Both cognitive and neurobiological models propose that a critical factor in the development of psychosis is the faulty appraisal or interpretation of anomalous experiences or events (Reference Garety and FreemanGarety & Freeman, 1999; Reference Freeman, Garety and KuipersFreeman et al, 2002; Reference KapurKapur, 2003; Reference Broome, Woolley and TabrahamBroome et al, 2005a ; Reference FreemanFreeman, 2007; Reference Garety, Bebbington and FowlerGarety et al, 2007). One aspect of appraisal, reasoning, can be studied using the ‘Beads’ paradigm, in which the subject is shown a series of different coloured beads and is required to guess which of two jars they have been drawn from. Patients with psychotic disorders require fewer beads to be drawn before they are sure of their source than controls, yet are not any less accurate. This ‘jumping to conclusions’ response style has been interpreted as reflecting a data gathering reasoning bias. As well as in patients with psychosis, jumping to conclusions has been described in volunteers with high levels of delusional ideation (Reference Linney, Peters and AytonLinney et al, 1998) and the relatives of patients with psychosis (Reference Van Dael, Versmissen and JanssenVan Dael et al, 2006). In all these groups jumping to conclusions has been particularly associated with the intensity of delusional ideation (Reference Linney, Peters and AytonLinney et al, 1998; Reference Garety and FreemanGarety & Freeman, 1999; Reference Peters, Joseph and GaretyPeters et al, 1999; Reference Garety, Freeman and JolleyGarety et al, 2005; Reference Van Dael, Versmissen and JanssenVan Dael et al, 2006). The mechanisms underlying jumping to conclusions are unclear, but it has been investigated in relation to an impaired ability to hold information online (Reference Dudley, John and YoungDudley et al, 1997a ) and to an inability to tolerate ambiguity (Reference Colbert and PetersColbert & Peters, 2002).
We tested the hypothesis that participants with an at-risk mental state would be more likely to jump to conclusions than controls. Secondary predictions were that the tendency to jump to conclusions would be associated with impaired working memory and an intolerance of uncertainty, and would predict the severity of abnormal beliefs.
METHOD
People with ‘prodromal’ symptoms of psychosis have a 25–40% risk of developing a psychotic disorder in the next 12 months (Yung et al, Reference Yung, Phillips and McGorry1998, Reference Yung, Phillips and Yuen2003; Reference Miller, McGlashan and RosenMiller et al, 2003) and thus have an at-risk mental state. Individuals with an at-risk mental state were recruited from Outreach and Support in South London (OASIS) (Reference Broome, Woolley and JohnsBroome et al, 2005b ). All met PACE criteria (Reference Yung, Phillips and YuenYung et al, 2003) for the at-risk mental state: an individual can meet criteria for this state in one or more of three ways. First, a recent decline in function coupled with either schizotypal personality disorder or a first-degree relative with psychosis. Second, ‘attenuated’ positive symptoms and third, a brief psychotic episode of less than 1 week's duration that resolves without antipsychotic medication. Each participant was assessed by two experienced clinicians using the Comprehensive Assessment for the at-risk mental state (CAARMS; Reference Yung, Phillips and YuenYung et al, 2003), and the diagnosis was confirmed at a consensus meeting with the clinical team. None of the participants had been exposed to antipsychotic medication.
Healthy volunteers (n=23) were recruited via advertisements in the local media.
All participants lived in the same borough of London (Lambeth), were native speakers of English and were right-handed. The groups were matched on sociodemographic variables. Participants were excluded if there was a history of neurological disorder or if they met DSM–IV criteria for a substance misuse or dependence disorder.
Assessment of psychopathology
Psychopathology was assessed using the CAARMS, the Peters' Delusions Inventory (PDI; Reference Peters, Joseph and GaretyPeters et al, 1999), the Positive and Negative Symptom Scale (PANSS; Reference Kay, Fiszbein and OplerKay et al, 1987) and the delusion subscale of the Scale for the Assessment of Positive Symptoms (SAPS; Reference AndreasonAndreason, 1984).
Reasoning task
The tendency for participants to ‘jump to conclusions’ was examined using a modified version of the ‘beads’ reasoning task (Reference Garety and FreemanGarety & Freeman, 1999; Reference FreemanFreeman, 2007). In the beads task, participants are shown two jars of coloured beads, informed of the relative proportions of beads in each, then told that they will be shown a series of beads drawn from one of the jars. They are then asked, on the basis of the observed sequence, to judge which jar is the source of the beads, and to be ‘as certain as possible’, but it is never possible to be completely certain as to which jar the beads have been drawn from (Reference Huq, Garety and HemsleyHuq et al, 1988; Reference Garety and FreemanGarety & Freeman, 1999).
