The literature on psychological or psychosocial interventions for young people with social disability and severe and complex mental health problems is sparse.Reference Fowler, French, Banerjee, Barton, Berry and Byrne1–Reference Burke, Shapero, Pelletier-Baldelli, Deng, Nyer and Leathem6 Of the four studies that we identified, only one, of a brief group workshop-based intervention targeting clinical symptoms and resilience, appeared significantly effective;Reference Burke, Shapero, Pelletier-Baldelli, Deng, Nyer and Leathem6 however, the study had no control group and the student sample was not a clinical sample.
Three-quarters of socially disabling long-term mental health problems begin in adolescence.Reference Kessler, Berglund, Demler, Jin, Merikangas and Walters7 Social disability is observable before the onset of mental health problems and if it is ongoing, transition to long-term problems of diagnostic severity is more likely.Reference Fowler, Hodgekins, Arena, Turner, Lower and Wheeler2,Reference Cross, Scott and Hickie8 Social disability can be defined as low time spent in structured activity. Young people without mental health problems spend 64 hours a week (‘weekly hours’) on average in structured activity, with under 30 h representing serious social disability and under 15 h severe social disability.Reference Hodgekins, French, Birchwood, Mugford, Christopher and Marshall9 Structured activity includes paid and voluntary employment, education, caring, sports and structured leisure.Reference Hodgekins, French, Birchwood, Mugford, Christopher and Marshall9 Young people at the greatest risk of long-term social disability present with emerging social withdrawal, emotional and behavioural problems, subthreshold psychosis and risky behaviours such as alcohol and drug use.Reference Kessler, Berglund, Demler, Jin, Merikangas and Walters7 This group is extremely vulnerable and their problems, if untreated, have severe, potentially lifelong personal and economic costs.Reference Kessler, Berglund, Demler, Jin, Merikangas and Walters7,Reference Knapp, King, Healey and Cicely10 This group is neglected in research and clinical care, with under 25% of young people with a diagnosable mental health problem gaining access to specialist mental health services.11 The significant social withdrawal makes engagement very challengingReference Fowler, Hodgekins, Arena, Turner, Lower and Wheeler2,Reference Cross, Hermens and Hickie5 and standard interventions may be inaccessible and ineffective. Recent reviews demonstrate that cognitive–behavioural therapy (CBT) has only small or short-term effects on social outcomes for people at risk of psychosis or with schizophrenia.Reference Devoe, Farris, Townes and Addington12,Reference Laws, Darlington, Kondel, McKenna and Jauhar13 Youth community services, for example serving young people not in employment, education or training (NEET), often provide excellent vocational support but lack the requisite mental health specialism for this complex group.Reference Scott, Fowler, McGorry, Birchwood, Killackey and Christensen14 Vocational interventions delivered in mental health services, such as individual placement and support, are effective in increasing paid employment for people with severe mental health problems, but do not target broader clinical and social outcomes.Reference van Rijn, Carlier, Schuring and Burdorf15 Early intervention in psychosis (EIP) services assertively engage people with severe and complex mental health problems in specialist mental health and socio-vocational support, but are only accessible with a confirmed or imminent first episode of psychosis, thus excluding people with non-psychotic yet severe and complex mental health problems. Furthermore, most people accessing EIP still experience persistent social disability 1 year later,Reference Hodgekins, Birchwood, Christopher, Marshall, Coker and Everard16 and non-psychosis specific youth mental health services, where these exist, effect reliable change for only a minority.Reference Cross, Scott, Hermens and Hickie4
We developed social recovery therapy (SRT), a specialist psychosocial intervention combining CBT, assertive outreach and multisystemic principles to treat social disability in the context of severe and complex mental health problems.Reference Fowler, Hodgekins, Berry, Clarke, Palmier-Claus and Sacadura17 The clinical and cost-effectiveness of SRT has been demonstrated in psychosis.Reference Barton, Hodgekins, Mugford, Jones, Croudace and Fowler18,Reference Fowler, Hodgekins, French, Marshall, Freemantle and McCrone19 The SUPEREDEN3 trialReference Fowler, Hodgekins, French, Marshall, Freemantle and McCrone19 showed that adding SRT to EIP produced large and significant improvements in structured activity and psychotic and mood symptoms. We hypothesised that providing SRT to a younger group with emerging severe problems would create early gains in social and clinical recovery, interrupting potentially lifelong trajectories of disability. We conducted the PRODIGY trial to test the benefit of adding SRT to optimised standard care for young people with severe and complex mental health problems who had not experienced an episode of psychosis. We conducted a qualitative process evaluation alongside the trial.Reference Notley, Christopher, Hodgekins, Byrne, French and Fowler20,Reference Gee, Notley, Byrne, Clarke, Hodgekins and French21 Here we present the trial outcomes. We aimed to test the primary hypothesis that SRT as an adjunct to enhanced standard care (ESC) would be superior to ESC alone in improving weekly hours in structured activity at 15 months post-randomisation.Reference Fowler, French, Banerjee, Barton, Berry and Byrne1 Secondary hypotheses were that the addition of SRT would lead to greater improvements in psychotic, mood and general symptoms at 9 and 15 months, and that improvements would persist until 24 months post-randomisation.Reference Fowler, French, Banerjee, Barton, Berry and Byrne1
Method
Study design
This was a pragmatic, multi-centre, single- (assessor-) blind, randomised controlled trial comparing the clinical and cost-effectiveness of social recovery therapy (SRT) and enhanced standard care (ESC) with ESC alone. The intervention period lasted 9 months post-randomisation. Outcomes were assessed at 9 and 15 months post-randomisation, with limited assessment of longer-term outcomes at 24 months post-randomisation.
