes on early psychosis and those who had not. Thus, given the low prevalence of early psychosis in private practice, it may be strongly assumed that mere educational programmes may be insufficient tools to improve qualitative knowledge levels among GPs. Rather, our results warrant the simultaneous provision of specialised and easily accessible, low-threshold counselling and assessment facilities for professionals in primary care such as GPs.
Treatment recommendations
The vast majority of GPs surveyed would treat a first episode of schizophrenic psychosis pharmacologically, indicating that they consider this to be a state requiring biological treatment. Therefore, this aspect of current treatment practice corresponds to treatment guidelines based on reviews of placebo-controlled studies in the acute and maintenance treatment of patients with first-episode and chronic psychosis (Work Group on Schizophrenia, 1977).
Among all the drug treatment recommendations (each GP could provide up to four) atypical antipsychotics were recommended only in 58%; however, 83% of the GPs who replied to this question mentioned atypical antipsychotics at least once. Thus, GPs in Switzerland, at least in their intended behaviour, seem to follow currently recommended use of atypical antipsychotics as first-line treatment for patients in their first episode of schizophrenia (Reference Marder, Essock and MillerMarder et al, 2002).
General practitioners tend to underestimate the relapse risk in untreated patients after a first episode of schizophrenia. Only a third of all GPs provided estimates that we considered correct. Consistently, 80% of the GPs considered the course of schizophrenia as favourable and only a third of GPs recommended maintenance treatment after a first episode of schizophrenia that conformed to internationally accepted guidelines. Even among the GPs who gave correct estimates of the relapse risk, only 37% would provide adequate maintenance treatment after a first schizophrenic episode. Surprisingly, GPs who had trained in psychiatry (usually 1 year in Switzerland) and those who had attended recent education courses about schizophrenia fared no better than those without psychiatric training or recent education. If one considers that the GPs responding in this survey are likely to be those who have some interest in schizophrenia, it has to be assumed that the overall number of GPs providing adequate treatment is even smaller.
With regard to maintenance treatment of patients with multiple episodes of psychosis, a slightly better picture emerged. About 51% of GPs would treat for at least 3-5 years. Those GPs with psychiatric training fared somewhat better on this question. Not surprisingly, GPs who provide correct maintenance treatment after a first episode significantly more often provide correct maintenance of multi-episode illness compared with the rest of the GPs.
Using the mean figure of 3.2 patients with established schizophrenia who are treated by GPs, it can be extrapolated that about a quarter of patients with schizophrenia (i.e. approximately 19 000) are treated by GPs in Switzerland. Thus, up to 9000 patients may potentially receive inadequate maintenance treatment. Even if these numbers are an overestimate, a considerable number of patients may experience relapses due to ill-considered treatment recommendations, leading to substantial subjective suffering and considerable health costs. Thus, it seems important to educate mental healthcare providers about evidence-based treatment recommendations.
APPENDIX
Study questionnaire
-
I. General information on the treatment of schizophrenic psychoses
1. How many patients with an established diagnosis of schizophrenia do you psychiatrically treat in your practice annually?
-
□ None
-
□ 1–2
-
□ 3–5
-
□ 6–9
-
□ ≥10
2. How much time do you generally invest for a consultation by someone with schizophrenia?
-
□ <10 min
-
□ 10–20 min
-
□ 20–30 min
-
□ >30 min
3. We are interested to know whether you encounter difficulties in the psychiatric treatment of patients with schizophrenia
-
□ No difficulties
-
□ Despite problematic behaviour (e.g. aggression, illicit drug use) of these patients I am able and wish to continue their psychiatric treatment in my practice
-
□ Because of problematic behaviour (e.g. aggression, illicit drug use) of these patients I prefer not to establish their psychiatric treatment in my practice
4. Are these patients treated by you alone, or in collaboration with other specialists or institutions? (more than one answer allowed)
-
□ Treatment exclusively in my practice
-
□ Occasional/regular consultation with a specialist to reassess/advise
-
□ Referral to a specialist for initial diagnosis and to establish the medication regimen, continuation of treatment in my practice
-
□ Referral to a specialist/psychiatric out-patient department and complete handover for treatment
5. In your opinion, what would be the ideal system of treatment for these patients? (more than one answer allowed)
-
□ Treatment exclusively in my practice
-
□ Occasional/regular consultation with a specialist to reassess/advise
-
□ Referral to a specialist for initial diagnosis and to establish the medication regimen, continuation of treatment in my practice
-
□ Referral to a specialist/psychiatric out-patient department and complete handover for treatment
6. Are you satisfied with the collaboration with specialists?
-
□ Yes
-
□ No
-
-
II. Specific information on the detection and treatment of a first schizophrenic episode
7a. How many patients in whom you suspect the onset of schizophrenia do you see in your practice?
