Given the opportunity, general practitioners (GPs) refer patients with common mental disorders to community mental health nurses, also known as community psychiatric nurses, effectively using them as counsellors (Reference Sibbald, Addington-Hall and BrennemanSibbald et al, 1993; Reference Naji, Naji and DonaldNaji et al, 1997; Reference Badger and NolanBadger & Nolan, 1999; Reference Crawford, Carr and KnightCrawford et al, 2001). However, this may not be cost-effective as these problems are often self-limiting. One previous trial of community mental health nurse care v. usual GP care demonstrated no clinical or economic advantage (Gournay & Brooking, Reference Gournay and Brooking1994, Reference Gournay and Brooking1995), but had a small sample size and high drop-out rate, and reported only one comparison at 6 months, possibly missing short-term benefits. Referral may be ineffective because community mental health nurses do not offer specific treatment for common mental disorders. Problem-solving treatment has been shown to be effective for depression in primary care (Reference Mynors-Wallis, Gath and DayMynors-Wallis et al, 2000) but was less effective for common mental disorders when delivered by non-mental health nurses (Reference Mynors-Wallis, Davies and GrayMynors-Wallis et al, 1997). We compared usual GP care for common mental disorders with generic community mental health nurse care and nurse problem-solving treatment, measuring effectiveness and costs.
METHOD
We compared, in a pragmatic three-arm randomised controlled trial, the effectiveness of usual GP care with generic community mental health nurse care, and with problem-solving treatment from specially trained community mental health nurses, in reducing symptoms and improving social function and quality of life. The methods have been described in detail previously (Reference Simons, Mynors-Wallis and PickeringSimons et al, 2001). We also undertook a cost-effectiveness comparison of usual GP care with each of the community mental health nurse treatments, evaluating not only the direct costs of treatment but also patient costs, including time off work.
Setting
Community mental health nurses were recruited from four mental health trusts serving the counties of Hampshire and Dorset, including city, suburban and rural populations. All nurses working in adult community mental health teams were asked whether they would participate. All general practices in the teams' catchment areas were also invited to participate.
Ethical approval
Approval was granted by the four local research ethics committees covering the trusts' catchment areas: Southampton & South West Hampshire; Isle of Wight, Portsmouth & South East Hampshire; North & Mid Hampshire; and East Dorset.
Inclusion and exclusion criteria
Inclusion criteria were: age between 18 and 65 years; a new episode of anxiety, depression or reaction to life difficulties; duration of symptoms 4 weeks to 6 months; and a score of 3 or more on the General Health Questionnaire 12-item version (GHQ-12; Reference Goldberg and BlackwellGoldberg & Blackwell, 1970). Exclusion criteria were: current contact with psychiatric services; current psychological treatment; severe mental disorder or substance misuse; dementia; active suicidal ideas; and lack of sufficient English to participate.
Recruitment
Suitable patients were identified by GPs during usual consultations and referred by fax. Participants were contacted within a few days, to obtain written informed consent and carry out the baseline interview.
Randomisation and masking
All community mental health nurses recruited from a particular trust were initially randomised to either the generic or the problem-solving treatment arms. As nurses dropped out during the study, later recruits were purposefully allocated to the two arms in order to ensure availability of both types of nurse intervention in all trust areas. Randomisation of patients was carried out by the study coordinator, through a telephone service provided by the University of York, and was stratified by referring GP, with a variable block size between three and six. Assessments were undertaken by research assistants, who as far as possible were masked to patient allocation. However, recognising that masking might be impossible to ensure, all patient assessments were self-completed, to avoid interviewer bias.
Interventions
Treatment in the usual GP care arm was left to the individual GP, except that GPs were asked not to refer patients for psychological treatments during the first 8 weeks of the study period.
Nurses in the generic nurse treatment arm were asked to use whatever treatments they thought appropriate for the patient's problems. They were asked to spend up to 1 h on an initial assessment and then to give up to five follow-up sessions, of approximately 30-45 min duration.
The nurses in the problem-solving treatment arm were asked to provide the same number and duration of sessions as those in the generic arm. Problem-solving treatment is a brief, structured intervention comprising seven stages: explanation of the treatment and its rationale; clarification and definition of problems; choice of achievable goals; generation of alternative solutions; selection of preferred solutions; clarification of the necessary steps for implementing them; and evaluation of progress. Training was undertaken by experienced problem-solving treatment therapists, and included an initial 3-day course, treatment of five patients under supervision and a follow-up day. Ongoing supervision was provided fortnightly by experienced therapists.
Nurses in both arms were asked to audiotape their sessions with patients so that fidelity to problem-solving treatment could be assessed and interventions offered by the generic arm could be described.
All patients remained free to consult their GPs throughout the study, and to be prescribed psychotropic drug treatments as the GP thought fit.
Outcome measures
Assessments were made at baseline and at 8 and 26 weeks after entry. The primary outcome measure was psychiatric symptoms on the self-completed Clinical Interview Schedule - Revised (CIS-R; Reference Lewis, Pelosi and ArayaLewis et al, 1992), computerised (PROQSY 3) version. This schedule, reliable in primary care, provides a total symptom score and a diagnosis according to the tenth revision of the International Classification of Diseases (ICD-10; World Health Organization, 1993).
The GHQ-12 and Hospital Anxiety and Depression Scale (HADS; Reference Zigmond and SnaithZigmond & Snaith, 1983) were administered to explore whether these rapid self-completed questionnaires could predict which patients might benefit from community mental health nurse treatment.
Social outcome was measured using the self-report Social Adjustment Scale (SAS), which is a 45-item scale measuring functioning in seven role areas (Reference Cooper, Osborn and GathCooper et al, 1982).
Patient satisfaction was measured at 26 weeks using a self-report questionnaire specially designed for the evaluation of problem-solving treatment, and used in a previous study (Reference Mynors-Wallis, Davies and GrayMynors-Wallis et al, 1997). Patients rated on a five-point scale their agreement with 10 statements about the quality of treatment they received, giving a total score between 10 and 50.
