Attempts have been made to prevent the development of post-traumatic stress disorder (PTSD) and other psychiatric disorders by providing psychological interventions shortly after major traumatic events. A Cochrane systematic review of randomised controlled trials of early single-session psychological interventions that involved some reliving of the traumatic experience compared with no intervention found no effect on subsequent psychological distress despite being well received by a majority of participants (Reference Rose, Bisson and WesselyRose et al, 2001). More complex early psychological interventions using cognitive–behavioural methods have provided more positive preliminary results (Reference André, Lelord and LégeronAndré et al, 1997; Bryant et al, Reference Bryant, Harvey and Dang1998, Reference Bryant, Sackville and Dang1999). This and the effectiveness of exposure therapy and cognitive therapy in the treatment of established PTSD (Reference ShermanSherman, 1998) led us to develop a four-session early intervention that included elements of exposure therapy and cognitive restructuring. This study was designed to test the hypothesis that the intervention would reduce symptoms of PTSD after physical injury and to identify factors that predict PTSD after physical injury.
METHOD
Participants were recruited through the Accident and Emergency Unit of the Cardiff Royal Infirmary, Wales, UK, between 1 March 1997 and 28 February 1998 following ethics committee approval. Individuals who appeared to satisfy the study inclusion criteria were sent a description of the study and were contacted by telephone 1 week after their physical injury by a research psychologist. Eligible and interested individuals were sent an information sheet that described the study, questionnaires and consent forms to be returned within 3 weeks of their injury. If no response was received, a reminder was sent.
Study entry criteria
The study entry criteria were: physically injured (e.g. in a motor vehicle accident, assault or industrial accident); local home address; aged between 16 and 70 years; no pre-existing major psychiatric disorder; no major physical disability or illness reported; no evidence of cognitive deficit; evidence of acute psychological distress on the three self-report questionnaires as determined by fulfilment of DSM–IV (American Psychiatric Association, 1994) PTSD symptom criteria on the PTSD Diagnostic Scale (Reference Foa, Riggs and DancuFoa et al, 1993), a score of >15 on the anxiety or depression sub-scale of the Hospital Anxiety and Depression Scale (HADS; Reference Zigmond and SnaithZigmond & Snaith, 1983) or a score of >35 on the Impact of Event Scale (IES; Reference Horowitz, Wilner and AlvarezHorowitz et al, 1979).
Design
The study was a randomised controlled trial in which standard care only (the control condition that involved no formal psychosocial intervention) was compared with standard care plus the four-session cognitive–behavioural intervention. A placebo intervention condition was not used to control for non-specific intervention effects, given the previous neutral and negative findings with one-off interventions (Reference Rose, Bisson and WesselyRose et al, 2001). The primary outcome measure was the change in IES score from baseline at 3 and 13 months after injury. Secondary outcome measures were a change in HADS scores and the total score on the clinician-administered PTSD Diagnostic Scale (Reference Blake, Weathers and NagyBlake et al, 1990) at 3 and 13 months after injury. All of these scales have been widely used in trauma research and have been shown to have strong psychometric properties.
Randomisation
Following study entry, participants were allocated randomly either to the intervention group or to standard care only (control) group. Randomisation codes were generated by computer in random-sized blocks of four and six participants to ensure equal-sized groups. Codes were written on cards and sealed in opaque envelopes to conceal their contents from the research psychologist prior to opening.
Intervention
The intervention consisted of four 1-hour weekly sessions between 5 and 10 weeks after the physical injury. They were administered by a research psychologist (R.P.), fully trained and supervised in the intervention by J.I.B. Intervention fidelity was ensured in two ways. The intervention was defined in detail in an intervention manual and 16 sessions were selected randomly for audio-recording. J.I.B. listened to the tapes and checked their content against the instructions contained in the manual. The tapes confirmed that the intervention was being delivered according to the instruction manual.
