In his concept of schizophrenia Bleuler (Reference Bleuler and Zinkin1911) gave pre-eminence to formal thought disorder (a disorder of ‘association’). Critical of the theoretical complexity of Bleuler's approach, Schneider (Reference Schneider, Hirsch and Shepherd1957) introduced the concept of ‘nuclear’ or ‘first-rank’ symptoms. These have acquired increasing prominence, along with a Kraepelinian component of poor outcome, in DSM-III, DSM-IV and ICD-10 criteria (American Psychiatric Association, 1980, 1994; World Health Organization, 1992). In addition to specific types of hallucination, Schneider drew attention to the significance of primary disorders of the experience of thought (withdrawal, insertion and broadcast) although the relationship of these to Bleuler's disorders of thought and association has remained obscure. To overcome some of the limitations of Bleuler's approach, Andreasen (Reference Andreasen1979a , Reference Andreasen b ) shifted the focus of investigation from ‘thought’ to the more objectively measurable ‘language behaviour’.
In this study we investigated the relationship of language abnormalities to Schneiderian first-rank symptoms in acute psychosis, and compared the predictive diagnostic validity of language disturbances and first-rank symptoms for an ICD-10 diagnosis.
METHOD
The data-set for this study was drawn from 30 consecutive cases of psychosis in which at least one Schneiderian first-rank symptom was currently active. The male and female patients, aged 18-65 years, were enrolled from February 1999 to January 2001; 22 were in-patients. A diagnosis of schizophrenia was not a requirement for inclusion. All patients but one resided in A.C.-N.'s catchment area (of approximately 150 000 general population) and were well known to him. The remaining patient had been referred to A.C.-N. for a second opinion. The main exclusion criterion was a recent history (within the previous 6 months) of any recreational drug use or alcohol dependence. A urine drug screen was performed in all suspected cases. In addition to these 30 patients, a further 11 patients were screened but did not satisfy all study criteria for inclusion. Enrolled patients were stratified into two main diagnostic subgroups according to whether or not they fulfilled the ICD-10 definition of schizophrenia. An additional control group of 15 patients who had never experienced first-rank symptoms and who fulfilled the ICD-10 criteria for severe depression were also enrolled in the study. Study procedures were completed in all patients within a week of hospital admission or referral to the out- patient clinic. All interviews and ratings were completed by one observer (A.C.-N.).
Table 1 shows the demographic characteristics of the analysed sample. The three diagnostic subgroups, defined using ICD-10 criteria, did not differ significantly from one another in current age, age at onset of illness, duration of illness, gender, ethnicity and mean severity of illness. All patients had experienced a new episode or an exacerbation of existing illness just prior to enrolment into this study. All patients with first-rank symptoms had been receiving antipsychotic medication for periods varying from a few days to several years.
Table 1 Demographic details of the study participants (n=45)
| SFRS schizophrenia group | SFRS other diagnoses | Depression group | |
|---|---|---|---|
| No. of patients | 17 | 13 | 15 |
| Age years | |||
| Mean (s.d.) | 38.9 (11.5) | 33.5 (10.0) | 43.1 (10.9) |
| 95% CI | 33.0-44.8 | 27.5-39.5 | 37.1-49.1 |
| Age at onset, years | |||
| Mean (s.d.) | 25.5 (7.9)1 | 26.0 (9.6) | 32.7 (12.1) |
| 95% CI | 21.3-29.7 | 20.2-31.8 | 26.0-39.4 |
| Duration, years | |||
| Mean (s.d.) | 13.6 (10.8)1 | 7.5 (10.2) | 10.4 (9.3) |
| 95% CI | 7.8-19.4 | 1.3-13.7 | 5.2-15.6 |
| Gender (n) | |||
| Female | 6 | 6 | 11 |
| Male | 11 | 7 | 4 |
| Ethnicity (n) | |||
| White | 16 | 13 | 15 |
| Asian | 1 | ||
| Severity of illness score2 | |||
| Mean (s.d.) | 5.2 (1.0) | 5.2 (0.83) | 4.8 (0.77) |
| 95% CI | 4.7-5.7 | 4.7-5.7 | 4.4-5.2 |
| ICD—10 diagnosis (n) | |||
| F20 Schizophrenia | 17 | ||
| F22 Persistent delusional disorder | 1 | ||
| F23 Acute and transient psychotic disorder | 2 | ||
| F25 Schizoaffective disorder | 4 | ||
| F31 Bipolar affective disorder | 2 | 1 | |
| F32 Depressive episode | 2 | 7 | |
| F33 Recurrent depressive episode | 2 | 6 | |
| F38 Other mood disorder | 7 |
Schneiderian first-rank symptoms
First-rank symptoms were rated as absent or borderline (0) or definitely present (1) using the definitions proposed by Mellor (Reference Mellor1970) and revised by Sims (Reference Sims1995). Clinical information was collected with a semi-structured interview which was largely based on the Present State Examination (PSE; Reference Wing, Cooper and SartoriusWing et al, 1974) with the addition of more-detailed questions focusing on first-rank symptoms. Symptoms were recorded as currently active if patients had experienced them within the week before the interview. In reality the great majority of enrolled patients had experienced first-rank symptoms in the few hours before or were still experiencing them during the clinical inteview.
