The community treatment order (CTO) is used to address medication non-adherence by provision of involuntary treatment but in a less restrictive environment than that afforded by in-patient care. These orders were first introduced in the USA in the mid-1970s and now are also available in several other countries. The CTO exists in different forms: for use immediately after a period of hospital detention; as an alternative to hospital detention; or to prevent deterioration before criteria for hospital detention are met. Other aspects of the CTO around the world also vary: duration (3 months or more); inclusion or exclusion of legal power to enforce medication in the community, requiring the police to escort the patient to hospital; Reference Swartz, Swanson, Wagner, Burns, Hiday and Borum1,Reference Torrey and Kaplan2 eligibility criteria; Reference Gray and O'Reilly3 and the person who is able to instigate the order (responsible clinician or formal judicial procedure involving a magistrate or judge).
Clinical effectiveness of CTOs
There have been two randomised controlled trials of CTOs; neither provided definitive evidence that CTOs are in themselves efficacious Reference Swartz, Swanson, Wagner, Burns, Hiday and Borum1,Reference Steadman, Gounis, Dennis, Hopper, Roche and Swartz4 and both had a number of problematic methodological issues. Reference Swartz and Swanson5–Reference O'Reilly and Bishop7 A recent Cochrane review pooled the data from the two trials and estimated that 85 people would need to receive a CTO in order to avoid one admission and that 238 people would need to receive a CTO in order to avoid one arrest. Reference Kisely, Campbell and Preston8 These numbers are substantially greater than one might expect. Further, a systematic review of over 70 studies concluded that CTOs lacked consistent evidence of benefit and that findings from naturalistic CTO studies were likely to be unreliable. Reference Churchill, Owen, Singh and Hotopf9 Thus, to date there is a lack of rigorous evidence from randomised controlled trials to support the use of such orders. One might speculate that research in this area suffers from the difficulties that hamper research on long-acting injections (LAIs) – those required to participate are the least likely to consent and participate. In addition, the trials to date have taken place in North America, and the substantial differences in structure and function of community services in this setting compared with countries such as Australia and the UK might influence the substantial number needed to treat.
Community treatment orders in the UK
The UK has long debated the introduction of the CTO, particularly in relation to managing risk. Reference Sensky, Hughes and Hirsch10 Many regarded it as a ‘toothless dragon’ under previous legislation because ‘the inability to allow enforced delivery of medications to patients is regarded by many as rendering CTOs ineffective’. Reference Ridley11 Since autumn 2008, under new legislation a CTO can be used after a patient has been detained under a hospital treatment order (Section 3) in England and Wales. 12 Since 2005, Scotland has had community-based compulsory treatment orders (CCTOs). 13 These can be applied either after detention in hospital, or de novo, usually as an alternative to a hospital order, but can only be instigated by the Mental Health Tribunal for Scotland. A number of disincentives exist in promoting their use in debatable cases and their rate of use is lower than in most other settings. Reference Lawton-Smith14
CTOs and antipsychotic long-acting injections
In clinical practice the decision to prescribe either LAI or oral medication often rests largely on an assessment of the risk of poor adherence in the individual patient and what resources are available to deal with this. Reference Barnes and Curson15–Reference Dignam17 Long-acting injections are an attempt to overcome unknown or covert non-adherence by involving a clinician in administering the injection, although it should be noted that some patients may still actively be non-adherent to LAI treatment, either from the outset or later on. Reference Levine, Schooler and Cassano18,Reference Patel and David19 In essence, the principal function of the CTO might be then to encourage patients to accept instigation of an LAI, or simply to help reduce the high defaulting rate of patients already receiving an LAI. Reference Ridley11,Reference Hardman20,Reference McLaren and Cookson21 Others have also noted that the CTO works by ‘persuading the persuadable’ to engage in treatment. Reference Pinfold, Bindman, Thornicroft, Franklin and Hatfield22
A number of studies in Australia have noted the particular relationship between LAIs and CTO administration. Reference Callaly and Trauer23–Reference Muirhead, Ingram and Harvey25 In an earlier study based in Victoria, CTO use was twice as likely with LAIs than with oral antipsychotics. Reference Callaly and Trauer23 As noted previously, there has been no clear signal to suggest that the use of a CTO with an LAI is particularly beneficial with respect to long-term outcomes. The CTO may first grant access to treating the patient with an LAI and also provide sufficient time to establish a regular injection routine. In turn, this allows patients a better chance of establishing some control over their illness and, with it, a measure of improved insight. This may enhance further adherence. Reference Cuffel, Alford, Fischer and Owen26,Reference Garavan, Browne, Gervin, Lane, Larkin and O'Callaghan27
The study reported here examines the changing trends in the use of CTOs and antipsychotic medications during the period of transition to full community treatment in Victoria, Australia. For patients with schizophrenia treated in the community we aimed, first, to estimate the rate of CTO use during the period 1998–2002 and, second, to understand its relationship to the prescription of LAI v. oral antipsychotics at both time points. We wished to determine whether the rate of use of CTOs significantly changed over this period, and to explore the balance of use of second-generation antipsychotics (SGAs) and first-generation antipsychotics (FGAs) in a healthcare system that was evolving to a full community-based model. We predicted that with the move to a fully deinstitutionalised model of care the rate of CTO use would increase, and that independently of changing trends in LAI and oral antipsychotic prescription rates, the prescribing of LAIs for patients on CTOs would be higher than that of oral antipsychotics.
