Explanatory models of illness encompass a person's ideas about the nature of their problem, its cause, severity, prognosis and treatment preferences (Reference KleinmanKleinman, 1980). Dissonance between patients’ and professionals’ explanatory models may affect help-seeking behaviour (MacCarthy, 1988), treatment compliance (Reference Foulks, Persons and MerkelFoulks et al, 1986), satisfaction (Reference Callan and LittlewoodCallan & Littlewood, 1998) and culturally sensitive clinical practice (Reference Bhui and BhugraBhui & Bhugra, 2002). In the context of cultural background, there is interest in explaining the higher rates of psychotic illness, involuntary admissions and dissatisfaction with services among first- and second-generation immigrants reported in the UK and The Netherlands (e.g. Reference Harrison, Glazebrook and BrewinHarrison et al, 1997; Reference Parkman, Davies and LeeseParkman et al, 1997; Reference Bhugra and BhuiBhugra & Bhui, 1998; Reference Selten, Veen and FellerSelten et al, 2001; Reference Bhui, Stansfeld and HullBhui et al, 2003). However, the generalisability of research has been limited by isolated samples in different countries (e.g. Reference Weiss, Sharma and GaurWeiss et al, 1986), lack of standardised instruments (e.g. Reference Callan and LittlewoodCallan & Littlewood, 1998) and heterogeneous samples (e.g. Reference Lloyd, Jacob and PatelLloyd et al, 1998).
METHOD
Aims
-
(a) To use a standardised measure to assess qualitatively the explanatory models among patients with schizophrenia in a local White British group and three second-generation ethnic groups living in similar socio-economic conditions in East London.
-
(b) To compare quantitatively the explanatory models across the four groups.
-
(c) To investigate the association between explanatory models and clinical and psychological characteristics in all of the patients.
The four groups were of African–Caribbean, Bangladeshi, West African and UK White origin. Second-generation patients were selected because: there are consistent differences in service use and outcome among this group; the findings would be less confounded by individual histories of migration and schooling because all interviewees have grown up in the same educational system and background culture; all interviews could be conducted in English because this is most relevant for clinical practice; and the material could be elicited in English and analysed without considering specific connotations in different languages. The inclusion criteria were selected to reduce the heterogeneity of the groups and increase the possibility of detecting specific differences despite relatively small sample sizes for each ethnic group.
Sample
The sample consisted of four groups of out-patients from four distinct cultural backgrounds aged between 18 and 48 years who met DSM–IV (American Psychiatric Association, 1994) criteria for a diagnosis of schizophrenia, were in the care of a community mental health team, had no known organic impairment and had no significant formal thought disorder as assessed on the Brief Psychiatric Rating Scale (BPRS; Reference Overall and GorhamOverall & Gorham, 1962). The four groups were recruited in East London and the three groups of non-UK origin were all second-generation immigrants. Patients were identified as second generation if they were either born in the UK with both parents of the specified origin or moved to the UK before the age of 12 years. Participants were included when clinical and self-report of ethnicity were in full agreement. In accordance with the central limit theorem, 30 participants per group were recruited so that the mean could be approximated closely by the normal distribution (Reference MukhopadhyayMukhopadhyay, 2000). Samples A, B and C comprised individuals of second-generation African–Caribbean, Bangladeshi and West African (from Nigeria or Ghana) ethnic origin. Sample D consisted of White English participants, all born in the UK.
Participants were recruited from secondary mental health services (i.e. four community mental health teams, a day hospital and a psychology service). Service managers, psychiatrists and support workers were consulted to identify those clients meeting the inclusion criteria. Diagnosis was clinical rather than derived from case notes. On clinicians’ recommendations, patients were contacted by letter, telephone or in person at clinics according to the individual patient's preferences and circumstances. All participants provided written informed consent to take part in the study.
Measures
A modified version of the Short Explanatory Model Interview (SEMI; Reference Lloyd, Jacob and PatelLloyd et al, 1998) enabled a qualitative assessment of patients’ conceptualisations of their illness within a structured framework that allowed for eventual quantification of data. Questions originally developed for use in primary care that were not relevant for people with chronic illness were omitted from the scale. The modified version was divided into three sections on the nature of the problem and its consequences, aetiology and treatment. Each patient interview was audio-recorded and transcribed.