Quality-adjusted life-years were used as the main outcome measure in the economic evaluation. Health-related quality of life was assessed using the EuroQol ES-5D instrument (EQ-5D Group, 1990), and from this utility levels were estimated using a published tariff of utility weights (Reference DolanDolan, 1997). Quality-adjusted life-years were calculated as the area under the curve from the health utility profile described by the EQ-5D utilities, assuming a linear interpolation between the values.
Costs
A cost-utility analysis from National Health Service (NHS) and societal perspectives was undertaken. The analysis was confined to the study period of 26 weeks, hence discounting was not necessary. Data on all healthcare resources and employment-related costs were collected from community mental health nurses and by using a specifically designed self-reported questionnaire given to patients at baseline, 8 and 26 weeks' follow up. The questionnaire gathered information on GP consultations, number and type of medications prescribed, nurse treatment delivered, nurse supervision, hospital care, care and treatments purchased by patients and the number of days off work for patients in paid employment. Nurses had to be trained in problem solving (see ‘Interventions’ above), and a portion of the cost of this based on expected total case-load was allocated to patients in the study. Days off work were valued using average national earnings according to gender. Information on health service use was also extracted from patients' GP records. The total cost of care per patient was calculated by summing the product of each resource use category and its associated unit costs. Unit costs (in 2003 pounds sterling) were obtained from four national sources to ensure generalisability: Unit Costs of Health and Social Care (Reference Netten, Dennett and KnightNetten et al, 2002), NHS Trust Financial Returns (Department of Health, 2000a ), New Earnings Survey (Office for National Statistics, 2003) and British National Formulary (British Medical Association & Royal Pharmaceutical Society of Great Britain, 2003).
Sample size calculation
The original sample size calculation was based on showing a difference of 4-points on the CIS-R between the groups. Given this difference, and a standard deviation (s.d.) of 10 points, as in a previous community nurse problem-solving study (Reference Mynors-Wallis, Davies and GrayMynors-Wallis et al, 1997), 121 patients followed up in each group would give 80% power for the main comparisons, using a two-sided test at the 2.5% level of significance (Bonferroni correction for multiple testing). After 12 months of slower than anticipated recruitment, we resized the study according to the actual CIS-R scores obtained for the first 60 patients recruited. The s.d. was 10.6, but the mean was 25, considerably higher than the mean of 19 in the study on which the original calculation was based. In view of the higher initial scores, we thought larger differences might be found. The sample size was recalculated using an expected difference of 5 points, concluding that 65 patients completing follow-up in each arm would give 80% power for the main comparisons, at the 5% significance level. To ensure 65 completers in each arm, allowing for the 20% drop-out rate found among the first 60 patients, 246 patients needed to be recruited.
Analysis of effectiveness
The primary outcome, CIS-R score, was compared between each of the two nurse groups and the usual GP care group, in an analysis of covariance, by intention to treat, incorporating baseline CIS-R scores and the referring GP, with separate analyses for the 8- and 26-week assessments. Mean differences with 95% confidence intervals (CIs) were estimated. The other clinical and social outcome measures were analysed in the same way.
Economic analysis
Mean cost differences with 95% CIs were also calculated for the two comparisons. Because of the expected skewness in the distribution of cost data, non-parametric bootstrapped CIs were computed (Reference Briggs and GrayBriggs & Gray, 1999). Generic nurse care and nurse problem-solving treatment were each compared with usual GP care, using an incremental analysis expressed as the net difference in cost divided by the net difference in quality-adjusted life-years. Uncertainty concerning this cost-effectiveness ratio was presented as a 95% confidence ellipse (Reference van Hout, Al and Gordonvan Hout et al, 1994) and plotted on the cost-effectiveness plane, a chart used to plot the incremental differences in costs and effects on a four-quadrant plane. Each quadrant represents different possibilities for the decision maker (Reference Stinnett and MullahyStinnett & Mullahy, 1997).
RESULTS
Between May 2000 and September 2001, 53 community psychiatric nurses were recruited, from approximately 200 approached, of whom 29 were assigned to the generic nurse care arm, and 24 to the nurse problem-solving treatment arm. Of 1130 GPs approached 98 referred patients, from 62 practices. Mean practice list size was 8601 patients (range 2240-27 239) and mean doctors per practice 5 (1-15); 18 practices (29%) were in urban, 33 (53%) were in suburban and 11 (18%) were in rural locations.
Recruitment
Figure 1 shows patient flow through the trial. Overall, 247 patients were randomised between February 2001 and April 2003. The imbalance between arms, more patients being randomised to problem-solving treatment, arose by chance and was owing to stratification by practitioner, because several referred only one or two patients each.

Fig. 1 Flow diagram of patient progression through the trial. Post/Tel, follow-up only by postal questionnaire or telephone interview; GP, general practitioner; CMHN, community mental health nurse; PST, problem-solving treatment.
Of 53 nurses recruited, 37 received referrals (referrals were slower in some areas than others, and some nurses left the study before patients could be assigned to them). Patients allocated per nurse ranged from 0 to 16 (mean 3.2). Of 169 patients allocated to nurse treatment, 156 attended at least one session. In the generic care arm, 0-8 sessions were given, mean 4.4 (s.d.=2.2); and in the problem-solving treatment arm 0-7 treatments were given, mean 4.1 (s.d.=2.0). In the generic arm 73% of patients received four or more therapy sessions, compared with 62% in the problem-solving arm.
Fidelity of problem-solving treatment delivered
In the event, the nurses audiotaped their sessions with only 30 patients; 7 in the generic community mental health nurse arm and 23 in the problem-solving arm, which was owing to reluctance by the patient or nurse, or both, to be recorded in the majority of cases. Masked rating of these audiotapes by one of the supervisors indicated that problem-solving treatment was being delivered faithfully in the sessions that were recorded. The supervisors also provided feedback that they believed that problem-solving treatment was in general being delivered as faithfully as in previous studies in which they had been involved.