Language abnormalities
The characteristics of language were assessed with the Clinical Language Disorder Rating Scale (CLANG; Reference Chen, Lam and KanChen et al, 1996). This consists of 17 observer-rated items anchored on a four-point severity scale (see Appendix).
Stratification into diagnostic groups
Based on the patients' ICD-10 diagnoses (Table 1), patient groups were compared as follows:
-
(a) comparison 1: Schneiderian first-rank symptom schizophrenia group (n=17) and Schneiderian first-rank symptom ‘other diagnoses’ group (n=13) v. depression group (n=15);
-
(b) comparison 2: Schneiderian first-rank symptom schizophrenia group (n=17) v. all conditions (n=28);
-
(c) comparison 3: non-affective psychoses (ICD-10 codes F20 to F25) group (n=24) v. mood disorders group (n=21).
Data analysis
The data were analysed as follows. Factor analysis (principal component analysis with varimax rotation) was applied to the 17 CLANG and 11 Schneiderian First-Rank Symptom (SFRS) Scale individual items (sample n=30; only patients with first-rank symptoms were analysed). Cronbach's α coefficient was computed for the CLANG and SFRS factors to assess the internal reliability of the whole scales and their sub-scales. Non-parametric correlation coefficients (Spearman's ρ) were computed between CLANG and SFRS factors and total scales (sample n=45, all patients). All these analyses were completed using the Statistical Package for the Social Sciences statistical software SPSS for Windows, Release 10.1.0.
Odds ratios and 95% confidence intervals were computed for selected CLANG items associated with first-rank symptoms. If one or more cells of 2 × 2 contingency were equal to zero, 0.5 was added to all cells. Fisher's exact test (two-tailed) was used to test the null hypothesis that there is no relationship between the CLANG and the SFRS items.
The abilities of the CLANG and SFRS scales to discriminate disease cases from control cases were evaluated using receiver operating characteristic (ROC) analysis. Sensitivity, specificity, positive likelihood ratios, the area under the ROC curve and their relative 95% confidence intervals were computed using Confidence Interval Analysis for Windows (Reference Altman and MachinAltman & Machin, 2000). The comparison of areas under the ROC curve using different diagnostic tests was computed with AccuROC for Windows, version 2.3, which uses a non-parametric approach.
RESULTS
Factorial structure of language disorder rated by CLANG
Two items (‘pragmatic disorder’ and ‘pressure of speech’) were never observed as present in our sample and consequently could not be entered into the analysis. Five factors were extracted, using an eigenvalue > 1 as the criterion for interpretation, accounting for 81% of total variance (Table 2). Most of the variance (65%) was accounted for by three factors, which we labelled ‘semantic’ (disorders), ‘poverty’ (of speech) and ‘excess’ (of speech). These three factors were adopted to create three sub-scales for the CLANG and their scores were used in further analysis.
Table 2 Factor structure (principal component analysis with varimax rotation) and internal reliability of the Clinical Language Disorder Rating Scale
| Items | Factor 1 Semantic | Factor 2 Poverty | Factor 3 Excess | Factor 4 Dysarthria | Factor 5 Prosody | Eigenvalue | Variance (%) | Cumulative variance (%) | Corrected item total correlation | Alpha if item deleted |
|---|---|---|---|---|---|---|---|---|---|---|
| 6 Discourse failure (loss of overall goal) | 0.94 | -0.08 | 0.05 | -0.11 | -0.12 | 5.41 | 36.04 | 36.04 | 0.90 | 0.87 |
| 4 Lack of semantic association (loss of semantic relationship) | 0.97 | -0.19 | -0.06 | -0.06 | 0.13 | 0.88 | 0.88 | |||
| 16 Neologisms | 0.87 | -0.16 | -0.07 | 0.33 | 0.18 | 0.85 | 0.88 | |||
| 1 Excess phonetic association (sound-based associations) | 0.76 | -0.16 | 0.05 | 0.52 | -0.19 | 0.75 | 0.89 | |||
| 17 Paraphasic error (substitution by imprecise words) | 0.73 | -0.17 | -0.09 | 0.04 | 0.18 | 0.56 | 0.91 | |||
| 2 Abnormal syntax (abnormal grammar structure) | 0.71 | -0.08 | 0.13 | -0.11 | -0.54 | 0.65 | 0.90 | |||