During the intervention, participants were educated regarding the stress response to injury. They were then encouraged to describe the traumatic incident in detail, in the first person present tense, including thoughts, feelings, sights, smells, noises, emotions and physical reactions. The account was read aloud by the participants and recorded on audio tape, which they were asked to listen to for at least half an hour every day throughout the intervention. The therapist also identified, discussed and challenged any cognitive distortions such as unrealistic beliefs about being responsible for their injury. Image habituation training (Reference Vaughan and TarrierVaughan & Tarrier, 1992), where a traumatic image is kept repeatedly in mind for 30s or more, was used when the participant was being troubled by specific distressing intrusive images. A graded in vivo exposure programme was devised if the participant was avoiding real-life situations, for example car travel. Homework tasks comprised listening to the tape daily, using image habituation training where necessary and the achievement of any agreed exposure goals. During the final session, discussion focused on successes and difficulties over the course of therapy. The participant was given a written summary that outlined successes, areas for attention, potential problem areas and how to cope with these. In all the sessions, progress, levels of functioning and homework compliance were reviewed.
No intervention
Individuals randomly allocated to the ‘no intervention’ group were advised of this and that they would be contacted again 12 weeks and 13 months after the trauma for further evaluation. Before randomisation, all individuals were advised that, should they be allocated to the ‘no intervention’ group, they would not receive an alternative intervention unless clinically indicated because this could compromise interpretation of the results. They were also advised that they could contact the investigators at any time, should the need arise.
Patient evaluations
Baseline measures were obtained using questionnaires designed to establish basic demographic information, levels of functioning and perceptions of the trauma and its impact. The HADS, IES and PTSD Diagnostic Scale were also completed. At 12 weeks and 13 months after injury the participants completed further questionnaires, including the HADS and IES, to determine the effects of injury. In addition, a second research psychologist (D.J.) interviewed all participants and administered the clinician-administered PTSD Diagnostic Scale blind to whether or not the participant had received the intervention. D.J. was asked to indicate to which group she thought that the participants had been allocated. Her classification was no different from chance, strongly suggesting successful blinding.
Statistical analysis
The protocol power calculation assumed a group difference in reduction of IES score of 10 points over 13 months, with a within-group s.d. at baseline of 15. In order to have a 95% probability of correctly detecting a significant difference and a 5% chance of incorrectly rejecting the null hypothesis, a minimum sample size of 60 patients in each group was required. The main analysis of the results was an intention-to-treat analysis based on all randomised participants as randomised. The last valid score of those who did not complete the trial was carried forward for the final analysis. Unfortunately there is no really satisfactory solution to the general problem of missing data. It was therefore decided also to analyse only those who completed, as a form of sensitivity analysis, and to examine the degree to which this and the intention-to-treat analysis differ. The mean values obtained from the main outcome measures at follow-up for the control group and the intervention group were compared using analysis of covariance, with the baseline score as covariate, and 95% confidence intervals. Analysis of covariance was performed separately for each variable and time point. No interactions were tested. Dichotomous variables were analysed using relative risks and 95% confidence intervals.
Forward linear stepwise regression analyses were performed to investigate the impact of independent variables selected a priori through a review of the results of previous studies of predictors of PTSD on the total IES score at 3 and 13 months. The independent variables selected were injury in assault, female gender, past psychiatric history, past trauma history, neuroticism, alexithymia, the intervention, compensation claim, visual analogue scales regarding degree of self-blame, blaming others and pain, and initial scores on the HADS anxiety and depression sub-scales and the IES intrusion and avoidance sub-scales. A variable was entered if the significance level of its F-to-enter was less than the entry value of 0.05, and removed if the significance was greater than the removal value of 0.1. All were measured at baseline with the exception of the compensation variable (proportion who claimed compensation for their injuries), which was determined at the 3- and 13-month follow-up interviews.
RESULTS
The trial profile is shown in Fig. 1. A total of 473 individuals were sent the initial questionnaires because they described psychological symptoms and, potentially, fulfilled the other inclusion criteria. Of the 201 (42%) who were screened, 26 did not fulfil the psychological distress criteria, 6 returned questionnaires too late, 10 had pre-existing major psychiatric disorder, 6 had major physical illness or disability and 1 would not have been available for follow-up. All 152 individuals who met all the criteria were randomised; there were 87 females (57%) and 65 males (43%).