Follow-up rates
Overall follow-up rates were 86% at 8 weeks and 77% at 26 weeks. However, rates were lower in the GP group, where 21% declined at 8 weeks, compared with 4% and 8% in the nursing arms (Fig. 1). Health economic data were extracted from GP medical records for 229 patients (93%); nine did not consent to their records being examined, and nine had incomplete, or no, records available at follow up.
Baseline characteristics
Table 1 shows the sociodemographic characteristics and past psychological history of randomised patients at baseline. There were no obvious differences apparent between groups. Table 2 shows baseline ICD-10 diagnoses generated by the CIS-R.
Table 1 Patient sociodemographic characteristics and past psychological history

| Characteristics and history | GP care (n=78) | Generic CMHN care (n=79) | PST CMHN care (n=90) |
|---|---|---|---|
| Age (years): mean s.d. | 34.9 (11.77) | 34.2 (11.33) | 35.8 (10.92) |
| Range | 18–64 | 18–64 | 18–62 |
| Gender, n (%) | |||
| Male | 24 (31%) | 24 (30%) | 25 (28%) |
| Female | 54 (69%) | 55 (70%) | 65 (72%) |
| Ethnic group, n (%) | |||
| White | 75 (96%) | 76 (96%) | 90 (100%) |
| Other | 3 (4%) | 3 (4%) | 0 (0%) |
| Marital status, n (%) | |||
| Married/cohabiting | 37 (48%) | 46 (58%) | 54 (60%) |
| Widowed/divorced/separated | 14 (18%) | 7 (9%) | 10 (10%) |
| Single | 27 (35%) | 26 (33%) | 26 (29%) |
| Social class | |||
| I | 2 (3%) | 2 (3%) | 4 (4%) |
| II | 22 (28%) | 25 (32%) | 25 (28%) |
| III (non-manual) | 18 (23%) | 22 (28%) | 23 (26%) |
| III (manual) | 14 (18%) | 14 (18%) | 18 (20%) |
| IV | 12 (15%) | 10 (13%) | 12 (13%) |
| V | 5 (6%) | 1 (1%) | 6 (7%) |
| Missing | 5 (6%) | 3 (4%) | 2 (2%) |
| Employment, n (%) | |||
| Full-time work | 36 (46%) | 40 (51%) | 34 (38%) |
| Part-time work | 18 (23%) | 19 (24%) | 25 (28%) |
| Permanently sick/disabled | 2 (3%) | 2 (3%) | 4 (4%) |
| Unemployed | 8 (10%) | 7 (9%) | 11 (12%) |
| Retired | 0 (0%) | 1 (1%) | 0 (0%) |
| Student | 5 (6%) | 3 (4%) | 3 (3%) |
| Housewife | 7 (9%) | 6 (8%) | 10 (11%) |
| Other | 2 (3%) | 1 (1%) | 3 (3%) |
| Highest educational level, n (%) | |||
| None | 7 (9%) | 11 (14%) | 9 (10%) |
| GCSE/O-level/CSE | 45 (58%) | 37 (47%) | 42 (47%) |
| A-level | 11 (14%) | 10 (13%) | 13 (14%) |
| Degree | 14 (18%) | 21 (26%) | 25 (28%) |
| Missing | 1 (1%) | 0 (0%) | 1 (1%) |
| Accommodation status, n (%) | |||
| Owner-occupied | 31 (40%) | 44 (56%) | 51 (57%) |
| Rented | 34 (44%) | 23 (29%) | 31 (35%) |
| Lives with parents | 10 (13%) | 10 (13%) | 7 (8%) |
| Other | 3 (4%) | 2 (3%) | 1 (1%) |
| Number of children, n (%) (16 years or under) | |||
| 0 | 42 (54%) | 47 (60%) | 50 (56%) |
| 1 | 13 (17%) | 12 (15%) | 15 (17%) |
| 2 | 15 (19%) | 13 (17%) | 19 (21%) |
| 3+ | 8 (10%) | 7 (9%) | 6 (7%) |
| Past history: number of previous episodes | |||
| requiring treatment, n (%) | |||
| 0 | 33 (42%) | 28 (35%) | 31 (34%) |
| 1 | 30 (39%) | 26 (33%) | 39 (43%) |
| 2 | 6 (8%) | 12 (15%) | 10 (11%) |
| 3+ | 9 (12%) | 13 (17%) | 10 (11%) |
| Previous drug treatment, n (%) | |||
| Yes | 42 (54%) | 43 (54%) | 50 (56%) |
| No | 3 (4%) | 8 (10%) | 9 (10%) |
| N/A | 33 (42%) | 28 (35%) | 31 (34%) |
| Previous psychological treatment, n (%) | |||
| Yes | 21 (27%) | 36 (46%) | 33 (37%) |
| No | 24 (31%) | 15 (19%) | 26 (29%) |
| N/A | 33 (42%) | 28 (35%) | 31 (34%) |
| Previous electroconvulsive therapy, n (%) | |||
| Yes | 0 (0%) | 1 (1%) | 0 (0%) |
| No | 45 (58%) | 50 (63%) | 58 (64%) |
| N/A | 33 (42%) | 28 (35%) | 31 (34%) |
| Missing | 0 (0%) | 0 (0%) | 1 (1%) |
| Previous in-patient for an emotional or mental health problem, n (%) | |||
| Yes | 2 (3%) | 4 (5%) | 4 (4%) |
| No | 43 (55%) | 47 (60%) | 55 (61%) |
| N/A | 33 (42%) | 28 (35%) | 31 (34%) |
| Family history of treatment for emotional or mental health problems, n (%) | |||
| Yes | 44 (56%) | 40 (51%) | 48 (53%) |
| No | 34 (44%) | 39 (49%) | 42 (47%) |
GP, general practitioner; CMHN, community mental health nurse; PST, problem-solving treatment; N/A, not applicable
Table 2 Baseline CIS–R-generated primary diagnoses
