Child sexual abuse (CSA) and lack of parental care are associated with depression in adults (Reference Bifulco, Brown and AdlerBifulco et al, 1991; Reference Mullen, Martin and AndersonMullen et al, 1993; Reference Fergusson, Horwood and LynskeyFergusson et al, 1996). However, in spite of the marked contrasts in the nature of these experiences, little is known about possible differences in the way they confer risk. Depressive disorders in adults are also associated with deficiencies in the quality and quantity of personal relationships, and these may mediate or moderate associations with childhood adversities (Reference Brown, Bifulco and VeielBrown et al, 1990). We predicted that adult relationships would play a different role in relation to risk for adult depression following CSA compared with that following poor parental care, thus suggesting a difference in mechanism. Relationships may be associated with depression because they are cause or consequence, or because both are influenced by a third variable. Examination of associations over time can help clarify the nature of the association. The temporal relations of intimate relationships and depression were examined, within the constraints of this retrospective study.
METHOD
Sample
Subjects were identified from among women who were living on the Wirral, a borough of Merseyside, in north-west England. Sampling was carried out in two phases: the first used questionnaire measures, and the second standardised interviews. Questionnaires were mailed to all women aged 25-36 years who were on the lists of five primary care practices, chosen because they covered areas with a wide range of socio-economic conditions. The aim was to recruit a sample with a distribution of childhood socio-economic status similar to that of the population of the UK in the mid-1970s, when the subjects were children.
First-phase questionnaires were posted out in batches of 200-300, targeting each practice in turn. These had an explanatory letter from the woman's primary care practitioner and questions covering childhood experiences and adult mental health problems. A second questionnaire was sent 6-8 weeks later to non-responders, and after a further 6-8 weeks a card was sent to those who had not responded enquiring whether they might at a later date be able to return a questionnaire. The response rate was 60.7% after accounting for those known to have moved. The possibility of bias arising from mental health problems in non-responders was investigated by comparing the primary care records of 99 responders and 101 non-responders (further details available from the author upon request). There were no significant differences between responders and non-responders in rates of psychotropic prescribing or referrals to secondary mental health services over a 2-year period.
Of the 1181 returned questionnaires, 44.5% were from women who had grown up in households from socio-economic groups I to IIIN according to the UK Standard Occupation Classification (Office of Population Censuses and Surveys, 1990), compared with the national figure for 1975 of 37% reported in the General Household Survey (Office of Population Censuses and Surveys, 1993).
The second-phase interview subjects were drawn at random from the 1181 responders using the random selection facility of ‘select cases’ in the Statistical Package for the Social Sciences, from three strata, defined on the basis of reported CSA before the age of 16 years (Reference Mullen, Martin and AndersonMullen et al, 1993), low maternal care in the Parental Bonding Instrument (Reference Parker, Tupling and BrownParker et al, 1979) without reported CSA, and the remainder. However, after August 1997, as a result of low specificity of the low-care stratum for the serious neglect with which we were concerned, the second stratum was redefined to require both low maternal and low parental care. Sampling fractions varied from practice to practice as it was considered un-reasonable to assign for interview subjects who had completed first-phase questionnaires more than 1 year previously, and the interviewing rate over the course of the study varied with staffing. Once assigned, 79% of these women agreed to take part and provided completed interviews.
Second-phase sampling weights were calculated in two steps, each being based on logistic regression models. The first was concerned with the sampling design and included the original and revised stratification and practice. The second was concerned with non-response after assignment, and although stratum, practice and interviewer were all included as predictors of response, only the interviewer effects were significant. The inverse of the product of the predicted probabilities from these two models was used as the combined sampling and response weight. Re-weighting the interviewed sample of 198 gave estimates for the population of women from which they were drawn as having, at the time of questionnaire return, a mean age of 30.8 years (s.d. 2.9), 1.3 (s.d. 1.2) children, with 69% working, 62% with a partner and having come from families with 2.4 (s.d. 1.9) siblings.