As in the classical version of the paradigm, participants in our study were informed that a series of beads would be drawn from one of two jars containing beads of two colours in the ratios 85:15 and 15:85. They were instructed to monitor the colours of successively drawn beads until they were as certain as they could be as to which of the jars the beads were being drawn from. A pseudo-random predetermined list was used to determine the colour of bead shown. Beads were presented on a computer screen at 1s intervals, with participants responding via a button press. The modified version involved 3 conditions: (a) 2 jars with bead ratios of 85:15, (b) 2 jars with 60:40 and (c) 3 jars with 44:28:28. Participants were asked to indicate which jar the beads were being drawn from when they were ‘as certain as possible’. Real jars of beads in the appropriate ratios and colours were shown to the subjects when the task was being explained beforehand.
Working memory
The ability to hold information about bead colour online was assessed using an adaptation of the digit span task that used a string of different coloured beads (between 5 and 9; as in the beads task) rather than numbers. Participants were presented with 5 different length strings of coloured beads, 2 trials of each, using a laptop. Beads were presented at 1 s intervals and after presentation participants were asked to recall the order of the colour in which beads were presented. Longest span of beads and total errors were recorded.
Tolerance of uncertainty
Tolerance of uncertainty was evaluated using the Freeston Intolerance of Uncertainty scale (Reference Freeston, Rheaume and LetarteFreeston et al, 1994). This questionnaire is a 27-item Likert scale and was designed to generate a single summary score and cover a wide range of concepts, but factor analyses of the scale identified constructs covering ‘behavioural attempts to control the future and avoid uncertainty, inhibition of action, emotional reactions such as frustration and stress, and cognitive interpretations that being uncertain reflects badly on a person’ (Reference Freeston, Rheaume and LetarteFreeston et al, 1994; p. 799). Intolerance of uncertainty is conceptualised as a manifestation of basic dysfunctional (trait) schema that may in turn guide information processing and appraisal. It can generate and maintain anxiety in ambiguous situations both through facilitating the perception of difficulties where none exist, and where difficulties do exist, lead to inefficient responses to them.
IQ
Premorbid and current intellectual function was estimated using the National Adult Reading Test (NART; Reference Nelson and WillisonNelson, 1991) and the Quick test (Reference Ammons and AmmonsAmmons & Ammons, 1962).
RESULTS
Descriptive statistics and comparisons of means
Controls and participants at risk were matched on a measure of current IQ as measured by the Quick test: controls 104.7 (s.d.=13.4); at-risk mental state 100.1 (s.d.=9.8) and on age: controls 24.9 years (s.d.=3.0); at-risk mental state 24.2 years, (s.d.=4.3), but differed on premorbid IQ as estimated by the NART: controls 110.9 (s.d.=7.3) and at-risk mental state 102.3 (s.d.=10.6). Participants with at-risk mental state had a mean PANSS total score of 52.1 (s.d.=14.5), and the positive symptom sub-scale was 12.2 (s.d.=3.9). For the delusion sub-scale of the SAPS, the at-risk mental state group had a mean score of 3.9 (s.d.=4.0).
Beads task
There was no significant difference in performance of the participants with at-risk mental state subjects in comparison to the control group on the classical (or ‘easy’) version of the beads task: the mean number of beads viewed by participants with at-risk mental state before they responded was 7.4 compared to 6.4 for controls (Table 1, Fig. 1). However, on both of the harder versions of the task (60:40 and 44:28:28) the at-risk mental state group drew fewer beads than controls before responding. For the intermediate version of the task the mean number of beads viewed by participants with at-risk mental state before they responded was 8.5, but for controls was 13.4 (P<0.001). On the hard version of the task, those with at-risk mental state viewed 12.5 beads and controls 17.5 (P=0.012). (Fig. 1, Table 1). Both these differences in performance remained significant after co-varying for differences in NART score.
Table 1 Beads task performance by task difficulty and group
| Controls (n=23) | Participants with at-risk mental state (n=35) | P | |
|---|---|---|---|
| mean (s.d.) | |||
| Easy — 85:15 | 6.4 (3.3) | 7.4 (4.4) | NS |
| Intermediate — 60:40 | 13.4 (5.9) | 8.5 (3.7) | < 0.001 |
| Hard — 44:28:28 | 17.5 (8.1) | 12.5 (5.7) | 0.012 |
Delusional ideation
There were highly significant differences between the at-risk mental state and control groups on the total PDI score, and on each of the distress, preoccupation and conviction sub-scales. On all these measures the at-risk mental state group scored higher than controls. (Table 2).
