Following traumatic injury, people often experience adverse psychological consequences including post-traumatic stress disorder (PTSD) (Reference O'Donnell, Creamer and BryantO'Donnell et al, 2003), other psychological symptoms (Reference Mason, Wardrope and TurpinMason et al, 2002a ) and socio-economic consequences (Reference Mason, Wardrope and TurpinMason et al, 2002b ). Effective treatments (Reference Ehlers, Clark and HackmannEhlers et al, 2003; Reference Harvey, Bryant and TarrierHarvey et al, 2003) exist but access is often limited by the availability of therapists. Accordingly, attempts have been made at early or time-limited interventions (e.g. 'psychological debriefing') but these have received little empirical support (Reference Litz, Gray and BryantLitz et al, 2002; Reference BissonBisson, 2003; Reference McNally, Bryant and EhlersMcNally et al, 2003). Nevertheless, the development of secondary prevention methods is attractive and one possible approach is the provision of self-help information, such as that commonly available in accident and emergency (A&E) departments. The present study constitutes a randomised controlled trial designed to assess the efficacy of providing information booklets to patients serially attending an A&E department following physical injury.
METHOD
Patients
Over a 4-month period 2818 patients who attended A&E at the Northern General Hospital in Sheffield between August and November 2001 were invited by letter to participate in the study. Inclusion criteria were: age between 16 and 65 years and injuries sustained only as a result of a road traffic accident (RTA), occupational injury or assault. Patients were excluded if they were non-English speaking because of difficulties with the written self-report assessments.
Procedure
Approval was obtained from the North Sheffield Research Ethics Committee. In liaison with consultant medical staff, clerical staff identified those patients visiting A&E following an RTA, occupational injury or assault. Prior to contact, patients were checked to ensure that they met the inclusion criteria and were not too physically unstable to be approached for consent.
Patients were first contacted by letter, asked to read an information sheet, and if they agreed to take part in the study, to return the consent form in a prepaid envelope provided. Within 2 weeks of A&E attendance they were sent the first questionnaire designed to gather baseline demographic data and information about the accident. On return of this questionnaire, participants were assigned, using random number tables by a masked independent investigator, to either the intervention or control groups. Participants within the intervention group were sent a self-help booklet about emotional reactions to physical injury, within 6-8 weeks of their attendance. Participants in the control group were sent a letter without the patient information. Four weeks later all participants were sent a second questionnaire to assess differences in psychological outcome. A follow-up questionnaire was sent to both groups between 24 and 26 weeks following attendance. Control participants were offered a copy of the self-help booklet at the end of the study.
Self-help information booklet
The self-help information comprised a booklet (8 pages, 550 words) entitled 'Responses to traumatic injury' and was based on a leaflet developed by the Psychology Department at Harrogate District Hospital. In the leaflet, common physiological, psychological and behavioural reactions to traumatic injury are described and normalised. Advice regarding non-avoidance and emotional support is also given, together with information on seeking further help. The booklet was approved by the Northern General Hospital's Patient Information Group, which included a user representative, and had a Flesch-Kincaid reading age (determined through Microsoft Word) of 8 years, well below the ceiling of 12 years recommended for use in the National Health Service (NHS).
Measures
Questionnaires at baseline (2 weeks), post-intervention (10-12 weeks) and follow-up (24-26 weeks) included the self-report measures below, together with questions relating to demographic information and the nature of the injury. The main outcomes were assessed as the difference in the following measures between baseline and post-intervention functioning 10-12 weeks after the accident.
Post-Traumatic Diagnostic Scale
The Post-Traumatic Diagnostic Scale (PDS) was selected as the primary outcome measure and is designed to self-assess PTSD according to DSM-IV criteria (American Psychiatric Association, 1994). The scale has good agreement with the Structured Clinical Interview for Diagnosis (Reference Foa, Cashman and JayloxFoa et al, 1997). The PDS asks about difficulties experienced over the previous 4 weeks. However, the wording of the questionnaire at baseline was changed to reflect difficulties since the incident.
Hospital Anxiety and Depression Scale
The Hospital Anxiety and Depression Scale (HADS) was selected as a secondary outcome measure to reflect more general psychological sequelae and is widely used to assess levels of anxiety and depression (Reference Snaith and ZigmondSnaith & Zigmond, 1994).