| 5 Referential failures (unclear links) | 0.69 | -0.27 | 0.51 | -0.11 | 0.13 | 0.67 | 0.91 | |||
| Sub-scale α=0.91 | ||||||||||
| 9 Aprosodic speech (flat, monotonous speech) | -0.13 | 0.85 | 0.14 | -0.09 | 0.06 | 0.63 | 0.70 | |||
| 14 Poverty of speech | -0.20 | 0.81 | -0.24 | -0.14 | 0.18 | 2.37 | 15.78 | 51.82 | 0.80 | 0.58 |
| 12 Dysfluency (abnormal rhythm) | 0.08 | 0.76 | -0.03 | 0.07 | 0.05 | 0.44 | 0.80 | |||
| 8 Lack of details | -0.34 | 0.51 | -0.41 | -0.34 | -0.07 | 0.55 | 0.73 | |||
| Sub-scale α=0.77 | ||||||||||
| 7 Excess details | 0.01 | -0.08 | 0.93 | -0.03 | -0.11 | 1.95 | 13.00 | 64.82 | 0.69 | |
| 3 Excess syntactic constraints (excessive grammar) | -0.09 | 0.02 | 0.87 | 0.01 | 0.18 | 0.69 | ||||
| Sub-scale α=0.61 | ||||||||||
| 13 Dysarthria (articulation difficulties) | -0.03 | -0.08 | -0.04 | 0.96 | -0.04 | 1.27 | 8.49 | 73.31 | - | - |
| 10 Abnormal prosody (bizarre quality of voice) | 0.15 | 0.06 | 0.11 | -0.08 | 0.86 | 1.16 | 7.75 | 81.07 | - | - |
| 11 Pragmatic disorder (defective knowledge of the world)1 | - | - | - | - | - | - | - | - | - | - |
| 15 Pressure of speech1 | - | - | - | - | - | - | - | - | - | - |
| Full-scale α=0.52 |
Internal reliability of CLANG
The internal consistency of the CLANG and the relative contribution of individual items were characterised by applying Cronbach's α coefficient to the data-set (n=30). The internal reliability for the first two sub-scales was high (α=0.92 for ‘semantic disorders’, α =0.77 for ‘poverty’), but less good for the third sub-scale (α=0.61) and the entire scale (α=0.52) (Table 2).
Factorial structure of psychotic symptoms rated by the SFRS Scale
Five factors were extracted using an eigen-value > 1 as the criterion for interpretation, accounting for 81% of total variance. Most of the variance (63%) was accounted for by the first three factors, which we labelled ‘voices’, ‘passivity’ and ‘hearing thoughts’ (Table 3). A fourth factor accounted for 9% of variance and was tentatively labelled ‘possessed’. Delusional perception was extracted as a separate factor, accounting for a further 9% of variance.
Table 3 Factor structure (principal component analysis with varimax rotation) and internal reliability of the Schneiderian First-Rank Symptom (SFRS) Scale
| Items | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Eigenvalue | Variance (%) | Cumulative variance (%) | Corrected item total correlation | Alpha if item deleted |
|---|---|---|---|---|---|---|---|---|---|---|
| Voices | Passivity | Hearing thoughts | Possessed | Delusional perception | ||||||
| 3 Voices arguing or discussing | 0.97 | 0.02 | 0.02 | 0.02 | -0.06 | 3.56 | 32 | 32 | 0.87 | |
| 4 Voices commenting on one's actions | 0.94 | 0.03 | 0.04 | -0.07 | -0.17 | 0.87 | ||||
| Sub-scale α=0.93 | ||||||||||
| 8 Passivity of affect (made feelings) | -0.08 | 0.92 | 0.14 | -0.04 | 0.08 | 2.17 | 20 | 52 | 0.63 | 0.76 |
| 11 Somatic passivity (influence playing on the body) | -0.02 | 0.75 | 0.21 | 0.30 | 0.05 | 0.66 | 0.73 | |||
| 10 Passivity of volition (made volitional acts) | -0.07 | 0.68 | 0.14 | 0.55 | -0.17 | 0.67 | 0.72 | |||
| Sub-scale α=0.81 | ||||||||||
| 7 Thought broadcast | -0.05 | 0.16 | 0.87 | 0.12 | 0.12 | 1.19 | 11 | 63 | 0.53 | |
| 2 Audible thoughts (écho de la pensée) | 0.14 | 0.18 | 0.79 | -0.05 | -0.19 | |||||
| Sub-scale α=0.69 | ||||||||||
| 9 Passivity of impulse (made drives) | -0.08 | 0.15 | -0.11 | 0.81 | -0.04 | 1.02 | 9 | 72 | 0.38 | 0.62 |
| 5 Thought withdrawal | 0.40 | 0.04 | 0.45 | 0.63 | 0.21 | 0.44 | 0.55 | |||
| 6 Thought insertion | -0.09 | 0.29 | -0.50 | 0.58 | -0.23 | 0.52 | 0.42 | |||
| Sub-scale α=0.64 | ||||||||||
| 1 Delusional perception | -0.19 | 0.06 | -0.06 | 0.01 | 0.95 | 1.01 | 9 | 81 | ||
| Full-scale α=0.73 | ||||||||||
| If factor 1 deleted α=0.77 |
Internal reliability of the SFRS Scale
The internal reliability for the first two sub-scales was high (α=0.93 for ‘voices’, α=0.81 for ‘passivity’) and just adequate for the remaining two (α=0.69 for ‘hearing thoughts’, α=0.64 for ‘possessed’). The full-scale α was 0.73, but α could be enhanced to 0.77 if item 1 (‘delusional perception’) was removed.