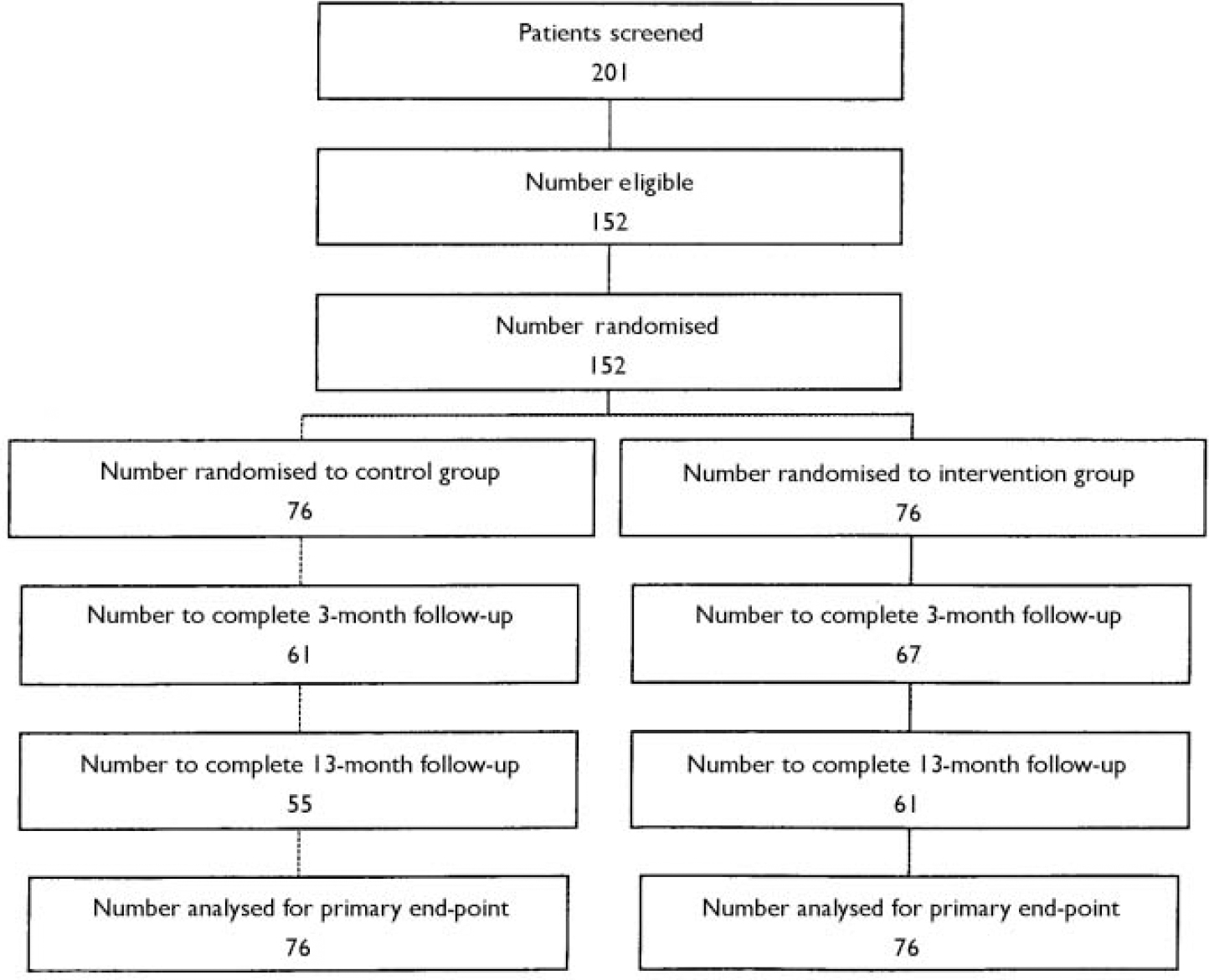
Fig. 1 Trial profile.
A total of 76 participants were randomised to each group: 67 (88%) of the intervention group and 61 (80%) of the control group completed the 3-month follow-up and 61 (80%) of the intervention group and 55 (72%) of the control group completed the 13-month follow-up. There appeared to be no major differences in relation to the outcome measures at baseline between the 116 participants who completed the follow-up period and the 36 (24%) who did not: mean initial IES score was 46.0 (s.d.=16.3) for the former and 45.8 (s.d.=15.5) for the latter. Background variables and dimensions of trauma are set out in Table 1. The intervention and control groups appeared equivalent. The mean number of intervention sessions was 3.30 (s.d.=1.24). Four (5%) of the intervention group completed no treatment sessions, 7 (9%) completed one, 5 (7%) completed two, 6 (8%) completed three and 54 (71%) completed all four. None of the control group received alternative treatment.