At follow-up patients within the intervention group were asked whether they had read the booklet and to rate how useful they had found it; they were also given the opportunity to complete some open questions about their experiences.
Statistical analysis
Questionnaires were analysed using SPSS for Windows Version 11. Multivariate analyses of variance (MANOVAs) and analyses of variance (ANOVAs) were used to compare groups (control and intervention) for outcome measures across time intervals. All results were taken as significant at the level of P<0.05 employing two-tailed tests unless specified otherwise. Power analysis, using a previously observed (Reference Ehlers, Clark and HackmannEhlers et al, 2003) small effect size of 0.27 for change in the PDS following provision of an information booklet, indicated a total sample size of 120 would be sufficient for an alpha level of 0.05 and power of 0.80 (Erdfelder et al, Reference Erdfelder, Faul and Buchner1996). On the basis of previous research (Mason et al, Reference Mason, Wardrope and Turpin2002a , Reference Mason, Wardrope and Turpin b ) we had estimated attrition from the trial of around 30%. Both intention-to-treat and completer analyses were conducted. The former included all participants who consented as per the protocol, including some administrative drop-outs and those that reported that they had not read the booklet (baseline values were substituted at all subsequent points in the analysis for these participants). However, the results focus on those completing the analysis to obtain representative changes in outcome. Qualitative data from the open-ended questions asked at follow-up were analysed using content analysis (Reference PattonPatton, 1987), which involves identifying the frequency of themes within the data.
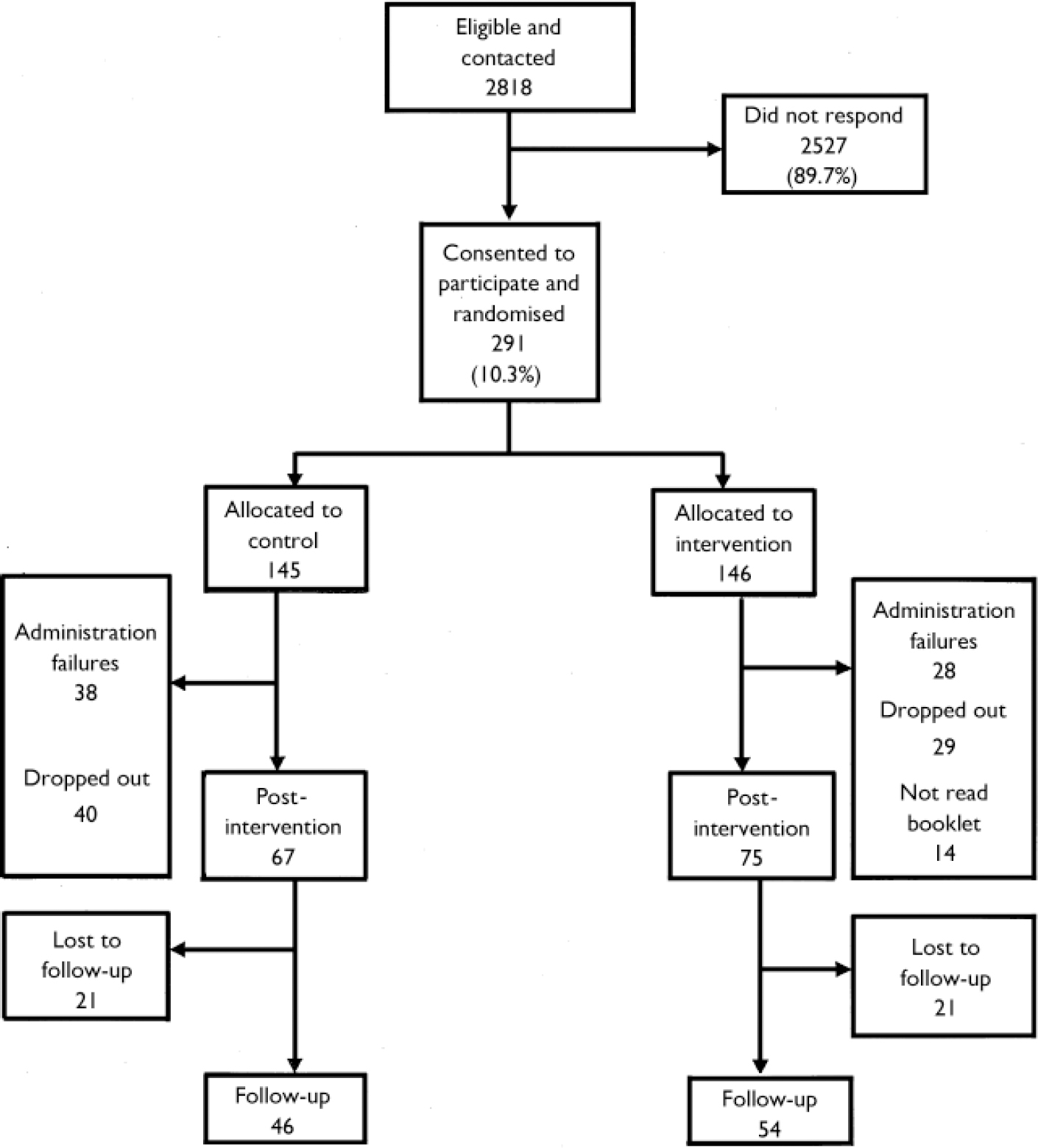
Fig. 1 Summary of trial.