Convergent validity
Convergent validity (Table 4) was assessed by analysing the correlation (non-parametric Spearman's ρ) of CLANG ratings with SFRS ratings in all patients (n=45), assuming correlations with ρ>0.5 and P<0.001 (with Bonferroni correction: α=0.05/336=0.00015) to be of interest. Positive correlations were found only between the sub-scale scores CLANG ‘poverty’ and SFRS ‘passivity’ (ρ=0.61, 95% CI 0.38-0.77) and between CLANG total score and both SFRS ‘hearing thoughts’ (ρ=0.52, 95% CI 0.27-0.71) and SFRS total score (ρ=0.63, 95% CI 0.41-0.78). A few individual items of the CLANG scale were positively correlated with SFRS items: SFRS item 3 (‘voices arguing or discussing’) correlated with two items of the CLANG semantic sub-scale — 1, ‘excess phonetic association’ (ρ=0.52, 95% CI 0.26-0.70), and 17, ‘paraphasic error’ (ρ=0.52, 95% CI 0.26-0.70). The SFRS item 10 ‘passivity of volition’ correlated with two items of the CLANG poverty sub-scale: 8, ‘lack of details’ (ρ=0.63, 95% CI 0.41-0.78) and 14, ‘poverty of speech’ (ρ=0.58, 95% CI 0.35-0.75). Finally, SFRS item 6 ‘thought insertion’ correlated with CLANG item 8 ‘lack of details’ (ρ=0.53, 95% CI 0.28-0.71), and SFRS item 8 ‘passivity of affect’ with CLANG item 14 ‘poverty of speech’ (ρ=0.54, 95% CI 0.29-0.72).
Table 4 Correlations (Spearman's rho) between scores on the Clinical Language Disorder Rating Score (CLANG) and factors on the Schneiderian First-Rank Symptom (SFRS) Scale factors (n=45)
| CLANG factor | SFRS factor | ||||
|---|---|---|---|---|---|
| 1 (Voices) | 2 (Passivity) | 3 (Hearing thoughts) | 4 (Possessed) | Total | |
| 1 Semantic disorder | |||||
| Correlation coefficient | 0.33 | 0.09 | 0.26 | 0.17 | 0.27 |
| Significance (2-tailed) | 0.025 | 0.557 | 0.082 | 0.271 | 0.068 |
| 2 Poverty (of speech) | |||||
| Correlation coefficient | -0.03 | 0.61*1 | 0.29 | 0.41 | 0.46 |
| Significance (2-tailed) | 0.831 | 0.001 | 0.051 | 0.005 | 0.002 |
| 3 Excess (of speech) | |||||
| Correlation coefficient | 0.09 | 0.09 | 0.25 | 0.07 | 0.12 |
| Significance (2-tailed) | 0.547 | 0.536 | 0.093 | 0.664 | 0.438 |
| Total | |||||
| Correlation coefficient | 0.06 | 0.45 | 0.52*2 | 0.46 | 0.63*3 |
| Significance (2-tailed) | 0.740 | 0.012 | 0.001 | 0.002 | 0.001 |
The association between poverty of speech and passivity phenomena was also confirmed by a 2 × 2 contingency table. Thirty patients (67%) scored positive for the presence of CLANG factor 2 (‘poverty’), of whom 15 (50%) also scored positive for SFRS factor 2 (‘passivity’). Only two further patients scored positive on SFRS factor 2, while scoring negative on CLANG factor 2. The odds ratio of passivity phenomena in patients with or without poverty of speech was 6.5 (95% CI 1.25-33.91) and the null hypothesis of no association between the two variables could be rejected (two-tailed Fisher's exact test, P=0.023). Also confirmed was the association between SFRS item 3 ‘voices arguing or discussing’ (present in 12 patients) and the presence of either CLANG item 1 (‘excess phonetic association’) or item 17 (‘paraphasic error’), which was observed in 6 patients with SFRS item 3 and in no patient without. The approximated odds ratio of paraphasic errors in patients with or without the symptom of voices arguing was 67 (95% CI 3.35-1341) and the null hypothesis of no association between the two variables could be rejected (two tailed Fisher's exact test, P=0.00011).
Diagnostic significance
The distribution of language abnormalities (CLANG items) was examined across the three main study groups: SFRS schizophrenia, SFRS ‘other diagnoses’ and depression without first-rank symptoms (further details available from the authors upon request). Only two items of the CLANG scale — 11, ‘pragmatic disorder’ (defective knowledge of the world, which is difficult to assess) and 15, ‘pressure of speech’ — were not scored in at least one member of the SFRS groups. Conversely, only three CLANG items were scored as present in the ‘depression’ control group: 8, ‘lack of details’, 9, ‘aprosodic speech’, and 14, ‘poverty of speech’. All language disturbances measured by CLANG, except abnormal prosody, were more frequently observed in the SFRS schizophrenia group. The largest differences in proportions between the SFRS schizophrenia and SFRS ‘other diagnoses’ groups were observed for CLANG items 5 ‘referential failures’ (difference 35%, 95% CI 6-59%; two-tailed Fisher's exact test, P=0.02) and 6, ‘discourse failure’ (difference 41%, 95% CI 11-64%; two-tailed Fisher's exact test, P=0.01). The first and third CLANG sub-scales (semantic disorder and excess of speech) received a zero score in all patients in the depression group. Scores on the ‘semantic disorders’ sub-scale were higher in the schizophrenia group (mean 2.76, 95% CI 0.59-4.93) than in the SFRS ‘other diagnoses’ group (mean 0.08, 95% CI 0-0.24); P=0.003 on two-tailed Kruskal—Wallis test.
