Suicide is a major public health concern, and factors that predict and protect against suicidal behaviours need to be better understood in order to develop prevention and intervention strategies. Cannabis is the most commonly used illicit drug worldwide, with usage increasing in low- and middle-income and in high-income countries. Reference Hall and Degenhardt1 A recent systematic review found a reasonably consistent relationship between cannabis use and subsequent risk of psychotic outcomes, but much less consistent and overall weaker evidence of association with depression, anxiety and suicidal ideation as outcomes. Reference Moore, Zammit, Lingford-Hughes, Barnes, Jones and Burke2 However, owing to the scarcity of epidemiological research and difficulties inherent in interpretation of results from observational studies, there remains uncertainty concerning many of the adverse psychological consequences of cannabis use. It is clear that the relationship between cannabis and suicide has not been studied in great detail, especially prospectively, Reference Wilcox, Conner and Caine3 and requires further study. One reason for the scarcity of empirical data concerning suicide risk in relation to cannabis use may simply be the fact that suicide is such a rare outcome. Perhaps for this reason, almost all previous studies examining cannabis and suicide have examined suicidal behaviours such as suicidal ideation and attempts rather than completed suicide. Those exhibiting suicidal behaviours undoubtedly share some similar characteristics with those who actually complete suicide, but there are clear differences in terms of the underlying pathology and risk factors for these behaviours.
It is conceivable that cannabis use could lead to an increased risk of suicide through a number of different mechanisms, including neurobiological effects, Reference Vinod and Hungund4 development of mental health problems such as depression or psychosis, or social disadvantages (such as poor academic achievement or unemployment) that might result from cannabis use. Reference Fergusson and Boden5 However, many factors associated with cannabis use (such as male gender, alcohol and other drug use, and antisocial behaviour) are also associated with suicide, and may therefore confound the relationship between cannabis and suicide.
In a longitudinal study of the relationship between cannabis and mortality in a Swedish conscript cohort there was an increased risk of suicide – and of overall mortality – in those who were heavy users of cannabis. Reference Andreasson and Allebeck6 Although the association with overall mortality was eliminated in the multivariable analysis, the authors did not investigate suicide deaths in more detail and examine effects of cannabis on this outcome independent of confounding. In this study we re-examined the same cohort, with an extended follow-up period to identify more suicides, and investigated the association between cannabis use and subsequent risk of completed suicide, both before and after adjustment for a range of potential confounders.
Method
Study population
The data used in this study were derived from a longitudinal study of 50 087 men who were conscripted during one year (1969–70) for compulsory military training in Sweden. Over 98% of the men were aged 18–20 years at the time of conscription. At that time, only 2–3% of men were exempt from conscription, usually because of severe disability or illness. All of the men completed two non-anonymous, self-report questionnaires at the time of conscription. The first concerned social background, upbringing conditions, friendships, relationships, attitudes, and adjustment at school and work. The other concerned the use of alcohol, tobacco and other drugs. Each man had a structured interview with a trained psychologist, who then assessed him on a series of psychological measures on the basis of data from the questionnaire and the interview. The conscripts were also given an IQ test. The psychologists' ratings were regularly checked for interrater reliability. Whenever a psychiatric disorder was reported by the conscript or suspected by the interviewing psychologist, the conscript was referred to a psychiatrist. Psychiatric diagnoses were coded according to the Swedish version of the ICD–8. Permission to use the data for research purposes was granted by the research ethics committee of the Karolinska Institute.
Measures
Exposure
Information on cannabis and other drug use was obtained from the questionnaires at the time of conscription. These questions assessed which drugs had ever been used, the number of occasions of drug use, which drugs were used most frequently, and the age at first drug use. Frequency of cannabis use was calculated for those who had selected cannabis as the drug they most often used, and coded as ‘never’ (in 1969–70), ‘1–10 times’, ‘11–50 times’ and ‘more than 50 times’. Data on age at first use of cannabis were only available for participants for whom cannabis was the first illicit drug they had used.