Method
The study was conducted in community clinics of the North-Western Mental Health Programme (NWMHP) in urban Melbourne, Victoria, Australia. In the state of Victoria, CTOs are defined as ‘orders under the Mental Health Act which enable involuntary patients to live in the community while they receive treatment for their mental illness’. 28 At the time of data collection the in-patient units in Victoria were described as being limited to providing intensive care, with 21.8 beds per 100 000 adults and an average length of stay (estimated in 2001) of around 14 days (see Auditor General, Victoria 2002, in Brophy et al). Reference Brophy, Reece and McDermott29 Further, the study was undertaken during the closure of long-stay mental health hospitals and the development of mainstream, integrated community psychiatry service delivery. Reference Singh30 Thus, the only remaining acute in-patient units in the state of Victoria were in general medical hospitals. The transition was completed by the end of 2000.
Procedure
As part of a larger project examining community-based antipsychotic treatment, Reference Lambert31 prescribing and demographic information were obtained from four community mental health clinics of the NWMHP. The patient sample was a random selection of patients from each clinic's list of unique record locators. Where files were not available, a random replacement was selected from active files in the clinic. All case files were manually inspected for prescribing information and the results entered into a database. Information relating to CTO status was obtained from the NWMHP central administrative database and matched to patients by their unique record locator at each specific survey time point.
The sample in 1998 (time 1) was derived from 919 patients with schizophrenia sampled from the four community centres that were within the NWMHP administrative network, of whom 563 patients had meaningful data on CTO status available and also were known to be receiving antipsychotic treatment (excluding pro re nata, or as required, prescriptions). In 2002 (time 2) another random selection of cases from the same four clinics provided 1142 patients with schizophrenia, of whom 806 had a valid active antipsychotic prescription and a matched record of their current CTO status.
Statistical analysis
For analyses of the relationship between CTO use and antipsychotic prescription, those receiving antipsychotic LAIs (either as monotherapy or in combination with other antipsychotics) were contrasted with all prescriptions for antipsychotics not involving an LAI. For SGA–oral analysis, these agents were compared with LAIs and FGA–orals. As a small number of patients at both time points were receiving both SGA–oral and FGA–LAI therapy, the analysis of the relationship of CTO patients to SGA–oral use was undertaken after exclusion of the patients also receiving an FGA–LAI (time 1: n = 9, 2.4% reduction in sample size; time 2: n = 59, 7% reduction in sample size). Analyses of categorical data employed chi-squared analysis. Where interval or ratio data were normally distributed, t-tests were used. Tests of proportions were calculated using the binomial test. Simple odds ratios were computed using Cochrane's and Mantel–Haenszel statistics.
Results
Demographic information at time 1 is shown in Table 1. The cross-sectional use of a CTO was unrelated to any demographic variable, other than the treating clinical centre, with one clinic using CTOs in 20% of its patients with schizophrenia, in contrast to 8–13% in the other clinics (P = 0.027).