Several items (further information available from the authors upon request) and sub-scales (Table 5) of CLANG were shown to be highly specific (up to 1, 95% CI 0.77-1) for the diagnosis of schizophrenia and other non-affective psychoses. This high specificity was obtained at the expense of a lower sensitivity: the highest figure was obtained for item 8, ‘lack of details’ (0.71, 95% CI 0.47-0.87). Detailed criteria for interpreting positive likelihood ratios have been described elsewhere (Geddes et al, 1996; Reference Peralta and CuestaPeralta & Cuesta, 1999). Briefly, a clinical test, in order to be considered of some usefulness, should have a positive likelihood ratio in excess of 4. As detailed in Table 5, CLANG factor 1 (semantic disorder), the sum score of the first three CLANG factors and the CLANG total score satisfied this minimum criterion in one or more diagnostic contrasts. The very wide spread of 95% confidence intervals seen here was the result of the small sample size of this study.
Table 5 Receiver operating characteristic analysis of Clinical Language Disorder Rating Scale (CLANG) and Schneiderian First-Rank Symptom (SFRS) Scale
| SFRS schizophrenia group (n=17) v. SFRS other diagnoses (n=13) | SFRS schizophrenia group (n=17) v. all other patients (n=28) | ICD—10 codes F20 to F25 (non-affective psychoses) (n=24) v. ICD—10 codes F31 to F38 (affective disorders) (n=21) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | +LR | AUC | Sensitivity | Specificity | +LR | AUC | Sensitivity | Specificity | +LR | AUC | |
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | (95% CI) | (95% CI) | (95% CI) | (95% CI) | (95% CI) | (95% CI) | (95% CI) | (95% CI) | |
| CLANG factors | ||||||||||||
| 1 Semantic | 0.47 | 1.00 | ∞ | 0.77 | 0.59 | 0.96 | 16.47 | 0.78 | 0.46 | 1.00 | ∞ | 0.73 |
| (0.26-0.69) | (0.77-1.00) | (1.95-∞) | (0.64-0.91) | (0.36-0.78) | (0.82-0.99) | (3.12-95.45) | (0.66-0.91) | (0.28-0.57) | (0.85-1.00) | (2.88-∞) | (0.63-0.83) | |
| 2 Poverty (of speech) | 0.35 | 0.92 | 4.59 | 0.47 | 0.35 | 0.96 | 9.88 | 0.63 | 0.29 | 1.00 | ∞ | 0.61 |
| (0.17-0.59) | (0.67-0.99) | (0.88-27.61) | (0.32-0.75) | (0.17-0.59) | (0.82-0.99) | (1.74-59.76) | (0.46-0.80) | (0.15-0.49) | (0.85-1.00) | (1.80-∞) | (0.45-0.78) | |
| 3 Excess (of speech) | 0.12 | 1.00 | ∞ | 0.56 | 0.12 | 1.00 | ∞ | 0.56 | 0.08 | 1.00 | ∞ | 0.54 |
| (0.03-0.34) | (0.77-1.00) | (0.46-∞) | (0.48-0.64) | (0.03-0.34) | (0.88-1.00) | (0.90-∞) | (0.48-0.64) | (0.02-0.26) | (0.85-1.00) | (0.48-∞) | (0.48-0.60) | |
| 1+2+3 | 0.59 | 0.92 | 7.65 | 0.80 | 0.59 | 0.96 | 16.47 | 0.87 | 0.46 | 1.00 | ∞ | 0.79 |
| (0.36-0.78) | (0.67-0.99) | (1.62-44.09) | (0.62-0.96) | (0.36-0.78) | (0.82-0.99) | (3.12-95.45) | (0.77-0.97) | (0.28-0.65) | (0.85-1.00) | (2.88-∞) | (0.66-0.92) | |
| CLANG total | 0.59 | 0.85 | 3.82 | 0.76 | 0.59 | 0.93 | 8.24 | 0.85 | 0.46 | 0.95 | 9.63 | 0.78 |
| (0.36-0.78) | (0.58-0.95) | (1.23-14.2) | (0.58-0.94) | (0.36-0.78) | (0.77-0.98) | (2.37-30.98) | (0.75-0.96) | (0.28-0.65) | (0.77-0.99) | (1.87-56.02) | (0.64-0.91) | |
