Generalised anxiety disorder (GAD) was introduced into the psychiatric nomenclature in 1980 with the publication of DSM-III (American Psychiatric Association, 1980). As noted in several comprehensive reviews (Reference Rickels and SchweizerRickles & Schweizer, 1990; Reference SchweizerSchweizer, 1995), the diagnostic changes applied to GAD between DSM-III and DSM-IV (American Psychiatric Association, 1994) have made it difficult to develop a consistent understanding of its course. Despite this, a number of reports (Reference Anderson, Noyes and CroweAnderson et al, 1984; Barlow et al, Reference Barlow, Blanchard and Vermilyea1986a , Reference Barlow, DiNardo and Vermilyea b ; Reference Angst and VollrathAngst & Vollrath, 1991; Reference Blazer, Hughes, George, Robins and RegierBlazer et al, 1991; Reference Durham, Allan and HackettDurham et al, 1997), including work from our group (Reference Yonkers, Warshaw and MassionYonkers et al, 1996), concur that GAD is a chronic illness with an average length of episode far exceeding the one month required by DSM-III or the six months stipulated by DSM-III-R (American Psychiatric Association, 1987) or DSM-IV. The Epidemiologic Catchment Area (ECA) study found that the duration of DSM-III GAD was longer than five years in 40% of patients (Reference Blazer, Hughes, George, Robins and RegierBlazer et al, 1991). We previously showed that only 15% and 25% of 164 patients remitted after one and two years, respectively (Reference Yonkers, Warshaw and MassionYonkers et al, 1996). Although systematic research is beginning to clarify the course of illness in GAD, much less is known about factors that influence the likelihood of remission or recurrence. Analyses from a longitudinal epidemiological study conducted in Zurich found several salient predictors of a poor outcome in GAD: an individual's past chronic course and the presence of comorbid major depressive disorder (MDD) or a personality disorder (Reference Angst and VollrathAngst & Vollrath, 1991). Factors influencing illness in patients who had previously participated (an average of 16 months prior) in a medication trial found that chronicity was associated with cluster B and C personality disorders or a concurrent Axis I disorder (Reference Mancuso, Townsend and MercanteMancuso et al, 1993). Concurrent Axis II psychopathology was also noted in a report analysing course predictors in 80 psychotherapy study completers (Reference Durham, Allan and HackettDurham et al, 1997). In the latter study, marital tension was an additional contributor to chronic illness.
HARP data set
Information from participants with GAD in the Harvard-Brown Anxiety Research Program (HARP) provides a unique data set to investigate factors predicting illness remission because subjects are re-interviewed multiple times at relatively short intervals (6-12 months) over the course of five years. Using this data set, we explored whether concurrent Axis I and Axis II psychopathology, as well as illness severity and patient characteristics, would influence the likelihood of chronic illness. The current report expands our previous three-year follow-up (Reference Yonkers, Warshaw and MassionYonkers et al, 1996) to five years and provides new information on predictors of remission and recurrence.
METHOD
As reported elsewhere (Reference Massion, Warshaw and KellerMassion et al, 1993; Reference Keller, Yonkers and WarshawKeller et al, 1994; Reference Yonkers, Warshaw and MassionYonkers et al, 1996), the HARP is a prospective, observational longitudinal study of patients with DSM-III-R-defined anxiety disorders. Patients were recruited from the psychiatric clinics of eleven Boston and central Massachusetts hospitals, which were primarily tertiary care centres. These clinics included general psychiatry clinics as well as speciality anxiety disorder clinics. Target diagnoses for the study included: panic disorder with or without agoraphobia (PD); agoraphobia without a history of panic disorder (AWOPD); GAD; or social phobia (SP). Exclusion criteria included age less than 18 years or organic mental disorder, schizophrenia or psychosis within six months prior to intake.