Psychopathology was observer rated using the 24-item version of the BPRS (Reference Overall and GorhamOverall & Gorham, 1962). Patient insight into their illness was observer rated using the Schedule for Assessment of Insight into Psychosis (SAI; Reference David, Buchanan and ReedDavid et al, 1992), which has three sub-scales: treatment compliance, awareness of illness and relabelling of symptoms. Ratings were based on information from the patient and additional information from the keyworker. Quality of life was self-rated with the Manchester Short Assessment of Quality of Life (MANSA; Reference Priebe, Huxley and KnightPriebe et al, 1999). A modified version of the Helping Alliance Scale (HAS; Reference Priebe and GruytersPriebe & Gruyters, 1993) was self-rated by the patient who assessed their primary therapeutic relationship, typically with their keyworker. Treatment satisfaction was self-rated using the Patient Care Satisfaction Questionnaire (PCSQ; Reference Barker, Shergill and HigginsonBarker et al, 1996). Finally, health locus of control was self-rated with the Health Locus of Control scale (HLC; Reference Wallston, Wallston and KaplanWallston et al, 1976), which has three sub-scales: external locus of control, internal locus of control and powerful others. Unless otherwise stated, mean scores for each measure are reported and were used in data analyses. For all of the scales, a higher score indicates greater presence of the construct, with the exception of the PCSQ where a higher score indicates greater treatment dissatisfaction.
Data analysis
The qualitative data collected using the SMI were content analysed and coded into categories a posteriori. Responses to the question ‘What do you think has caused your problem’ were initially coded into ten categories derived from the content analysis: do not know; drugs/alcohol/medication; interpersonal problems; supernatural causes; mental illness; physical illness/trauma; personality; stress; negative childhood events; and other. Given the small cell counts, these categories were then collapsed to form four categories: biological (physical illness/substance misuse); social (interpersonal problems/stress/negative childhood events/personality); supernatural (supernatural); and non-specific (do not know/mental illness/other). Although the heterogeneity of responses in the non-specific category renders it clinically meaningless, it is retained for the sake of completeness of the data. A power calculation in detecting differences between the groups of explanatory models and treatment preferences in categorical analyses indicated that: a large effect size (i.e. a difference in proportions when translated into a fourfold product moment r ranges between 0.37 and 0.39) would be detected with 87% power on a two-tailed significance test where P=0.05; a medium effect size (when translated r=0.25) would be detected with 49% power; and a small effect size (when translated r=0.10) with only 12% power (Reference CohenCohen, 1988). Interrater agreement in classifying the raw data into categories was calculated using the κ statistic. The four causal categories were compared on socio-demographic, clinical and psychological variables. The therapeutic relationship scores were recorded into a score below or above the midpoint on the scale, indicating a generally positive v. a generally negative therapeutic relationship. Differences between the groups according to explanatory model and ethnicity were analysed using analysis of variance and χ2 or Fisher's exact test. Where multiple tests were conducted, the Bonferroni-adjusted significance levels are reported.
RESULTS
A total of 180 patients were identified by clinicians as meeting the inclusion criteria, 131 were sent letters informing them about the study and requesting their participation. Of these, 72 were interviewed, 10 did not consent and 49 did not respond at all. Fourteen patients were contacted by telephone: thirteen were interviewed and one did not consent. Thirty-five patients were approached at clinics, of whom thirty-four were interviewed and one did not consent. Of those patients who were approached by telephone or in person, the non-consent rate was 8.4%. The total number of people interviewed, all in face-to-face interviews, represented 66% of the potential sample.
Thirty African–Caribbeans, Bangladeshis and UK Whites and 29 West Africans were interviewed. Their socio-demographic and clinical history characteristics are presented in Table 1. Bangladeshis were younger and had a shorter duration of illness than African–Caribbeans and UK Whites. They were also less likely to live alone than West Africans.