| SFRS factors | ||||||||||||
| 1 Voices | 0.53 | 0.77 | 2.29 | 0.61 | 0.53 | 0.89 | 4.94 | 0.69 | 0.50 | 1.00 | ∞ | 0.73 |
| (0.31-0.74) | (0.50-0.92) | (0.87-6.93) | (0.43-0.80) | (0.31-0.74) | (0.73-0.96) | (1.69-15.26) | (0.55-0.84) | (0.31-0.69) | (0.85-1.00) | (3.15-∞) | (0.61-0.84) | |
| 2 Passivity | 0.29 | 0.85 | 1.63 | 0.51 | 0.53 | 0.71 | 1.85 | 0.64 | 0.54 | 0.81 | 2.84 | 0.68 |
| (0.13-0.53) | (0.58-0.98) | (0.43-6.71) | (0.30-0.71) | (0.31-0.74) | (0.53-0.85) | (0.88-3.86) | (0.49-0.80) | (0.35-0.72) | (0.60-0.92) | (1.20-7.47) | (0.55-0.82) | |
| 3 Hearing thoughts | 0.82 | 0.54 | 1.78 | 0.37 | 0.53 | 0.71 | 1.85 | 0.58 | 0.54 | 0.81 | 2.84 | 0.65 |
| (0.59-0.94) | (0.29-0.77) | (1.03-3.64) | (0.16-0.57) | (0.31-0.74) | (0.53-0.85) | (0.88-3.86) | (0.43-0.73) | (0.35-0.72) | (0.60-0.92) | (1.20-7.47) | (0.50-0.79) | |
| 4 Possessed | 0.94 | 0.23 | 1.22 | 0.46 | 0.59 | 0.75 | 2.35 | 0.64 | 0.58 | 0.86 | 4.08 | 0.71 |
| (0.73-0.99) | (0.08-0.50) | (0.90-1.91) | (0.25-0.67) | (0.36-0.78) | (0.57-0.87) | (1.12-5.03) | (0.49-0.79) | (0.39-0.76) | (0.65-0.95) | (1.54-12.19) | (0.58-0.84) | |
| 1+2+3+4 | 0.88 | 0.31 | 1.27 | 0.49 | 1.00 | 0.61 | 2.55 | 0.76 | 0.92 | 0.71 | 3.21 | 0.81 |
| (0.66-0.97) | (0.13-0.58) | (0.87-2.12) | (0.26-0.72) | (0.82-1.00) | (0.42-0.76) | (1.63-3.98) | (0.62-0.90) | (0.74-0.98) | (0.50-0.86) | (1.79-6.69) | (0.67-0.94) | |
| SFRS total | 0.71 | 0.62 | 1.84 | 0.44 | 1.00 | 0.54 | 2.15 | 0.74 | 1.00 | 0.71 | 3.50 | 0.84 |
| (0.47-0.87) | (0.36-0.82) | (0.94-4.16) | (0.22-0.67) | (0.82-1.00) | (0.36-0.71) | (1.56-3.39) | (0.59-0.89) | (0.86-1.00) | (0.50-0.86) | (1.84-6.65) | (0.70-0.97) | |
Table 5 reports the areas under the ROC curve for CLANG and SFRS sub-scales using different diagnostic definitions for positive and negative groups. At least in our small sample, only CLANG factor 1 and CLANG sum scales showed adequate diagnostic performance (the confidence interval included the 0.5 value) in all diagnostic contrasts. The SFRS dimensions proved to have adequate diagnostic performance only in separating non-affective psychoses from affective disorders.
Figure 1 compares ROC curves (a graph that plots the true positive rate as a function of the false positive rate at different cut-off points) for the sum of the scores of first three CLANG factors, and the first four SFRS factors, defining as positive cases ‘SFRS schizophrenia’ and as negative cases ‘SFRS other diagnoses’. The difference between areas under the ROC curve was 0.30 (95% CI 0.02-0.59; Z=2.09, two-tailed P=0.037).
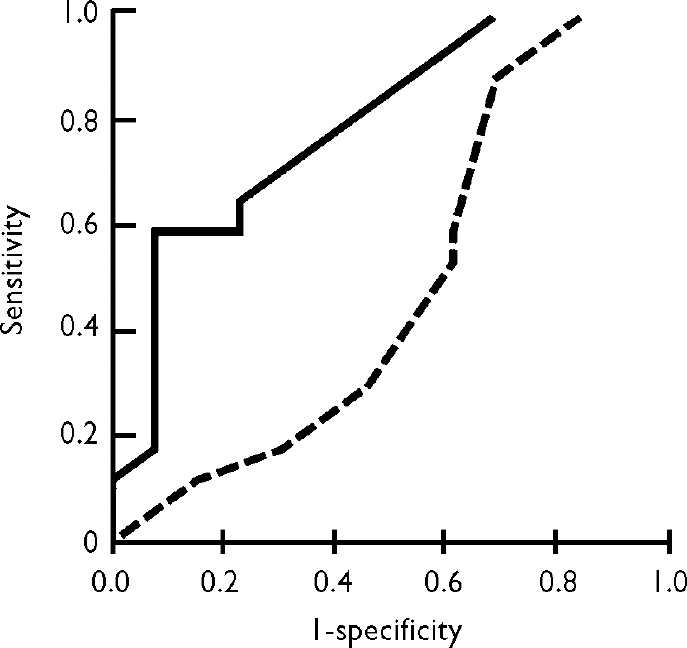
Fig. 1 Comparison of receiver operating characteristic curves for Clinical Language Disorder Rating Scale (CLANG) factors 1+2+3 (solid line) and Schneiderian First-Rank Symptom (SFRS) Scale factors 1+2+3+4 (broken line). Positive group, SFRS schizophrenia, n=17; negative group, SFRS other diagnoses, n=13.