Psychiatric evaluation
The initial comprehensive evaluation included selected items from the Personal History of Depressive Disorders (available upon request from Dr Hirschfeld, University of Texas Medical Branch, Department of Psychiatry, Galveston, TX 77550, USA), the Structured Clinical Interview for DSM-III-R, Patient Version (Non-Affective Disorders Section and Psychosis Screen) (SCID-P; Reference Spitzer, Williams and GibbonSpitzer et al, 1990) and the Research Diagnostic Criteria Schedule for Affective Disorders and Schizophrenia - Lifetime (Affective Components) (SADS-L; Reference Endicott and SpitzerEndicott & Spitzer, 1978). Items from the SCID-P and SADS-L were combined to create the SCALUP (available upon request from Dr Keller, Butler Hospital, 345 Blackstone Boulevard, Providence, RI 02906, USA). The DSM-III-R exclusion of a diagnosis of GAD in the setting of another psychiatric disorder was set aside. Overall ratings of well-being were assessed using the Global Assessment Scale (GAS; Reference Endicott, Spitzer and FleissEndicott et al, 1976).
Follow-up was conducted at six-month intervals for the first two years and then annually using the Longitudinal Interval Follow-Up Evaluation (LIFE-UP; Reference Keller, Lavori and FriedmanKeller et al, 1987), which gathered information prospectively on syndrome and overall illness severity, treatment, non-psychiatric medical illness and psychosocial functioning.
Personality disorders were determined by administration of the Personality Disorder Evaluation (PDE; Reference Loranger, Susman and OldhamLoranger et al, 1987) given at the 12-month interview.
Psychiatric status ratings
The LIFE assesses psychopathology by employing a six-point psychiatric status rating (PSR) scale that is scored on a week-by-week basis at each interview. Full DSM-III-R criteria for GAD, including major disruption or functional impairment, is indicated by a PSR score of 6. A PSR score of 5 includes full symptom criteria without major disruption or impairment in psychosocial or work functioning. A PSR score of 4 indicates worry in conjunction with three to five symptoms for most days or worry for less than 50% of the time and six symptoms. A PSR score of 3 indicates three symptoms and worry for less than half the time. Occasional worry is assigned a PSR score of 2, and lack of symptoms is assigned a PSR score of 1.
Interrater reliability and validity
All intake interviews were conducted by experienced clinical interviewers who underwent an initial three- to six-month training period. Ongoing monitoring for interrater reliability included review and comparison of raw data with an interview summary and one video-taped interview per month. The latter was rated independently by other monitors who also met to discuss ratings. Three sub-studies to assess interrater reliability, subject recall and validity of the LIFE-UP PSRs were conducted using subjects already enrolled in HARP (Reference Warshaw, Keller and StoutWarshaw et al, 1994). Median intraclass correlation ranges for PSRs according to disorders were: PD=0.67-0.88, AWOPD=0.49-0.64, SP=0.75-0.86, MDD=0.73-0.74, GAD=0.78-0.86 and GAS=0.72-0.77. The long-term test-retest reliability of subjects' retrospective recall over a one-year period found excellent reliability for GAD (range 0.97-1.00) and very good to excellent reliability for all other index disorders and for MDD (0.89-1.00). An independent external validity assessment comparing the summed PSRs to the GAS found a significant inverse correlation (lower GAS scores reflect lower functioning, whereas higher PSR scores are indicative of greater impairment) of 0.57 (P=0.0001).
Definitions of remission and relapse
Full remission is defined as occasional or no symptoms (PSR=1 or 2) for eight consecutive weeks, a period of time that can detect noticeable changes in morbidity and minimise transient changes in psychopathological state. Partial remission is defined as a decrease in symptoms to PSR=3 (i.e. worry less than 50% of the time accompanied by three symptoms).
Patients were considered to be in an episode at intake if they met full criteria (PSR=5 or 6) for GAD at any point during the six months before intake and had not met the full remission criteria outlined above. This meant that some patients who were considered ‘in episode’ at intake (PSR>2) may not have met full criteria at the moment of intake because they never fully remitted.
Patients who experienced a full remission were designated as relapsed if their PSR score increased to either 5 or 6 (full criteria) for 2 weeks.