Participants
The target sample size was 270 participants, 135 in each arm.Reference Fowler, French, Banerjee, Barton, Berry and Byrne1 This target was calculated using a minimal clinically important effect size of 0.4 standard deviations in weekly structured activity hours, with 90% statistical power, two-sided 5% significance level, and allowing 20% attrition. Inclusion criteria were: aged 16–25 years; persistent social disability; severe and complex mental health problems. Persistent social disability was operationalised as <30 weekly hours of structured activity, with history of social impairment for at least 6 months. The presence of severe and complex mental health problems was operationalised as meeting at risk mental state for psychosis (ARMS) criteria and/or scoring ≤50 on the Global Assessment of Functioning Scale (indicating at least serious symptoms and/or serious impairment in social, occupational or school functioning) with persistence of at least moderate symptoms for at least 6 months. Exclusion criteria were: active psychotic symptoms or history of psychosis measured using Comprehensive Assessment of At Risk Mental States (CAARMS) criteria; severe intellectual disability; non-English speaking; disease or physical problems likely to undermine participation. Participants were recruited from primary and secondary youth and adult National Health Service (NHS) mental health services, and third-sector, youth, employment, and educational support organisations.
Randomisation and masking
Following baseline assessment, participants were randomly allocated 1:1 to receive SRT plus ESC or ESC alone. Remote randomisation was performed by Norwich Clinical Trials Unit (NCTU) using pre-determined lists with randomly distributed block sizes of 4 or 6. Randomisation was stratified by age (16–19 and 20–25 years), site (Sussex, East Anglia or Manchester), social disability severity (low functioning: 16–30 weekly hours of structured activity; versus very low functioning: 0–15 weekly hours) and whether ARMS criteria were met. The allocation sequence was hidden from all system users. A remote web-based system notified the allocation to NCTU and nominated trial staff.
Research assistants collecting baseline and follow-up data were masked to intervention allocation. Masking was maintained by restricted access to the data management system and in-office precautions. Thirty-one unmaskings occurred during the trial, in which the assessor became aware of whether a participant had or had not received SRT in addition to ESC. All unmaskings were successfully managed by reallocating outcome data collection to another masked assessor.
Procedures
Ethical approval was provided by the East of England Research Ethics Committee (12/EE/0311) and the Preston Research Ethics Committee North West (15/NW/0590). Potentially eligible participants were approached by their usual care provider, who (with permission) shared contact details with the research team. Potential participants were provided with written and verbal information describing trial involvement, and were invited to provide written informed consent and complete a screening assessment. Eligibility was confirmed through trial management group review. Eligible participants completed a baseline assessment and were randomised.
All participants received enhanced standard care (ESC). ESC involved services already received or offered throughout the trial, including psychological therapies where applicable. We anticipated that standard care might be limited and inaccessible. We enhanced standard care by offering a comprehensive assessment report, detailing current mental health and social functioning, to all participants and providers at trial entry and follow-up assessments. Providers were additionally given a comprehensive best practice guide, detailing local services and organisations to which participants could be referred. Providers were encouraged to offer optimal clinical evidence-based services according to National Institute for Health and Care Excellence (NICE) guidelines. All three participating research sites were centres of excellence for youth mental health and psychosis.
Participants randomised to social recovery therapy (SRT) plus ESC additionally received up to 9 months of individual SRT sessions. SRT (www.socialrecoverytherapy.co.uk) incorporates assertive outreach, multisystemic and CBT techniques. Compared with traditional CBT, SRT focuses on assessment and formulation of barriers to social recovery, with a particular focus on using behavioural work and engaging with structured activity providers and others in the surrounding system to maintain social recovery. SRT was delivered according to the therapy manual.Reference Fowler, Hodgekins, Berry, Clarke, Palmier-Claus and Sacadura17 First, efforts were made to initiate engagement and develop a positive therapeutic relationship, with assessment of goals and barriers used to derive a social recovery formulation. Sessions were intended to be weekly at outset, reducing to fortnightly or monthly towards the end of the intervention period. Behavioural assessment during activities in the community informed the assessment and formulation. Following this, therapy focused on increasing time spent in structured activities linked to personal goals. Cognitive techniques promoted hopefulness and addressed negative beliefs about the self and others. Multi-layered behavioural experiments were used to manage symptoms while participants were engaging in structured activity; examples are provided in the therapy manual.Reference Fowler, Hodgekins, Berry, Clarke, Palmier-Claus and Sacadura17 SRT appears to improve structured activity through augmenting positive self-beliefs.Reference Hodgekins and Fowler22 The SRT therapists were clinical psychologists, occupational therapists, or mental health nurses with CBT accreditation. All the therapists received training in SRT and regular expert individual and peer supervision. Three raters measured SRT adherence with our developed checklistReference Lowen, Hodgekins, Pugh, Berry, Fitzsimmons and French23 using session audiotapes and therapist notes. Interrater reliability was excellent; Krippendorff's α = 0.9 (95% CI 0.87–0.98). A full SRT dose was defined as six or more sessions, with a social recovery assessment and formulation, and two or more pieces of behavioural work in the community with the therapist. Adherence data showed that 64% of sessions included behavioural work, 36% of which included a behavioural experiment. Of the face-to-face sessions, 53% were delivered in the participant's home, 24% in the community (e.g. meeting in a city centre), 10% in an educational setting (e.g. meeting at college) and 13% in a clinic setting. Therapist competence was rated using session audiotapes. Competence was defined as a total score ≥36 on the Revised Cognitive Therapy Scale (CTS-R).Reference Blackburn, James, Milne, Baker, Standart and Garland24 The CTS-R measures the therapist's general competence in delivering cognitive therapy, i.e. using therapeutic skills and techniques, such as collaboration and feedback, to support cognitive change.