Table 1 Socio-demographic characteristics of the four groups
| A African–Caribbean (n=30) | B Bangladeshi (n=30) | C West African (n=29) | D UK White (n=30) | Statistics (d.f.) | |
|---|---|---|---|---|---|
| Age: mean (s.d.) | 35.7 (6.5) | 30.6 (7.7) | 33.3 (6.3) | 36.9 (5.8) | F(3)=5.3 P=0.002* |
| Male: % | 57 | 77 | 69 | 73 | NS |
| Length of illness, years: mean (s.d.) | 12.9 (8.5) | 6.9 (4.1) | 10.0 (5.9) | 12.9 (6.8) | F(3)=5.4 P=0.002* |
| Admissions, n: mean (s.d.) | 3.7 (2.4) | 3.1 (2.2) | 4.0 (2.5) | 3.4 (2.3) | NS |
| Involuntary admissions, n: mean (s.d.) | 1.8 (1.8) | 0.8 (1.1) | 2.2 (2.3) | 1.6 (2.4) | NS |
| Length of hospitalisation in months: mean (s.d.) | 13.9 (14.7) | 9.5 (13.4) | 14.0 (20.9) | 23.1 (38.0) | NS |
| Unemployed: % | 90 | 80 | 89 | 83 | NS |
| Living alone: % | 41 | 17 | 48 | 46 | χ2=24.1 P=0.063† |
The four ethnic groups were also compared on clinical and psychological characteristics and there were no significant differences between the groups on any of these variables (data available on request).
Explanatory models
Responses to the SEMI questions concerning concept, severity, course, aetiology and treatment from the sample as a whole were content analysed and are presented in Table 2. Although an individual may have cited more than one response, particularly with respect to aetiology and treatment preferences, the first response provided by each participant was coded for the purpose of this analysis. Four raters independently coded the raw data from the transcripts into categories. The chance-corrected proportional interrater agreement between the four raters was very good: κ=0.87 (Reference AltmanAltman, 1991).
Table 2 Content analysis of responses to questions on concept, cause, treatment, severity and course of illness
| Concept | Cause | Treatment | Severity | Course | |||||
|---|---|---|---|---|---|---|---|---|---|
| Do not know | 9.2% | Do not know | 21.4% | Do not know | 12% | Do not know | 2.7% | Do not know | 18.6% |
| Schizophrenia/psychosis | 20.2% | Drugs/alcohol | 7.7% | Medication/brain scan | 19.7% | Not severe | 17.9% | Short | 3.1% |
| Depression/manic depression | 18.5% | Interpersonal | 16.2% | Practical help | 5.4% | Moderately severe | 31.3% | Episodic | 2.7% |
| Mental illness | 16.0% | Supernatural | 15.4% | Counselling/understanding illness | 18.8% | Very severe | 29.5% | Long | 47.8% |
| Others say I have schizophrenia | 9.2% | Mental illness | 5.1% | Social activities/occupational therapy | 4.5% | Variable | 18.8% | ||
| Non-specific illness | 3.4% | Physical illness | 5.1% | Natural remedies | 5.4% | ||||
| Spiritual experience | 5.9% | Personality | 8.5% | Get better | 12.5% | ||||
| Nothing wrong | 5% | Stress | 9.4% | Receiving right treatment | 2.7% | ||||
| Other | 12.6% | Childhood events | 7.7% | None | 4.5% | ||||
| Other | 3.4% | Other | 15.2% |
Approximately 20% of the sample called their problem schizophrenia/psychosis and 18.5% called it depression/manic depression. Almost two-thirds said that their illness was either moderately or very severe. Approximately half stated that their illness had a long course and almost one-third said that it had a short course.
There was substantial variation in the primary causes of illness cited: 21.4% said they did not know; 16.2% cited interpersonal factors (e.g. ‘break-up of relationship’, ‘emotional baggage’); 15.4%, supernatural factors (e.g. ‘someone did magic to me when I was a little boy’, ‘evil forces’); 9.4%, stress mostly arising from training or employment (‘stress from work’, ‘working very hard’); 8.5%, personality factors (e.g. ‘myself for not being wiser’, ‘lack of knowledge of when I was becoming stressed’); 7.7%, drugs/alcohol (e.g. ‘heavy drinking’, ‘took crack’); 7.7%, negative childhood events (e.g. ‘physical and mental abuse in childhood’, ‘influence in life when I was young’); 5.1%, mental illness (e.g. ‘depression at a young age’, ‘breakdown’); and 5.1%, physical illness or injury (e.g. ‘heart disease’, ‘run over by a car and was in a coma’).