Outcome
Suicide and undetermined deaths in the cohort were identified by linkage with the National Cause of Death Register up to the year 2003. The register records all deaths among people registered in Sweden and is more than 99% complete. The causes of death for all people domiciled in Sweden are coded and recorded at Statistics Sweden from information on their death certificates. Cause of death was coded according to the Swedish versions of the ICD–8 (ICD–9 from 1987, ICD–10 from 1997). The ICD codes for suicide were E950–959 (ICD–8 and ICD–9) and X60–X84 (ICD–10); codes for undetermined causes of death were E980–989 (ICD–8 and ICD–9) and Y10–Y34 (ICD–10). 7–9
Confounders
Sociodemographic and individual factors associated with both an increased risk of suicide and increased cannabis use include family history of psychiatric disorder, socioeconomic position, social isolation, alcohol use and presence of psychiatric and personality disorders. Reference Dorard, Berthoz, Phan, Corcos and Bungener10–Reference Morgan and Williams13 We selected relevant variables from the psychological assessments and questionnaires to control for confounding. These included age, family economic status, parental occupation, parental use of psychotropic medication, psychiatric diagnosis at the time of conscription, IQ score (nine categories), tobacco use, alcohol and other drug use, problem behaviour during childhood (composite score from questions regarding truancy, contact with police or child-care authorities and running away from home), psychological adjustment (composite score from questions regarding sensitivity, feeling nervous, feeling low, feeling angry and taking psychotropic medication) and social relations (composite score from questions regarding the number of personal friends, presence of a girlfriend and feelings of insecurity with others).
Intermediate pathway variables
As the development of mental health disorders such as psychosis might have been an intermediate pathway in the development of suicidal outcome, we examined to what extent any association between cannabis and suicide was explained by development of psychiatric disorder during the follow-up period. Participants admitted to psychiatric care during the follow-up period were identified through linkage with the National Hospital Discharge Register. The linkage reported here was from 1970 to 2004. Individuals were given a clinical diagnosis according to ICD–8 (ICD–9 from 1987, ICD–10 from 1997). Furthermore, as the temporal relationships between cannabis use and other substance use as well as between cannabis use and psychiatric diagnosis at conscription could not be determined, given that these were all measured at the same time, it is possible that these variables could act either as confounders or as intermediate variables in the relationship between cannabis use and suicide.
Statistical analysis
We used Stata version 10 for Windows to perform logistic regression to calculate odds ratios and 95% confidence intervals for the outcome of suicide, in men who used cannabis compared with men with no history of cannabis use, both before and after adjustment for potential confounders. We also examined suicide in relation to frequency of cannabis use, and examined this relationship separately for suicides occurring within the first 15 years as opposed to the subsequent 18 years of follow-up.
We examined the impact of each individual confounder on the relationship between cannabis use and suicide. Crude and individually adjusted results of association between cannabis use and suicide were computed for each potential confounder, and the variables with the strongest effects were included in the final regression model. We adopted the strategy of first examining the outcomes of suicide and undetermined deaths (possible suicide) separately to assess heterogeneity, and if results were consistent across these outcomes, combining these outcomes in order to maximise statistical power. As a sensitivity analysis we also present results for completed suicides only. We also compared the outcome of suicide or possible suicide in those who had first used cannabis at age 16 years or earlier, v. those who had first used cannabis at age 17 years or later.
Results
Among all 50 087cohort members there were 459 (0.9%) definite suicides and 141 (0.3%) deaths due to undetermined causes (‘undetermined deaths’) during the 33 years of follow-up. About a tenth of the whole cohort (10.7%, n = 5380) had used cannabis v. 41 394 (82.6%) who had not; 3313 (6.6%) participants failed to report whether or not they had tried cannabis. Of the 5391 men who had used cannabis, data on frequency of use were missing for 1127 (20.9%).
Selection of confounders
Occurrence of cannabis use was more frequent in those with higher IQ scores, those who used more alcohol, tobacco and other drugs, those who reported more problematic behaviour during childhood, those with lower levels of psychological adjustment, and those with a psychiatric diagnosis at conscription (Table 1). Adjusting for age, parental occupation and family economic status had no effect on the association between cannabis use and suicide and these factors were excluded from the multivariable model. In total 8441 (16.8% of the cohort) had missing data for cannabis use or for at least one of the nine confounding variables included in the final adjusted model. The frequency of cannabis use and suicide were higher in the group excluded because of missing data (13.4% and 1.5% respectively) compared with the 41 646 participants included in the final adjusted analysis (11.1% and 1.1% respectively).