Predictor variables
Information regarding marital status (married or living together, divorced/widowed/separated or never married), quality of relationship with spouse, satisfaction with life, socio-economic status and gender were culled from the LIFE at the intake interview. Satisfaction with life and quality of relationships were rated on a scale of 1-5, with 5 reflecting the lowest satisfaction. The severity of illness was determined from the intake GAS score. Intake concurrent Axis I psychopathology was determined by the SCALUP, as was information on length of illness, age of illness onset and age at intake. Axis II diagnoses were determined by the PDE. These covariates were used to predict remission. Too few subjects experienced a relapse to investigate adequately the predictor variables for this event, although the rate of relapse is reported.
Statistical analysis
All statistical analyses were conducted using SAS Version 6.07 (SAS Institute, Carey, NC) using PROC FREQ, PROC NPAR1WAY, PROC TTEST and PROC LIFE TEST. Longitudinal data were analysed using standard survival analysis techniques (Reference Kalbfleish and PrenticeKalbfleish & Prentice, 1980). Kaplan-Meier life tables were constructed for times to remission and time to relapse. Cox regression analysis was applied to continuous variables to identify predictors of remission and relapse.
Subjects
A total of 179 subjects were entered into the study with a lifetime diagnosis of GAD. Of these, 167 patients had at least one follow-up interview and this constitutes the study cohort for this report: 159 (95%) were interviewed at one year, 150 (90%) at two years, 130 (78%) at three years, 118 (71%) at four years and 105 (63%) at five years. Seventy-two per cent of subjects with GAD were female and the average age at illness onset was 21 years (range 2-61). At intake, the average age was 41 years (range 19-75). Personality disorders were common in this cohort and about 36% had a concurrent personality disorder (Reference Dyck, Phillips and WarshawDyck et al, 2000). As reported earlier, comorbid Axis I disorders occurred frequently in HARP probands (83% had another active anxiety disorder) and individual Axis I diagnoses of any type ranged from 5% to 41% (Reference Yonkers, Warshaw and MassionYonkers et al, 1996).
RESULTS
Course
The probabilities for full and partial remission are given in Tables 1 and 2. As can be seen, a total of 55 subjects experienced a full remission and 66 subjects experienced a partial remission in the five-year period. The likelihood of a full remission doubled between the first and fifth years but, none the less, remained low (38% at five years). Even though the chances for partial remission were more favourable, less than 50% of subjects attained this level of well-being by five years. Among patients who experienced full or partial remission, 27% and 39%, respectively, experienced a full relapse during the three years of follow-up (Tables 3 and 4).