With respect to participants’ first treatment preference, 19.7% thought that they should receive medication; 18.8% wanted counselling, including help understanding the illness; 12.5% wanted something to make them get better but did not specify what; 5.4% wanted natural remedies (e.g. ‘natural herbal remedies’, ‘alternative herbal treatment instead of medication’); 5.4% wanted practical help (e.g. ‘help with accommodation’, ‘help with housing problems and around the house’); 4.5% wanted social/occupational activities (e.g. ‘occupational therapy’, ‘something to do like a club’); 2.7% said they were getting the right treatment; and 15.2% mentioned specific treatments that did not fit into the general categories (e.g. ‘equal opportunities as the system hates Black people’, ‘X-ray’).
Explanatory models and ethnicity
Concept of illness, or the name patients used to describe their problem, did not differ significantly between the four groups (χ2=18.9, P=0.09), nor did perceived severity of illness (χ2=16.02, P=0.18). Cause of illness, coded into four categories broken down by ethnic group is displayed in Table 3 and Fig. 1.
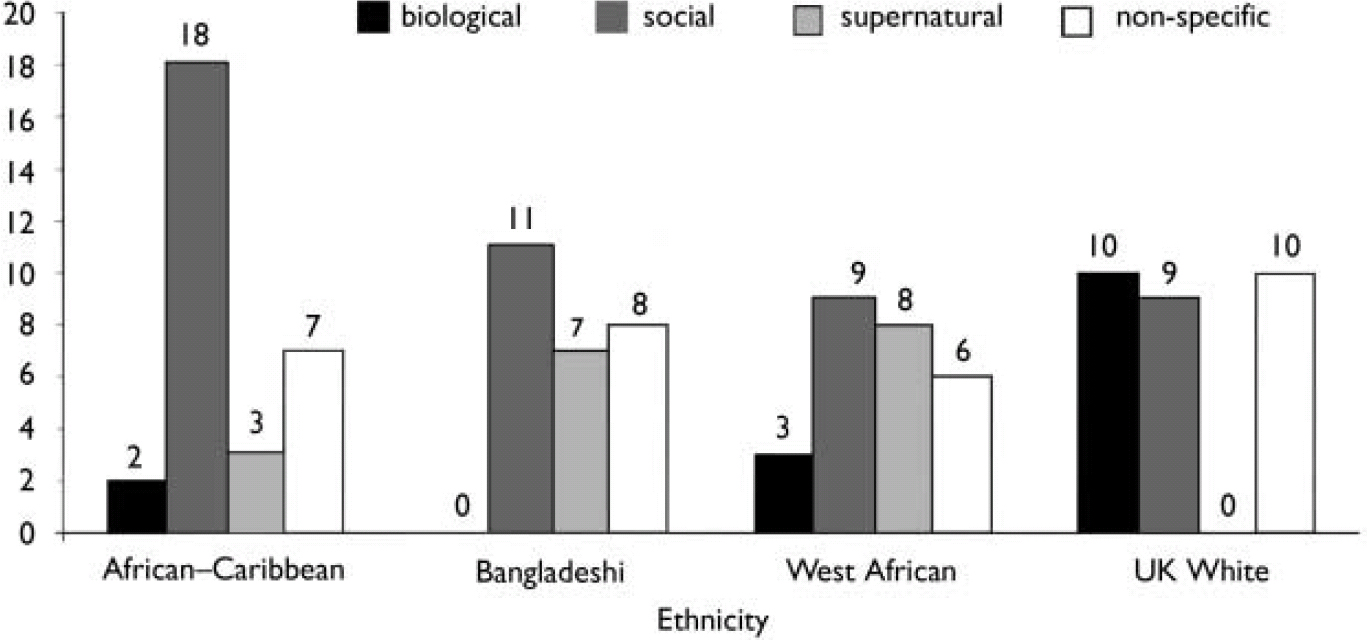
Fig. 1 Cause of illness by ethnic group.