| ICD–10 diagnosis | GP group | Generic CMHN group | PST CMHN group |
|---|---|---|---|
| (n=78) | (n=79) | (n=90) | |
| Severe depressive episode | 6 (8%) | 15 (19%) | 15 (17%) |
| Moderate depressive episode | 17 (22%) | 16 (20%) | 8 (9%) |
| Mild depressive disorder | 2 (3%) | 2 (2%) | 1 (1%) |
| Mixed anxiety and depressive disorder | 16 (20%) | 16 (20%) | 28 (31%) |
| Mixed anxiety and depressive disorder, mild | 17 (22%) | 15 (19%) | 12 (13%) |
| Social phobia | 7 (9%) | 3 (4%) | 12 (13%) |
| Agoraphobia | 4 (5%) | 3 (4%) | 4 (5%) |
| Panic disorder | 4 (5%) | 3 (4%) | 2 (2%) |
| Specific (isolated) phobic disorder | 1 (1%) | 2 (2%) | 0 (0%) |
| Obsessive–compulsive disorder | 0 (0%) | 1 (1%) | 0 (0%) |
| No diagnosis identified | 4 (5%) | 3 (4%) | 8 (9%) |
CIS–R, Clinical Interview Schedule–Revised; GP, general practitioner; CMHN, community mental health nurse; PST, problem-solving treatment
Clinical outcome, social function and quality of life
Table 3 shows the results of the comparisons between groups for clinical outcomes, social function and quality of life. None of the comparisons at either of the follow-up points showed significant differences in effectiveness between arms. The 95 CIs suggest that we can rule out differences between the groups of 6 or more points on the CIS-R scale. At 26 weeks estimated differences and 95% CIs were similar to those at 8 weeks.
Table 3 Comparison of outcomes between treatment groups

| Mean score (s.d.) | Mean difference (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|
| GP (n=51) | Generic CMHN (n=62) | PST CMHN (n=71) | Generic CMHN–GP | PST CMHN–GP | ||||
| Clinical Interview Schedule–Revised total score | ||||||||
| Baseline | 24.7 (9.8) | 27.0 (9.8) | 25.4 (10.3) | |||||
| 8 weeks | 13.8 (13.9) | 16.9 (12.1) | 15.0 (11.4) | 1.40 (–2.79 to 5.60) 1 | –1.21 (–5.23 to 2.80) 1 | |||
| 26 weeks | 10.1 (10.9) | 10.4 (9.4) | 12.8 (12.0) | –1.39 (–5.54 to 2.77) 1 | 1.13 (–2.88 to 5.14) 1 | |||
| General Health Questionnaire (12-item) total score | ||||||||
| Baseline | 10.08 (2.26) | 9.94 (2.30) | 10.03 (2.47) | |||||
| 8 weeks | 3.54 (4.29) | 3.18 (4.44) | 2.79 (4.01) | –0.71 (–2.37 to 0.95) 1 | –1.24 (–2.84 to 0.37) 1 | |||
| 26 weeks | 2.87 (3.93) | 1.78 (2.98) | 2.32 (3.43) | –1.06 (–2.56 to 0.45) 1 | –0.81 (–2.25 to 0.63) 1 | |||
| Hospital Anxiety and Depression Scale depression score | ||||||||
| Baseline | 9.24 (3.83) | 9.96 (3.62) | 10.04 (4.23) | |||||
| 8 weeks | 5.62 (4.89) | 5.99 (4.09) | 6.06 (4.50) | –0.62 (–2.20 to 0.96) 1 | –0.92 (–2.46 to 0.63) 1 | |||
| 26 weeks | 4.64 (4.28) | 4.32 (3.28) | 4.71 (4.47) | –0.89 (–2.39 to 0.60) 1 | –0.51 (–0.98 to 0.95) 1 | |||
| Hospital Anxiety and Depression Scale anxiety score | ||||||||
| Baseline | 14.01 (3.39) | 13.42 (3.74) | 13.53 (3.77) | |||||
| 8 weeks | 9.23 (3.95) | 9.77 (3.67) | 9.57 (4.15) | 0.67 (–0.75 to 2.09) 1 | 0.07 (–1.31 to 1.44) 1 | |||
| 26 weeks | 7.57 (4.28) | 8.19 (3.76) | 8.68 (4.54) | 0.93 (–0.73 to 2.59) 1 | 1.58 (–0.02 to 3.18) 1 | |||
| Social Adjustment Scale total score | ||||||||
| Baseline | 2.80 (0.39) | 2.80 (0.39) | 2.84 (0.39) | |||||
| 8 weeks | 2.46 (0.48) | 2.46 (0.37) | 2.50 (0.40) | –0.02 (–0.17 to 0.13) 1 | 0 (–0.14 to 0.14) 1 | |||
| 26 weeks | 2.34 (0.39) | 2.29 (0.38) | 2.44 (0.41) | –0.04 (–0.18 to 0.12) | 0.11 (–0.04 to 0.26) | |||
| EuroQol EQ-5D utility level | ||||||||
| Baseline | 0.70 (0.23) | 0.70 (0.26) | 0.63 (0.29) | |||||
| 8 weeks | 0.83 (0.19) | 0.82 (0.19) | 0.80 (0.19) | –0.01 (–0.07 to 0.07) | –0.03 (–0.10 to 0.05) | |||
| 26 weeks | 0.83 (0.19) | 0.85 (0.17) | 0.81 (0.24) | 0 (–0.06 to 0.07) | –0.04 (–0.12 to 0.04) | |||
| Quality-adjusted life-years gained | ||||||||
| Over the 26 weeks' follow up | 0.40 (0.07) | 0.40 (0.07) | 0.39 (0.09) | 0 (–0.03 to 0.03) | –0.02 (–0.05 to 0.012) | |||
GP, general practitioner; CMHN, community mental health nurse; PST, problem-solving treatment
1. Adjusted for referring general practitioner and baseline value
Table 4 shows that patients in both nurse groups reported significantly higher levels of satisfaction than those in the GP arm.