Table 1 Probability of full remission over five years
| Year | Number eligible for full remission | Probability of remission (PSR < 3 for 8 weeks) | Number of patients remitting | Number of censored observations |
|---|---|---|---|---|
| 1 | 167 | 0.15 | 26 | 8 |
| 2 | 133 | 0.25 | 14 | 8 |
| 3 | 111 | 0.28 | 4 | 16 |
| 4 | 91 | 0.36 | 9 | 9 |
| 5 | 73 | 0.38 | 2 | 6 |
Table 2 Probability of at least partial remission over five years
| Year | Number eligible for full remission | Probability of remission (PSR ≤ 3 for 8 weeks) | Number of patients remitting | Number of censored observations |
|---|---|---|---|---|
| 1 | 160 | 0.24 | 38 | 8 |
| 2 | 114 | 0.33 | 13 | 7 |
| 3 | 94 | 0.37 | 5 | 13 |
| 4 | 76 | 0.46 | 9 | 9 |
| 5 | 58 | 0.47 | 1 | 5 |
Table 3 Probability of relapse over three years for those who previously experienced full remission
| Year | Number eligible for relapse | Probability of relapse (PSR ≥ 5 for 2 weeks) | Number of patients relapsing | Number of censored observations |
|---|---|---|---|---|
| 1 | 55 | 0.11 | 6 | 4 |
| 2 | 45 | 0.21 | 4 | 5 |
| 3 | 30 | 0.27 | 2 | 6 |
Table 4 Probability of relapse over three years for those who previously experienced partial remission
| Year | Number eligible for relapse | Probability of relapse (PSR ≥ 5 for 2 weeks) | Number of patients relapsing | Number of censored observations |
|---|---|---|---|---|
| 1 | 66 | 0.24 | 15 | 5 |
| 2 | 46 | 0.33 | 5 | 10 |
| 3 | 31 | 0.39 | 2 | 8 |
Predictors of full remission
In a univariate model, higher scores (more impairment) on the following quality-of-life variables significantly predicted a lower likelihood of full remission during the five-year follow-up period: worse overall satisfaction with life (risk ratio=0.67, 95% CI=0.51-0.89; P=0.006), poorer quality of relationship with spouse (risk ratio=0.58, 95% CI=0.38-0.87, P=0.008) and worse quality of relationship with relatives (risk ratio=0.65, 95% CI=0.48-0.89, P=0.003). Concurrent personality disorders also significantly predicted remaining in an episode of illness. Patients with at least one concurrent personality disorder had a risk ratio of 0.30 (95% CI=0.14-0.61, P=0.001), a cluster B personality disorder led to a risk ratio of 0.23 (95% CI=0.06-0.94, P=0.04) and a cluster C personality disorder was associated with a risk ratio of 0.31 (95% CI=0.15-0.66, P=0.002) for remitting from GAD. Finally, a higher GAS score indicated an increased likelihood of remission (risk ratio=2.15, 95% CI=1.19-3.89, P=0.01) (see Fig. 1). Covariates that were not significant included age of onset, length of illness, male gender, marital status, socio-economic, status, general medical health at intake, recreational enjoyment, comorbid MDD, dysthymic disorder, post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), SP or PD.
