Extrapyramidal symptoms are the most common reason for non-adherence to schizophrenia treatment, leading to treatment failures and preventable morbidity, mortality and economic costs (Reference KnappKnapp, 1997; Reference Lindstrom and BingeforsLindstrom & Bingefors, 2000). The majority of studies reporting that atypical antipsychotics are less likely to cause extrapyramidal symptoms than typical antipsychotics are clinical trials (Reference Tran, Tollefson and SangerTran et al, 1999; Reference Bouchard, Merette and PourcherBouchard et al, 2000; Reference Costa e Silva, Alvarez and MazzottiCosta e Silva et al, 2001; Reference Inada, Yagi and MiuraInada et al, 2001; Reference Ritchie, Chiu and HarriganRitchie et al, 2003). However, those with schizophrenia have a high degree of comorbidity (Reference Buckley, Miller and ChilesBuckley et al, 1999) and low adherence rates (Reference Lindstrom and BingeforsLindstrom & Bingefors, 2000), which are often not reflected in clinical trials, but have an important influence on treatment outcome. Observational studies have not evaluated the long-term effectiveness of antipsychotics on extrapyramidal symptoms (Reference Bobes, Gibert and CiudadBobes et al, 2003; Reference Montes, Ciudad and GasconMontes et al, 2003; Reference Soholm and LublinSoholm & Lublin, 2003), although antipsychotics are generally used indefinitely. Most observational studies have included only in-patients (Reference Coley, Carter and DaPosColey et al, 1999; Reference Barak, Shamir and WeizmanBarak et al, 2002; Reference Bobes, Gibert and CiudadBobes et al, 2003; Reference Soholm and LublinSoholm & Lublin, 2003), but many chronically ill individuals with schizophrenia receive maintenance pharmacotherapy in primary care (Reference Lang, Johnstone and MurrayLang et al, 1997; Reference FreedmanFreedman, 2003). This study evaluates the use of antiparkinsonian medication before and after switching antipsychotics in a community population of individuals with schizophrenia in UK general practices.
METHOD
Data
Data were extracted from the General Practice Research Database (GPRD) in the UK. This is a computerised database of anonymised patient data that contains approximately 30 million patient-years of information. The GPRD has been collecting patient records in the UK continuously since 1987. Currently, the database collects information on approximately 3 million patients, equivalent to approximately 4.7% of the UK population. Data are provided by contributing general practices from all around the UK. The information recorded by general practitioners includes demographics, medical diagnosis, all prescriptions, referrals to hospitals and treatment outcomes, including hospital discharge reports where individuals have been referred to hospital for treatment. The high quality and completeness of these data for research have been confirmed (Reference Walley and MantganiWalley & Mantgani, 1997).
Study group
We studied 6356 individuals from 266 general practices who had been diagnosed with schizophrenia and prescribed antipsychotics between 1992 and 2000. Schizophrenia diagnoses were derived from the records of out-patient contacts with general practitioners. We focused on those who had been switched from typical to atypical antipsychotics (TA group) or from typical to different typical antipsychotics (TT group) between 1994 and 1998, and who were present in the database for at least 2 years before and after the switch. Only those who were diagnosed with schizophrenia at least 2 years before the switch were evaluated. We defined the TA group as those who had been prescribed typical antipsychotics before the switch, completely stopped typical antipsychotics and subsequently switched to atypical antipsychotics, with no typical antipsychotic use for at least 2 years after the switch. The TT group included patients who were prescribed one typical antipsychotic (e.g. chlorpromazine) and then switched to a different typical antipsychotic (e.g. haloperidol), and who never received an atypical antipsychotic. The analysis included 209 in the TA group and 261 in the TT group.
Because risperidone and olanzapine were the most commonly prescribed (87%) atypical antipsychotics after the switch in the TA group, we also focused on those within that group who had been switched from typical antipsychotics to either of these two atypical antipsychotics. Using the same inclusion criteria as above, we defined the risperidone, TAR (or olanzapine, TAO) recipients as those who had been prescribed typical antipsychotics with no atypical antipsychotics before the switch, and then switched to either risperidone or olanzapine between 1994 and 1998, with no typical antipsychotic or other atypical antipsychotics for at least 2 years after the switch. Thus, 87 risperidone and 78 olanzapine recipients were studied.