Table 1 Demographic details of the sample at time 1
| All n (%) | No CTO n (%) | On CTO n (%) | Significance | |
|---|---|---|---|---|
| Gender | ||||
| Female | 219 (39) | 192 (39) | 27 (38) | |
| Male | 341 (61) | 296 (61) | 45 (62) | χ2 = 0.03 |
| Total a | 560 (100) | 488 (87) | 72 (13) | P = 0.865 |
| Age | ||||
| <30 years | 164 (29) | 142 (30) | 22 (31) | χ2 = 0.01 |
| ⩾30 years | 395 (71) | 345 (71) | 50 (69) | P = 0.917 |
| Total | 559 (100) | 487 (87) | 72 (13) | |
| Marital status | ||||
| Previous or current relations | 207 (40) | 181 (40) | 26 (39) | |
| Never married | 313 (60) | 273 (60) | 40 (61) | χ2 = 0.01 |
| Total | 520 (100) | 454 (87) | 66 (13) | P = 0.999 |
| Ethnicity | ||||
| English-speaking COB | 328 (62) | 286 (62) | 42 (65) | |
| NESB COB | 199 (38) | 176 (38) | 23 (35) | χ2 = 0.08 |
| Total | 527 (100) | 462 (88) | 65 (12) | P = 0.775 |
| Benefits | ||||
| No pension | 49 (9) | 46 (10) | 3 (4) | Fisher's |
| Pension or benefits | 495 (91) | 429 (92) | 66 (96) | χ = 0.18 |
| Total | 544 (100) | 475 (87) | 69 (13) | P = 0.105 |
| Accommodation | ||||
| Independent | 469 (86) | 414 (87) | 55 (80) | |
| Supported/homeless | 75 (14) | 61 (13) | 14 (20) | χ2 = 2.22 |
| Total | 544 (100) | 475 (87) | 69 (13) | P = 0.136 |
| Education | ||||
| Primary or secondary | 344 (83) | 303 (82) | 41 (89) | Fisher's |
| Tertiary | 72 (17) | 67 (18) | 5 (11) | χ = 0.30 |
| Total | 416 (100) | 370 (89) | 46 (11) | P = 0.154 |
| Clinic | ||||
| A | 135 (24) | 117 (24) | 18 (25) | |
| B | 157 (28) | 140 (29) | 17 (24) | |
| C | 144 (26) | 132 (27) | 12 (17) | χ2 = 9.14 |
| D | 124 (22) | 99 (20) | 25 (35) | P = 0.027 |
| Total | 560 (100) | 488 (87) | 72 (13) |
COB, country of birth; CTO, community treatment order; NESB, non-English-speaking background
a. Of the 563 patients, 3 had missing demographic data
Rates of CTO use
For patients with schizophrenia who were prescribed an antipsychotic, the rate of CTO use was 13% (74/563) at time 1 and 26% (209/806) at time 2. The increase in the proportion of patients with a CTO over this period was significant (time 1 v. time 2, binomial P<0.001) (Fig. 1).
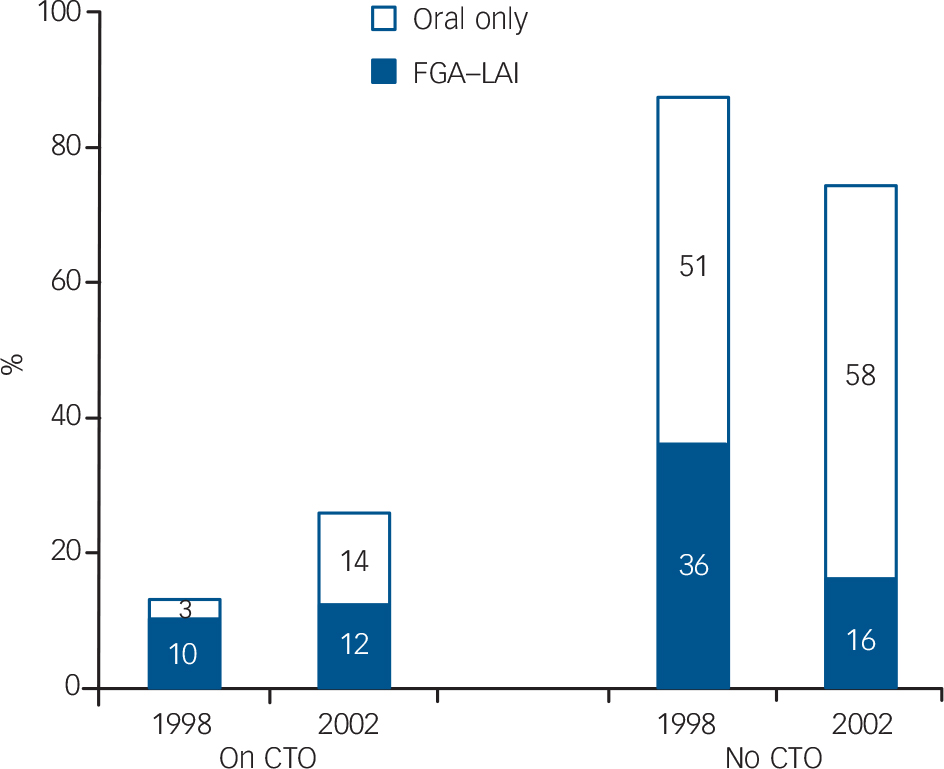
Fig. 1 Proportion of patients with schizophrenia according to community treatment order (CTO) status and antipsychotic formulation (FGA, first-generation antipsychotic).