Outcomes
Participants were assessed at baseline, 9 and 15 months post-randomisation, with limited assessment of maintenance at 24 months. Research assistants used flexible, assertive engagement to facilitate involvement, conducting assessments mainly in participants’ homes. High interrater reliability for assessor-rated measures was ensured through regular supervision and training.
The primary outcome was weekly hours spent in structured activity.Reference Hodgekins, French, Birchwood, Mugford, Christopher and Marshall9 Using a structured interview derived from the Office for National Statistics Time Use Survey,Reference Short25 time spent over the past month in structured activity was captured. Past month activity was divided to reflect average weekly hours in constructive economic (paid and voluntary employment, childcare, housework and chores) and structured activity (constructive economic activity plus sports and leisure). The primary end-point was 15 months post-randomisation.
Levels of attenuated psychotic symptoms were measured using the Comprehensive Assessment of At Risk Mental States (CAARMS). Derived outcomes included transition to psychosis and CAARMS symptom severity and symptom distress scores.Reference Morrison, Stewart, French, Bentall, Birchwood and Byrne26 Negative symptoms were assessed using the Scale for Assessment of Negative Symptoms (SANS). General psychopathology was measured as change in mood, anxiety, somatoform and eating disorders using the Structured Clinical Interview for DSM-IV, and additionally with the self-report Beck Depression Inventory II (BDI-II), Social Interaction Anxiety Scale (SIAS), and the assessor-rated Global Assessment of Functioning (GAF), Global Assessment of Symptoms (GAS) and Social and Occupational Functioning Scale (SOFAS). Putative mediators were assessed using the Acceptance and Action Questionnaire II (AAQ-II), Meaning in Life Questionnaire (MLQ), Trait Hope Scale (THS), Brief Core Schema Scales (BCSS) and Schizotypal Symptoms Inventory (SSI). Putative moderators were verbal memory, captured using the Logical Memory I subtest of the Wechsler Memory Scale, Third Edition (LMS), and verbal fluency, captured using the Controlled Oral Word Association Test (COWAT). Other outcomes were scores on the Beck Hopelessness Scale (BHS), Alcohol Use Disorders Identification Test (AUDIT) and Drug Use Disorders Identification Test (DUDIT). Health economic outcomes were NHS and personal social service use, captured using the Health Service Resource Use Questionnaire adapted from the Client Service Receipt Inventory (CSRI), and health-related quality of life, captured using the EuroQol EQ-5D-3L. Adverse events were recorded throughout the trial and reported to trial oversight committees.
Statistical analysis
Primary and secondary hypotheses were pre-registered (ISRCTN47998710; 29 November 2012) and published in the protocol.Reference Fowler, French, Banerjee, Barton, Berry and Byrne1 A detailed statistical analysis plan was agreed between the chief investigators, trial manager, trial statistician and health economist on 4 July 2018, prior to analysis. The primary analysis was intention to treat (ITT) comparing SRT plus ESC with ESC alone on weekly structured activity hours at 15 months post-randomisation. A per protocol analysis was also conducted, involving participants who received full-dose SRT. All analyses were conducted by the trial statistician and health economist. All hypothesis testing was conducted using a two-sided significance level of 5%, with corresponding 95% confidence intervals.
We anticipated that the primary outcome might have positive skew and require a logarithmic transformation. Assuming normal (or transformed to normal) distribution, a general linear model was constructed for primary and then secondary analyses. For the primary outcome analyses, baseline logical memory and verbal fluency were included as prognostic variables, alongside stratification variables (site as a random factor) and allocation. Secondary outcomes were analysed using an analogous approach: a linear model with appropriate link for the outcome (e.g. logistic regression for binary outcomes) and including stratification variables, pre-defined prognostic variables and allocation. Available baseline values of the outcome were included. Planned moderation analysis considered the impact on the intervention effect of baseline social disability (low or very low functioning), ARMS status, logical memory and verbal fluency. One addition was made to the statistical analysis plan after publication of the registered trial protocol: we added models that excluded time spent in childcare, as this variable showed an imbalance towards females that considerably inflates structured activity. Both model types are presented here. Analyses were conducted using SAS for Windows (version 9.4).
Health economic outcomes were analysed using a within-trial cost–utility ITT approach, where costs (at 2017–2018 levels) and benefits were estimated over 24 months, with a 3.5% discount in the second year. SRT costs included therapy training, supervision and delivery. ESC costs were derived from reported service contacts. Total quality-adjusted life-year (QALY) scores were estimated using EQ-5D-3L data. Regression was used to estimate (separately) the mean incremental cost and mean QALY gain. The incremental cost-effectiveness ratio (ICER) (mean incremental cost/mean QALY gain) was estimated, with value for money corresponding to the cost-effectiveness threshold of £20 000 per QALY. The level of uncertainty, according to the cost-effectiveness acceptability curve, was assessed at the same cost-effectiveness threshold value. Multiple imputation was used in the base-case analysis.