Procedure
Women selected for the second-phase interview were contacted by telephone or letter and asked to participate. All of the interviewers were female. The childhood and adult interviews were carried out and rated independently by two interviewers. All of the interviews were audiotaped, and ratings made from the recordings. Subjects were offered £30 on completion of the interviews. The study was approved by the Wirral Health Authority ethical committee.
Measures
Recalled childhood experiences were assessed using the Childhood Experience of Care and Abuse interview (Reference Bifulco, Brown and LillieBifulco et al, 1997). This enquires in detail about a range of positive and negative experiences, including companionship, antipathy, neglect, physical abuse, psychological abuse, institutional care and sexual abuse. Adversities are rated as marked, moderate or mild, and only ratings of ‘marked’ or ‘moderate’ are taken as denoting presence of abuse or neglect. In this report neglect and experiences in care have been combined into a ‘poor parental care’ variable. The interviewers were trained by the principal developer of the measure (Antonia Bifulco), and difficult ratings were reviewed with her regularly.
Depression in adult life was assessed using the Schedule for Affective Disorders and Schizophrenia (Reference Spitzer and EndicottSpitzer & Endicott, 1975). The questions were adapted so that research diagnostic criteria (RDC) and DSM-IV ratings of major depression since the age of 16 years could be made (American Psychiatric Association, 1994). The onset and duration of all episodes were recorded so that they could be assigned to age periods. The interviewers were trained by J. H., who participated in the development and evaluation of the investigator-based version of the measure used in this study (Reference Harrington, Hill and RutterHarrington et al, 1988). Ratings were reviewed regularly with J. H. None of the interviewers and raters, with the exception of R. D., were clinicians. Reliability of the ratings by the non-clinicians was checked by comparison with those of the psychiatrist (R. D.) from the audiotapes of 20 subjects. There was one disagreement in rating DSM-IV major depression in the 5-year age periods 21-25 years and 26-30 years (κ=0.91). Adult love relationships were assessed using the Adult Personality Functioning Assessment (APFA) interview (Reference Hill, Harrington and FudgeHill et al, 1989). This enquires about functioning over periods of 5 years or 10 years in six domains: work, love relationships, friendships, non-specific social interactions, and negotiations and coping. Ratings are made in each domain and over each period on a scale of 0 to 5, where 0 reflects a high level of adaptation and 5 very poor functioning. The scoring system ensures that any period over which there is significant dysfunction is rated as 3, 4 or 5, so that binary variables indicating presence or absence of dysfunction can readily be generated for each domain. Previous studies have demonstrated good interrater reliability and subject—informant agreement, and have shown that pervasive dysfunction in the APFA is associated with personality disorder (Hill et al, Reference Hill, Harrington and Fudge1989, Reference Hill, Fudge and Harrington1995, Reference Hill, Fudge and Harrington2000). In this study ratings over the 10-year age period 21-30 years have been used to examine links between relationships, depression and childhood adversities, and functioning over the age periods 21-25 years and 26-30 years to test for temporal sequences between love relationships and depression. Further interviews covering childhood psychopathology, adult attachment status and personality disorder were also carried out, but are not discussed here.
Variables and analyses
In the majority of analyses DSM-IV major depression was the outcome variable of interest within logistic regression. In this study CSA, neglect and institutional care (but not physical abuse) were each independently associated with adult depression (further details available from the author upon request). As the numbers who experienced institutional care were low, the ‘neglect’ and ‘in-care’ variables were combined to form an index of ‘poor parental care’. To obtain correct effect estimates and their confidence intervals required proper account to be taken of the two-phase study design (Reference Pickles, Dunn and Vazquez-BarqueroPickleset al, 1995). This was achieved by the inverse probability weighting, as described by Dunn et al (Reference Dunn, Pickles and Tansella1999), all analyses being performed in STATA (StataCorp, 1999). Reported probability values are calculated from t and F tests using the survey-based parameter covariance matrix.