RESULTS
Response rates
Of the 2818 patients who were eligible and invited to take part in the study, 291 (10.3%) consented to participate, completed the baseline questionnaire and were randomised into two groups. Of these, 222 (76.3%) completed questionnaires at baseline and post-intervention. However, 66 patients did not receive either the control letter or the booklet within the specified 6-8 weeks of their attendance at A&E, and were therefore removed from the analysis. This was owing to an early administrative failure in printing the booklet and letters, which was beyond the control of the researchers. Each arm of the trial was similarly affected. Fourteen patients from the intervention group reported that they had not read the booklet and were also removed from the study, reducing the final sample to 142. Of these, 100 (70.4%) returned their questionnaires at follow-up. These data are summarised in Fig. 1
Differences between non-responders, responders and those who dropped out
Differences between responders (n 291), non-responders (n=2527) and those who dropped out from the intervention (n=69) are summarised in Table 1.
Table 1 Characteristics of non-responders, responders and those who dropped out from intervention and follow-up
| Non-responders (n=2527) | Responders (n=291) | Dropped out at 6-8 weeks (n=69) | Dropped out from follow-up (n=42) | |
|---|---|---|---|---|
| Type of accident | ||||
| Assault | 753 (29.9%) | 67 (23.0%) | 21 (30.4%) | 10 (23.8%) |
| Occupational | 1074 (42.5%) | 103 (35.4%) | 21 (30.4%) | 16 (38.1%) |
| Road traffic accident | 700 (27.7%) | 121 (41.6%) | 27 (39.1%) | 16 (38.1%) |
| Age, mean (s.d.) | 33.07 (12.15) | 38.52 (11.20) | 33.58 (11.20) | 37.40 (11.47) |
| Gender | ||||
| Male | 1833 (72.5%) | 159 (54.6%) | 40 (58.0%) | 17 (40.5%) |
| Female | 693 (27.5%) | 132 (45.4%) | 29 (42.0%) | 25 (59.5%) |
At baseline, significant differences were found between responders (n 291) and non-responders (n 2527) for trauma type (χ2(2)=4.52, P<0.001) which resulted from a higher proportion of occupational injuries and assaults in the non-responders. Conversely, there were more RTAs among responders than non-responders. There was also a higher (w2(1) 40.62, P<0.001) proportion of males (72.5%) in the non-responders than the responders (54.6%). Non-responders were also significantly younger (t(2816)=5.44, P<0.001) than the responders (mean 33.07 v. 37.35 years; s.d.=12.15 v. 12.76). Post-intervention, the only difference (t(289) 2.841, P<0.001) between those remaining in the study and those who dropped out was age: those who dropped out were younger (mean=33.58, s.d. 11.20) than those who completed (mean=38.52, s.d.=11.20). A similar analysis comparing original responders with those who dropped out at follow-up revealed only a significant gender effect (χ2(1) 3.97, P<0.05), with more men remaining in the study.