Table 1 Comparison of background variables and dimensions of trauma between intervention and control groups
| Intervention group (total n=76) | Control group (total n=76) | |
|---|---|---|
| Age, years (n (%)) | ||
| 16-24 | 20 (26%) | 21 (28%) |
| 25-34 | 25 (33%) | 16 (21%) |
| 35-44 | 17 (22%) | 15 (20%) |
| 45-54 | 9 (12%) | 12 (16%) |
| 55-64 | 5 (7%) | 11 (14%) |
| 65-69 | 0 (0%) | 1 (1%) |
| Female gender (n (%)) | 43 (57%) | 44 (58%) |
| Employed (n (%)) | 48 (63%) | 46 (61%) |
| Married (n (%)) | 27 (36%) | 30 (40%) |
| Past psychiatric history (n (%)) | 19 (25%) | 17 (22%) |
| Previous trauma history1 (n (%)) | 26 (34%) | 28 (37%) |
| Motor vehicle accident (n (%)) | 44 (58%) | 41 (24%) |
| Assault (n (%)) | 25 (33%) | 28 (37%) |
| Other trauma (n (%)) | 7 (9%) | 7 (9%) |
| Category (n (%)) | ||
| Minor | 62 (82%) | 62 (82%) |
| Moderate | 12 (16%) | 11 (15%) |
| Serious | 2 (3%) | 3 (4%) |
| How stressful2 (mean (s.d.)) | 8.68 (1.88) | 8.84 (1.85) |
| Blame others2 (mean (s.d.)) | 8.38 (2.80) | 8.46 (2.85) |
| Blame self2 (mean (s.d.)) | 2.37 (2.61) | 2.26 (2.46) |
| Thought might die2 (mean (s.d.)) | 3.96 (3.46) | 4.11 (3.65) |
| Required rescue (n (s.d.)) | 26 (34%) | 37 (49%) |
| Others injured (n (s.d.)) | 21 (28%) | 23 (30%) |
Dimensions of trauma
Of the intervention group 44 (58%) had been injured as a result of a motor vehicle accident, compared with 41 (54%) of the control group; 25 (33%) of the intervention group had been injured as a result of an assault, compared with 28 (37%) of the control group; and 7 (9%) of the intervention group had been injured as a result of other incidents, compared with 7 (9%) of the control group. The latter included an electrocution, partial amputation of fingertips, falls and a variety of industrial injuries. The majority of individuals in both groups – 61 (80%) of the intervention group and 62 (82%) of the control group – had an Abbreviated Injury Scale (Association for the Advancement of Automotive Medicine, 1990) score of 1 (denoting minor injury). Twelve (16%) of the intervention group scored 2 (moderately severe injury), compared with eleven (15%) of the control group; and two (3%) of the intervention group and three (4%) of the control group scored 3 (serious injury). One incident involved the death of another individual.
Outcome measures
The results of an intention-to-treat analysis of the main outcome measures based on all 152 subjects are shown in Table 2. The mean reduction in the IES scores was significantly greater in the intervention group than in the control group at 13 months and was greater at 3 months, although this was not significant. These findings apply to the IES total score and to both the intrusion and avoidance sub-scales. The clinician-administered PTSD Diagnostic Scale scores were also lower in the intervention group at both 3 and 13 months but the differences were not significant. There were no significant differences in the reductions in the anxiety or depression sub-scale scores of the HADS between the groups at any time point. The ‘completers-only’ analysis revealed very similar results. The mean reduction in IES scores was significantly greater in the intervention group at 13 months and was greater than in the control group at 3 months, although this was not significant. At 13 months the adjusted mean difference between scores for those in the intervention group who completed the trial (n=61) and those in the control group was 10.0 (95% CI 3.4–16.6, P=0.003). There were no significant differences in the reductions in the anxiety or depression sub-scale scores of the HADS between the completer groups at any time point.