RESULTS
The findings reported here refer to the 198 subjects who were interviewed in the second phase. Of these, 71 had experienced moderate or marked child sexual abuse; 50 had experienced moderate or marked neglect; and a further 8 were taken into care during childhood. Thus, a total of 58 had experienced poor parental care. Weighting back to the general population questionnaire sample, 71% were exposed to neither CSA nor poor care, 11% to poor care only, 10% to CSA only and 8% to both. Both CSA and poor parental care were associated with DSM-IV major depression in the age period 21-30 years, with simple (weighted) odds ratios of 6.10 (95% CI 2.83-13.12) and 7.90 (CI 3.48-17.89) respectively. Logistic regression of depression with both CSA and poor parental care as predictors suggested a negative interaction term (P=0.05), implying that the effect of CSA and poor care together was less than the product of the odds ratios expected under the simple ‘main effects only’ model. The odds ratio for CSA alone was 8.76 (CI 3.12-24.54), for poor parental care 11.77 (CI 3.69-37.57) and for the combination of CSA and poor parental care 17.61 (CI 5.71-54.35).
Two participants did not want to talk about love relationships and so the sample size was reduced to 196 for these analyses. Child sexual abuse and poor childhood care were each independently associated with poor love relationships over the age period 21-30 years; the odds ratio for CSA was 4.16 (CI 1.95-8.87) and for poor care was 4.65 (CI 2.02-10.59). There was no significant interaction term. However, as was the case for depression, the risk associated with the combination of CSA and poor care was less than expected if there were multiplicative effects of the childhood factors.
Poor love relationships in the age period 21-30 years were associated with major depression over the same age period: OR 5.85 (CI 2.45-14.00). This raises the possibility of either poor relationships mediating the effects of adverse childhood experiences on major depression, or major depression mediating the link between adverse experiences and relationships. In order to determine which is the more likely explanation, the temporal association of relationships and depression in the age periods 21-25 and 26-30 years was examined. In a logistic model with both effects, poor love relationships at age 26-30 years were strongly predicted by poor relationships at age 21-25 years: OR 8.71 (CI 2.68-28.25), but not by major depression in the age period 21-25 years: OR 0.93 (CI 0.30-2.89). In contrast, major depression at age 26-39 years was predicted by major depression in the age period 21-25 years: OR 11.15 (CI 3.08-40.27); and by poor love relationships: OR 4.10 (CI 1.64-10.25). Thus, the quality of love relationships was associated with an altered rate of risk of depression in a subsequent age period, and not vice versa.
Having established that the quality of intimate relationships was associated with an altered risk for depression, we return to the question of their possible moderating or mediating role in relation to CSA and poor care in childhood. Mediation is identified by a reduction in the main effects for depression of the childhood risks following the addition of intimate relationships as a predictor. Moderation is identified by an interaction between intimate relationships and the childhood adversity. In the case of poor parental care there was no such interaction (P=0.7) and the main effects model gave an OR estimate of 4.08 (CI 1.68-9.92) for bad intimate relationships and 5.56 (CI 2.24-13.84) for poor care, a reduction of 2.34 from the simple OR for poor care of 7.90. In the case of CSA, a substantial interaction was identified, with an OR of 0.15 (CI 0.03-0.83) (P=0.03). This implied that the quality of intimate relationships had a major impact on those without prior CSA but little effect on those with CSA. Estimated ORs were 8.77 (CI 2.46-31.34) for those with poor intimate relationships only, 13.73 (CI 3.52-53.38) for those with CSA only, and 18.20 (CI 5.16-64.19) for those with both, these last two being little different.