Table 1 Participants exposed to each confounding variable, stratified by cannabis use, and odds ratios for suicide or possible suicide in relation to ever use of cannabis after individual adjustment for each confounder
| Participants exposed to confoundera | Odds ratio for suicideb | |||
|---|---|---|---|---|
| Confounder | Used cannabis n (%) | Never used n (%) | Crude OR (95% CI) | Individually adjusted OR (95% CI) |
| Lowest IQ group | 103 (1.9) | 1744 (4.2) | 1.69 (1.36-2.11) | 1.82 (1.46-2.27) |
| Alcohol consumption >250 g/week | 723 (13.4) | 1049 (2.6) | 1.68 (1.34-2.09) | 1.38 (1.09-1.74) |
| Both parents taken psychotropic medication | 304 (5.6) | 1261 (3.0) | 1.65 (1.31, 2.06) | 1.54 (1.22-1.93) |
| Smoke >20/day | 502 (9.4) | 1187 (2.9) | 1.69 (1.35-2.10) | 1.39 (1.10-1.75) |
| Used other drugs | 1756 (32.6) | 1005 (2.4) | 1.71 (1.38-2.12) | 1.34 (1.04-1.72) |
| Psychiatric diagnosis at conscriptionc | 1112 (21.2) | 3579 (8.7) | 1.74 (1.40-2.17) | 1.49 (1.19-1.87) |
| High problematic behaviour scored | 3020 (58.9) | 9408 (23.6) | 1.75 (1.40-2.18) | 1.17 (0.92-1.50) |
| Poor psychological adjustmentd | 2409 (46.2) | 11209 (27.3) | 1.70 (1.36-2.12) | 1.36 (1.08-1.71) |
| Poor social relationsd | 1378 (26.3) | 12249 (29.8) | 1.71 (1.37-2.13) | 1.71 (1.37-2.14) |
Use of cannabis
The crude and adjusted odds ratios with 95% confidence intervals for outcome of any suicide (suicide and undetermined deaths) given a history of ever having used cannabis are presented in Table 2. Although the odds of suicide were greater in those who had used cannabis compared with those who had never used the drug, this association did not persist after adjustment.
Table 2 Crude and adjusted odds ratios for suicide or possible suicide in relation to cannabis and other drug use
| Participants n | Cases n (%) | OR (95% CI) | ||
|---|---|---|---|---|
| Crude | Adjusteda | |||
| Cannabis use | ||||
| None | 37 016 | 396 (1.1) | 1 | 1 |
| Ever use | 4 630 | 80 (1.7) | 1.63 (1.28-2.07) P < 0.001 | 0.88 (0.65-1.20) P = 0.430 |
| Frequency of cannabis useb | ||||
| None | 37 016 | 396 (1.1) | 1 | 1 |
| 1-10 times | 2 501 | 36 (1.4) | 1.35 (0.95-1.90) | 0.89 (0.61-1.29) |
| 11-50 times | 588 | 8 (1.4) | 1.27 (0.63-2.57) | 0.55 (0.26-1.20) |
| >50 times | 583 | 21 (3.6) | 3.45 (2.21-5.39) | 1.04 (0.57-1.91) |
| LRT for frequency of use | 40 166 | 461 (1.1) | χ2 = 23.4, d.f. = 3 P < 0.001 | χ2 = 2.7, d.f. = 3 P = 0.440 |
| Other drug use | ||||
| None | 39 340 | 420 (1.1) | 1 | 1 |
| Ever use | 2 306 | 56 (2.4) | 2.31 (1.74-3.06) P < 0.001 | 1.40 (0.99-1.99) P = 0.060 |
| Frequency of other drug use | ||||
| None | 39 340 | 420 (1.1) | 1 | 1 |
| 1-10 times | 346 | 12 (3.5) | 3.33 (1.86-5.97) | 2.36 (1.30-4.31) |
| 11-50 times | 174 | 3 (1.7) | 1.63 (0.52-5.11) | 1.06 (0.33-3.42) |
| >50 times | 146 | 7 (4.8) | 4.67 (2.17-10.03) | 1.79 (0.78-4.10) |
| LRT for frequency of use | 40 006 | 442 (1.1) | χ2 = 22.3, d.f. = 3 P < 0.001 | χ2 = 7.6, d.f. = 3 P = 0.054 |
Frequency of cannabis use
The odds ratio for a linear trend of increasing frequency of use was 1.42 (95% CI 1.24–1.63, P<0.001) in the crude analysis and 1.00 (95% CI 0.83–1.20, P = 0.961) after adjustment. However, the relationship between frequency of cannabis use and suicide was not very consistent with a dose–response effect (Table 2). Suicide was more common primarily in those who had used cannabis more than 50 times, although this association was eliminated after adjustment for confounders. There was also no association between frequency of cannabis use and suicide after adjustment if we examined suicide outcome during years 1–15 and years 16–33 of follow-up separately (online Table DS1).