Results
One hundred participants were recruited in an internal pilot, from 1 January 2013 to 1 February 2014 (n = 50 in East Anglia and n = 50 Manchester). The remaining 170 participants (n = 57 in Sussex, n = 59 in East Anglia and n = 54 in Manchester) were recruited during an extension phase between 1 September 2015 and 31 May 2017. In total, 270 participants were randomised to receive social recovery therapy (SRT) plus enhanced standard care (ESC) (n = 138) or ESC alone (n = 132). Baseline characteristics were similar across groups (Table 1). The ESC alone group was evenly balanced between sexes, but the SRT plus ESC group over-represented males. Baseline data (Table 2) reflect severe social disability and psychiatric health symptoms. Most participants met diagnostic criteria for major depression and almost half for current social phobia.
Table 1 Baseline characteristics of the study populationa
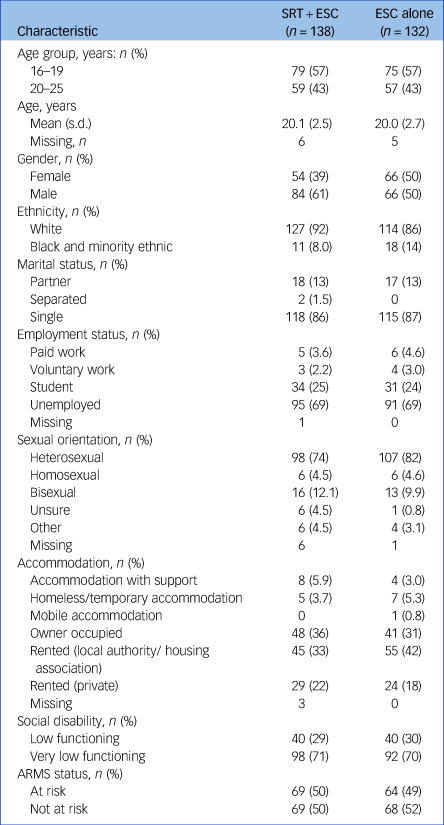
SRT, social recovery therapy; ESC, enhanced standard care; ARMS, at risk mental state for psychosis.
a. Group differences were not statistically tested at baseline.
Table 2 Descriptive outcome dataa
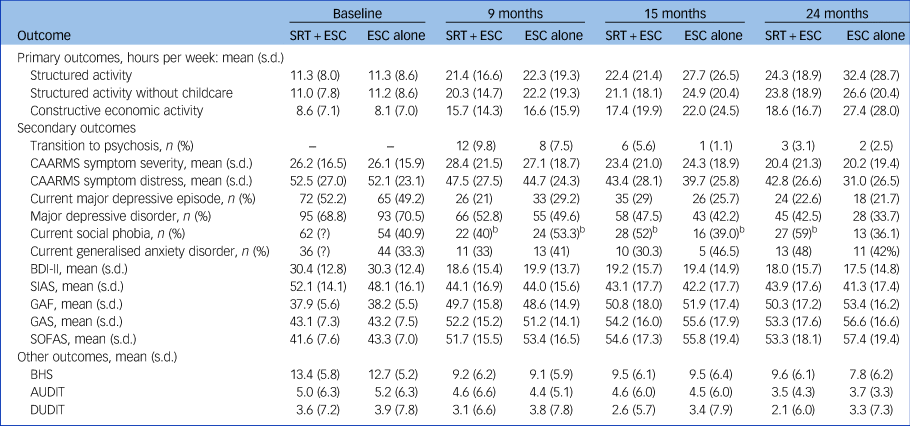
SRT, social recovery therapy; ESC, enhanced standard care; CAARMS, Comprehensive Assessment of At Risk Mental States; BDI-II, Beck Depression Inventory II; SIAS, Social Interaction Anxiety Scale; GAF, Global Assessment of Functioning; GAS, Global Assessment of Symptoms; SOFAS, Social and Occupational Functioning Scale; BHS, Beck Hopelessness Scale; AUDIT, Alcohol Use Disorders Identification Test; DUDIT, Drug Use Disorders Identification Test. Dashes indicate the variable was not captured at baseline.
a. At 9 months, 15 months and 24 months, for each diagnosis, the prevalence is based on the total number at baseline with a positive diagnosis (discounting ‘missing’ or negative diagnosis at baseline). Follow-ups were conducted between 30 November 2012 and 13 June 2019.
Participants allocated to SRT received a mean of 16.77 therapy sessions, with a range of 0 to 33. SRT adherence ratings demonstrated that 91 (66%) participants received the full dose, 23 (17%) a partial dose and 24 (17%) no dose (n = 2 attended zero sessions). Seventy-five session tapes, at least one per therapist, were rated for competence. The mean CTS-R score was 47.24, with 97% of sessions rated above the competence threshold of 36. ESC provision was substantial in both arms. Over 80% of participants in both arms accessed NHS mental health services at trial entry, which continued for more than two-thirds throughout the intervention period, and for more than half throughout the trial. Between each assessment point, a mean of 38% of ESC and 39% of SRT participants saw a care coordinator or case manager on average 9–11 times, and 33% of ESC and 25% of SRT participants saw a psychological therapist, on average for 7–12 sessions. An average of 66% of ESC and 72% of SRT participants saw their general practitioner on average 3–5 times between each assessment point. An average of 19% of ESC and 14% of SRT participants saw a psychiatrist between each assessment point, on average 1–3 times. An average of 51% ESC and 54% of SRT participants reported antidepressant use, and a substantial minority reported use of other medications, between each assessment point. One-third of participants in both arms reported support for employment over the trial for a mean total of 11.3 (ESC: range 0.3–76.5 h) and 75.3 h (SRT: range 0.5–842.4 h). Over 40% of ESC participants and 32% of SRT participants reported other contact with youth, financial, educational, social, housing, statutory and telephone support services over the trial, for a mean total of 14.6 (ESC: range 0.2–225.0 h) and 7.9 h (SRT: range 0.2–74.0 h).
