Low birth weight at term is a marker of intrauterine growth restriction and can result from prenatal exposure to high maternal levels of steroids (Reference Gur, Diav-Citrin and ShechtmanGur et al, 2004). As maternal stress results in raised cortisol, psychological symptoms during pregnancy may cause intrauterine growth restriction. Depression and anxiety are common during pregnancy, but evidence for any effect on intrauterine growth is conflicting (e.g. Reference Kelly, Russo and HoltKelly et al, 2002; Reference Andersson, Sundström-Poromaa and WulffAndersson et al, 2004). In this large prospective study we investigated whether mothers with symptoms of depression and anxiety during the second trimester of pregnancy are at greater risk of having babies of low birth weight at term.
METHOD
We used data collected as part of the Avon Longitudinal Study of Parents and Children (ALSPAC; http://www.alspac.bris.ac.uk). In total, 14 541 women were enrolled and 13 194 (90.7%) completed a questionnaire at 18 weeks' gestation.
Questionnaires included the Edinburgh Postnatal Depression Scale (EPDS; Reference Cox, Holden and SagovskyCox et al, 1987) and sub-scales of the Crown-Crisp Experiential Index (CCEI), which measures ‘free-floating’ anxiety (Reference Crisp, Jones and SlaterCrisp et al, 1978) which were completed at 18 and 32 weeks of pregnancy. The EPDS has been validated for use during pregnancy and at other times (Reference Murray and CoxMurray & Cox, 1990; Reference ShakespeareShakespeare, 2001). The CCEI correlates well with other measures of anxiety in women during pregnancy and the internal consistency exceeds 0.8.
Birth weight was obtained directly by research staff. We included only those babies delivered between 37 and 43 weeks' inclusive and we excluded multiple births as these babies are more likely to be of lower birth weight.
Data on confounding factors came from the self-report postal questionnaires and included gender of the baby, gestational age, smoking, maternal age, parity, educational level, alcohol and caffeine use during pregnancy, chronic disease, pre-pregnancy body mass index, ethnicity and a history of miscarriage, Caesarean section, prior low birth weight, or preterm births.
We used linear and logistic regression analyses with birth weight as a continuous outcome or dichotomised as low birth weight (<2500 g) at term. We used the multiple imputation by chained equation method to impute missing data for confounders (Reference van Buuren, Boshuizen and Knookvan Buuren et al, 1999).
RESULTS
Analyses were performed on 10 967 women, of whom 1519 (13.9%, 95% CI 13.2-14.5%) scored >12 on the EPDS at 18 weeks of pregnancy, indicating a likely diagnosis of depression. There were 8427 (76.8%) women with complete data on all confounding variables. We imputed missing data on confounders in all adjusted analyses.
Women scoring >12 on the EPDS at 18 weeks of pregnancy had babies that were 33.8 g lighter (95% CI 8.0-59.7, P=0.01) compared with women with an EPDS score <13. Following adjustment for confounders, an EPDS score >12 was no longer significantly associated with birth weight: babies born to mothers with probable depression were 1.1 g lighter (95% CI -22.1 to 24.3, P=0.4). The strongest confounder appeared to be smoking. The coefficient following adjustment for gender, maternal age and gestation was -25.9 (95% CI -49.9 to -2.02), this dropped to -1.0 (95% CI -24.9 to 22.9) following additional adjustment for smoking. Using anxiety as the exposure variable we found similar results (details available from the authors).
Following adjustment, there was no effect restricted to those with higher symptom scores; mothers scoring ⩾16 on the EPDS at 18 weeks of pregnancy had babies that were 22.5 g lighter (95% CI -12.5 to 57.4, P=0.207) than those scoring <13.
We repeated these analyses with the outcome categorised into low birth weight at term according to the traditional definition of <2500 g) (Fig. 1). The drop in the estimated odds ratio was greatest following adjustment for smoking. The odds ratio following adjustment for gender, gestation and maternal age was 1.57 (95% CI 1.08-2.29), dropping to 1.38 (95% CI 0.94-2.01) after adjustment for smoking.