Outcome measures
First we examined the antipsychotic prescribing rates yearly between 1992 and 2000, calculated as the number with schizophrenia prescribed antipsychotics divided by the number of all those with schizophrenia each year, adjusted for age (≤39, 40-64, ≥65 years) and gender. Then we examined the annual percentage of those prescribed either typical or atypical antipsychotics among those prescribed antipsychotics.
We measured rates of prescribing for antiparkinsonian drugs quarterly for 2 years before and after the switch, by switching group. We regarded prescribing of antiparkinsonian drugs (including benztropine, biperidine, orphenadrine, procyclidine and trihexyphenidyl) as indication of treatment of extrapyramidal symptoms. This has frequently been used in previous studies (Reference Tran, Tollefson and SangerTran et al, 1999; Reference Costa e Silva, Alvarez and MazzottiCosta e Silva et al, 2001; Reference Inada, Yagi and MiuraInada et al, 2001; Reference Bobes, Gibert and CiudadBobes et al, 2003; Reference Montes, Ciudad and GasconMontes et al, 2003), and the use of antiparkinsonian medication is highly correlated with clinical indices of extrapyramidal symptoms (Reference Costa e Silva, Alvarez and MazzottiCosta e Silva et al, 2001; Reference Inada, Yagi and MiuraInada et al, 2001; Reference Bobes, Gibert and CiudadBobes et al, 2003; Reference Montes, Ciudad and GasconMontes et al, 2003). The antiparkinsonian drug prescribing rate was calculated as the number of individuals during an observation period who were prescribed an antiparkinsonian drug divided by the number in each switching group. We adjusted gender and age to the combined study population at the time of switching. Because individuals switched at different times, the quarter when the switch occurred was treated as the start of the follow-up period (‘point 0’).
We also examined the mean daily dose of antiparkinsonian drugs prescribed for 2 years before and after switching. We analysed only tablets and capsules, which accounted for 98% of all antiparkinsonian drug prescriptions. Daily dose was estimated by dividing total dose by duration of antiparkinsonian medication use before and after the switch. Only the TA and TT groups were investigated because of the small sample sizes for the two subgroups.
Statistical analyses
We conducted interrupted time series analyses to estimate changes in the rates of prescribing of antiparkinsonian drugs after drug switching, controlling for the trend before the switch (SAS Institute, 2000a ; Reference Wagner, Soumerai and ZhangWagner et al, 2002). Our models included the trend in the rate of antiparkinsonian drug prescribing before the switch, and changes in the trend and level of antiparkinsonian drug prescribing after switching. The switch point quarter (point 0) was excluded from analyses because it was not clear whether the outcome in that quarter resulted from antipsychotics used before or after switching. We used t-tests to compare the mean daily dose of antiparkinsonian drugs before and after the switch (SAS Institute, 2000b ).
We used SAS Version 8.2 for all statistical analyses. All statistical analyses were performed separately for each group.
RESULTS
Patient characteristics
Table 1 summarises the characteristics of the study population. Those in the TA group were more likely to be male, whereas those in the TT group were more likely to be female (χ2=8.54, d.f.=1, P=0.004). Mean age of the TT group was higher than the TA group (t= -3.25, d.f.=468, P=0.001). There were no statistically significant differences in gender and age between those switching to risperidone or olanzapine.
Table 1 Characteristics of the study population

| Characteristic | All individuals (n=6356) | TA group (n=209) | TT group (n=261) | P (TA v. TT) | TAR group (n=87) | TAO group (n=78) | P (TAR v. TAO) |
|---|---|---|---|---|---|---|---|
| Age range (%) | |||||||
| ≤39 years | 36.7 | 39.2 | 30.3 | 37.9 | 43.6 | ||
| 40-64 years | 43.1 | 47.4 | 47.9 | 43.7 | 46.1 | ||
| ≥65 years | 20.2 | 13.4 | 21.8 | 18.4 | 10.3 | ||
| Age: mean (s.d.) | 48.6 (17.4)1 | 45.7 (14.7)2 | 50.4 (16.2)2 | 0.001 | 46.8 (16.3)2 | 44.4 (13.2)2 | 0.304 |
| Gender (%) | |||||||
| Male | 56.8 | 60.3 | 46.7 | 55.2 | 67.9 | ||
| Female | 43.2 | 39.7 | 53.3 | 0.004 | 44.8 | 32.1 | 0.093 |
| Co-medication (%)3 | |||||||
| Psychoactive drugs | 54.4 | 52.6 | 54.0 | 0.764 | 48.3 | 55.1 | 0.379 |
| Non-psychoactive drugs | 76.5 | 76.1 | 75.9 | 0.957 | 77.0 | 73.1 | 0.559 |
Individuals in the TT and the TA groups were equally likely to be co-prescribed other medications when prescribed antipsychotics prior to switching, including both psychoactive drugs (54.0% v. 52.6%) and other non-psychoactive drugs (75.9% v. 76.1%). There were also no significant differences in baseline rates of use of psychoactive and non-psychoactive medicines among those switched to risperidone v. olanzapine.