When both the interaction effects of poor care and CSA and also CSA and intimate relationships were fitted within the logistic regression for depression, their estimated effects both remained substantially different from 1 (ORs of 0.25 and 0.22 respectively) and they were jointly significant:F(2,193)=2.96, P=0.05. The estimated odds ratios and predicted rates of depression from this model are shown in Fig. 1. The effect of each risk factor is shown by the branching of the paths, their thickness reflecting the estimated relative frequencies of occurrence. On the right-hand side are given the estimated proportion of women exposed to each combination of risk factors (with the unweighted ‘raw’ frequency in the sample) and the predicted rate of depression from the chosen model (and odds ratio compared with the low-risk category). The separate effects of CSA and poor care described earlier are evident, and it can be seen that CSA in the presence of poor care did not add very much to the risk of depression. It is evident also that in the absence of CSA or poor parental care the overwhelming majority of subjects experienced good love relationships, while in the presence of both childhood adversities two-thirds had poor relationships.
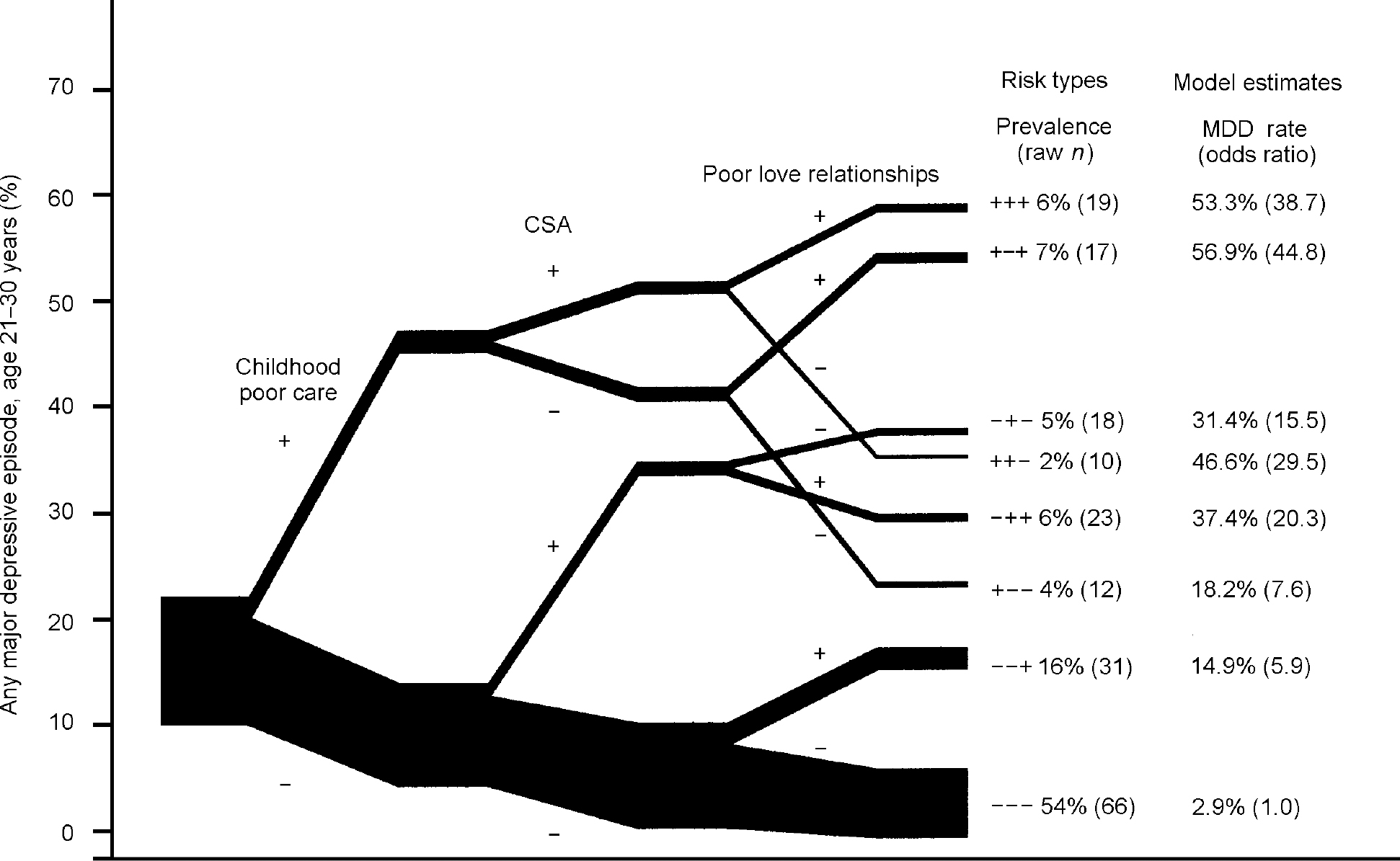
Fig. 1 Childhood experience, adult love relationships and depression. The paths indicate the simple weighted prevalence estimates for depression (y axis). These do not match exactly the estimates on the right, which are derived from a ‘parsimonious’ model. The width of the paths reflects the weighted estimates of the prevalence of risk factor combinations in the population of women. As a consequence of the weighting these do not correspond to the relative frequencies based on the raw n values. CSA, child sexual abuse; MDD, major depressive disorder.
The rates of major depression associated with poor love relationships varied considerably depending on childhood experiences, indicating that relationships differed in the extent to which they mediated the effects of childhood adversity. In the absence of either childhood adversity, poor relationships increased the rate of depression from 2.5% to 16.0%. For the women who had experienced poor care in childhood the rate of depression among those with good love relationships was 22.0% compared with 53.7% where there were poor love relationships. In contrast, in the group that