No other significant differences were found between responders and those who dropped out with respect to accident type, gender, employment status, marital status or alcohol intake (P≥0.23). Similarly, a MANOVA and three 263 ANOVAs were employed to assess significant differences between responders and those who dropped out on measures of psychological disorder at baseline. Neither MANOVA (Wilks' lambda F(3,238)=0.99, P 0.68) nor separate ANOVAs revealed significant differences between responders and those who dropped out regarding symptom severity, (Fs(1,287)50.85, P>0.36).
Comparison of groups prior to intervention
Characteristics of the groups are presented in Table 2. The groups were compared using appropriate statistics, but as expected no differences were observed.
Table 2 Comparison of background variables and dimensions of trauma between intervention and control groups
| Intervention group (n=75) | Control group (n=67) | |
|---|---|---|
| Age (years) | ||
| Mean | 39.74 | 37.42 |
| Median | 40.00 | 35.00 |
| s.d. | 12.48 | 12.13 |
| Female gender | 34 (45%) | 36 (54%) |
| Employed | 65 (87%) | 50 (75%) |
| Marital status | ||
| Single | 22 (29%) | 27 (40%) |
| Married | 38 (51%) | 32 (48%) |
| Divorced/widowed | 15 (20%) | 8 (12%) |
| Trauma type | ||
| Assault | 12 (16%) | 16 (24%) |
| Occupational | 30 (40%) | 28 (42%) |
| Road traffic accident | 33 (44%) | 23 (34%) |
| Baseline symptoms | ||
| PDS, mean (s.d.) | 10.92 (11.50) | 9.61 (10.77) |
| HADS-A, mean (s.d.) | 6.81 (4.96) | 7.07 (4.20) |
| HADS-D, mean (s.d.) | 4.08 (4.54) | 3.84 (3.52) |
PDS, Post-Traumatic Diagnostic Scale; HADS, Hospital Anxiety and Depression Scale; A, anxiety; D, depression.
Effects of the intervention
The effect of providing an information booklet was assessed by comparing group differences across time, with relation to symptom severity for PTSD, anxiety and depression and the prevalence of clinical caseness. The primary outcome measure, however, was reduction in symptom severity in the PDS 4 weeks following the intervention. Initially, MANOVA was used to assess group differences in improvement scores (post-intervention7baseline) for symptom severity scores for PDS, anxiety and depression. No significant differences were found for either the analysis of those completing the study (Wilks' lambda F(3,138)=0.94, P=0.12) or intention-to-treat including just the non-readers (Wilks' lambda F(3,152)=0.97, P=0.18) or the total respondent sample (Wilks' lambda F(3,218)=0.98, P=0.19).
Given that the intervention might have differentially targeted the various outcome measures employed, with a greater emphasis on PTSD symptoms, individual univariate tests were also conducted comparing baseline and post intervention. Analysis of changes in PDS severity only revealed a time effect (F(1,140)=5.93, P<0.05), whereby scores decreased post-intervention (mean=10.30 v. 8.93, s.d.=11.14 v. 11.68), all other effects and interactions were not significant (P=0.57). The findings from the intention-to-treat analyses were all consistent, with time being the only significant effect. Across the 142 patients who completed, caseness for meeting criteria for PTSD according to the PDS was also assessed and yielded 44 (31%) at baseline. Post-intervention, only 21% of patients from the intervention group (5/24) had improved, whereas 50% from the control group (10/20) showed improvement and were no longer classified as having PTSD. This difference between the groups almost reached significance (χ2(1)=4.13, P=0.06).
The pattern of findings for anxiety and depression were similar to those described above. Significant time effects were found for reductions in caseness and severity for both anxiety (w2(1) 31, P<0.001; F(1,140)=5.29, P<0.05) and depression (w2(1)=32.58, P<0.001; F (1,140) 4.47, P=0.05). No significant differences between groups for anxiety or depression were obtained in either caseness (w2(1)=1.71 and 1.25, P>0.19) or severity (F(1,140)=0.84 and 0.70, P 0.73 and 0.40). No interactions were significant. Analyses based on intention-to-treat, which included all participants as per protocol, yielded an identical pattern of significant effects, with the exception of an almost significant group effect for depression (F(1,220)=3.76, P 0.054): the booklet group was more depressed (mean 4.88) than the control (mean=3.80).