Table 2 Group comparison for delusional ideation, intolerance of uncertainty, Bead span and errors on Bead span
| Controls (n=23) | Participants with at-risk mental state (n=35) | P | |
|---|---|---|---|
| mean (s.d.) | |||
| PDI total | 29.2 (26.0) | 99.0 (57.0) | 0.000 |
| PDI distress | 9.0 (10.3) | 34.4 (23.0) | 0.000 |
| PDI preoccupation | 8.9 (7.7) | 32.4 (20.7) | 0.000 |
| PDI conviction | 11.5 (9.1) | 32.1 (16.2) | 0.000 |
| Intolerance of Uncertainty | 58.3 (15.3) | 79.8 (22.8) | 0.000 |
| Maximum bead span | 7.8 (0.6) | 6.6 (1.0) | 0.000 |
| Total errors on bead span | 3.7 (3.4) | 10.2 (8.9) | 0.001 |
Working memory
The at-risk mental state group had a significantly shorter span for correct responses than controls on the beads span task, and made significantly more errors (Table 2).
Intolerance of uncertainty
The at-risk mental state group had significantly higher ratings on the Freeston Intolerance of Uncertainty scale than controls (Table 2).
Correlations with beads task performance
PDI scores
For both groups on both the intermediate and hard conditions of the beads task there was an inverse relationship between the number of beads viewed before the response and scores on the PDI and each of its sub-scales. These were statistically significant for the total PDI score and all three PDI sub-scales on intermediate (60:40) version of the task and evident as trends for the hard version (Table 3). The strongest and most significant correlation was with scores on the conviction sub-scale of the PDI. There were no significant correlations between performance on the easy (85:15) version and any of the PDI measures.
Table 3 Correlations with performance (beads drawn) on the intermediate1 and hard2 versions of the bead task across all groups (i.e. at-risk mental state and controls).3
| PDI total | PDI distress | PDI preoccupation | PDI conviction | Intolerance of Uncertainty | |
|---|---|---|---|---|---|
| Pearson correlation, r (P) | |||||
| Beads — intermediate1 | -0.331 (0.019) | -0.275 (0.05) | -0.325 (0.021) | -0.375 (0.007) | -0.322 (0.019) |
| Beads — hard2 | -0.237 (0.097) | -0.196 (0.171) | -0.244 (0.88) | -0.258 (0.071) | -0.242 (0.081) |
Intolerance of uncertainty
In both groups the number of beads viewed was inversely related to the Intolerance of Uncertainty score, with a significant correlation on the intermediate version and a trend on the hard version of the task (Table 3).
Symptom scores
Within the at-risk mental state group there were no significant or trend correlations between task performance (on any version) and either the PANSS (both total score and positive sub-scale), or the delusion sub-scale of the SAPS.
Working memory
There were no significant correlations between performance on the beads task and the bead span across both groups of participants combined, but there were correlations within each group. In controls the number of beads drawn in all versions of the task was directly correlated with the number of errors on the bead span task, although this only reached significance on the intermediate version (Table 4). Conversely, in the at-risk mental state group there was a negative correlation between beads viewed and errors on the bead span task. Again this was only significant on the intermediate version of the task (Table 4).
Table 4 Pearson correlations with bead span errors by group and task difficulty
| Controls (n=23) | Participants with at-risk mental state (n=35) | |
|---|---|---|
| Pearson correlation r (P) | ||
| Easy | 0.277 (0.213) | -0.143 (0.452) |
| Intermediate | 0.444 (0.039) | -0.562 (0.0.001) |
| Hard | 0.237 (0.289) | -0.279 (0.135) |
DISCUSSION
Jumping to conclusions
Our first hypothesis was confirmed in that the at-risk mental state group demonstrated a jumping to conclusions style of thinking, although this was evident when the task demands were increased by making the proportions of the respective beads more similar (60:40) or by introducing a third colour of bead (44:28:28), rather than during the ‘classic’ (85:15) version. Our findings are consistent with those of Linney et al (Reference Linney, Peters and AytonLinney et al, 1998), who reported that non-clinical individuals with high scores on the PDI showed a jumping to conclusions response style, although in that case differences were evident using the classical version of the task. Our findings are also consistent with work demonstrating an association between a jumping to conclusions bias and both psychosis liability (as indexed by family history of psychosis and/or psychotic experiences) and delusional ideation (Reference Linney, Peters and AytonLinney et al, 1998; Reference Peters, Joseph and GaretyPeters et al, 1999; Reference Van Dael, Versmissen and JanssenVan Dael et al, 2006). While the jumping to conclusions style of thinking in subjects at very high risk of psychosis has not been examined before, the at-risk mental state has been associated with deficits in working and episodic memory and executive functions (Reference Wood, Pantelis and ProffittWood et al, 2003; Reference Brewer, Francey and WoodBrewer et al, 2005; Reference Broome, Matthiasson and Fusar-PoliBroome et al, 2007, submitted – further information available from author). Further, recent work on the bias in groups at differing liability to psychotic illness, has revealed a dose–response relationship between the jumping to conclusions bias and both delusional ideation and psychosis liability (Reference Van Dael, Versmissen and JanssenVan Dael et al, 2006); leading to the suggestion that the jumping to conclusions bias is both a trait and state variable in the risk and progression of psychosis.