Table 3 Explanatory models of the four groups
| Primary cause of illness | Biological n (%) | Social n (%) | Supernatural n (%) | Non-specific n (%) |
|---|---|---|---|---|
| A African–Caribbean (n=30) | 2 (6.7%) | 18 (60%) | 3 (10%) | 7 (23.3%) |
| B Bangladeshi (n=30) | 0 (0%) | 11 (42.3%) | 7 (26.9%) | 8 (30.8%) |
| C West African (n=29) | 3 (10.7%) | 9 (31%) | 8 (28.6%) | 6 (21.4%) |
| D UK White (n=30) | 10 (34.5%) | 9 (31%) | 0 (0%) | 10 (34.5%) |
| Total (%) | 15 (13%) | 49 (43%) | 18 (16%) | 31 (27%) |
Cause of illness differed significantly according to ethnicity (see Fig. 1) in a 4×4 analysis (χ2=28.7, d.f.=9, P<0.001). Because the 4×4 analysis does not show which groups differed on which measures, the effect was broken down into a series of focused 2×2 comparisons using χ2 and Fisher's exact test in the case of low cell counts.
The sources of the overall effect were somewhat localised. Overall, there were no differences between African–Caribbeans, Bangladeshis and West Africans except when social causes were compared with supernatural causes; African–Caribbeans were more likely (P=0.053) to cite social causes than West Africans.
By contrast, Whites were distinguished from the other groups in four cases. First, when biological causes were compared with supernatural causes, Whites cited biological causes more frequently than African–Caribbeans (P=0.022), Bangladeshis (P<0.001) and West Africans (P=0.001). Second, when biological causes were compared with social causes, Whites cited biological causes more frequently than African–Caribbeans (P=0.05) and Bangladeshis (P=0.003). Given the statistical power of the study, a trend (P=0.072) for the same pattern when Whites were compared with West Africans is worth noting. Third, when biological causes were compared with non-specific causes, Whites cited biological causes more frequently than Bangladeshis (P=0.014). Finally, when supernatural causes were compared with social and non-specific causes, both Bangladeshis (cf. social P=0.016, cf. non-specific P=0.013) and West Africans (cf. social P=0.024, cf. non-specific P=0.004) cited supernatural causes more frequently than Whites.
Treatment preference also differed according to ethnicity (χ2=24.7, P=0.054). Bangladeshis were less likely to want treatment of any kind than Whites (P=0.019) and African–Caribbeans (P=0.049). Both Whites and African–Caribbeans were more likely to want counselling and, additionally, Whites were more likely to want medication (P=0.051) or to be unsure about what they wanted (P=0.029). Bangladeshis were also more likely to want non-conventional forms of treatment, including natural remedies and spiritual activities, than Whites (P=0.008), who were more likely to be unsure about what they wanted.
Cause of illness and clinical and psychological characteristics
Because there was substantial variation within ethnic groups, explanatory models (independent of ethnicity) were analysed with respect to the clinical and psychological characteristics assessed. With respect to concept of illness, patients who called their problem a specific or non-specific psychiatric illness or breakdown were more likely to accept that they had a mental illness than those who named it differently (P=0.05). For severity of illness, patients who perceived their illness to be very severe had a lower external health locus of control than those who thought that their illness was moderately severe (P=0.05).
Cause of illness cited by patients was significantly related to treatment satisfaction, therapeutic relationships and acceptance of mental illness (see Table 4). People who cited biological causes were more likely to say that they were receiving the right treatment for them (P=0.021), were more satisfied with treatment (P=0.041) and had better therapeutic relationships (P=0.006) than those who cited social causes. They were also more satisfied with treatment (P=0.012) and had better therapeutic relationships (P=0.044) than those who cited non-specific causes. People who cited social causes were most likely to accept that they had a mental illness, significantly more so than those who cited supernatural causes (P=0.044), but had worse therapeutic relationships than the latter (P=0.046). Cause of illness cited was not associated with treatment compliance (F=1.3, P=0.28). Hence, having a biological explanatory model was not associated with better treatment compliance.