reported CSA only, the rates of depression were similar irrespective of the quality of love relationships (37.4% v. 29.3%). The impact of relationships following both CSA and poor care appeared to be intermediate between those where only one or the other had occurred. Thus, there was little evidence for poor love relationships either mediating or moderating risk associated with CSA. However, it seemed that a history of CSA moderated the effect of relationships — that is to say, the beneficial effects of good relationships were not evident following sexual abuse.
The role of quality of love relationships in modifying risk for depression associated with CSA and poor parental care was explored further in separate analyses of the associations of each risk factor with depression at each level of love relationships. The results for CSA reflected the significant interaction in the logistic model between CSA and love relationships. Child sexual abuse was strongly associated with depression in the presence of good relationships (OR 10.07, P=0.006), but not where there were poor relationships (OR 1.63, P=0.4). The estimated odds ratios for the effect of poor parental care were similar in the contexts of good (OR 3.56,P=0.2) and poor love relationships (OR 4.77, P=0.007), although only the latter was significant, possibly owing to lower statistical power arising from the relatively small number of subjects with a history of poor care and good relationships in adult life.
DISCUSSION
The findings from this study were in many respects consistent with those of previous studies in demonstrating a substantial association between CSA, poor parental care (neglect and institutional care) and risk of major depression in adult life among women. In addition we found that CSA and poor care in childhood were each independently associated with long-term patterns of poor adult love relationships, and that these were associated with major depression over the age period 21-30 years. However, there were marked and potentially informative differences between CSA and poor parental care in the way the quality of love relationships affected risk for depression. The sampling method allowed results from the interview phase of the study to be weighted back to the larger questionnaire sample, and hence provided estimates of the size of effects of the childhood risk factors and adult relationships in the general population.