Table 2 Main outcome measures
| Psychometric measure | Intervention group (n=76) Mean (s.d.) | Control group (n=76) Mean (s.d.) | Adjusted mean difference (95% CI) | F | P 1 |
|---|---|---|---|---|---|
| HADS—A | |||||
| Initial score | 12.0 (4.4) | 11.7 (4.4) | |||
| Reduction at 3 months | 2.1 (4.1) | 1.8 (3.7) | 0.3 (-0.9 to 1.5) | 0.2 | 0.7 |
| Reduction at 13 months | 2.8 (4.4) | 2.4 (4.3) | 0.3 (-1.0 to 1.6) | 0.2 | 0.6 |
| HADS—D | |||||
| Initial score | 8.5 (4.3) | 8.8 (4.5) | |||
| Reduction at 3 months | 2.0 (3.5) | 1.8 (4.0) | 0.3 (-0.8 to 1.5) | 0.1 | 0.6 |
| Reduction at 13 months | 3.0 (3.9) | 2.6 (4.7) | 0.5 (-0.8 to 1.9) | 0.8 | 0.4 |
| IES | |||||
| Initial score | 47.0 (16.7) | 45.0 (15.5) | |||
| Reduction at 3 months | 10.0 (18.0) | 5.4 (16.3) | 4.1 (-1.3 to 9.4) | 1.5 | 0.1 |
| Reduction at 13 months | 20.7 (22.3) | 11.2 (18.1) | 8.4 (2.4 to 14.4) | 9.0 | 0.006 |
| IES—I | |||||
| Initial score | 24.1 (8.9) | 23.8 (8.4) | |||
| Reduction at 3 months | 5.1 (9.9) | 3.8 (8.3) | 1.2 (-1.6 to 4.0) | 0.3 | 0.4 |
| Reduction at 13 months | 11.4 (11.7) | 7.6 (9.4) | 3.6 (0.5 to 6.7) | 7.5 | 0.02 |
| IES—A | |||||
| Initial score | 23.0 (9.5) | 21.1 (9.0) | |||
| Reduction at 3 months | 5.0 (10.2) | 1.6 (9.8) | 2.7 (-0.3 to 5.8) | 2.4 | 0.1 |
| Reduction at 13 months | 9.4 (12.4) | 3.6 (10.8) | 4.8 (1.4 to 8.2) | 7.8 | 0.006 |
| CAPS | |||||
| 3 months2 | 31.1 (21.3) | 34.8 (24.6) | -3.7 (-11.4 to 4.1) | 0.4 | |
| 13 months2 | 20.9 (16.6) | 27.5 (24.2) | -6.6 (-13.6 to 0.4) | 0.07 |
Twenty (30%) of both the intervention and control groups satisfied the DSM–IV criteria for PTSD according to the clinician-administered PTSD Diagnostic Scale at 3 months (relative risk=1.0, 95% CI 0.5–2.1). At 13 months, 10 (16%) of the intervention group satisfied the DSM–IV criteria for PTSD compared with 15 (27%) of the control group (relative risk=0.6, 95% CI 0.3–1.5). A 50% reduction in the baseline IES score was found in 19 (25%) of the intervention group at 3 months compared with 15 (20%) of the control group (relative risk=0.73, 95% CI 0.3–1.6). At 13 months 34 (45%) of the intervention group had achieved a 50% reduction in the baseline IES score compared with 21 (28%) of the control group (relative risk=0.5, 95% CI 0.2–0.9).
Participants in the intervention group appeared to value the intervention, as judged by a mean score of 8.3 (s.d.=1.7) when asked to evaluate the usefulness of the intervention on a 0–10 scale (0=‘no use at all’; 10=‘as useful as I can imagine’).
Linear regression analyses
Total IES at 3 months
Table 3 displays the results of this analysis. The first variable to be added was the initial intrusion score on the IES (IES–I), which accounted for 31% of the total variance. The variable entered in step 2 was the initial depression score on the HADS (HADS–D), which, along with the IES–I score, accounted for 33% of the total variance of the IES total score at 3 months. No further variables were added to the results because the predetermined 0.05 limit was reached. This shows that the initial IES–I score influenced the total IES score at 3 months more than any other independent variable, and that the initial HADS–D score had a small additional influence on the total IES at 3 months independently of the IES–I.