When individually adjusting for each confounder, the variables with the strongest confounding effects were problematic behaviour during childhood, other drug use, psychological adjustment, alcohol consumption, tobacco use and psychiatric diagnosis at conscription.
Age at first use of cannabis
We compared the risk of suicide in those who first used cannabis at age 16 years or earlier with those who first used cannabis after age 16 years. The two groups did not differ substantially when risk of suicide or undetermined death was studied in relation to frequency of cannabis use (online Table DS2), with adjusted odds ratios for a linear trend across categories of cannabis use frequency of 1.03 (95% CI 0.83–1.29) in those who first used cannabis at age 16 years or earlier, v. 0.86 (95% CI 0.65–1.13) in those who first used cannabis at age 17 years or later.
Other drug use
Use of drugs other than cannabis was reported by 2761 participants. Of these, the majority had used stimulants (52.6%), with a smaller proportion having used opiates (20.4%) or one of a number of other non-prescribed substances (37.2%). The odds of suicide were increased in participants who had ever used drugs other than cannabis (adjusted OR = 1.40, 95% CI 0.99–1.99, P = 0.060), although there was little evidence to support a dose–response effect for frequency of use (Table 2). There were insufficient numbers of individuals who used drugs other than cannabis to allow us to examine the effects of specific drug classes separately.
Definite suicides only
The results for cannabis use were more or less identical when we examined only cases of definite suicide and excluded undetermined deaths, although estimates were slightly less precise. For example, the adjusted odds ratio for definite suicide given a history of ever using cannabis was 0.90 (95% CI 0.63–1.29). For use of drugs other than cannabis there was stronger evidence of an association with undetermined deaths (adjusted OR = 2.06, 95% CI 1.11–3.80) than with definite suicide (adjusted OR = 1.13, 95% CI 0.73–1.75).
Intermediate pathways
As it was possible that psychiatric diagnosis at conscription or other drug use at conscription mediated rather than confounded the relationship between cannabis use and suicide, we repeated the analyses while omitting these variables from the adjusted model. However, even in this analysis there was no evidence of any association between frequency of cannabis use and suicide or possible suicide (adjusted odds ratio for trend 1.07, 95% CI 0.92–1.25). There was no rationale for further adjusting for psychiatric diagnosis post-conscription as an intermediate or mediating variable as we did not find any association between cannabis use and suicide.
Discussion
In this study cohort cannabis use was associated with an increased risk of suicide in the crude analysis. This association was seen primarily in men using cannabis most frequently, and results were not consistent with a dose–response effect. The relationship between cannabis use and suicide was eliminated after controlling for social and personal factors. Results were similar whether we examined only definite suicides or also included undetermined deaths as our outcome. There was some evidence that use of drugs other than cannabis was associated with an increased risk of suicide and undetermined death. However, we were unable to differentiate specific effects of drugs such as opiates, which are most strongly associated with suicide, Reference Wilcox, Conner and Caine3 from effects of other drugs such as hallucinogens or sedatives, where associations with suicide are likely to be much weaker.
There are a number of explanations that we considered as possible reasons for finding no evidence of association between cannabis and suicide in our study. First, if some of the variables controlled for in this study were intermediate pathway variables between cannabis use and suicide, then it would have been inappropriate to control for them as this would lead to an incorrect interpretation that cannabis use was not causally related to suicide; for example, part of the relationship between cannabis and suicide was explained by other drug use. Although this is consistent with other drug use being a confounding factor (i.e. it was the other drugs that led to an increased risk of suicide), an alternative explanation is that cannabis use led to other drug use, and that this then led to an increased risk of suicide (i.e. the data could be considered consistent with the much debated ‘stepping stone’ hypothesis). Reference Kandel and Logan14,Reference Hall and Lynskey15 Similarly, psychiatric diagnosis at the time of conscription could also be an intermediate pathway variable. Studies examining cannabis use and mental health outcomes indicate that there may be a causal association between cannabis use and psychotic disorders, and possibly also mood disorders. Reference Hall and Degenhardt1,Reference Moore, Zammit, Lingford-Hughes, Barnes, Jones and Burke2 Considering that suicide rates are much higher in those with psychiatric illness, especially psychotic illness, it is plausible that some suicides in this cohort were caused by cannabis use indirectly, with psychiatric illness at conscription lying on the causal pathway. If this were the case, then adjusting for psychiatric diagnosis at the time of conscription in this cohort would be inappropriate. However, excluding both psychiatric diagnosis at conscription and other drug use from the analysis did not affect our results.