Follow-up
A separate analysis of those patients (n=100) who completed questionnaires throughout the study and at follow-up revealed significant effects of time in symptom severity for PDS (F(1,98) 6.22, P<0.05) and for anxiety and depression (F(1,98)=2.83 and 3.35; P<0.05 respectively) but no group differences (P>0.5). There was also a significant interaction of group6time (F(1,98)=3.14, P<0.05) for depression, whereby severity decreased further in the control rather than in the intervention group. Caseness was assessed across the three time periods and between groups, using a 362 randomisation test (Reference Todman and DugardTodman & Dugard, 2001). The only significant effect was across time for anxiety (F(2)=3.57, P<0.05); all other main effects (P>0.21) and their interactions (P>0.13), were non-significant across all three measures. Changes in caseness and symptom severity across all three time periods are displayed in Table 3.
Table 3 PDS and HADS severity and caseness at baseline, post-intervention and follow-up
| Baseline(n=142) | Post-intervention(n=142) | Follow-up(n=100) 1 | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Severity | Caseness | Severity | Caseness | Severity | Caseness | ||||||||||||||||
| Mean | (s.d.) | n | (%) | Mean | (s.d.) | n | (%) | Mean | (s.d.) | n | (%) | ||||||||||
| Control (n=67) | |||||||||||||||||||||
| PDS | 10.02 | (11.50) | 20 | (14) | 9.26 | (12.43) | 10 | (7) | 7.80 | (10.61) | 10 | (10) | |||||||||
| HADS anxiety | 7.17 | (4.37) | 31 | (22) | 5.38 | (4.31) | 18 | (13) | 6.17 | (5.15) | 13 | (13) | |||||||||
| HADS depression | 3.96 | (3.52) | 9 | (6) | 3.11 | (3.82) | 10 | (7) | 2.80 | (2.80) | 7 | (7) | |||||||||
| Intervention (n=75) | |||||||||||||||||||||
| PDS | 10.15 | (11.30) | 24 | (17) | 8.83 | (10.93) | 19 | (13) | 8.33 | (10.91) | 14 | (14) | |||||||||
| HADS anxiety | 6.46 | (5.01) | 37 | (26) | 6.38 | (4.56) | 29 | (20) | 6.22 | (4.78) | 14 | (14) | |||||||||
| HADS depression | 4.17 | (4.75) | 17 | (12) | 4.22 | (4.48) | 15 | (11) | 4.15 | (2.80) | 18 | (18) | |||||||||
PDS, Post-Traumatic Diagnostic Scale; HADS, Hospital Anxiety and Depression Scale.
1. Forty-six in the control group completed the follow-up questionnaire and 54 in the intervention group.
Injury type
Additional subgroup analyses were conducted to assess whether the type of injury might have affected the outcome. A MANOVA comparing injury types for PTSD, anxiety and depression severity scores was significant (Wilks' lambda F(6,268)=0.83, P<0.001). However, univariate analyses revealed only significant time effects (P<0.04) for PDS and anxiety severity, irrespective of whether completer or intention-to-treat analyses were performed, and reflected a decline in scores. Depression revealed no significant effects. In order to adjust for the possible combined effects of injury type and associated PTSD severity on outcome, a series of analyses of covariance (ANCOVAs) was run using the baseline PDS score as the covariate against post-intervention outcomes for PTSD, anxiety and depression. None of these ANCOVAs was significant (F(1,139)=0.34, 1.57 and 0.48, P=0.56, 0.21 and 0.36, respectively). Similar analyses based on intention-to-treat analyses were also non-significant (P<0.59).
Patient perception of the self-help booklet
Out of 75 patients, 68 rated the usefulness of the booklet on a scale of 0 (not useful) to 5 (very useful), resulting in a mean rating of 2.98 (median=3, mode 4, range 5). Overall, 66% deemed the booklet useful. With respect to the content analysis, 38% of people completed the qualitative portion of the questionnaire. When asked what was particularly helpful, 16 people (47%) referred to information and advice and 11 people (32%) the normalisation of reactions.