Oral antipsychotics v. LAIs
The relationship between the use of CTOs and the prescription of LAIs is shown in Table 2. In 1998, of the 13% of patients given a CTO, 77% (n = 57) were prescribed an LAI, in contrast to the 23% (n = 17) who were prescribed only oral antipsychotics. At this time for a patient with a CTO the odds of being prescribed an LAI were 4.7 times that of being prescribed only an oral antipsychotic. In 2002, of the 26% of patients given a CTO, 47% were prescribed an LAI and 53% were prescribed an oral antipsychotic only. This indicates that although the use of CTOs is split almost equally between LAI and oral drugs, the odds of having a CTO with an LAI are 3.2 times those of having a CTO with an oral antipsychotic.
Table 2 Community treatment order status and use of long-acting injections: 1998 to 2002
| All n (%) | No CTO n (%) | On CTO n (%) | OR (95% CI) a | |
|---|---|---|---|---|
| 1998 | ||||
| Oral only | 302 (54) | 285 (58) | 17 (23) | 4.68 (2.65–8.29) |
| FGA–LAI | 261 (46) | 204 (42) | 57 (77) | |
| Total | 563 (100) | 489 (87) | 74 (13) | |
| 2002 | ||||
| Oral only | 575 (71) | 465 (78) | 110 (53) | 3.17 (2.27–4.43) |
| FGA–LAI | 231 (29) | 132 (22) | 99 (47) | |
| Total | 806 (100) | 597 (74) | 209 (26) |
CTO, community treatment order; FGA, first-generation antipsychotic; LAI, long-acting injection
a. FGA–LAI (oral) v. oral antipsychotics only (first or second generation)
For all patients with schizophrenia treated with antipsychotic medication, Fig. 1 shows the changes in CTO and formulation use between 1998 and 2002. It is notable that the CTO rate was increasing, along with a decrease in the use of FGA–LAIs and an increase in numbers of patients treated with oral formulations only. However, as a proportion of all antipsychotic-treated patients at each time point, the rate of patients on a CTO with an FGA–LAI remained reasonably stable (10% in 1998 and 12% in 2002). This is in contrast to the patients on a CTO with oral medication only, where the respective rates were 3% of all patients in 1998 and 14% in 2002.
Oral SGAs v. FGAs (oral and LAI)
Table 3 shows the relationship between the use of CTOs and the prescription of oral SGAs. In the period between 1998 and 2002, SGA–oral prescriptions grew from 33% to 74%. Excluding patients with polypharmacy of an SGA–oral with an FGA–LAI, 13% of patients at time 1 had a CTO; of these, 14% were treated with an SGA–oral and the other 86% were treated with an FGA (oral or LAI). At time 2 a quarter (26%) of patients had a CTO; of these, 54% were prescribed an SGA–oral and the other 46% were treated with an FGA (oral or LAI). However, in keeping with the analysis presented above, it is significantly less likely that patients given a CTO will receive an SGA–oral rather than an FGA (oral or LAI) when compared with those not given a CTO.