Overall use of antipsychotics
The adjusted average rate of antipsychotic prescribing between 1992 and 2000 was 80%, with a range of 78-82%. Of those prescribed antipsychotics, 47% were prescribed atypical antipsychotics in 2000, increasing from 3% in 1992. The percentage of those prescribed typical antipsychotics declined from 99% in 1992 to 70% in 2000.
Effect of switching on antiparkinsonian medication use
Figure 1 presents prescribing rates for antiparkinsonian drugs 2 years before and after the switch in the TA and TT groups. Controlling for baseline trends in the time series analysis, switching from typical to atypical antipsychotics was associated with a sudden drop by 9.2% in the antiparkinsonian drug prescribing rate (t= -6.10, d.f.=1, P<0.0001) and a decreased trend of 0.5% per quarter thereafter (t= -2.52), d.f.=1, P=0.027). In contrast, when individuals were switched from one typical antipsychotic to another, the switch was followed by a sudden increase in the rate of use of antiparkinsonian medication by 12.9% (t=13.34, d.f.=1, P=0.0001), but the rate decreased by 0.7% per quarter thereafter (t= -5.09, d.f.=1, P=0.0003).
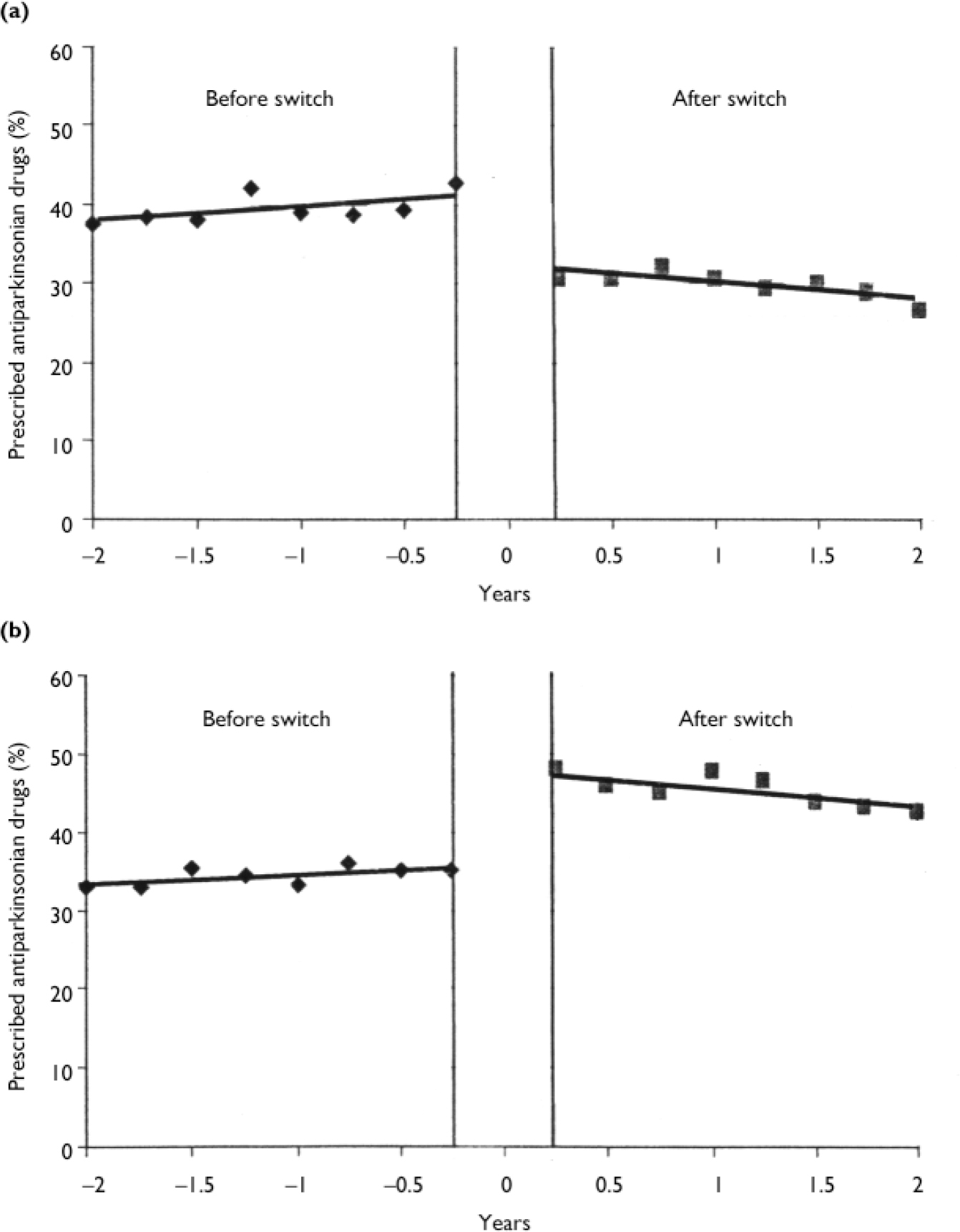
Fig. 1 Rates of antiparkinsonian drug prescribing before and after switching (a) from typical to atypical antipsychotics (n=209) and (b) from typical to different typical antipsychotics (n=261).