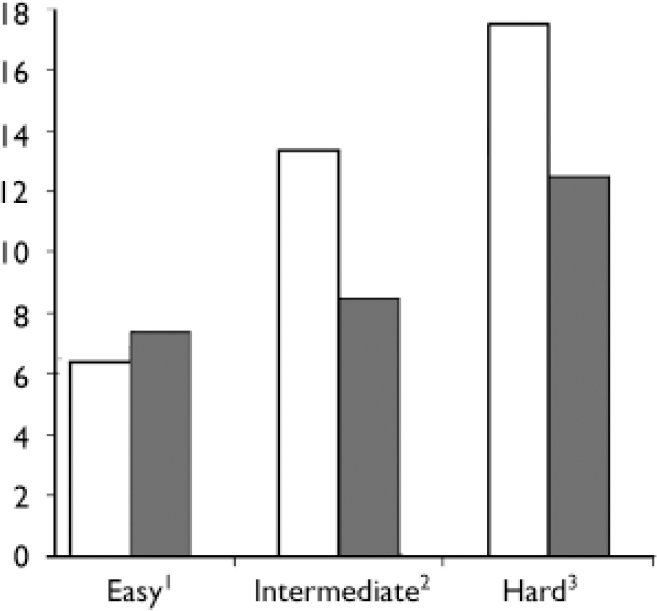
Fig. 1 Draws to decision by task difficulty and group. ░, at-risk mental state group; □, controls.
The finding that jumping to conclusions bias is present in those at high risk of psychosis is consistent with cognitive models that suggest that the faulty appraisal of anomalous experiences plays a fundamental role in the development of the disorder (Reference Broome, Woolley and TabrahamBroome et al, 2005a ; Garety et al, Reference Garety, Freeman and Jolley2005, Reference Garety, Bebbington and Fowler2007). While ‘jumping to conclusions’ has consistently been found in patients with established psychosis (Reference Garety and FreemanGarety & Freeman, 1999), its presence in individuals at very high risk of the disorder suggests that the presence of this impairment may influence whether an individual who is experiencing psychotic symptoms progresses to frank psychosis. Van Dael and colleagues (Reference Van Dael, Versmissen and Janssen2006) suggest that the jumping to conclusions bias, as well as being a trait vulnerability, may have a state component and one would expect such a bias to increase, and be detectable at lower levels of task demand, as at-risk mental state participants made the transition to psychosis. Conversely, those in whom the at-risk mental state remitted may demonstrate an attenuation of the jumping to conclusions bias. This could be tested in a longitudinal study of subjects with an at-risk mental state.
Jumping to conclusions and the severity of abnormal beliefs
Consistent with previous studies (Reference Garety, Freeman and JolleyGarety et al, 2005), we found that jumping to conclusions response style was associated with the severity of abnormal beliefs, as indexed by the PDI. However, this finding was evident across all subjects, rather than being specific to the at-risk mental state group. This is further evidence that rather than being a correlate of frank psychosis, the tendency to jump to conclusions may vary continuously across clinical categories. The association with delusions does not seem simply to reflect jumping to conclusions in those subjects with the most psychotic symptoms, as there was no correlation with either the total PANSS score or the positive symptom sub-scale, or with the SAPS delusion sub-scale score. A specific association with delusions is consistent with studies in established psychosis (Reference Garety and FreemanGarety & Freeman, 1999) and has face validity, in that of all the psychotic symptoms, abnormal beliefs are the most dependent on the participant's interpretation of his experiences. A parsimonious interpretation of the data would be that jumping to conclusions is a sign of faulty appraisal, which is the basis of delusional beliefs, regardless of whether these are held by an individual with psychosis, at-risk mental state, or without psychosis. According to this model, the worse the jumping to conclusions, the more severe the appraisal problem and the more severe the delusions. Faulty appraisal may not distinguish people with psychotic symptoms from people with a psychotic illness in a categorical way, rather faulty appraisal may underlie the subset of psychotic symptoms that depend on the conscious evaluation of sensory/internal information, i.e. delusional beliefs (and perhaps hallucinations), as opposed to the syndrome of psychosis. Appraisal and jumping to conclusions may be less relevant to psychotic symptoms that are less dependent on the conscious appraisal of experiences, for example formal thought disorder, negative symptoms.