Table 3 Community treatment order status and use of oral second-generation antipsychotics: 1998 to 2002

| All n (%) | No CTO n (%) | On CTO n (%) | OR (95% CI) a | |
|---|---|---|---|---|
| 1998 | ||||
| FGA (oral or LAI) | 373 (67) | 312 (65) | 61 (86) | |
| SGA–oral | 181 (33) | 171 (35) | 10 (14) | |
| Total | 554 (100) | 483 (87) | 71 (13) | 0.30 (0.15–0.60) |
| 2002 | ||||
| FGA (oral or LAI) | 198 (26) | 110 (20) | 88 (46) | |
| SGA–oral | 549 (74) | 445 (80) | 104 (54) | |
| Total | 747 (100) | 555 (74) | 192 (26) | 0.29 (0.21–0.42) |
CTO, community treatment order; FGA, first-generation antipsychotic; LAI, long-acting injection; SGA, second-generation antipsychotic
a. Oral SGA only v. FGA (oral or LAI)
Discussion
In 1998 in the NWMHP catchment area in urban Melbourne, 13% of patients with schizophrenia were subject to a CTO. This is consistent with the findings of others for this region. Reference Callaly and Trauer23,Reference Vaughan, McConaghy, Wolf, Myhr and Black24 This rate doubled over the subsequent 4 years, so that by 2002 a quarter of patients with schizophrenia were on CTOs. This occurred in the final phase of transition from a traditional hospital-based service delivery system to a more community-based system, with a small number of short-term acute psychiatric beds. Reference Goldberg32 Despite a changing balance in the type of antipsychotics prescribed, the association between CTOs and LAIs remained strong throughout the study. By 2002 just under half of those on CTOs were also prescribed an LAI. In essence, as a proportion of all antipsychotic-treated patients at each time point, the rate of patients subject to a CTO with an LAI remained relatively stable over time. In 1998, of the patients receiving a CTO, three-quarters were prescribed an LAI, but in 2002, of those receiving a CTO only slightly less than half were prescribed an LAI. Thus, there was a reduction in the proportion of patients on CTOs who were also prescribed an LAI, but it still remained relatively high. It is likely that LAI prescribing is, in the main, a clinician response to poor adherence and that the CTO is the mechanism used to compel reluctant patients to take the injection. Two main aspects regarding use of an LAI with a CTO include the changing treatment patterns for schizophrenia and the nature of psychiatric service provision.
Effect of changing treatment patterns
With the demonstrated trend towards the use of oral SGAs, it is likely that those who could have been switched to and successfully maintained on SGA–orals would have done so. Thus, those remaining on LAIs may represent a particularly difficult group of patients. The actively and assiduously non-adherent patient may require a CTO in order to have any chance of commencing an LAI. Such patients may be more difficult, more reluctant to accept treatment, and have longer, more established histories consistent with ‘revolving door’ characteristics. In such circumstances, there may be a requirement for the added ‘authority to treat’ associated with the use of CTOs to be applied in order for patients to accept their LAI injections.
Given that the rate of LAI use fell from 46% to 29%, more marginal cases that might have been treated with LAIs in the pre-SGA era might instead have been given the benefit of the doubt and treated with an oral SGA in the expectation of improved outcomes. Although by 2002, given the increase in SGA–oral prescribing in general and the expected risks of oral non-adherence, the increase in use of CTOs with SGA–orals was lower than might otherwise have been expected. This may reflect the difficulty of accurately assessing non-adherence to oral medication regimens. Reference Levine, Schooler and Cassano18 Thus, the threshold for revoking the CTO and returning the oral SGA-treated patient to hospital is less clear-cut, and there will be considerable reluctance to revoke a CTO merely on the suspicion that patients are not taking their oral medication.
Service and community aspects of CTO use
One criticism of the CTO is that when patients subject to an order refuse to take their medication (i.e. non-adherence) forced treatment in the community does not necessarily follow, as seen in the USA. Reference Steadman, Gounis, Dennis, Hopper, Roche and Swartz4 In the state of Victoria, revoking a CTO allows for the patient to be returned to hospital. However, this occurs mainly for florid relapse and only rarely to ensure treatment adherence. Arguably, CTOs are most successful when patients perceive (if erroneously) that they can be treated against their wishes outside the hospital setting. Reference Dawson33 This remains a form of coercion over and above the legislation itself. Hence, CTOs may serve to ‘persuade the persuadable’, in the hope that the patient does not test the resolve of the community teams to rescind the CTO for breaches relating to non-adherence. Reference Ridley11,Reference Hardman20,Reference Swartz, Swanson, Wagner, Burns and Hiday34 Although it is uncommon, patients who have known risk histories and who refuse their injections may have their CTO revoked, be admitted to hospital for the injection, and then discharged immediately. This may be because in all countries with CTO legislation, public safety has been a part of the justification for CTO instigation, and this may be considered over and above the needs of the individual patient. Reference Appelbaum35