The mean daily doses of antiparkinsonian medication, calculated in benztropine equivalents, were not different before and after switching in either group (TA group: 1.87 mg/day before, 1.75 mg/day after, t= -0.74, d.f.=181, P=0.462; TT group: 1.97 mg/day before, 1.86 mg/day after, t= -0.77, d.f.=248, P=0.441).
Figure 2 presents antiparkinsonian drug prescribing rates before and after switching from typical antipsychotics to risperidone or olanzapine. Average daily prescribed doses of risperidone and olanzapine were 6.4 mg (s.d. 5.4 mg) and 12.2 mg (s.d.=6.2 mg) respectively, which were in the optimal dose range (Reference Tran, Hamilton and KuntzTran et al, 1997). There were no changes either in the level or in the trend of antiparkinsonian drug prescribing rate associated with the switch to risperidone. The switch to olanzapine caused a sudden drop in the rate of use of antiparkinsonian medication by 19.2% (t= -7.13, d.f.=1, P<0.0001) and a gradual decline by 1.5% per quarter thereafter (t= -3.84, d.f.=1, P=0.002).
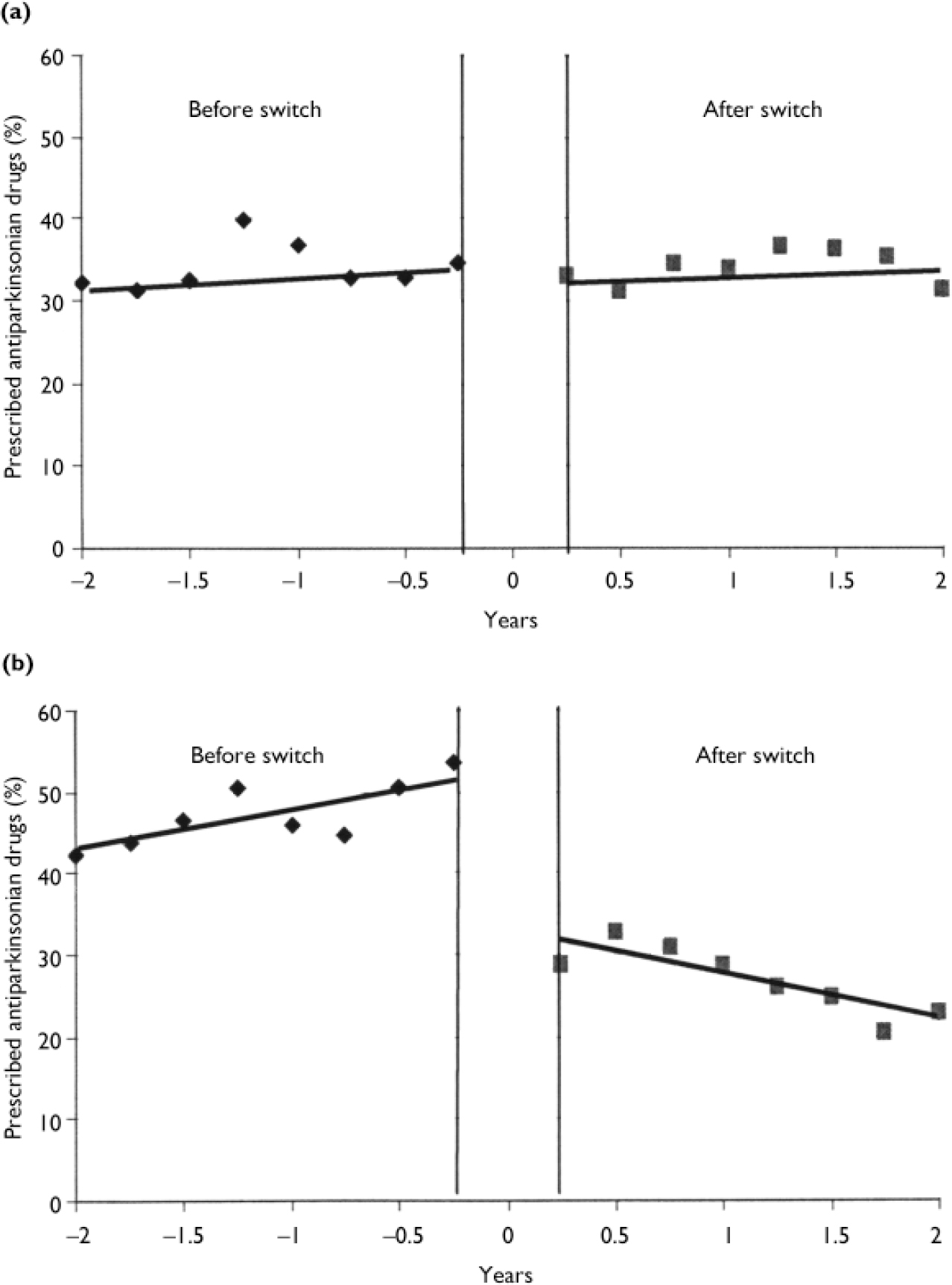
Fig. 2 Rates of antiparkinsonian drug prescribing before and after switching from typical antipsychotics to (a) risperidone (n=87) and (b) olanzapine (n=78).
DISCUSSION
Using a longitudinal database of community-based individuals with schizophrenia, we examined the effect of switching antipsychotics on treatment of extrapyramidal symptoms with antiparkinsonian medications. Antiparkinsonian drug prescribing dropped immediately after switching from typical to atypical antipsychotics and continued to decrease slightly thereafter. Although individuals were not randomised, this result confirms the findings of previous clinical studies that atypical antipsychotics are associated with a significantly lower incidence of extrapyramidal symptoms and with a lower use of antiparkinsonian medication than are typical antipsychotics (Reference Tran, Tollefson and SangerTran et al, 1999; Reference Bouchard, Merette and PourcherBouchard et al, 2000; Reference Costa e Silva, Alvarez and MazzottiCosta e Silva et al, 2001; Reference Inada, Yagi and MiuraInada et al, 2001; Reference Ritchie, Chiu and HarriganRitchie et al, 2003). In those who switched within the class of typical antipsychotics, antiparkinsonian drug prescribing increased immediately after the switch, but gradually decreased for 2 years thereafter. This suggests that physicians might have prescribed antiparkinsonian drugs for prophylactic control of extrapyramidal symptoms when they started to prescribe different typical antipsychotics.