Table 4 Satisfaction ratings at 26 weeks
| Group | n | Mean score (s.d.) | Unadjusted difference from GP arm | Adjusted difference from GP arm | ||||
|---|---|---|---|---|---|---|---|---|
| Mean (95% CI) | P | Mean (95% CI) | P | |||||
| GP | 48 | 31.6 (7.6) | ||||||
| Generic CMHN | 59 | 37.2 (5.9) | 5.59 (3.13– 8.04) | <0.001 | 5.00 (2.14–7.86) | 0.001 | ||
| PST CMHN | 66 | 37.6 (5.8) | 6.01 (3.61–8.40) | <0.001 | 5.67 (2.89–8.45) | <0.001 | ||
GP, general practitioner; CMHN, community mental health nurse; PST, problem-solving treatment
1. Adjusted for referring general practitioner
Differential follow-up rate
Because of the different follow-up rates in the GP arm compared with the nurse arms, we performed sensitivity analyses exploring whether the results changed depending on assumptions made about missing data. We used five methods to replace missing values: last observation carried forward, back to baseline, mean replacement, mean difference replacement and individual regression lines. The main findings were not particularly sensitive to these analyses. Two of ten comparisons between GP care and generic nursing care achieved statistically significant differences at the 5% level. These comparisons were both of the 26-week CIS-R results, one based on last observations carried forward and one on back to baseline, both of which tended to maximise differences between the groups, as most patients improved over time.
Economic outcomes
Complete resource use data for the 26 weeks were available for 159 patients (64%) (Table 5). The cost-effectiveness results presented were based on 184 patients, for whom complete CIS-R data were available over the 6-month period, using conditional (group and follow-up point) mean imputation to estimate results for 25 patients with CIS-R scores and incomplete resource-use information.
Table 5 Costing resource-use items (costs expressed in 2002/2003 prices), CIS–R complete cases analysis only

| Cost category | GP (n=51) | Generic CMHN (n=62) | PST CMHN (n=71) | Generic CMHN–GP | PST CMHN–GP | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Volume per patient Mean (s.d.) | Cost per patient Mean (s.d.) | Volume per patient Mean (s.d.) | Cost per patient Mean (s.d.) | Volume per patient Mean (s.d.) | Cost per patient Mean (s.d.) | Mean cost difference (95% non-parametric CI) | Mean cost difference (95% non-parametric CI) | ||||
| Intervention | |||||||||||
| Training and supervision | 0 | £0 | £0 | £36 | |||||||
| costs | |||||||||||
| Treatment costs | 0 | £0 | £295 (163) | £267 (114) | £295 (256 to 336) *** | £267 (243 to 294) *** | |||||
| Intervention sub-total (I) | 0 | £0 | £295 (163) | £303 (114) | £295 (259 to 337) *** | £303 (275 to 327) *** | |||||
| Other direct NHS | |||||||||||
| services | |||||||||||
| Medication prescribed | £44 (51) | £36 (53) | £40 (74) | –£8 (–28 to 10) | –£4 (–24 to 18) | ||||||
| GP visits at the surgery | 4.39 (3.67) | £91 (76) | 3.94 (3.22) | £81 (67) | 2.72 (2.14) | £56 (44) | –£9 (37 to 17) | –£35 (–57 to –10) ** | |||
| GP home visits | 0.04 (0.20) | £3 (12) | 0.05 (0.28) | £3 (18) | 0.11 (0.65) | £7 (41) | £0 (–5 to 6) | £4 (–3 to 16) | |||
| GP consultation over the telephone | 0.27 (0.69) | £7 (16) | 0.63 (1.76) | £15 (42) | 0.49 (1.58) | £12 (38) | £8 (–1 to 22) | £5 (–2 to 17) | |||
| Practice nurse visit at the surgery | 0.48 (0.70) | £5 (7) | 0.40 (0.73) | £4 (8) | 0.56 (1.08) | £6 (11) | –£1 (–3 to 2) | £1 (–2 to 4) | |||
| Counsellor at the surgery | 0.57 (1.8) | £18 (57) | 0.11 (0.89) | £4 (29) | 0.21 (1.01) | £7 (31) | –£14 (–34 to 0) | –£11 (–29 to 3) | |||
| Visits to social worker | 0.16 (0.99) | £8 (51) | 0.18 (1.17) | £9 (58) | 0 | £0 | £1 (–14 to 22) | –£8 (–27 to 0) | |||
| Home social worker | 0 | £0 | 0.20 (1.40) | £9 (66) | 0.06 (0.38) | £3 (18) | £9 (0 to 33) | £3 (0 to 8) | |||
| Psychiatrist visit at the hospital clinic | 0.14 (0.40) | £12 (36) | 0.10 (0.43) | £9 (39) | 0.13 (0.51) | £11 (45) | –£4 (–17 to 10) | –£1 (–16 to 13) | |||
| Psychiatrist visit at home | 0.06 (0.31) | £5 (28) | 0 | £0 | 0.10 (0.72) | £9 (65) | –£5 (–19 to 0) | £4 (–10 to 25) | |||
| Psychologist visit | 0.69 (4.48) | £20 (130) | 0 | £0 | 0.10 (0.61) | £3 (18) | –£20 (–74 to 2) | –£17 (–57 to 4) | |||
| Out-patient visit | 0 | £0 | 0.05 (0.22) | £6 (26) | 0.07 (0.49) | £8 (55) | £6 (0 to 11) | £8 (0 to 22) | |||
| Accident and Emergency visit | 0.14 (0.49) | £7 (25) | 0.16 (0.45) | £8 (23) | 0.06 (0.23) | £3 (12) | £1 (–9 to 9) | –£4 (–9 to 9) | |||
| Hospital admissions | 0.16 (0.99) | £27 (171) | 0.08 (0.37) | £14 (65) | 0.16 (0.95) | £27 (165) | –£13 (–78 to 22) | £0 (–74 to 54) | |||
| Other hospital contacts | 0.39 (1.22) | £36 (113) | 0.82 (1.84) | £76 (171) | 1.22 (3.33) | £113 (310) | £40 (–13 to 96) | £77 (10 to 166) ** | |||