Table 4 Differences in clinical characteristics according to cause of illness
| Non-specific | Biological | Social | Supernatural | Statistics | |||||
|---|---|---|---|---|---|---|---|---|---|
| Receiving the right treatment1 | 5.7 | 7.8 | 4.9 | 6.5 | F=3.3 P=0.022 | ||||
| Treatment satisfaction1 | 54.7 | 45.6 | 53.1 | 52.1 | F=3.5 P=0.019 | ||||
| Acceptance of mental illness1 | 4.2 | 4.5 | 4.8 | 3.2 | F=2.7 P=0.051 | ||||
| Therapeutic relationship2 | Below 15 | Above 15 | Below 2 | Above 12 | Below 26 | Above 19 | Below 5 | Above 12 | χ2=10.3 P=0.016 |
With respect to treatment, those who wanted practical help had higher levels of symptomatology than those who wanted medication (P=0.005) or no treatment (P=0.038). Those who wanted medication were more likely to be compliant with treatment (P=0.041). Finally, those who wanted medication were more likely to accept that they had a mental illness (P=0.001).
DISCUSSION
Explanatory models and ethnicity
In the main there were no differences between the three non-White groups. However, there were consistent differences between the White and non-White groups. When biological causes were compared with supernatural causes of illness, Whites cited biological causes of illness more frequently than the three non-White groups, who cited supernatural causes more frequently. When biological causes were compared with social causes, Whites cited biological causes more frequently than African–Caribbeans and Bangladeshis. Conversely, both African–Caribbeans and Bangladeshis cited social causes more frequently. When social causes were compared with supernatural causes, Whites cited social causes more frequently than Bangladeshis and West Africans, who were more likely to cite supernatural causes.
Explanatory models, ethnicity and treatment
Bangladeshis, who cited supernatural causes more frequently, either wanted alternative forms of treatment such as religious activities or no treatment at all. Conversely, Whites, who cited biological and social causes more frequently, preferred medication and counselling. Type of explanatory model, independent of ethnicity, was related to satisfaction with treatment, suggesting that what people believe about their illness influences their experience of and benefit from mental health services (cf. Reference DeinDein, 2002). There was a marked difference between a biological or social explanatory model and corresponding perceptions of treatment. People with a ‘biological’ explanatory model more often said that they were receiving the right treatment for them, were more satisfied with the treatment and had better therapeutic relationships than those with a ‘social’ explanatory model. Although the clinician's explanatory model was not assessed in this study, it seems reasonable to suggest that because the predominant treatment model is medication-based it is primarily biological. This finding seems to support Callan & Littlewood (Reference Callan and Littlewood1998), who found that satisfaction is higher when there is concordance between the patient's and psychiatrist's explanatory models.
Although cause of illness stated by patients was related to their treatment preferences and perceived benefit from and satisfaction with treatment, it was not associated with treatment compliance. A similar finding was also reported by Holzinger et al (Reference Holzinger, Löffler and Müller2002), who investigated subjective illness theory and compliance with atypical antipsychotics among people with schizophrenia.
People who cited supernatural causes of illness were less insightful (i.e. less likely to accept that they had a mental illness) but were not less compliant with treatment. Goldberg et al (Reference Goldberg, Green-Paden and Lehman2001) found that ethnic minorities were more likely to be rated as having poor insight. It may be that insight is narrowly assessed as a difference between the perspective of the rater and the person being rated in how mental illness is conceptualised, without taking account of differences in social cultural attributions. The fact that type of explanatory model was not related to treatment compliance may highlight the lack of explanatory power of insight if assessed in this way (cf. Reference McCabe, Quayle and BeirneMcCabe et al, 2000; Reference McCabe and QuayleMcCabe & Quayle, 2002). Indeed, other sociocultural factors, such as varying degrees of social deference, may mediate readiness to comply with treatment.