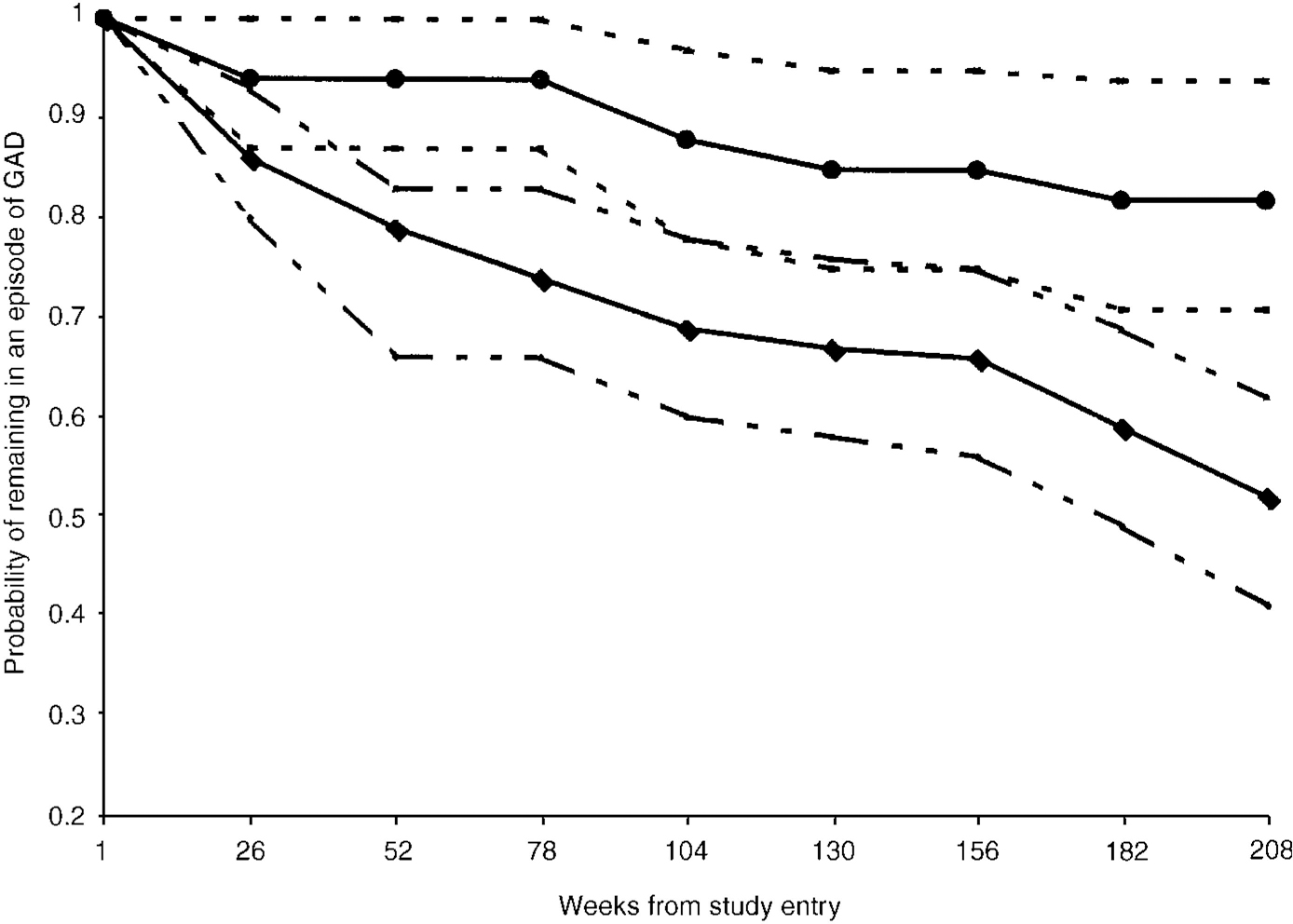
Fig. 1 Probability of remission from generalised anxiety disorder (GAD) in patients with ([UNK]) and without (♦) a cluster C personality disorder. Personality disorder data were available for 155 of 167 individuals with GAD. Eight of 50 patients with a cluster C personality disorder remitted, whereas 45 of 105 without a cluster C personality disorder experienced remission. The 95% upper and lower confidence intervals are given for each group: (—) with cluster C personality disorder; (—) without cluster C personality disorder. Log rank χ2=10.39, d.f.=1 and P=0.002.
When the above positive predictor variables were entered into a multivariate model, having a cluster C personality disorder and poor relationship with relatives remained significant predictors of remaining ill.
Given the findings by others that MDD predicted chronicity, we explored whether the use of selective serotonin reuptake inhibitor (SSRI) biased our results and obscured meaningful differences. Of the 65 subjects with MDD and GAD, 29% took an SSRI, whereas 18% of GAD subjects who had no concurrent MDD took an SSRI. There was a trend towards a difference in groups (χ2=3.08, P=0.79).
Partial remission
The following quality-of-life variables predicted a lower likelihood of partial remission during the five-year follow-up period: worse overall satisfaction with life (risk ratio=0.62, 95% CI=0.47-0.81, P=0.0005), worse quality of relationship with spouse (risk ratio=0.68, 95% CI=0.49-0.94, P=0.02) and poorer quality of relationship with relatives (risk ratio=0.72, 95% CI=0.55-0.95, P=0.02). As with full remission, the existence of any concurrent personality disorder lowered the probability of partial remission (risk ratio=0.48, 95% CI=0.27-0.84, P=0.01). Specifically, a cluster B personality disorder (risk ratio=0.35, 95% CI=0.13-0.98, P=0.05) and a cluster C personality disorder (risk ratio=0.54, 95% CI=0.30-0.96, P=0.04) increased the likelihood that a patient would remain ill. Greater well-being at baseline predicted partial remission, as illustrated by the GAS (risk ratio=1.9, 95% CI=1.14-3.20, P=0.015). Covariates that were not significant included age of onset, length of illness, relationship with friends, male gender, martial status, socio-economic status, general medical health at intake, recreational enjoyment, comorbid SP, MDD, dysthymic disorder, PTSD, OCD or PD.
As above, significant predictors were entered into a multivariate model and covariates that remained significant were worse satisfaction with life and impaired relationships with relatives.