Table 3 Stepwise linear regression analysis results using scores on the intrusion sub-scale of the Impact of Event Scale (IES—I) at 3 months and 13 months as the dependent variable
| Variable | Regression coefficient (B) | Standard error of B | T | P |
|---|---|---|---|---|
| Three months | ||||
| IES—I | 1.16 | 0.19 | 6.08 | < 0.001 |
| HADS—D | 0.79 | 0.38 | 2.07 | 0.04 |
| (Constant) | 1.81 | 4.55 | 0.40 | 0.69 |
| Thirteen months | ||||
| IES—I | 0.80 | 0.20 | 4.09 | < 0.001 |
| Intervention | 8.86 | 3.36 | 2.64 | 0.01 |
| Pain | 1.38 | 0.66 | 2.10 | 0.04 |
| (Constant) | -14.52 | 7.45 | -1.95 | 0.05 |
Total IES at 13 months
The first variable to be added was initial IES–I score, which accounted for 12% of the total variance. The variable entered in step 2 was the intervention, which, along with IES–I, accounted for 19% of the total variance. The level of pain reported initially was entered in step 3, which, along with the intervention and the IES–I score, accounted for 21% of the total variance of the IES total score at 13 months. No further variables were added to the results because the predetermined 0.05 limit was reached. This shows that the initial IES–I score influenced the total IES score at 13 months more than any other independent variable. Receipt of the intervention also significantly influenced the total IES score at 13 months to a lesser extent, as did the level of initial pain reported.
DISCUSSION
The main finding in this study was that symptoms of PTSD as measured by the IES had decreased significantly more in the intervention group than in the control group at the 13-month follow-up. The avoidance sub-scale scores of the IES had decreased significantly more at 3 months. The treatment effect was modest and the clinician-administered PTSD Diagnostic Scale and the HADS scores did not drop differentially across the two groups. There were no other significant differences between the groups over time. Time had a marked effect: symptoms in both groups decreased significantly over the 13 months on all measures. Linear regression analyses found that higher initial intrusion and depression scores were predictive of worse outcome at 3 months and that higher initial intrusion scores, not receiving the intervention and higher levels of reported pain initially were predictive of worse outcome at 13 months.
Design
Rigorous study design and methodological soundness were key objectives because many previous studies of the effectiveness of brief interventions have been characterised by porous methodology. The sample size was larger than in previous studies of early multiple-session interventions following traumatic events and those who completed the follow-up period were representative of those included. The 13-month follow-up period enabled longer-term assessment of the intervention than in previous studies. The exclusion criteria may have led to some bias but were likely to result in the exclusion of individuals less likely to respond to a brief, focused intervention.
Efficacy and mechanism
In common with the three previous positive-outcome randomised controlled trials (Reference André, Lelord and LégeronAndré et al, 1997; Bryant et al, Reference Bryant, Harvey and Dang1998, Reference Bryant, Sackville and Dang1999) but contrary to the findings of investigations of early single-session interventions (Reference Rose, Bisson and WesselyRose et al, 2001), the results of this study suggest that a four-session cognitive–behavioural intervention reduces the symptoms of PTSD following physical injury and is well tolerated. However, this study is not directly comparable with the studies of Bryant et al (Reference Bryant, Harvey and Dang1998, Reference Bryant, Sackville and Dang1999) because Bryant and colleagues worked with patients identified as having acute stress disorder and the intervention was planned to be applied within 2 weeks. In our study individuals had to be experiencing symptoms but no diagnosis was required and the intervention was between 5 and 10 weeks post-trauma.
Possible mechanisms for the positive outcome in this study include the fact that processing may occur with regular controlled exposure, as happens with multiple-session but not single-session interventions. This explanation is consistent with psychological theories in which it is argued that the formation of fear structures and associated avoidance behaviour leads to the development of PTSD (e.g. Reference Foa and KozakFoa & Kozak, 1986). The educational component and cognitive restructuring may also have facilitated the processing of traumatic material. The absence of a significant effect on outcome 3 months after injury except on the avoidance sub-scale of the IES and the fact that rates of PTSD were equal in both groups may be due to the recent completion of the month-long intervention. It might have been desirable on this basis to have delayed the post-treatment assessment until 1 month after completion of the intervention, although previous studies have not found equivalent rates of PTSD after intervention (e.g. Bryant et al, Reference Bryant, Harvey and Dang1998, Reference Bryant, Sackville and Dang1999). Ongoing confrontation of feared stimuli may have resulted in the positive effects of exposure work increasing over time, as has been shown in treatment trials of exposure therapy for established PTSD (Reference Marks, Lovell and NoshirvaniMarks et al, 1998).