DISCUSSION
Our findings bear upon three issues: the relationship between disturbances of language and psychiatric syndromes; current diagnostic practice as exemplified by the use of the ICD—10 and its relationship to Bleuler's and Schneider's concepts of schizophrenia; and language disturbance as the core of the pathophysiology of psychosis.
CLANG structure
We attempted to replicate the original validation study of the CLANG scale (Reference Chen, Lam and KanChen et al, 1996). The factor structure found in our study — three main factors: ‘semantic’, ‘poverty’ and ‘excess’ of speech — partially matched the structure observed by Chen, whose three main factors were ‘syntactic’, ‘semantic’ and ‘production’. Most of the items composing Chen's first two factors (including paraphasias, abnormal syntax and neologisms in his first factor) were grouped to form our first factor. Chen's ‘production’ factor was made up of three of the four items characterising our ‘poverty’ factor. The most appealing aspect of our very simple factor structure is its close resemblance to the main factors found by Andreasen & Grove (Reference Andreasen and Grove1986) as well as to Bleuler's classification of thought disorders. Andreasen & Grove observed three main components on factor analysis. At least their first two factors closely resemble our first two. The first factor, which they called ‘fluent disorganisation’, was marked by high positive loadings on pressure of speech, derailment, incoherence, illogicality, loss of goal, and perseveration, and high negative loading on poverty of speech; this includes components of our first factor. The second factor, called ‘emptiness’, had high positive loadings on poverty of speech, poverty of content and tangentiality, and a negative loading on pressure of speech and circumstantiality, clearly resembling our second factor ‘poverty’.
Bleuler's classification of thought disorder
Bleuler's classification is even more similar to the factors extracted in our analysis. He described one main group of thought disorders, which he named ‘loose associations’, and suggested the presence of two other types of disturbance with opposite ‘time relationships’ (positive and negative), which he believed could respectively resemble the manic flight and the depressive slowing of ideas. The contrasting disorders observed by Bleuler in schizophrenia were ‘impulsive ideation’ at one extreme and ‘thought block/withdrawal’ at the other of this time-dependent spectrum. It is evident that our second and third factors, ‘poverty’ and ‘excess’, closely resemble the two time-related dimensions of Bleuler's construct.
Our second CLANG factor, ‘poverty’, correlated highly (ρ=0.61) with the second SFRS factor, ‘passivity’. This positive correlation was confirmed by associations between individual items forming the two factors in a 2 × 2 contingency table analysis. We interpret these findings as indicating that a primary negative psychomotor syndrome, which affects predominantly speech (‘poverty’), is sometimes associated with a delusional interpretation by the patient of being controlled. In summary, our first factor (‘semantic’) encompasses Bleuler's fundamental symptom of loosening of association and Andreasen & Grove's (Reference Andreasen and Grove1986) fluent disorganisation and relates them to failures of discourse and reference, to excess phonetic associations and, in symptomatology, to verbal hallucinations; our second factor (‘poverty’) incorporates poverty and aprosody of speech and relates to Bleuler's negative time factor, to Andreasen & Grove's emptiness factor and to passivity phenomena; our third factor (‘excess’) comprising excess details and constraints, may relate to Bleuler's positive time factor, but its definition and clinical correlates are less clear.
Diagnostic validity of CLANG
A significant but unexpected finding is the superior diagnostic validity of various dimensions of the CLANG (positive likelihood ratios >4) compared with the SFRS scale in differentiating ICD—10 schizophrenia from other diagnostic categories, including ICD—10 non-schizophrenic psychoses with nuclear symptoms. We had thought that the CLANG would not fare much better than the SFRS for the following reasons: Chen did not devise the CLANG for diagnostic purposes (Reference Chen, Lam and KanChen et al, 1996); Andreasen's Thought, Language and Communication scale had shown only a weak diagnostic validity in differentiating schizophrenias from schizo-affective disorders (Reference Andreasen and GroveAndreasen & Grove, 1986); the ICD—10 diagnostic criteria for schizophrenia give more prominence to Schneider's first-rank symptoms than to Bleuler's loose associations, and the methods of our study (excluding patients with schizophrenia but without first-rank symptoms) were biased in favour of the diagnostic relevance of first-rank symptoms. Therefore, our finding that the application of ICD—10 criteria leads to the selection of cases more consistent with Bleuler's views than with Schneider's is a paradox that requires explanation. The reason why our 13 patients with at least one first-rank symptom were not classified as suffering from schizophrenia was either that first-rank symptoms and other qualifying symptoms had not been documented before the onset of a disturbance of mood (10 patients) or that they had been present for less than 1 month (3 patients). From our data one could conclude that in the application of the ICD—10 criteria, the presence of first-rank symptoms was useful as a screen (on account of its sensitivity), and then, by the exclusion of patients who were predominantly ‘mood-disordered’ and with short-lasting first-rank symptoms, a group of patients characterised by a more profound disruption of thought processes (independently recognised by the CLANG) was defined.