DISCUSSION
The five-year full remission rate found in this prospective study of 167 patients with GAD was nearly identical to the rate found in the ECA study (38% in HARP and 40% in ECA), even though diagnostic criteria and populations under study varied substantially in these two studies. Given that the ECA study required an illness duration of one month and we required six months, shortening the length of episode for GAD does not appreciably affect the likelihood that a patient will remit. This is reinforced by our finding that prior chronic course does not predict whether a proband is able to achieve a full or partial remission from GAD. Given that relapses are common at three years (27%), course may be better described as chronic and relapsing. Risk factors for relapse will be important to investigate when this cohort has been followed for a longer period and when more relapse events have occurred.
Others (Reference Angst and VollrathAngst & Vollrath, 1991) have found, although we did not, that an enduring illness is a predictor of future chronic course. Different findings from those studies may be due to diverging methodologies; for example, the Zurich study was an epidemiological study and the percentage of patients who were very ill may have been lower than it was in HARP. In addition, data in that report included only one follow-up assessment rather than multiple assessments over time. On the other hand, the frequent contact with mental health researchers during HARP follow-up visits may have had a therapeutic effect, thus lessening the deleterious effects of a prior chronic illness course.
In contrast to the work of others, Axis I disorders and specifically concurrent MDD, OCD or PTSD did not significantly inhibit the chances of remission (Reference Angst and VollrathAngst & Vollrath, 1991; Reference Mancuso, Townsend and MercanteMancuso et al, 1993; Reference Durham, Allan and HackettDurham et al, 1997). In HARP, comorbidity in general was high (83% had an additional anxiety disorder), possibly obscuring a specific effect for MDD (Reference Yonkers, Warshaw and MassionYonkers et al, 1996). In addition, treatment was not controlled in HARP and therapeutic interventions aimed at other conditions could have reduced the untoward effects of psychiatric comorbidity on the course of generalised anxiety. This is especially likely because the subjects with a greater number of disorders are more likely to receive aggressive treatment. We found a trend towards greater SSRI use in patients with concurrent MDD and GAD; these and other agents also could have been used in the past.
Predictors of full remission were similar to those for partial remission, with the exception that cluster C personality disorders were significant in the multivariate model only for full remission, and life satisfaction was significant in the multivariate model for partial remission. Findings from these models should be interpreted cautiously, given the limited number of remission events that occurred. Even so, others have suggested that comorbid personality disorders worsen the course of GAD (Reference Barlow, Blanchard and VermilyeaBarlow et al, 1986a ; Reference Mancuso, Townsend and MercanteMancuso et al, 1993). Results from Mancuso et al (Reference Mancuso, Townsend and Mercante1993) are in agreement with our findings that probands with cluster B and C personality disorders are less likely to remit from GAD. Another study comparing patients with MDD to either mixed anxiety and depression or non-panic chronic anxiety found higher rates of cluster C disorders (avoidant and dependent PD) in the chronic anxiety group (Reference Alnaes and TorgersenAlnaes & Torgersen, 1990). Reference Gasperini, Battaglia and DiaferiaGasperini et al (1990) did not find any particular personality disorder to be associated with chronic GAD, but their study did not evaluate prospectively the effects of personality disorders on clinical course.
Generalised anxiety disorder in the setting of a personality disorder results in greater morbidity, which perhaps leads to a lower likelihood of remission. The co-occurring personality disorder may cause disruptions in an individual's interpersonal relationships, which can sustain anxiety and psychiatric illness. We find some support for an association between personality disorders and disrupted relationships in our data. The variable ‘disturbed martial relationships’ was no longer significant in the multivariate model, suggesting that it is not independent of a cluster C personality disorder. On the other hand, patients with dependent or avoidant personality disorders may be more vulnerable to anxiety if intimate relationships are disturbed.
As in our study, Mancuso et al (Reference Mancuso, Townsend and Mercante1993) found that poor overall life satisfaction and impaired ratings of the individual's relationships were more highly associated with continuing to suffer from GAD. Durham et al (Reference Durham, Allan and Hackett1997) found that marital tension predicted a less favourable outcome. The consistency of these findings with ours strengthens the association between these predictors and the course of GAD.