| Other direct NHS | £283 (300) | £274 (273) | £305 (500) | –£9 (–120 to 90) | £22 (–113 to 175) | ||||||
| services sub-total (2) | |||||||||||
| Total NHS (1)+(2) | £283 (300) | £569 (350) | £608 (501) | £286 (174 to 411) *** | £325 (204 to 484) *** | ||||||
| Out of pocket (3) | £33 (82) | £30 (55) | £23 (52) | –£3 (–32 to 19) | –£10 (–43 to 12) | ||||||
| Over-the-counter items | |||||||||||
| Other direct NHS services+ | £316 (327) | £303 (291) | £328 (502) | –£13 (–133 to 98) | £12 (–118 to 176) | ||||||
| out-of-pocket (2)+(3) | |||||||||||
| Total cost of care | £316 (327) | £599 (366) | £631 (501) | £283 (154 to 411) *** | £315 (183 to 481) *** | ||||||
| (1)+(2)+(3) | |||||||||||
| Days off work | 10.7 (18.18) | £3787 (7540) | 10.2 (22.7) | £3694 (8464) | 13.8 (27.6) | £5880 (12 727) | –£93 (–3304 to 2843) | £2093 (–1175 to 6013) | |||
CIS–R, Clinical Interview Schedule–Revised; GP, general practitioner; CMHN, community mental health nurse; PST, problem-solving treatment
** P < 0.01
*** P < 0.001
There were no obvious differences found between groups with respect to NHS contacts made in the 4 weeks before randomisation, so adjustment with regard to baseline costs was considered unnecessary.
Table 6 reports summary costs related to the intervention, other direct NHS costs, over-the-counter items and total costs of care by trial arm. Overall, statistically significant additional costs were associated with the two nurse interventions. No significant differences were found between any of the arms in number, or cost, of days off work. Within the treatment-related total costs, differences between arms were statistically significant with respect to treatment and training costs (mean difference between generic nursing care and GP arms £295 per patient (95% CI 259-337), and between nurse problem-solving treatment and GP arms £303 (95% CI 275-327)); GP consultation costs (the problem-solving group had fewer consultations than the GP group (2.72 v. 4.39), yielding a mean cost difference per patient of £35 (95% CI 13-36)); and costs of other hospital contacts (the problem-solving group had more hospital contacts than the GP group (1.22 v. 0.39), yielding a mean cost difference per patient of £77 (95% CI 10-166)).
Table 6 Summary of mean treatment costs, days off work according to arm of study, and cost differences per patient; CIS–R complete cases analysis only (costs expressed in 2002/2003 prices)

| Cost category | GP (n=51) | Generic CMHN (n=62) | PST CMHN (n=71) | Generic CMHN–GP | PST CMHN–GP |
|---|---|---|---|---|---|
| Mean (s.d.) | Mean (s.d.) | Mean (s.d.) | Mean cost difference (95% non-parametric CI) | Mean cost difference (95% non-parametric CI) | |
| Intervention (1) | £0 | £295 (163) | £303 (114) | £295 (259 to 337) *** | £303 (275 to 327) *** |
| Other direct NHS services (2) | £283 (300) | £274 (273) | £305 (500) | –£9 (–120 to 90) | £22 (–113 to 175) |
| Total NHS (1)+(2) | £283 (300) | £569 (350) | £608 (501) | £286 (174 to 411) *** | £325 (204 to 484) *** |
| Out-of-pocket (3) | £33 (82) | £30 (55) | £23 (52) | –£3 (–32 to 19) | –£10 (–43 to 12) |
| Other direct NHS services+out-of-pocket (2)+(3) | £316 (327) | £303 (291) | £328 (502) | –£13 (–133 to 98) | £12 (–118 to 176) |
| Total cost of care (1)+(2)+(3) | £316 (327) | £599 (366) | £631 (501) | £283 (154 to 411) *** | £315 (183 to 481) *** |
| Days off work | £3787 (7540) | £3694 (8464) | £5880 (12727) | –£93 (–3304 to 2843) | £2093 (–1175 to 6013) |
CIS–R, Clinical Interview Schedule–Revised; GP, general practitioner; CMHN, community mental health nurse; PST, problem-solving treatment
*** P < 0.001
An additional analysis was conducted with resource-use information gathered from the GP medical records for 229 (93%) of the patients rather than self-reported data, with conditional mean imputation for missing items. Overall, the results did not change significantly.
Figure 2 shows the incremental costs and effectiveness of nurse problem-solving treatment compared with GP care, and of generic nursing care compared with GP care. The 95% confidence ellipses represent the uncertainty around the incremental cost-effectiveness ratio: that is, the area within which it is likely the true cost-effectiveness ratio lies. In Fig. 2a , the ellipse is slightly left of the y-axis, indicating that problem-solving treatment seems to be less effective than GP care. It is also above the x-axis, suggesting that problem-solving treatment is more costly than GP care. In the second comparison (Fig. 2b ), there is no difference in effectiveness, but the intervention is more costly. Consequently, neither intervention can be considered cost-effective in comparison with usual GP care.