DISCUSSION
This trial did not support the efficacy of routinely providing an educational booklet on psychological consequences of injury to A&E attenders. Patients in receipt of the booklet did not report either less severe or fewer symptoms of PTSD, anxiety or depression than those patients that did not receive the booklet. Indeed, some data suggested a trend for more patients who had originally met the criteria for PTSD at baseline to improve in the control group. Similarly, there was a suggestion that the control group showed greater improvement in depression scores over time. Nevertheless, over two-thirds of patients who received the booklet rated it as useful.
What can we conclude, therefore, about the utility of providing information to A&E attenders following injury? The provision of self-help materials is strongly advocated within the NHS as a means of informing patients of their condition and its treatment (Department of Health, 2001; King's Fund, 2003). Moreover, psychoeducation generally is said to have proven efficacy (e.g. Reference Gould and ClumGould & Clum, 1993). In contrast, these data argue against the provision of information and suggest that providing information may not only be ineffective but may even have a detrimental effect. Such a conclusion is consistent with previous reviews of other early interventions such as debriefing (e.g. Reference BissonBisson, 2003) and resonate with authors who have warned of the dangers of sensitising trauma victims and disrupting the natural recovery process (Reference Herbert, Sageman and RosenHerbert & Sageman, 2004). We suggest, however, a degree of caution in reaching both these conclusions given that this is the first systematic study to specifically assess the efficacy of provision of information.
How generalisable was the trial?
What would argue against the conclusion that provision of information is ineffective? First, we need to assess whether the current trial recruited a sample sufficiently representative of A&E attenders. Unfortunately, only around 10% of eligible patients consented to participate in the trial. This reluctance to participate may reflect previously reported low uptake rates and high attrition for traumatised populations accessing therapy (Reference Rose, Brewin and AndrewsRose et al, 1999; Reference WeisaethWeisaeth, 2001). Even so, this does not necessarily indicate that A&E attenders would not utilise routinely provided information but may reflect a reluctance to volunteer for research. Were those recruited characteristic of the overall population of A&E attenders? Analysis of trial responders and non-responders did
indicate some differences; participants were more likely to have been injured in RTAs, whereas non-participants were more likely to be male and younger, and have received occupational injuries. Those who dropped out from follow-up were more likely to be women. These data are generally consistent with patterns of recruitment and dropout in our previous research (Mason et al, Reference Mason, Wardrope and Turpin2002a , Reference Mason, Wardrope and Turpin b ) but may also reflect the acceptability of an information leaflet to these different groups of A&E attenders. Given the wide variation in the prevalence of PTSD following injury (Reference O'Donnell, Creamer and BryantO'Donnell et al, 2003), however, it is difficult to conclude that the trial sample was not generally representative of A&E samples.
How sensitive was the trial?
Although there were some differences between participants and non-participants, the random allocation to the two trial groups was successful; neither the individual groups nor those who dropped out of the trial differed substantially. The retention rates for the trial participants was 76.3% post-intervention and 70.4% at follow-up which compare reasonably with rates for other trials involving brief psychological interventions. It is unlikely, therefore, that overall group characteristics might have accounted for the lack of significant effects of the intervention. Similarly, the sample sizes ought to have had sufficient statistical power to demonstrate a medium effect size for the primary outcome measure. Indeed, significant improvements in symptom severity and associated reductions in caseness were obtained across time, but no overall group differences were obtained. Some individual group differences did emerge but these were the opposite direction to that hypothesised. The control group behaved differently to the intervention group post-intervention with a trend towards lower PTSD caseness and depression severity. Similarly, although there were no overall group differences at follow-up, the control group again showed a significant decrease in depression. Taken together, these effects suggest greater improvement within the control group. However, it should be recognised that these apparently detrimental effects require replication to rule out the possibility of type 1 errors arising from multiple outcome assessments.