Overall, 235 (87%) participants provided data for the primary outcome of weekly hours in structured activity at 15 months post-randomisation, with data missing for 13% of participants (n = 11 in the SRT plus ESC group, n = 24 in the ESC alone group; Fig. 1 and Table 2). The primary ITT analysis provided no evidence for the superiority of SRT plus ESC over ESC alone in improving structured activity or constructive economic activity (Table 3). Interaction terms for ARMS status (in an at risk mental state for psychosis versus not) and social disability (low versus very low functioning) were non-significant. There was no evidence for the superiority of SRT plus ESC over ESC alone for structured activity at 9 or 24 months post-randomisation (Table 3). At 24 months, there was weak evidence of greater structured activity in the ESC alone group (Table 3). The per protocol analysis was consistent with the ITT analysis at all time points (Table 3). General linear models did not provide any evidence for the superiority of SRT over ESC at any assessment point in terms of transition to psychosis, attenuated psychotic symptoms, general mental health or other symptoms (Table 4). There was no evidence of the superiority of SRT for negative symptoms or rates of diagnosable mood, eating or somatoform disorders (supplementary information, available at https://doi.org/10.1192/bjp.2021.206). It is notable that in both trial arms, significant improvements were made from baseline to follow-up in time spent in structured activity, reduction in depression and anxiety symptoms and diagnoses, and improvements in other symptoms and markers of psychological well-being.
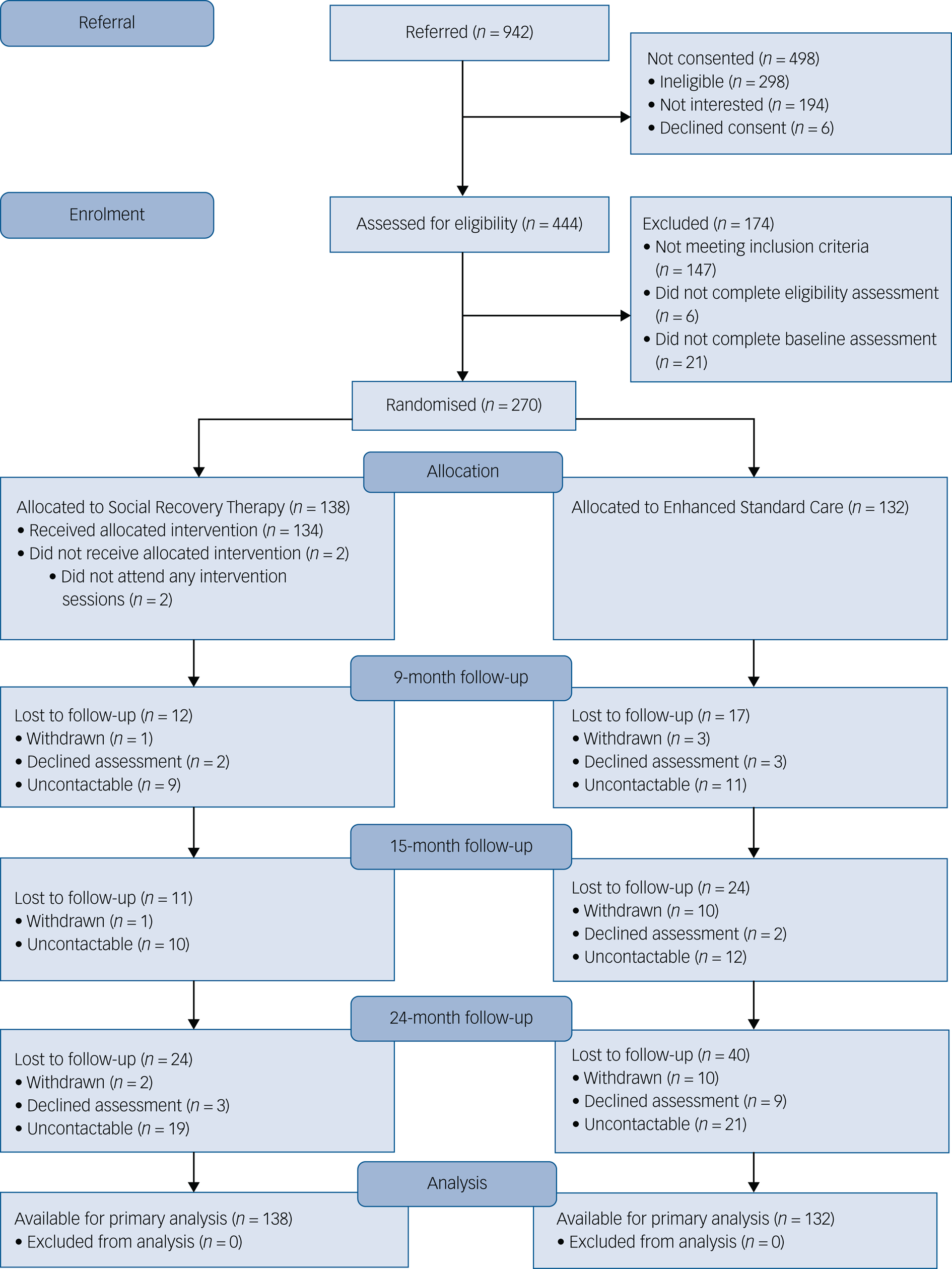
Fig. 1 Participant flow diagram.