Second, although it is possible that bias might have led to an underestimate of association, it seems unlikely that bias would have occurred to an extent that would have obscured any association between cannabis and suicide. Misreporting of cannabis use is certain to have occurred to some extent. For example, the questionnaires used to assess cannabis use were not anonymous, and some participants might have been wary about giving information regarding illegal substances. Indeed, people who consume large quantities of cannabis have been found to give higher estimates of consumption when giving data anonymously, Reference Angst, Baumann, Muller and Ruppen16 and fewer participants in this cohort claimed to have used cannabis and other illicit drugs compared with similar Swedish conscript cohorts that used anonymous questionnaires. Reference Andreasson and Allebeck17 If misreporting was similar for the whole cohort and not affected by future risk of suicide, the effect of such non-differential misclassification would lead to an underestimate of effect size. This may be present in our study but it seems unlikely that this would explain the lack of any association observed in the adjusted analysis. It is also possible that individuals who subsequently completed suicide might have been more likely to underreport their cannabis use (for example, if they were more reclusive and isolated) or, conversely, more likely to report their use honestly (for example, if they were more impulsive and less inhibited). It is not possible to gauge to what extent, if at all, either of these scenarios might have led to our under- or overestimating the relationship between cannabis use and suicide in this study. Sample bias and attrition bias are also unlikely to explain our findings as this cohort included over 97% of all men aged 18–20 years in Sweden at the time, and only a negligible proportion (those who had emigrated) were lost to follow-up.
Another potential reason why we may have failed to find an association between cannabis use and suicide is lack of statistical power. However, this study had 90% power to find an odds ratio of 1.5 and 99% power to find an odds ratio of 1.7 or higher, sufficient to detect an effect size of the magnitude reported in most previous studies that have examined the relationship between cannabis and suicidal ideation or attempts. Furthermore, if cannabis were truly a causal factor for suicide, then we might expect a stronger association for completed suicides than for suicidal ideation or attempts. The upper limits of the confidence intervals in our study allow us to exclude a large or even moderate effect of cannabis use on risk of suicide.
Unmeasured confounding factors, leading to increased cannabis use and decreased risk of suicide (for example, in this study those with higher IQ scores were more likely to use cannabis and less likely to complete suicide), might have contributed to an underestimation of the association. However, given that almost all confounders in our study attenuated the association between cannabis and suicide, it seems unlikely that such residual confounding could explain our failure to find an association.
The most likely explanation for our results is that the apparent association between cannabis and suicide was in fact explained by confounding, and that there is perhaps little or no causal relationship between cannabis and suicide. Adjusting for an almost identical set of confounders in a previous study within this cohort reduced the estimate of association between cannabis use and schizophrenia, Reference Zammit, Allebeck, Andreasson, Lundberg and Lewis18 but did not eliminate that association in the way that we observe for suicide. Comparing the patterns of association between cannabis use and suicide with those for cannabis use and schizophrenia in this cohort (Fig. 1) suggests that bias or inappropriate adjustment for mediators is unlikely to explain the results from this study, and lends support to the argument that cannabis is a risk factor for schizophrenia, Reference Moore, Zammit, Lingford-Hughes, Barnes, Jones and Burke2 but not for suicide.