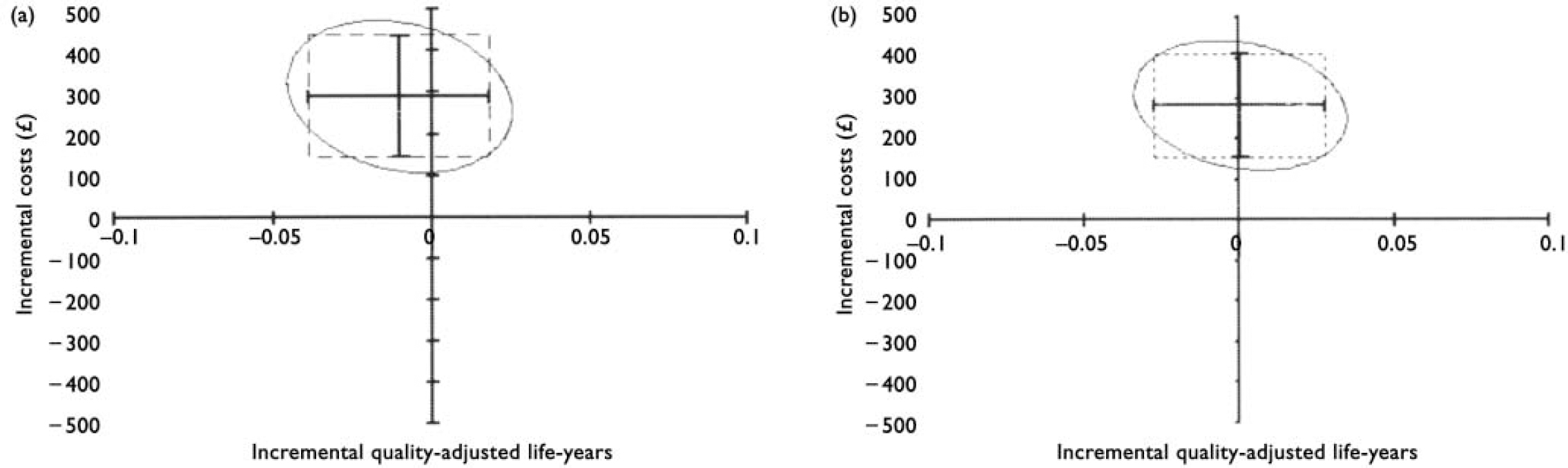
Fig. 2 Cost-utility analysis of community mental health nurse (a) compared with usual general practitioner care problem-solving and (b) generic communitymental health nurse care compared with usual general practitioner care on the cost-effectiveness plane (bars show 95% confidence intervals for cost and effect differences; ellipses show 95% confidence interval for joint distribution of cost and effect differences).
DISCUSSION
Principal findings
This study provides strong evidence that referral of unselected primary care patients with common mental disorders to a specialist mental health nurse confers no additional benefit over usual GP care. This remains true whether the nurses are providing treatment in line with what they believe is best practice according to their skills and experience, or whether they are trained to provide problem-solving treatment. Patients' mean symptom scores, social functioning and quality of life were all significantly improved by 8 weeks, with a small further improvement by 26 weeks, with no significant differences between treatment arms.
The economic results provide good evidence that community mental health nurse care is significantly more expensive than usual GP care. Health service costs over 26 weeks were approximately doubled in the two nursing groups compared with the GP group. On average, generic nursing care cost an extra £283, and nurse problem-solving treatment an extra £315, per patient. There was a significant reduction in the cost of consultations with their GPs among patients referred to the problem-solving arm, but the savings from this were only approximately 10% of the extra costs of nurse treatment. We found no significant differences in costs of drug treatment. We also found no significant difference in days off work unlike the previous trial of referral of such patients to community psychiatric nurses (Reference Gournay and BrookingGournay & Brooking, 1995). Patients treated by the nurses were significantly more satisfied than those randomised to usual GP care, suggesting patients appreciated the support provided by the nurse, but this did not enhance recovery and hence cannot be justified on cost-effectiveness grounds.
Our study findings were in line with the one previous controlled trial of community mental health nursing care v. usual GP care for common mental disorders (Gournay & Brooking, Reference Gournay and Brooking1994, Reference Gournay and Brooking1995). They are also consistent with the study of problem-solving treatment for such disorders delivered by non-mental health community nurses (Reference Mynors-Wallis, Davies and GrayMynors-Wallis et al, 1997), suggesting that problem-solving treatment is no more effective than usual GP care for patients with common mental disorders, unlike in moderate depression, where it has been shown to be of benefit (Reference Mynors-Wallis, Gath and Lloyd-ThomasMynors-Wallis et al, 1995; Reference Dowrick, Dunn and Ayuso-MateosDowrick et al, 2000; Reference Mynors-Wallis, Gath and DayMynors-Wallis et al, 2000; Reference Unutzer, Katon and CallahanUnutzer et al, 2002).
Strengths of the study
This was a real-life study using NHS community mental health nurses. All such nurses in the relevant trusts were invited to participate. The inclusion of patients in inner-city, suburban and rural general practices across a wide area of south-central England suggests that the results are likely to be generalisable to other settings with similar service provision.
The study represents a considerable improvement on the previous study of community mental health nursing care for common mental disorders (Reference Gournay and BrookingGournay & Brooking, 1994) in terms of its greater sample size, inclusion of an assessment immediately following treatment and good follow-up rates of 86% at 8 weeks and 77% at 26 weeks. It is also much larger than the previous study of problem-solving treatment for common mental disorders delivered by non-mental health community nurses (Reference Mynors-Wallis, Davies and GrayMynors-Wallis et al, 1997). In fact, it is one of the largest studies of problem-solving conducted so far.
Limitations of the study
Although we managed to recruit the (revised) sample size we aimed for, we cannot rule out a 4- to 5-point difference in the CIS-R scores between arms with 95% confidence, although a type II error owing to lack of power is unlikely, seeing that there was no consistent trend in any outcome measure in the direction of benefit from nurse care. The differences in CIS-R scores between nurse care and GP care were in different directions for the two nurse arms, at both 12 and 26 weeks.