-
□ None
-
□ 1–2/year
-
□ 3–5/year
-
□ ≥5/year
7b. In order to estimate how many patients with a suspected onset of schizophrenia are seen in a general practice, we should like you to indicate the overall number of patients you treat annually
— patients
8. Which are the symptoms that you encounter most frequently when you assess for a suspected onset of schizophrenia? (more than one answer allowed)
-
□ Hallucinations/delusions
-
□ Social withdrawal
-
□ Psychosomatic complaints
-
□ Suicidality
-
□ Depression/anxiety
-
□ Bizarre behaviour
-
□ Drug misuse
-
□ Conflicts with parents/teachers/employers
-
□ Functional decline (school/work)
9. Do you think that a first episode of schizophrenia is preceded by early warning signs?
-
□ Yes
-
□ No
10. What do you generally do to corroborate the diagnosis? (more than one answer allowed)
-
□ Personal history
-
□ Family history
-
□ Information from significant others (family/employer/school)
-
□ Observation over several days and weeks
-
□ Observation over several months
-
□ Neurological assessment
-
□ Neuropsychological assessment
-
□ Other examinations (radiographic, electro-physiological)
-
□ Laboratory tests
-
□ Urine toxicology
-
□ Consultation with/referral to a specialist
-
□ Other (specify) —
11. What should the treatment system of patients with a first schizophrenic episode look like ideally?
-
□ Treatment exclusively in my practice
-
□ Occasional/regular consultation with a specialist to reassess/advise
-
□ Referral to a specialist for initial diagnosis and to establish the medication regimen, continuation of treatment in my practice
-
□ Referral to a specialist/psychiatric out-patient department and complete handover for treatment
12. What therapy would you recommend for a patient with a suspected first schizophrenic episode (independent of whether you treat these patients yourself)? (more than one answer allowed)
-
□ Psychotherapy
-
□ Pharmacotherapy
-
□ Family therapy
-
□ Observe and wait only
13. If you medicate, what medication do you most commonly use in patients with a first schizophrenic episode that you treat in your practice, and what are the doses you use?
— (name) — mg/day
— (name) — mg/day
— (name) — mg/day
— (name) — mg/day
14a. For how long would you maintain antipsychotic medication after a first schizophrenic episode in your patients?
-
□ Few days
-
□ 3–4 weeks
-
□ 1–6 months
-
□ 6–12 months
-
□ 12–24 months
-
□ 3–5 years
14b. For how long would you maintain antipsychotic medication in patients with multiple episodes after the remission of an episode?
-
□ Few days
-
□ 3–4 weeks
-
□ 1–6 months
-
□ 6–12 months
-
□ 12–24 months
-
□ At least 3–5 years
15. How high do you estimate the relapse risk of untreated patients during the first year after a first schizophrenic episode?
—%
16. Which are the two clinically most relevant side-effects of long-term antipsychotic treatment that you encounter?
—
—
17. Based on your experience, how do you judge the prognosis of a treated patient after a first schizophrenic episode? (more than one answer allowed)
-
□ The prognosis may be favourable; one single episode with maintenance of performance level is possible
-
□ Mostly several episodes with possible maintenance of performance level
-
□ Mostly several episodes with progressive decline of performance level and severe course of illness
18. With regard to regard to treatment of treatment of early schizophrenic psychosis, which psychiatric services would you like in your region? (more than one answer allowed)
-
□ More continuing education (□ one-day □ half-day □workshops (2 h))
-
□ Specialised mobile team for assessment in your practice
-
□ Specialised, low-threshold referral and consulting service
19. Did you participate in continuing education on schizophrenia or early schizophrenic psychosis in the past few months?
-
□ No
-
□ Yes; please indicate name, place and date of education
-
-
Demographics
20. Please indicate your degree of specialty
-
□ General medicine
-
□ Internal medicine
-
□ Other
21. Was psychiatry part of your specialty training?
-
□ Yes
-
□ No
22. How many years ago did you finish medical school?
— years
23. Do you practise in an urban or in a rural region?
-
□ City without university
-
□ City with university
-
□ Rural region
-
-
Coding system for the anonymisation of your answers
-
• Day of birth of your mother (e.g. 28.06.1930)
 Example:
Example: 
-
• Year of birth of your mother (e.g. 28.06.1930)
 Example:
Example: 
-
• Day of birth of your father (e.g. 04.12.1925)
 Example:
Example: 
-
• Your gender (m or f)

-
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ General practitioners (GPs) play an important part in the treatment of established schizophrenia, and a substantial number of patients in the early stages of schizophrenia are seen at some point by a GP.
-
▪ General practitioners need low-threshold, easily accessible specialised services to which they can refer these patients.
-
▪ The knowledge of GPs about the signs and symptoms of emerging schizophrenia and about the diagnostic steps to be taken is insufficient; they particularly miss the insidious but probably most predictive features of schizophrenia onset.
LIMITATIONS
-
▪ The study was a postal survey with no direct questioning of GPs; thus, our results may overestimate the actual level of knowledge of most GPs, since those who responded were likely to be more interested and thus more knowledgeable about this topic.
-
▪ Since most patients have the freedom to choose any doctor for treatment in Switzerland, our findings may not be applicable to different healthcare systems in which GPs act as gatekeepers.
-
▪ Since our results are based on a postal survey, the actual behaviour of GPs when assessing patients in the early phases of schizophrenia may be different from that indicated in their responses.
Acknowledgements
We thank Dr Alois Tischopp, Institute of Social and Preventive Medicine, University of Zurich, for his statistical advice and help.
The study was supported by an unrestricted grant from Sanofi-Synthélabo SA, Switzerland, to the Swiss Early Psychosis Project.








eLetters
No eLetters have been published for this article.