Table 3 Pre-specified primary outcome analysis, and secondary time use outcome analysis, using intention-to-treat population and per protocol populationa
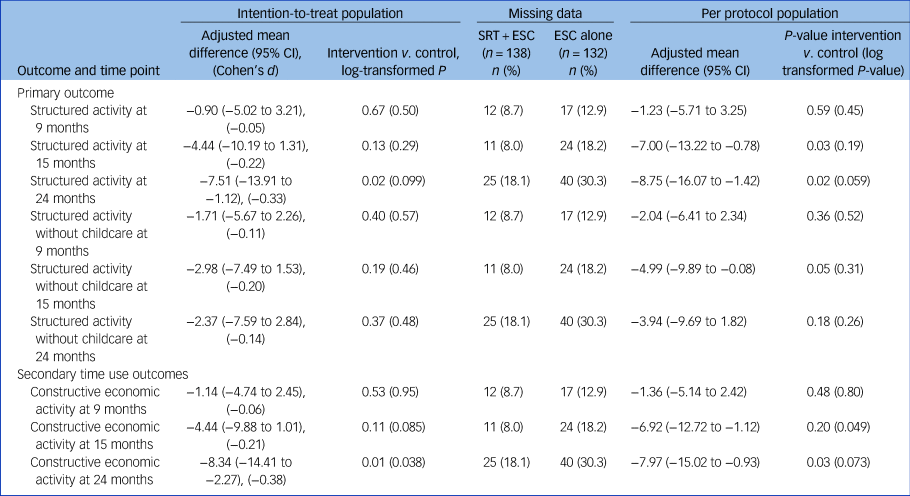
SRT, social recovery therapy; ESC, enhanced standard care.
a. The 24-month assessment point was a late addition to the study protocol during the internal pilot at funder request and therefore reflects greater missing data. For log-transformed outcomes, the P-value comes from the log-transformed data analysis but estimates and confidence intervals are in the original units.
Table 4 Pre-specified secondary and other outcome analysis using intention-to-treat populationa
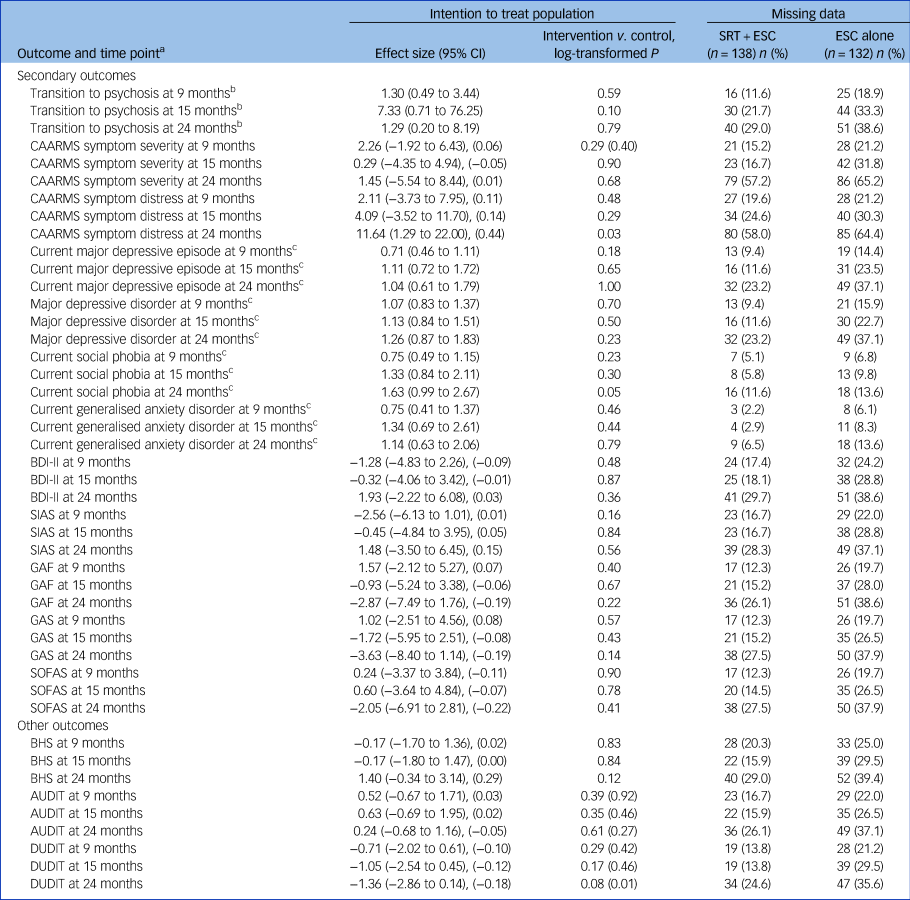
SRT, social recovery therapy; ESC, enhanced standard care; CAARMS, Comprehensive Assessment of At Risk Mental States; BDI-II, Beck Depression Inventory II; SIAS, Social Interaction Anxiety Scale; GAF, Global Assessment of Functioning; GAS, Global Assessment of Symptoms; SOFAS, Social and Occupational Functioning Scale; BHS, Beck Hopelessness Scale; AUDIT, Alcohol Use Disorders Identification Test; DUDIT, Drug Use Disorders Identification Test.