Methodological issues
In this study, individual accounts of cause of illness were not fixed but fluid and often people did not cite a single, but multiple causes. Williams & Healy (Reference Williams and Healy2001) suggested that ‘exploratory map’ rather than ‘model’ might reflect more accurately how people construct narratives about illness. This may be particularly relevant among people of different ethnic origin in the UK, who will vary in degree of acculturation and so may draw on multiple social and linguistic resources in narratives about illness. The fluidity of accounts of illness during the course of a single interview is compounded when test–retest reliability is considered. The stability of explanatory models over time appears to be low (Reference McCabe and PriebeMcCabe & Priebe, 2004), thus limiting their value in predicting long-term outcome.
The current study used an operationalised method to assess explanatory models, as suggested by Bhui & Bhugra (Reference Bhui and Bhugra2002). It highlighted the limitations as well as the potential benefits of such methods (cf. Reference Canino, Lewis-Fernandez and BravoCanino et al, 1997). There was a tension in reducing explanatory models to single categories to link them with quantitative outcomes. A necessarily reductionistic approach in condensing complex accounts of illness to fixed simple categories resulted in the loss of rich contextual information, underlining the tension between the anthropological framework within which the concept of explanatory model of illness was originally developed and a reductionistic approach for quantification (Reference McCabe and PriebeMcCabe & Priebe, 2004). Moreover, the categories derived from the qualitative analysis appear to be more sensitive in discriminating White from non-White groups and less sensitive in discriminating between the three non-White groups. It is possible that the analyst's categories are less finely tuned than those members themselves (i.e. in this case the different cultural groups) use to order the social world.
The low statistical power of the small sample sizes precluded the identification of small effect sizes. Consequently, negative findings, such as the failure to detect a significant association between explanatory model and treatment compliance, must be interpreted cautiously. Also, although post hoc testing between groups for specific results was Bonferroni adjusted, there was no adjustment for multiple testing across all tested associations. This approach is justified, however, in an exploratory study investigating a number of independent research questions (Reference PernegerPerneger, 1998).
Although it is a strength of the study that all groups were assessed with standardised instruments and that the groups were comparable in their socio-economic conditions, there may have been a selection bias. Those who did not agree to participate or were not in contact with services are likely to be less satisfied with treatment and may differ more in their explanatory models. Further research is required to shed light on the influence of explanatory models in the early phases of illness on contact with services and benefit from treatment. A related issue is that it remains unclear whether and, if so, how contact with clinicians affected patients’ explanatory models.
Although various methodological issues remain unresolved, this study is a step forward because it successfully linked qualitative data elicited in semi-structured interviews with conventional quantitative outcomes and yielded statistically significant associations that are clinically relevant and may guide further research. The differences in explanatory models between ethnic groups may be considered reliable because Fisher's exact test is a conservative statistical test (Reference Rosenthal and RosnowRosenthal & Rosnow, 1991) and so is unlikely to lead to Type I errors.
In conclusion, this study suggests that explanatory models differ reliably according to cultural background and are associated with treatment preferences and satisfaction but not with treatment compliance. Although Whites are more likely to have a biological explanatory model, African–Caribbeans, West Africans and Bangladeshis are more likely to have a social or supernatural explanatory model. Moreover, having a biological explanatory model, especially compared with a social explanatory model, is linked with greater treatment satisfaction and better therapeutic relationships.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ A biological explanatory model of illness among patients with schizophrenia is associated with greater treatment satisfaction and better therapeutic relationships than a social explanatory model.
-
▪ Type of explanatory model does not appear to be associated with treatment compliance.
-
▪ Although explanatory models varied according to ethnicity, they also varied substantially within ethnic groups.
LIMITATIONS
-
▪ The small sample sizes facilitated the detection only of large differences between the groups.
-
▪ Although explanatory models were assessed qualitatively in detail, complex individual accounts were distilled into fixed categories for quantitative analyses.
-
▪ The selection of patients in contact with secondary services may have distorted the findings because patients not in contact with services may be less satisfied and differ more in their explanatory models.
Acknowledgements
We thank Dave Barker who was involved in discussions about the design of the study, Abigail Collinge and Funke Adetimole who assisted with the data collection, the clinicians who assisted in identifying possible participants and all of the participants who generously gave their time and made this study possible. This research was funded by the East London and the City Mental Health National Health Service Trust.








eLetters
No eLetters have been published for this article.