This study has a number of strengths, including the large sample size, thorough assessments using standardised instruments and multiple regular-interval follow-up interviews over a period of five years. Weaknesses include primarily the possibility that follow-up and uncontrolled treatment may have influenced the course of illness. Second, although the reliability in HARP for diagnoses was generally good across raters, the interrater reliability in HARP for diagnoses was generally good across raters, the interrater reliability of agoraphobia without a history of panic was lower, leading us potentially to underdiagnose comorbidity with this disorder. Third, we did not have an ongoing assessment of life stressors, which have been postulated to play a role in the onset of GAD (Reference Angst and VollrathAngst & Vollrath, 1991). However, variables important in the onset of a disorder may not be germane to maintaining the illness (Wittchen & Zerssen, 1988, cited in Reference Angst and VollrathAngst & Vollrath, 1991; Reference Mancuso, Townsend and MercanteMancuso et al, 1993).
In summary, we find that over the five years of follow-up, less than 50% of people with GAD experience either a full or partial remission. Relapse rates are substantial at three years (27%), supporting a chronic relapsing course for GAD. As with previous research, our study finds that personality disorder comorbidity (particularly cluster C disorders), life satisfaction and relationship with spouse and family are significant predictors of clinical course.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ The remission rate from generalised anxiety disorder (GAD) was only 0.38 at five years.
-
▪ A lower likelihood of remission occurred in patients with GAD having poor-quality family relationships and concurrent personality disorders.
-
▪ Comorbid major depressive disorder or other Axis I psychiatric diagnoses did not influence the chronicity of GAD.
LIMITATIONS
-
▪ Data from clinical samples may be representative of patients with more severe, comorbid, chronic illnesses rather than simple GAD.
-
▪ Ongoing measures of life stress were not queried in this cohort.
-
▪ Multivariate models should be interpreted cautiously, given the relatively few remission events.
ACKNOWLEDGEMENTS
The Harvard-Brown Anxiety Research Program is conducted with the participation of the following investigators: P. Alexander, MD, J. Eisen, MD, A. Gordon, MD, M. B. Keller, MD (Chairperson), K. Phillips, MD, S. Rasmussen, MD and R. Stout, PhD (Butler Hospital; Brown University School of Medicine); M. G. Warshaw, MSS, MA (Brown University School of Medicine); T. Shea, PhD (Veterans Administration Hospital, Providence; Brown University School of Medicine); J. Cole, MD and G. Mallya, MD (McLean Hospital; Harvard School of Medicine); E. Fierman, MD and F. Rodriguez-Villa, MD (Beth Israel Hospital; Harvard Medical School); M. P. Rogers, MD (Brigham and Women's Hospital; Harvard Medical School); R. M. Goisman, MD and N. Weinshenker, MD (Massachusetts Mental Health Center; Harvard Medical School); R. Vasile, MD (New England Deaconess Hospital; Harvard Medical School); J. Ellison, MD, MPH (Harvard Community Health Plan and the Cambridge Hospital; Harvard Medical School); A. Massion, MD (University of Massachusetts Medical School); G. Steketee, PhD (Boston University School of Social Work); K. Yonkers, MD (Yale University School of Medicine). Additional contributions from: J. Curran, MD, I. Goldenberg, PsyD and R. Hirschfeld, PhD (University of Texas, Galveston); J. Hooley, DPhil (Harvard University); P. Lavori, PhD (Stanford University); J. Perry, MD (Jewish General Hospital; McGill School of Medicine, Montreal); L. Peterson (Veterans Administration Hospital, Tcgus, Maine); J. Reich, MD, MPH and J. Rice, PhD (Renard Hospital; Washington University School of Medicine, St Louis); H. Samuelson, MA (Brigham and Women's Hospital); D. Shera, MS and M. Weissman, PhD (Columbia University); K. White, MD (St Elizabeth's Hospital, Brighton, MA). This investigation was supported in part by the Upjohn Company and in part by National Institute of Mental Health Grants MH51415 and K08-MH01648-01. The Quintiles Corporation provided valuable consultation services to this project. This manuscript has been reviewed by the Publications Committee of the Harvard-Brown Anxiety Research Program and has its endorsement.








eLetters
No eLetters have been published for this article.