The role of intimate-love relationships
This study focused on relatively persistent patterns of intimate-love relationships rather than broader social support over short periods of time, for five main reasons. First, the role of intimate-love relationships as risk or protective factors for depression may be different from that of relationships more generally. In particular, they probably represent the most salient, although not the sole, adult attachment relationship, and hence provide an indication of the role of attachment processes in adult life in altering risk of depression (Reference McCarthy and TaylorMcCarthy & Taylor, 1999). Second, relatively stable patterns of functioning are good candidates for enduring vulnerability and protective factors for psychopathology. Third, if there is an effect of childhood experiences on adult functioning, this is likely to be identified as an association with relatively stable characteristics. Fourth, relatively stable interpersonal dysfunction is central to many types of personality disorder (Reference Hill, Ruttei, Rutter, Taylor and HersovHill & Rutter, 1994), and so an estimate of its role creates the possibility of direct links with the assessment of the role of personality functioning more broadly (Hill et al, Reference Hill, Harrington and Fudge1989, Reference Hill, Fudge and Harrington2000). Given the strong association of depression with personality disorder (Reference Nestadt, Romanoski and SamuelsNestadt et al, 1992), it is important to study the interplay between interpersonal functioning, personality functioning and depression (Reference RodgersRodgers, 1996a ). Fifth, although we do not know very much about the way in which relationships do alter risk, many of the most likely explanations imply a temporal sequence whereby relationships need to be established before they can act as a resource. For instance, if good relationships are protective because they are a reliable source of support at times of stress, or they aid problem-solving or promote self-esteem (Reference Brown, Bifulco and VeielBrown et al, 1990), these are unlikely to be immediate outcomes of the establishment of supportive relationships.
The association of both CSA and poor care with difficulties in close relationships over 5-year and 10-year periods suggested that there was an impact of these childhood experiences on relatively stable aspects of relating. The effects of relationships are likely to be evident after these relationships have been established for some time, and therefore there should be both concurrent associations of relationships with depression, and a temporal sequence whereby quality of relationships was predictive of depression. Conversely, if episodes of depression have a negative effect on patterns of close relationships, that should also be evident in a temporal association. We found strong support for a temporal sequence of poor relationships followed by depression, and none for depression followed by poor relationships.
The finding that the association of poor parental care with depression was mediated — at least in part — by poor love relationships was consistent with previous studies. Rodgers (Reference Rodgers1996b ) found that in women aged 43 years, a combination of available emotional support, extent of social network and interpersonal life events mediated the majority of the association between parental care and control (assessed using the Parental Bonding Instrument) and adult affective symptoms. In studies of inner-city mothers, Brown and colleagues showed that childhood adversity comprising neglect, physical abuse or sexual abuse was associated with depression only in the presence of environmental or psychological vulnerability. The environmental component of vulnerability included ‘negative elements in core relationships’ based on difficulties with spouse and children (Reference Brown, Bifulco and VeielBrown et al, 1990). More specific associations of marital support with psychosocial functioning have been shown in studies of children who were raised in residential care (Reference Quinton, Rutter and LiddleQuinton et al, 1984; Reference Rutter, Quinton, Hill, Robins and RutterRutter et al, 1990). Men and women who had been in care had poorer psychosocial functioning than control subjects, but only in the absence of a supportive cohabiting relationship. The likelihood of being in such a relationship was reduced among those with a history of childhood conduct disorder, and altered by a chain of processes in the transition from adolescence to adulthood, including whether the adolescent had shown evidence of planning for work and had entered a cohabitation with a deviant partner by age 20 years (Reference Quinton, Pickles and MaughanQuinton et al, 1993).
Different associations and mechanisms linking childhood adversity and depression
As far as we are aware, the possibility that there might be different mechanisms behind the associations of CSA and poor parental care with depression has not been examined. In this study the difference was striking. The presence of good love relationships did not reduce the risk of depression associated with CSA, and neither did poor relationships add to the risk. In contrast, the quality of love relationships made a substantial difference to the likelihood of depression following poor parental care. This difference is brought out in a comparison of the odds ratios for depression in the presence of the combination of each of the childhood risk factors with love relationships. The odds ratio for depression in the presence of both CSA and good love relationships, compared with no CSA and good love relationships, was 23.5, and in the presence of CSA and poor love relationships it was 16.3. The odds ratio for depression in the presence of poor care and good love relationships was 11.7, but for the combination of poor care and poor love relationships, compared with neither, it was 45.6. The role of love relationships in relation to the combination of CSA and poor care seemed to be intermediate between that of each risk factor occurring alone.