A new nosological perspective
If the diagnostic process proposed by ICD—10 (and similarly by DSM—IV) reflects current clinical practice, it is clear that an alternative and more rational procedure is possible. We do not propose that Schneiderian first-rank symptoms should be substituted by language abnormalities in the diagnosis of schizophrenia, as the CLANG requires extensive training in its use, and it is not clear how easily it could be adopted in practice. In contrast, first-rank symptoms have become popular in diagnosis because they are easy to recognise. However, the popularity of first-rank symptoms as a diagnostic tool may also represent a drawback, since these symptoms can be feigned or concealed by patients as easily as they can be recognised by clinicians; simulation and concealment of CLANG abnormalities would require much more skill and initiative from a less-collaborative patient. Therefore, at least in a forensic setting, CLANG could prove to be useful in defining the core group of psychoses.
From the viewpoint of nosological theory our observations can be interpreted as a challenge to the categorical and disease-entity-related concepts of both Bleuler and Schneider (and their precursor in the original Kraepelinian dichotomy). It has been argued that the phenomena of psychosis and the human capacity for language share an origin in the genetic changes that defined the species and that these changes were critically related to differentiation of function of the two hemispheres (Crow, Reference Crow1995, Reference Crow1997). Thus, delusions can be considered as deviations in the capacity to attach significance to the phonological representations that are the primary building blocks of words, and Schneider's nuclear symptoms can be conceived as disorders of the transitions from thought to speech, and from perceived speech to meaning, within a reference frame that distinguishes the self of the speaker from that of interlocutors in the outside world (Crow, Reference Crow1998, Reference Crow2000).
This view has the merit that it relates the phenomena of psychosis to the components of a specific capacity (language) and to its neural basis in the differentiation of function of the two hemispheres. The prospect that emerges is the possibility of relating a dimensional description of the phenomena of psychosis, various versions of which have been widely discussed (Reference CrowCrow, 1980; Reference Andreasen and OlsenAndreasen & Olsen, 1982; Reference LiddleLiddle, 1987) but which sit uneasily within the classical Kraepelinian categories (with which they may actually be in conflict), to disturbances of the components of the core function of the human brain, which is the capacity for language (Reference DeLisiDeLisi, 2001).
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ The Clinical Language Disorder Rating Scale (CLANG) is a reliable and valid instrument for the assessment of language disturbances in psychosis.
-
▪ Language disturbances are more specific than first-rank symptoms in the diagnosis of ICD—10 schizophrenia.
-
▪ The assessment of language disturbances may prove particularly useful in a forensic setting and whenever patients' cooperation and sincerity is questionable.
LIMITATIONS
-
▪ This study did not include patients with mania in the control group. Therefore no conclusion can be drawn regarding the diagnostic validity of CLANG in discriminating schizophrenia from mania.
-
▪ The use of CLANG was not compared with other assessment instruments of language disturbance, such as the Scale for the Assessment of Thought, Language and Communication; therefore it is not possible to conclude that it represents any real advantage compared with the other instruments.
-
▪ The assessments of first rank symptoms, CLANG and diagnosis were not made blind.
APPENDIX
Clinical Language Disorder Rating Scale score sheet
Rating guide:
-
• 0 Normal
-
• 1 Mild: no more than 10% of the time
-
• 2 Moderate, regular occurrence: 10-50% of the time
-
• 3 Severe, pervasive: more than 50% of the time
-
• [] Space provided for marking instances of abnormality
| 1 Excess phonetic association (sound-based associations) | 0 | 1 | 2 | 3 | [] |
| 2 Abnormal syntax (abnormal grammar structure) | 0 | 1 | 2 | 3 | [] |
| 3 Excess syntactic constraints (excessive grammar) | 0 | 1 | 2 | 3 | [] |
| 4 Lack of semantic association (loss of semantic relationship) | 0 | 1 | 2 | 3 | [] |
| 5 Referential failures (unclear links) | 0 | 1 | 2 | 3 | [] |
| 6 Discourse failure (loss of overall goal) | 0 | 1 | 2 | 3 | [] |
| 7 Excess details | 0 | 1 | 2 | 3 | [] |
| 8 Lack of details | 0 | 1 | 2 | 3 | [] |
| 9 Aprosodic speech (flat, monotonous speech) | 0 | 1 | 2 | 3 | [] |
| 10 Abnormal prosody (bizarre quality of voice) | 0 | 1 | 2 | 3 | [] |
| 11 Pragmatic disorder (defective knowledge of the world) | 0 | 1 | 2 | 3 | [] |
| 12 Dysfluency (abnormal rhythm) | 0 | 1 | 2 | 3 | [] |
| 13 Dysarthria (articulation difficulties) | 0 | 1 | 2 | 3 | [] |
| 14 Poverty of speech | 0 | 1 | 2 | 3 | [] |
| 15 Pressure of speech | 0 | 1 | 2 | 3 | [] |
| 16 Neologisms | 0 | 1 | 2 | 3 | [] |
| 17 Paraphasic error (substitution by imprecise words) | 0 | 1 | 2 | 3 | [] |
Acknowledgements
The authors thank Dr L. E. DeLisi for her valuable comments on earlier versions of the paper and Dr J. Geddes for statistical advice.









eLetters
No eLetters have been published for this article.