Jumping to conclusions and intolerance of uncertainty
The basis of the data gathering bias is unclear. One factor may be the decision-making style of the individual. Although jumping to conclusions is not simply related to impulsivity (Dudley et al, Reference Dudley, John and Young1997a , Reference Dudley, John and Young b ), it may be more evident in individuals who find it difficult to tolerate ambiguity (Reference Colbert and PetersColbert & Peters, 2002). The at-risk mental state group scored higher on the Intolerance of Uncertainty scale than controls. Difficulties tolerating uncertainty may thus have contributed to the jumping to conclusions response style in the at-risk mental state group. As with the PDI, there was a significant correlation across both groups between intolerance of uncertainty and the data gathering bias. The group differences in tolerating uncertainty may be related to the relatively high prevalence of personality and neurotic disorder among participants with at-risk mental state (Reference Broome, Woolley and JohnsBroome et al, 2005b ).
Jumping to conclusions and working memory
Another factor that could contribute to jumping to conclusions is impaired working memory, with subjects making earlier decisions because of difficulties holding material that would inform their judgement online, although the evidence for this is limited. Consistent with previous studies of working memory in participants with at-risk mental state (Reference Wood, Pantelis and ProffittWood et al, 2003; Reference Brewer, Francey and WoodBrewer et al, 2005; Brett et al, 2007, in press), the at-risk mental state group displayed poorer performance on the bead span task than controls. This is consistent with our prediction that impaired working memory would contribute to a jumping to conclusions response style. Moreover jumping to conclusions on one of the harder versions (60:40 bead ratio) of the beads task in the at-risk mental state group was correlated with impaired performance on the beads span task. These data suggest that a difficulty in holding information online may contribute to participants making judgements in which they can never be certain sooner than they might do otherwise. Dudley et al (Reference Dudley, John and Young1997a ) did not find an association between jumping to conclusions response style and memory impairments in patients with psychosis, but this may reflect the use of the classical beads task without the more difficult conditions, or the fact being reminded of the beads one has seen does not guarantee that that information is itself able to be utilised in reasoning. In the present study, the effect of memory impairment was divergent in the two groups: in the control group, there was an increased conservatism and caution in those with poorer ability to recall sequences of beads, the opposite to what was evident in the at-risk mental state group. This suggests that controls with poor working memory compensated by seeking more information, or did not find being uncertain how to respond as aversive as the participants at-risk.
In summary, people who are at high risk of psychosis display a jumping to conclusions reasoning style which is associated with a difficulty in tolerating uncertainty and impaired working memory. A reasoning bias may be a critical factor in the development of clinically significant psychotic phenomena and contribute to the high risk of frank psychosis in this group. More generally, the findings are compatible with data from structural (Reference Pantelis, Velakoulis and McGorryPantelis et al, 2003) and functional neuroimaging (Reference Morey, Inan and MitchellMorey et al, 2005; Reference Broome, Matthiasson and Fusar-PoliBroome et al, 2007, submitted – further information available from author) and neuropsychological studies (Reference Wood, Pantelis and ProffittWood et al, 2003; Reference Brewer, Francey and WoodBrewer et al, 2005 in subjects with an at-risk mental state, which broadly indicate that this group displays abnormalities that are qualitatively similar to those seen in patients with schizophrenia but quantitatively less severe. Approximately one third of those with an at-risk mental state will develop psychosis (Reference Yung, Phillips and YuenYung et al, 2003; Reference Morrison, French and WalfordMorrison et al, 2004; Reference Broome, Woolley and TabrahamBroome et al, 2005a ). We are currently in the process of following up our at-risk mental state sample to establish whether task performance predicts development of psychosis subsequent to testing.
Acknowledgements
Special thanks go to all those who took part in the study and the staff of the OASIS team.
The study was supported by the Guy's and St Thomas' Charitable Foundation and the Mental Health Foundation. Modification, piloting of the task, and initial data collection was carried out when M.R.B. was supported by the South London and Maudsley NHS Trust as Maudsley Research Registrar to the Institute of Psychiatry.








eLetters
No eLetters have been published for this article.