This study had methodological limitations against which these findings should be judged. The use of retrospective measures of childhood adversity has been criticised on several grounds (Reference Maughan and RutterMaughan & Rutter, 1997). Nevertheless, studies of adults with known abuse histories (Reference WilliamsWilliams, 1994), of siblings' reports (Reference Bifulco, Brown and LillieBifulco et al, 1997; Reference Duggan, Sham and MinneDuggan et al, 1998) and of genetic influences on reports of parenting (Reference KendlerKendler, 1996) suggest that reports of major childhood adversities are reasonably robust. The quality of recall of adult lifetime psychiatric disorder is variable (Reference Andrews, Anstey and BrodartyAndrews et al, 1999), although test-retest reliability for depression over similar periods to those in this study have been moderate to good (Reference Prusoff, Merikangas and WeissmanPrusoff et al, 1988; Reference Kendler, Neale and KesslerKendler et al, 1993).
It would not be surprising if there were differences in mechanisms linking child sexual abuse and poor care to depression, given the contrasting nature of the experiences. In the majority of instances of sexual abuse occurring within the general population, the number of incidents experienced by victims is relatively low, and the duration of each incident is generally a few minutes. However, frequently the experience is frightening, confusing, disorienting, painful or shaming, and therefore traumatic. This is likely to lead to the development of active coping strategies to regulate affect. For instance, Williams (Reference Williams and Rubin1996) has proposed that the use of generalised autobiographical memories in adult life may be a consequence of attempts to deal with painful memories associated with childhood trauma. An association of CSA with overgeneral memories was found in a referred sample with depression (Reference Kuyken and BrewinKuyken & Brewin, 1995), and association of overgeneral memories with depression has been demonstrated in studies of referred samples (Reference Williams and ScottWilliams & Scott, 1988). Traumatic stress in childhood may also have an effect on the hypothalamic—pituitary—adrenal (HPA) axis, with consequent vulnerability to depression (Reference Weiss, Longhurst and MazureWeiss et al, 1999). These vulnerabilities to depression may be relatively independent of the quality of intimate-love relationships. In contrast, neglect is generally chronic and so likely to affect a child's sense of self-worth, but is not associated with high affect, and so is less likely to require active regulatory strategies or lead to disturbances of the HPA axis.
A second crucial difference concerns the context of CSA and neglect and institutional care. Child sexual abuse occurring in the absence of poor parental care commonly is perpetrated by someone who is not a parental figure (82% in this study), and so is unlikely to have an effect on the child's attachment security. Neglect is perpetrated by parental figures, and institutional care generally entails disruption of links with parental figures and exposure to multiple caretakers. This is likely to lead to insecure attachment and to low self-esteem, which is closely linked to the quality of intimate relationships. Under these circumstances the vulnerability to depression is likely to be influenced markedly by the quality of adult attachment relationships.
The findings reported here, if replicated, provide pointers to heterogeneity in the origins or recurrence of depression. They imply that the mechanisms associated with depression following CSA and following neglect or institutional care are different, and this should be evident in differences of biological and psychological, as well as interpersonal, processes.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
• The causes of onset or recurrence of depression in adult life may be different depending on recalled childhood experiences.
-
• Risk of depression is strongly associated with quality of adult intimate-love relationships in some women.
-
• Depression following reported child sexual abuse and poor parental care may require different therapeutic approaches.
LIMITATIONS
-
• Child and adult measures were retrospective.
-
• No account was made in the design for genetic influences on depression.
-
• Low numbers in some of the subgroups of interest limited statistical power.




eLetters
No eLetters have been published for this article.