The reduction in use of antiparkinsonian medication was not evenly distributed among different atypical antipsychotics. Switching from typical agents to olanzapine resulted in an abrupt decrease in the use of antiparkinsonian medication, whereas switching to risperidone caused no change in rate. Previous studies have reported the superiority of olanzapine over risperidone in reducing extrapyramidal symptoms (Reference Tran, Hamilton and KuntzTran et al, 1997; Reference Montes, Ciudad and GasconMontes et al, 2003; Reference Soholm and LublinSoholm & Lublin, 2003). Because of the difference in baseline trends in use of antiparkinsonian medication in our study, it is necessary to be cautious regarding comparison of the effectiveness of olanzapine and risperidone in reducing extrapyramidal symptoms (Fig. 2). Specifically, physicians may have been more likely to prescribe olanzapine for those with a higher prevalence of extrapyramidal symptoms since this drug was launched with clinical data supporting its advantage over risperidone in lowering the risk of these symptoms (Reference Tran, Hamilton and KuntzTran et al, 1997). Nevertheless, olanzapine may have a lower risk of extrapyramidal symptoms than risperidone based on the large differences in the observed rates of reduction in use of antiparkinsonian agents between those initiated on olanzapine and risperidone.
Switching to atypical antipsychotics did not change the average daily dose of antiparkinsonian drugs among those prescribed these medications. This implies that switching to atypical antipsychotics may not have mitigated the severity of extrapyramidal symptoms among those continuing to receive antiparkinsonian medications despite the overall reductions in the rate of antiparkinsonian drug use. Those with milder extrapyramidal symptoms may be more likely to have discontinued antiparkinsonian therapy after switching to atypical antipsychotics. For example, among individuals in the TA group who received lower than the median daily dose of antiparkinsonian agents before switching to atypical antipsychotics, 42% discontinued antiparkinsonian medication after the switch, compared with a discontinuation rate of 27% among those in the group who received higher than the median daily dose of antiparkinsonian drugs before switching. However, for some it is possible that the antiparkinsonian medication was simply neglected, leading to no change in dose.
Comparison with clinical trials
In this study, the effect of switching to olanzapine on the treatment of extrapyramidal symptoms was not as large as in clinical trials (Reference Costa e Silva, Alvarez and MazzottiCosta e Silva et al, 2001). Moreover, the daily dose of antiparkinsonian medication did not decrease after switching to atypical antipsychotics in the community, which contrasts with findings from previous clinical studies that daily doses of antiparkinsonian medication were lower in those using atypical antipsychotics than those using typical antipsychotics (Reference Tran, Tollefson and SangerTran et al, 1999; Reference Costa e Silva, Alvarez and MazzottiCosta e Silva et al, 2001; Reference Inada, Yagi and MiuraInada et al, 2001).
These differences might result from differences in study design. Participants in the clinical trials were typically younger and the observation periods were shorter than ours. Typical antipsychotics only included haloperidol, a high-potency antipsychotic with a high risk of extrapyramidal symptoms, which accounted for less than 10% of typical antipsychotic use in our study.
Another possible explanation for the differences is the poor adherence of those in the community compared with those in the controlled environments of clinical trials. In addition, physician prescribing in community settings might be more susceptible to other factors such as patient demand, pharmaceutical marketing and resulting physicians' perceptions of benefits and risks of specific medications.
Limitations
As the design of this observational study did not include randomisation, groups might have differed in demographic characteristics, severity and duration of disease, or treatment course. For example, those switching within typical antipsychotics were older and more likely to be female than those switching from typical to atypical antipsychotics. The use of low-potency typical antipsychotics with a low incidence of extrapyramidal symptoms was higher in the TT group (27%) than in the TA group (19%) before switching. Thus, it is difficult to compare the effect of switching between groups, even though age and gender were adjusted for in our analyses. Nevertheless, our results are valid within groups since we observed the same individuals over 4 years.
Those who switched medications might also have been different from those who remained on the same treatment. In additional analyses of those who received new prescriptions for antipsychotics and did not switch therapy, rates of antiparkinsonian drug prescribing were 10% lower among new atypical antipsychotic users compared with rates observed after switching to atypical antipsychotics, whereas the rates in new recipients of typical antipsychotics were not different from rates observed before switching to atypical antipsychotics. Those who had been switched seemed more likely to be prescribed antiparkinsonian drugs than those who had not been switched, even though they commonly used atypical antipsychotics.
In addition, switching might have resulted from several factors, including side-effects or lack of efficacy. Our data do not permit evaluation of the reasons for switching, which might differ between patient groups. For example, the prescribing of high-potency typical antipsychotics (e.g. haloperidol) with a high incidence of extrapyramidal symptoms increased after switching between two typical antipsychotic agents (from 36% before switching to 42% after switching). Some of this switching between typical antipsychotics is likely to have been caused by reasons other than extrapyramidal symptoms. Therefore, we cannot infer the appropriateness of switching based only on the change in the rate of antiparkinsonian prescribing.