The positive impact of the intervention was not very large. There are several potential explanations for this. It may be that the intervention was not long enough, that the cognitive–behavioural techniques used were not effective for some individuals or that the relative inexperience of the therapist had a bearing on the results. These explanations would appear to be supported by a study of acute stress disorder in which individuals appeared to improve more following five 1.5-h sessions delivered by more experienced therapists (Reference Bryant, Harvey and DangBryant et al, 1998). However, the precisely defined nature of the therapy and the supervision and fidelity checks should have helped to reduce any negative impact of therapist experience. Previous research suggests that therapist inexperience has a small negative impact on outcome (Reference Stein and LambertStein & Lambert, 1995).
The focus of the intervention on PTSD may account for the finding that there were no significant differences in depression and anxiety scores between the intervention and control groups: the intervention neither decreased nor increased anxiety and depression relative to the control group. This raises questions about the significance of the effect of treatment of anxiety and depression. It seems probable that other symptoms such as anxiety and depression may require treatment in their own right through psychological or pharmacological techniques.
Predictors
The finding that initial intrusion symptoms on the IES are predictive of poor outcome at both 3 and 13 months is supported by previous studies (Reference Brewin, Andrews and RoseBrewin et al, 1998). The association of a poorer outcome with initial depression is also supported by other studies (Reference Wallace and LeesWallace & Lees, 1988; Reference Freedman, Brandes and PeriFreedman et al, 1999). The other factors identified as being predictive of poorer outcome at 13 months were the absence of intervention and higher levels of initial pain. The finding of an association with physical pain is interesting. Physical pain may make the initial experience more traumatic or be another index of psychological distress. Pain has been much researched and found to be associated with poorer psychological outcome in other studies (Reference Perry, Cella and FalkenbergPerry et al, 1987; Reference Difede, Jaffe and MusngiDifede et al, 1997). The absence of an association of IES score with the other variables considered is also important.
Clinical implications
This study suggests that individuals presenting to accident and emergency departments with minor/moderately severe injury can be helped by routine screening to detect the presence of acute psychological sequelae and, if these are present, by a four-session cognitive–behavioural intervention. This intervention is straightforward and could be delivered by mental health professionals or counsellors with specific training and supervision. Implementation would have major resource implications, however, because there is no similar intervention being carried out routinely in trauma centres at present.
Given the lack of evidence of the effectiveness of early single-session interventions, we consider it unlikely that a shorter intervention than this one is likely to be beneficial. Streamlining the intervention could reduce costs but would be unlikely to be cost-effective. It could be argued that it is not cost-effective to treat all cases this early, given the high rate of remission in the control group. An alternative ‘stepped care’ approach could be introduced where only those individuals who remain symptomatic at, say, 3 months are offered a four-session intervention, which would be likely to result in a reduction of the numbers entering treatment. This could, however, result in the development of more established and potentially more difficult-to-treat disorders than those present 1 month after injury. Investment could, potentially, lead to reduced morbidity and improved functioning in what is a very large population of those with physical injury.
There remain many unanswered questions. Not everyone in the intervention group experienced improvement and although there was a modest reduction in PTSD symptoms at 13 months it was apparent that several individuals continued to experience significant distress. However, this study is evidence that early interventions can help and serves as a catalyst to further research in this area. Future research should investigate intervention timing in more detail, specific interventions for coexisting anxiety and depressive symptoms and application to those with more serious trauma.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Four sessions of early cognitive–behavioural therapy can modestly reduce symptoms of post-traumatic stress disorder, but not depression or anxiety, in individuals distressed following physical injury.
-
▪ The benefits of four sessions of early cognitive–behavioural therapy appear to increase over time.
-
▪ A stepped-care approach could be implemented with routine screening and the offer of four sessions of cognitive–behavioural therapy to symptomatic individuals.
LIMITATIONS
-
▪ No interview data were collected at baseline and there was no placebo intervention condition.
-
▪ The severity of injury was mild to moderate and it is not known if this intervention would help more severely injured individuals.
-
▪ The cost-effectiveness of early intervention needs to be tested.
Acknowledgements
This study was supported by a grant from the Welsh Office of Research and. Development for Health and Social Care. We thank Frank Fincham for his. valuable support and suggestions throughout the study and the Cardiff. Emergency Department staff for allowing us to approach their patients. We also. thank the participating patients.







eLetters
No eLetters have been published for this article.