All other effect sizes are given as adjusted mean differences, with Cohen's d additionally provided in parentheses.
a. The 24-month assessment point was a late addition to the study protocol during the internal pilot at funder request and therefore reflects greater missing data.
b. Effect size: odds ratio.
c. Effect size: relative risk..
Primary outcome missing data was 11% at 9 months and 24% at 24 months post-randomisation. Missing data was greater for secondary outcomes across time points (Table 2). Moreover, there was evident differential missingness and a bias towards greater attrition in the ESC alone arm throughout the trial. Missing data modelling was performed using full information maximum likelihood and multiple imputation approaches. The missing data analysis was consistent with the ITT analysis and provided no evidence for the superiority of SRT plus ESC compared with ESC alone on any outcome.
There were 84 adverse events and 83 serious adverse events during the trial, affecting 59 and 42 individuals respectively. More serious adverse events, for example medication overdose, were reported by SRT plus ESC participants (n = 53) compared with ESC participants (n = 30). However, event frequencies became very similar when adjusting for only those reported at trial assessments and excluding those reported to SRT therapists: (SRT plus ESC: n = 36; ESC alone: n = 30). No events were attributable to the trial.
For health economic outcomes, the mean total intervention cost per SRT participant was £3268.94 (SRT plus ESC was estimated at £5927.73) versus £2420.61 for ESC alone. The mean incremental cost for SRT was estimated to be £3910.59 (range: £2708.32–5112.86) compared with ESC, with a QALY gain of 0.001 (range: −0.099 to 0.10). Therefore, SRT was not estimated to be cost-effective.
Discussion
The aim of this trial was to determine the clinical and cost-effectiveness of adding social recovery therapy (SRT) to enhanced standard care (ESC), compared with ESC alone, for young people with social disability and severe and complex mental health problems. We found no evidence of the superiority of SRT as an adjunct to ESC in the primary outcome of weekly hours in structured activity at the primary 15-month end-point or at 9 or 24 months post-randomisation. We found no evidence that SRT was superior to ESC in secondary or other outcomes at any time point. SRT was not estimated to be cost-effective.
On some outcomes, including negative symptoms at 15 months and structured activity at 24 months post-randomisation, there were mean differences in favour of ESC alone. However, these findings were inconsistent and rarely approached statistical significance. For other outcomes, including depression and anxiety diagnoses and drug use, there was weak evidence in favour of SRT plus ESC. Similarly, these results were inconsistent and not statistically significant.
There were very large gains made in both trial arms across primary and secondary outcomes. In both trial arms, there was an average gain of 11 h in structured activity at 15 months post-randomisation, which constitutes an almost threefold increase in clinically meaningful effect. There was more than 50% reduction in the prevalence of diagnosable depression, social phobia, panic disorder and agoraphobia in both groups, and large improvements in self-reported depression, social anxiety, hopelessness, schizotypy, and drug and alcohol disorders. This was surprising as only a minority of young people with emerging complex problems show reliable improvements following specialist youth mental health service provision.Reference Cross, Scott, Hermens and Hickie4 Current participants had greater symptomatology than those in this prior study and therefore more change may have been possible. However, current participants had been experiencing significant difficulties for at least 6 months and were accessing treatment as usual, so change without specialist intervention was unexpected. Nonetheless, our results support those of the IMPACT adolescent depression trial,Reference Goodyer, Reynolds, Barrett, Byford, Dubicka and Hill27 in which optimised case management (i.e. including, as per this trial, psychological, employment and practical support) appeared equally effective with and without the addition of different psychotherapies. Moreover, recent studies demonstrate that some individuals at elevated risk of psychosis may show symptomatic and functional improvement over time.Reference Yung, Nelson, Thompson and Wood28 The present sample was heterogeneous with respect to symptoms and comorbidities and therefore may have included participants who naturally recovered, in addition to subgroups who responded well to shorter- or longer-term specialised interventions.Reference Hickie, Scott, Hermens, Naismith, Guastella and Kaur29
Anticipating that standard care might be limited and inaccessible, we provided thorough assessment feedback and a best practice referral guide. The data show that comprehensive packages of evidence-based interventions of case management, psychological therapy, medication and support with employment were delivered to both arms of the trial in three youth mental health centres of excellence. It is important that the large gains made in social and clinical recovery occurred in the context of this very active and comprehensive provision, which constituted optimal care according to NICE guidelines. In the context of such comprehensive evidence-based care, what the trial perhaps shows is that providing further adjunctive specialised social recovery therapy is not required. Further research is warranted in understanding how benefits occurred and the factors associated with improvement. The implication for services is to try to actively engage, and deliver comprehensive assessment and treatment, to maximise outcomes for this often-neglected group.