Relationship to other early intervention studies
If we conclude that the current trial fails to provide support for the use of patient information, how does this relate to existing literature? As we have already indicated, reviews of psychological debriefing have stressed negative or contraindicative results. In contrast, some recent studies (Reference Litz, Gray and BryantLitz et al, 2002; Reference Ehlers, Clark and HackmannEhlers et al, 2003; Reference Bisson, Shepherd and JoyBisson et al, 2004) of targeted, early cognitive-behavioural interventions have suggested more promising results. Ehlers et al (Reference Ehlers, Clark and Hackmann2003) employed an information booklet as a control condition but failed to demonstrate any significant effects compared with an assessment-only control. A similar lack of effect of education compared with either assessment only or a debriefing and education condition was also observed by Rose et al (Reference Rose, Brewin and Andrews1999). O'Donnell and colleagues assessed the provision of a more extensive psychoeducational booklet to patients attending a regional trauma centre (M. Creamer, personal communication, 2005). They found that those who had received the booklet reported less deterioration in quality of life and a non-significant increase in symptoms compared with those who did not receive a booklet. Finally, very high levels of patient satisfaction have been reported (Reference Robertson, Klein and BullenRobertson et al, 2002) for a similar self-help booklet, but unfortunately the efficacy of the leaflet in reducing symptoms was not investigated. It would appear therefore that other researchers have also failed to obtain convincing evidence of the efficacy of self-help information when used in isolation.
Need for future research
Before we finally conclude the ineffectiveness of information provision, we must consider some further questions. Many have argued (Reference Litz, Gray and BryantLitz et al, 2002; Reference Ehlers and ClarkEhlers & Clark, 2003) that early interventions ought to be targeted at those patients who are unable to recover naturally from trauma. This can be achieved either by a 'stepped care' approach, whereby interventions are delayed until a time from the injury when the recovery process ought to be complete (e.g. 6 months) and then identifying patients who are still symptomatic, or by employing predictors of later PTSD. Future research, therefore, might determine whether psychoeducation is more efficacious when it is more effectively targeted at those in need. Unfortunately, the results of a recently completed psychoeducation study with A&E patients identified on the basis of acute stress disorder has also failed to demonstrate any efficacy of self-help provision (Reference ScholesScholes, 2004).
It may also be the case that the content of the information booklet was not sufficient. Researchers (Reference Rosen, Glasgow, Moore, Lilienfield, Lynn and LohrRosen et al, 2003) have stressed the limitations of self-help approaches to psychological problems. More specifically it has been suggested (Reference Litz, Gray and BryantLitz et al, 2002) that information for trauma ought to be more action-orientated, encouraging patients to reduce avoidance and confront their traumatic memories, and should emphasise the importance of cognitive restructuring and social support. The current booklet was more an information than a detailed self-help guide but a recent study of a more extensive guide again failed to obtain differences (Reference ScholesScholes, 2004).
Finally, a particularly important issue regarding effective treatment of chronic PTSD is early diagnosis and encouragement of trauma victims to present later for treatment within primary care settings. Indeed, recent guidance (National Collaborating Centre for Mental Health, 2005) suggests 'watchful waiting' and follow-up assessments 4 weeks after trauma to establish whether adverse psychological effects have been exacerbated or failed to dissipate. However, the interface between emergency and primary care is by its very nature sporadic and unsystematic. Moreover, there are resource implications and an accompanying reluctance in primary care to routinely screen for PTSD following traumatic events or attendance at A&E departments. This might effectively place responsibility for seeking subsequent treatment very much with the patient; information booklets which are considered helpful have an important role in prompting patients at risk for chronic PTSD to seek future treatment, if their initial psychological disturbance is not resolved during the recovery period.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ The provision of information leaflets to patients recovering from traumatic injury fails to reduce the severity or incidence of future symptoms of post-traumatic stress disorder.
-
▪ Patients not receiving this information reported less depression following injury.
-
▪ Nevertheless, booklets were perceived as helpful and may have a role in prompting patients to seek future treatment if initial problems are unresolved.
LIMITATIONS
-
▪ Outcomes were assessed by survey and self-report, direct interviews were not feasible.
-
▪ The sample represented only a relatively small proportion of accident and emergency attenders and they were not selected for the impact of the injury on initial psychological well-being.
-
▪ Greater efficacy might be influenced by the provision of more timely or detailed and 'action-orientated' advice about recovery from trauma.
Acknowledgements
The research reported was completed in partial fulfilment of a DClinPsy, University of Sheffield. We would like to acknowledge the invaluable statistical advice of Adrian Simpson. Financial assistance was provided by a British Association for Accident and Emergency Medicine Research Grant. Copies of the information booklet are available from the authors on request.







eLetters
No eLetters have been published for this article.