Our results from those who switched antipsychotics in primary care might not be generalisable to all people with schizophrenia. However, the well-integrated healthcare delivery system in the UK might enable general practitioners to collaborate with specialists and follow their recommendations. Of those who switched antipsychotics in this study, 14% had been referred to specialists during the 6-month period before switching, whereas only 5% had been referred between 6 months and 1 year before switching. This suggests that some switches in this study might have reflected specialists' recommendations.
We measured antiparkinsonian drug prescribing to assess the effect of switching on treatment of extrapyramidal symptoms. Although antiparkinsonian drug prescribing has been used in previous studies to assess extrapyramidal symptoms (Reference Tran, Tollefson and SangerTran et al, 1999; Reference Costa e Silva, Alvarez and MazzottiCosta e Silva et al, 2001; Reference Inada, Yagi and MiuraInada et al, 2001; Reference Bobes, Gibert and CiudadBobes et al, 2003; Reference Montes, Ciudad and GasconMontes et al, 2003), it is only a marker and cannot accurately reflect their incidence. Moreover, our data did not permit us to ascertain whether clinical tests of extrapyramidal symptoms were performed before prescription of antiparkinsonian drugs. Their prescription might also have been influenced by practice variables or environmental factors. The results of this study should be interpreted in the light of these limitations.
Our study recorded prescribing, not dispensing. Drugs recorded might not have been dispensed or taken by patients. This should also be considered in the interpretation of results.
Finally, we cannot exclude the possibility that some individuals might have been prescribed antiparkinsonian medications because they had Parkinson's disease, not because they had extrapyramidal symptoms caused by antipsychotics. However, we do not have data on the prevalence of Parkinson's disease in the study population.
Implications
This study investigated changes in the use of antiparkinsonian medication after switching antipsychotics. We found that the magnitude of the effects of switching from typical to atypical antipsychotics on reducing antiparkinsonian medication use was considerable in community practices, but not as large as the effects observed in clinical trials. The effects of switching antipsychotics on antiparkinsonian medication use also varied substantially between risperidone and olanzapine. The differences between specific atypical agents as well as between typical and atypical antipsychotics should be considered in treatment decisions and policies concerning antipsychotic use (Reference TammingaTamminga, 2003). Several US Medicaid programmes require individuals to undergo a trial of use of the lowest-cost atypical antipsychotic before approval of more expensive agents, which may not lead to optimum control of extrapyramidal symptoms (Reference SoumeraiSoumerai, 2004). Further research is needed on the relationship between extra-pyramidal symptoms and treatment adherence and the quality of life of those with schizophrenia, as well as on clinical outcomes of cost containment policies that restrict access to specific antipsychotic agents.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ The magnitude of reduction of use of antiparkinsonian medication after switching from typical to atypical antipsychotics in community practice was not as large as in clinical trials.
-
▪ There were substantial differences in rates of use of antiparkinsonian medication with different atypical agents.
-
▪ The differences between specific atypical agents as well as between typical and atypical antipsychotics should be considered in treatment decisions and policies concerning antipsychotic use.
LIMITATIONS
-
▪ Antiparkinsonian medication use is only a marker of extrapyramidal symptoms and results should be interpreted considering this limitation.
-
▪ The study population is from general practice, which might not represent all people with schizophrenia.
-
▪ We should be cautious in comparing the effects of switching between groups because this was not a randomised controlled trial.
Acknowledgements
We thank Fang Zhang for advice on statistical analysis. We acknowledge the UK Medicines and Healthcare Products Regulatory Agency (MHRA), which allowed the use of the GPRD database. S.P. was a Fellow in Pharmaceutical Policy at Harvard Medical School when this work was completed. D.R.-D. and S.B.S. are investigators in the Health Maintenance Organization Research Network Center for Education and Research in Therapeutics, which is supported by a grant from the US Agency for Healthcare Research and Quality (grant No. U18HS1039-01). This work was also supported by the Harvard Pilgrim Health Care Foundation.






eLetters
No eLetters have been published for this article.