Participants’ experience of the trial
Our qualitative process evaluation found that SRT was experienced positively by the participants interviewed, that SRT was challenging but beneficial, and that it provided participants with a positive therapeutic relationship and specific tools needed to pursue social recovery goals.Reference Gee, Notley, Byrne, Clarke, Hodgekins and French21 Participants in both arms described benefits of trial involvement, experiencing the assessment process as facilitating self-reflection and highly valuing contact with warm, empathic assessors.Reference Notley, Christopher, Hodgekins, Byrne, French and Fowler20 SRT was contrasted with standard care, which participants described as too limited.Reference Gee, Notley, Byrne, Clarke, Hodgekins and French21 It is notable that trial assessment procedures were experienced by participants as facilitating hopeReference Notley, Christopher, Hodgekins, Byrne, French and Fowler20,Reference Gee, Notley, Byrne, Clarke, Hodgekins and French21 and may have increased standard treatment engagement alongside our deliberate attempts to encourage providers to offer comprehensive treatment packages. Our previous SUPEREDEN3 trialReference Fowler, Hodgekins, French, Marshall, Freemantle and McCrone19 found that SRT as an adjunct to EIP was superior in improving social and clinical recovery. Thus, adjunctive SRT may become necessary and effective only following transition to psychosis and, moreover, in a group characterised by greater homogeneity, i.e. male gender, and persistent and severe symptoms and social disability despite prior provision of specialist mental health services, such as in the SUPEREDEN3 trial.Reference Fowler, Hodgekins, French, Marshall, Freemantle and McCrone19 This is in keeping with the plasticity of the adolescent brain, which while conferring heightened vulnerability also provides greatest receptivity and malleability to resilience-enhancing factors, meaning that adolescence is a period of greatest therapeutic gains.Reference Malhi, Das, Bell, Mattingly and Mannie30 Further research is needed to disentangle the characteristics that distinguish persistence of social disability in psychosis from what appears from this trial to be greater responsivity to treatment in the absence of psychosis but in the presence of mental health problems of equivalent severity and complexity.
Limitations
As evident at baseline, trial participants were extremely withdrawn and severely symptomatic. The inclusion of this group in an intervention trial was challenging. We made considerable efforts to engage and retain participants but despite this, there was marked missing data, with greater disengagement in the control arm. There was an overrepresentation of males in the SRT plus ESC arm. Sex was not a stratifier, nor was any related analysis planned a priori, and the sex imbalance might have biased estimates. Nonetheless, the primary outcome analysis was regarded as appropriate and within pre-specified limits against bias, and alternative missing data models, full information maximum likelihood and multiple imputation were used to support this.
Future research and clinical implications
Future research should aim to further explore the factors associated with youth mental health problems that are persistent and resistant to standard treatment,Reference Cross, Scott, Hermens and Hickie4,Reference Cross, Hermens and Hickie5 and the characteristics and mechanisms associated with good response to existing intervention packages. Future research should identify how to optimise standard care depending on need and how to implement optimal combinations of evidence-based interventions for young people with complex problems.Reference Cross, Scott, Hermens and Hickie4,Reference Cross, Hermens and Hickie5 This may involve the consideration of stepped-care approaches to identify young people who are more treatment-resistant and require longer-term specialist social recovery intervention.Reference Cross, Scott, Hermens and Hickie4,Reference Cross, Hermens and Hickie5 Existing research suggests that young people with severe and complex problems struggle to access interventions.Reference Cross, Scott, Hermens and Hickie4,Reference Cross, Hermens and Hickie5 However, this study shows that, even with very severe social disability and complex mental health problems, young people can make very significant improvements if comprehensive packages of evidence-based care are provided. Such packages include detailed engagement and assessment, and access to psychological therapies and vocational support, alongside medical and social interventions. The gains obtained by such provision have been shown to be large in this study, and in this context, the addition of specialised social recovery therapy does not provide superior social or clinical recovery, nor is it cost-effective. The message of this trial is to recommend equitable provision of optimised evidence-based care packages for clinical and social recovery within services that are appropriate and accessible for young people. Participants in the trial's process evaluation emphasised the importance of motivation and self-agency in social recoveryReference Notley, Christopher, Hodgekins, Byrne, French and Fowler20,Reference Gee, Notley, Byrne, Clarke, Hodgekins and French21 and delivering this care to young people in the context of hopefulness appears essential.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2021.206.
Data availability
The data that support the findings of this study are available from the corresponding author on reasonable request.
Acknowledgements
We are very grateful to the young people who participated in the trial and all family members, friends, referring services, clinicians and other people who supported their involvement. We thank the PRODIGY Advisory Team, Trial Steering Committee, and Data Monitoring and Ethics Committee members for their invaluable involvement and guidance throughout this trial. We wish to acknowledge the support of our National Institute for Health Research programme manager. We thank all staff in the sponsoring and hosting organisations for supporting the project. We are grateful to Norwich Clinical Trials Unit for their support with data management, statistical and health economic analysis. Finally, we thank all the PRODIGY therapists and research assistants for their enthusiasm and dedication to supporting participants in their involvement with PRODIGY.
Author contributions
D.F. and P.F. were co-chief investigators for this trial. T.C. and C.B. were pilot and extension phase trial managers respectively. C.B. wrote the first draft of this manuscript with D.F. and J.H.. L.S. and G.B. analysed the data. J.H., T.C., L.S., G.B., C.N., R. Byrne, R. Banerjee, K.G., R.F., S.P., J.W. and A.R.Y. were co-investigators and contributed to the study design and delivery. All authors contributed to and approved this final manuscript. Multiple authors had access to the complete study data and the authors were fully responsible for the decision to publish this manuscript.
Funding
This project was funded by the National Institute for Health Research Health Technology Assessment programme (10/104/51, 10/104/501). The funding source had no role in the design of the study, data collection, analysis, interpretation nor in this manuscript.
Declaration of interest
None.









eLetters
No eLetters have been published for this article.