The increase in the use of CTOs in the face of reductions in hospital beds may be an understandable reaction by clinicians. However, this does not tell us whether the increase in CTOs actually reduced relapse rates through increased adherence or enhanced the perception of public safety. Further, it has been noted that changes in CTO law do not translate simply into changes in practice, particularly where entrenched positions exist among those charged with carrying out CTO policy at the level of community mental health services. Reference Churchill, Owen, Singh and Hotopf9,Reference Dawson33
The future of long-acting injections and CTOs
Thus far, the evidence for enduring LAI adherence due to the administration of a CTO is minimal, as seen in a related study by Lambert et al. Reference Lambert, de Castella, Kulkarni, Ong and Singh36 That study showed that when 1-year LAI adherence was examined using a multivariate model comprising known associations of LAI adherence, CTOs did not remain in the final model when predicting adherence; 55% of the study cohort were on CTOs. Similarly, in the larger of the two randomised controlled trials on this topic, patients on an LAI were 2.5 times more likely to be adherent to treatment, but this was independent of the CTO effect. Reference Swartz, Swanson, Wagner, Burns and Hiday34 Measuring effectiveness of LAIs in comparison to oral formulations is also pertinent, Reference Patel and David19,Reference Hogarty, Schooler, Ulrich, Mussare, Ferro and Herron37 and we suggest studies of at least 2 years' duration are required for investigation of LAI use in combination with a CTO. Directions for future research include:
-
(a) the role of the CTO in maintaining medication treatment adherence;
-
(b) identification of the best outcome measure for effectiveness of CTOs (relapse or other); Reference Kisely, Campbell, Scott, Preston and Xiao38
-
(c) identification of characteristics of the patients most likely to benefit from a CTO; Reference Brophy, Reece and McDermott29
-
(d) comparisons of SGA–oral v. LAI (FGA and SGA), both with or without use of a CTO;
-
(e) optimal duration of the CTO;
-
(f) enduring duration of treatment adherence and clinical benefits beyond the expiry of the CTO.
Limitations
One limitation of our study relates to its dependence on administrative databases for CTO data. It is possible that the bias may be towards overestimating the proportion of patients receiving CTOs. However, given that the rates were similar to other studies reported in Victoria at this time (which did not depend on a centralised database), and also given that the structure of services is mandated to be consistent throughout Victoria, any such bias is likely to be minimal. There also exists a problem in acquiring demographic data from case-file systems. Missing data due to technical and administrative problems may bias the relationships between key variables. Also, there was no measure of illness duration, number of previous hospitalisations or dangerousness available for analysis, which might be thought to influence CTO use. One should also consider that the CTO in the state of Victoria is relatively easy to apply – there is no magistrate or judicial process involved, and this may bias the estimates of the frequency of its use compared with other systems.
The generalisability of our findings to other settings such as the UK is limited by the fact that SGA–LAIs were not available at the time of data collection and that oral SGAs are now better understood in terms of their different side-effect profiles (with somewhat enhanced risk of developing metabolic syndrome). These developments may potentially alter the rates of concomitant use of LAIs and CTOs, although in which direction would be subject to further enquiry.
Implications of the study
Community treatment orders provide a mechanism for involuntary treatment beyond the hospital setting. The proportion of patients on such orders increased during the observation period (1998–2002) such that by 2002 a quarter of patients with schizophrenia were receiving CTOs. This took place in a system with several years' experience of the CTO but during a time when the last of the long-stay in-patient beds were closed.
The most consistent association with CTO use is the prescription of antipsychotic LAIs, and both are used in the management of treatment non-adherence. For patients subject to a CTO, an LAI is more than twice as likely to be prescribed as an oral antipsychotic. Thus, as a proportion of all antipsychotic-treated patients at each time point, the rate of patients with a CTO prescribed an FGA–LAI remained relatively stable. That said, the proportion of patients given a CTO who were also prescribed an FGA–LAI declined over time, but remained high (Fig. 1). This is despite the general trends in prescribing for schizophrenia whereby the proportion of SGA–orals increased and that of LAIs decreased. Even with the advent of SGA–orals, the use of CTOs remains strongly associated with the prescription of LAIs relative to oral medications.
Long-acting antipsychotic injections have been described as potentially ‘the best authenticated method of preventing relapse in non-adherent, or forgetful patients’, Reference Hale39 but defining those who specifically require the added measure of a CTO requires further elucidation. With increasing uptake of CTO legislation as found in England and Wales, whether LAIs (first- and second-generation) will be as preferentially chosen over oral antipsychotics remains to be seen.
Acknowledgements
We thank Drs Mark Taylor and Donald Lyons, who provided information regarding use of the community treatment order in Scotland, Professor George Szmukler for comments on earlier drafts of this paper, and Ms Joyce Goh, who facilitated the acquisition of the CTO data in Melbourne.







eLetters
No eLetters have been published for this article.