We cannot be absolutely sure that problem-solving treatment was delivered faithfully by all the trained nurses. Unfortunately, only a relatively small proportion of their sessions was rated directly, because of reluctance on their part, or the patient's part, to be tape-recorded. However, the treatment was being delivered faithfully in the sessions rated, and the experienced therapists giving ongoing supervision to the nurses believed they were delivering the treatment as faithfully as in previous, positive studies. Furthermore, ongoing qualitative work with patients treated in both nursing arms (to be reported separately) showed that patients in the problem-solving group reported that their problems were addressed by the nurses using a structured approach with homework between sessions.
The participating GPs obviously did not refer all the patients they saw who would have been eligible for the trial, since many of them referred only one patient each, introducing the possibility of referral bias. We have no information on patients who might have been referred but were not, and so cannot be sure that those who were referred are representative of all patients presenting with common mental disorders.
It is difficult to tell whether the lower follow-up rate in the GP care arm biased the findings in a particular direction. We do not know whether drop-outs remained more or less symptomatic than those followed-up. However, the sensitivity analyses suggest that nursing care, whether generic or problem-solving, was unlikely to be more effective than GP care, unless we make the extreme assumption that all drop-outs remained as symptomatic as at baseline or their last assessment. The resource-use questionnaires filled out by patients had gaps in a number of cases. In addition, only patients with complete CIS-R assessments were included in the economic analysis, further reducing the sample size. However, the findings were not altered by augmentation of the service-use information from medical record data which were available for 93% of patients.
Implications for practice and future research
We conclude that community mental health nurses should not be referred unselected patients with common mental disorders. Usual GP care for at least 8 weeks will result in many such patients recovering. An alternative is referral for non-directive counselling, which has been shown to confer modest benefits for patients with anxiety and depression in the short term (6 weeks to 4 months) compared with usual GP care, but no additional advantages in the longer term. As with nursing care, patient satisfaction is higher with counselling, and unlike nursing care it appears not to be more costly than GP care, although the evidence on differences in costs is quite limited (Reference Bower, Rowland and Mellor ClarkBower et al, 2002). These findings suggest that best practice for the initial management of patients with common mental disorders is watchful waiting, rather than referring for early and possibly wasteful interventions.
These findings are important, because GPs continue to want direct access to refer patients to community mental health nurses (Reference Badger and NolanBadger & Nolan, 1999; Reference Crawford, Carr and KnightCrawford et al, 2001). The participating community mental health nurses in this study confirmed that this is still the case in 2005 (in qualitative interviews to be published in due course). Department of Health policy has not been entirely consistent in this area. The National Service Framework for Mental Health (Department of Health, 1999) emphasised that less-severe mental health problems were very common and that the majority of them should be managed in primary care, with agreed protocols for referral to specialist services, in line with the recommendations of the Mental Health Nursing Review Team (1994). On the other hand however, the community health team policy implementation guide (Department of Health, 2002a ) suggested that teams should provide for two groups of patients, stating that:
‘most patients treated by the CMHT [community mental health team] will have time limited disorders and be referred back to their GPs after a period of weeks or months (an average 5-6 contacts) when their condition has improved. A substantial minority, however, will remain with the team for ongoing treatment, care and monitoring for periods of several years’. Even where teams operate referral policies that restrict ongoing care to people with severe and enduring mental health problems, they often still provide at least one-off assessment for people with less-severe problems, which represents a significant call on their time, even if patients are then referred straight back to the primary care team for further management. Some teams have responded to the demands of primary care by developing specific services for people with common mental disorders, for example the Fylde Assessment and Short-Term Intervention service (Department of Health, 2002b ), and, within the catchment area of our study, the community mental health team in Andover, and the Poole and Bournemouth Primary Care Mental Health Teams.
Primary care trusts have increased power to determine the range of secondary care services provided through commissioning, in accordance with the government policy of a ‘primary care led NHS’ (Department of Health, 2000b ). Commissioning is currently being devolved further, down to the level of general practices. This study provides important evidence for those commissioning care in the UK, that community mental health nursing care should not be provided for unselected patients with common mental disorders. Nurses could play other roles in primary care, such as consultation-liaison to support the primary care team, or the provision of cognitive-behavioural therapy for patients with depression not responding to self-help or primary care team interventions, in managed care systems (Reference Katon, von Korff and LinKaton et al, 1999; Reference Wells, Sherbourne and SchoenbaumWells et al, 2000; National Institute for Clinical Excellence, 2004). However, this will compete with the need for community mental health nurses within teams to deliver evidence-based therapies for patients with severe and enduring mental illness, such as compliance therapy (Reference Kemp, Hayward and ApplethwaiteKemp et al, 1996) or cognitive-behavioural therapy for psychosis (Reference Sensky, Turkington and KingdonSensky et al, 2000).
During the course of the study, the NHS Plan was published, heralding the introduction of 1000 graduate primary care mental health workers (Department of Health, 2000b ). It is proposed that such workers should be trained in brief therapy techniques with proven effectiveness, and employed to help GPs treat common mental disorders. Our results suggest that training workers to offer individual problem-solving treatment for unselected patients with common mental disorders is not likely to be any more effective than usual GP care, although such care might also increase patient satisfaction, and presumably will be less expensive than specialist nursing care. There would, however, need to be many more primary care mental health workers trained, as the initial 1000 represents an average of only three per primary care trust.
Future research needs to identify predictors of chronicity in common mental disorders, to target extra treatment to those patients who are less likely to recover within weeks with usual GP care. Optimum treatment for those with more chronic problems has not been clarified by this study, but research from the USA suggests a managed care approach might be beneficial (Reference Katon, von Korff and LinKaton et al, 1999; Reference Wells, Sherbourne and SchoenbaumWells et al, 2000). The internationally important conclusion of this study is that problem-solving treatment should be reserved for patients with depressive disorders of at least moderate severity, who have not responded to initial management by primary care physicians.
Acknowledgements
We thank all the patients, the community mental health nurses and the GPs who participated in this study, all the research team and the trainers and supervisors.











eLetters
No eLetters have been published for this article.