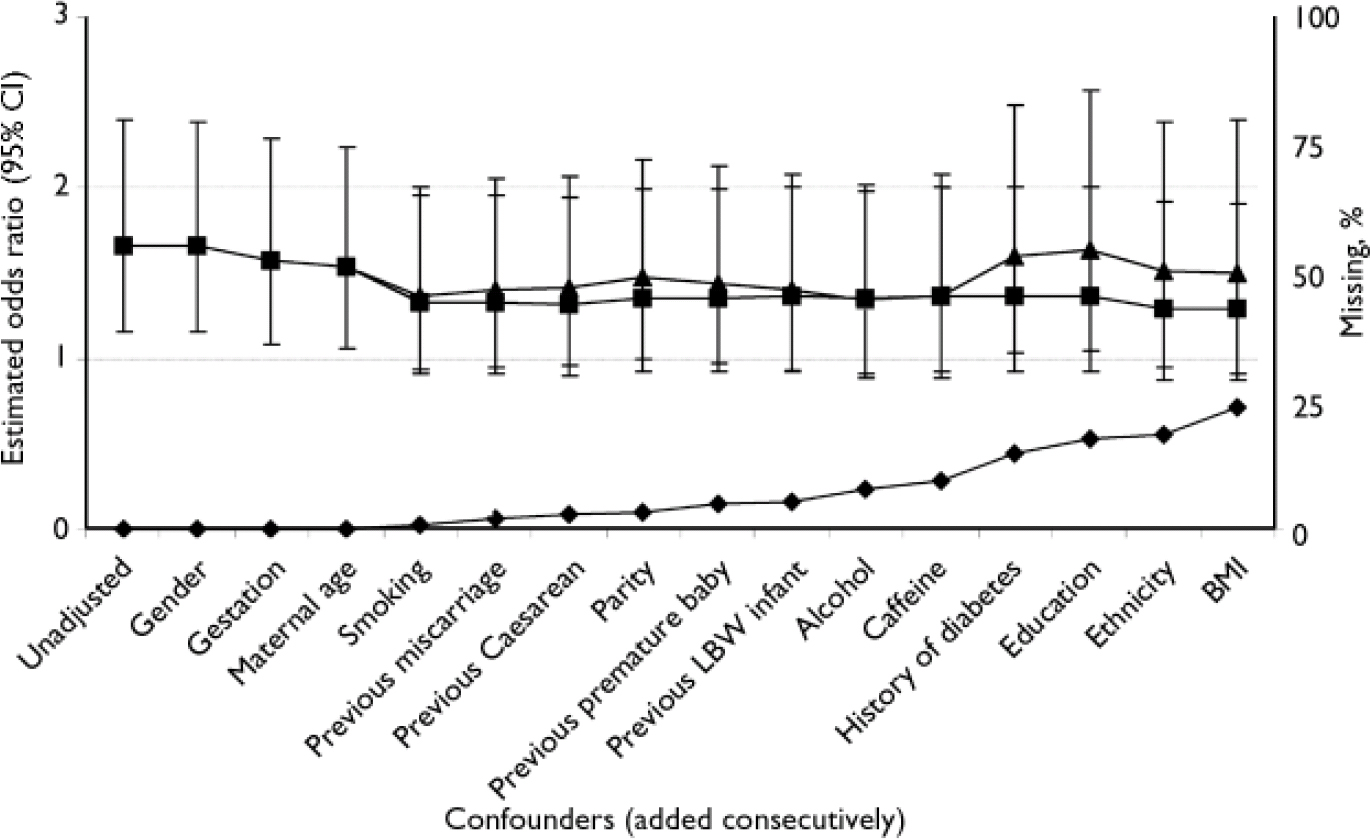
Fig. 1 Odds ratio of low birth weight for offspring of mothers with depression at 18 weeks of pregnancy: effect of adding confounders comparing complete data and including missing data imputed using multiple imputation by chained equation (MICE); —♦—, percentage with missing data when confounders added consecutively; —▴—, complete data; —▪—, MICE estimate. LBW, low birth weight; BMI, body mass index.
With anxiety as the exposure variable we found very similar results to those seen for depression (details available from the authors). We found a weak association with prolonged exposure to depressive symptoms. Those scoring >12 on the EPDS at both 18 and 32 weeks of pregnancy had babies that were 40.2 g lighter (95% CI 3.8-76.6, P<0.05) than those with an EPDS score <13 at both times. This association diminished and was no longer statistically significant following adjustment.
DISCUSSION
This is the largest longitudinal study investigating the association between maternal mood during pregnancy and low birth weight. We found no evidence to support an independent association between depressive or anxiety symptoms during pregnancy and low birth weight at term. There is a widespread assumption that depression and anxiety during pregnancy can impair intrauterine growth. This study challenges that assumption.
This study was large enough to ensure that we could detect small effects. The findings are limited by the use of a self-report measure for depression and by the loss of data from a quarter of participants because of missing data on confounding variables. We conducted sensitivity analyses using multiple imputation for missing data. There was little difference between the results from the analyses using only available data and those including imputed data, suggesting that missing data were unlikely to have substantially biased our findings.
One large retrospective study that found an association between psychiatric disorder at discharge and low birth weight did not measure important confounders such as smoking and was restricted to those with severe mental illness (Reference Kelly, Russo and HoltKelly et al, 2002). Some smaller prospective studies (Reference Copper, Goldenberg and DasCopper et al, 1996; Reference Chung, Lau and YipChung et al, 2001; Reference Andersson, Sundström-Poromaa and WulffAndersson et al, 2004) reported no association of depression in pregnancy and various measures of intrauterine growth restriction, although one (Reference Copper, Goldenberg and DasCopper et al, 1996) reported an association of low birth weight with a measure of perceived stress during pregnancy. These studies were too small to exclude modest effects and interpretation is complicated by the inclusion of preterm births. Some studies have found an association between depressive symptoms and preterm birth (Reference Orr, James and Blackmore PrinceOrr et al, 2002). Adjusting for gestation might not be sufficient to distinguish risk factors for intrauterine growth restriction from those for preterm birth. We addressed this problem by restricting our analyses to babies born at term.
In this study we adjusted for a range of confounding variables including smoking. It remains possible that smoking lies on the causal pathway between depression and intrauterine growth restriction. Adjustment for smoking removed any evidence of a direct association between mean birth weight at term and mood during pregnancy.
Although a woman with a high depressive symptom score in the mid trimester of pregnancy has a slightly increased risk of having a low birth weight infant, this is most likely to be owing to health behaviours associated with depressive symptoms.
Low birth weight at term is only one marker of foetal development. Studies in animals suggest there are long-term effects of exposure to prenatal stress (Reference Barbazanges, Piazza and Le MoalBarbazanges et al, 1996). It is possible that psychological symptoms during pregnancy have other effects on development of offspring that only become apparent after birth. This remains an important area for investigation (Reference O'Connor, Heron and GoldingO'Connor et al, 2002).




eLetters
No eLetters have been published for this article.