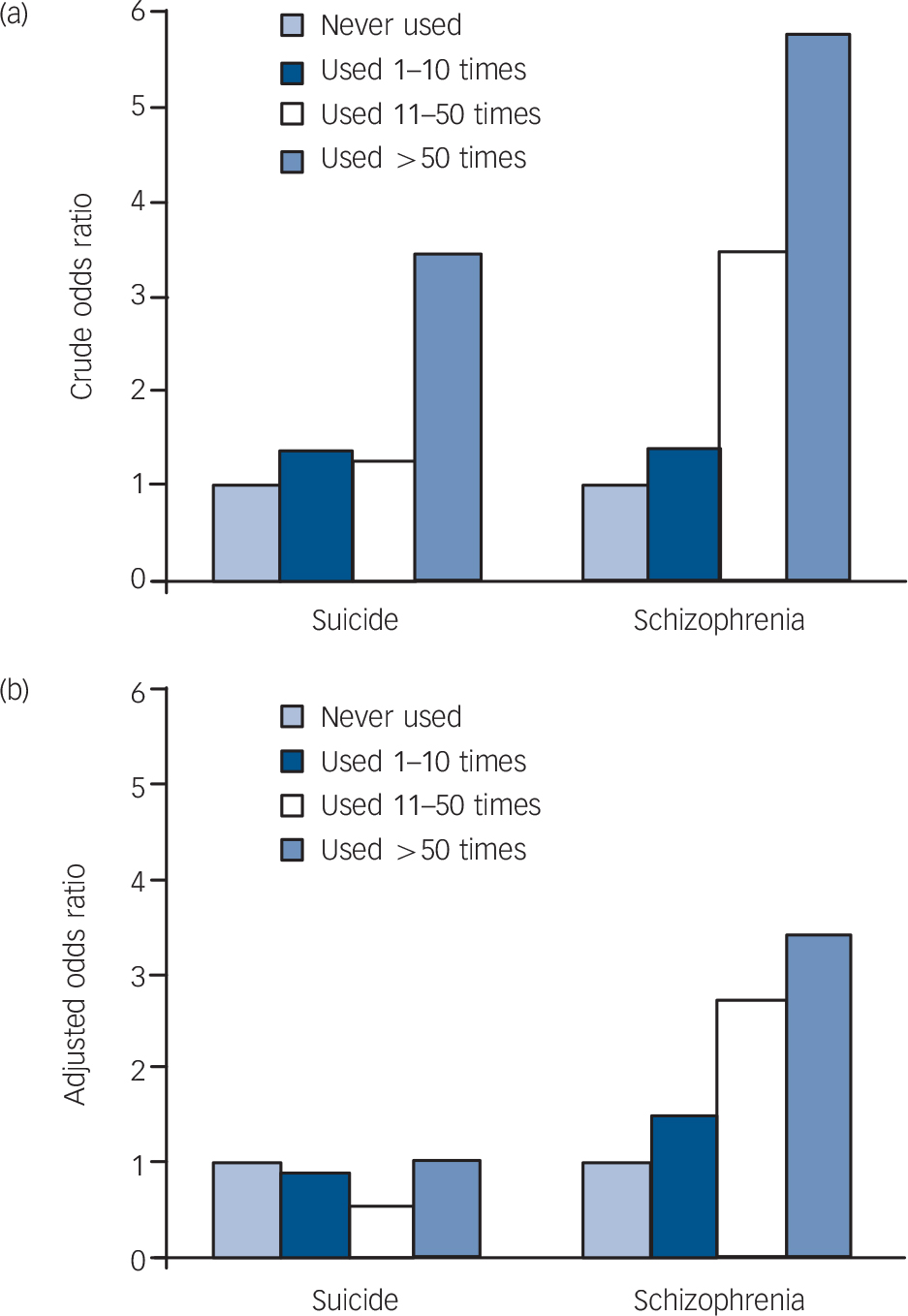
Fig. 1 Crude (a) and adjusted (b) odds ratios for suicide and schizophrenia in relation to frequency of cannabis use.
If cannabis really increases the risk of psychosis we would expect to observe an association between cannabis and suicide given that psychosis is an established risk factor for suicide. However, if cannabis is associated with suicide only through its effect on risk of psychosis, it is likely that statistical power to detect this in our study would be low given that few suicides result from psychosis. In this cohort, for example, only 37 of 600 men who completed suicide (6.2%) had been previously admitted to hospital with schizophrenia during follow-up.
Strengths and limitations
As far as we are aware this is the largest study to date that has examined the relationship between cannabis and suicide. One of the strengths of our study is that we have been able to control for numerous psychosocial and individual factors, which is rare in a cohort of this size. Furthermore, the sample is representative of the Swedish young male population of that time. We were able to identify suicides and deaths from undetermined causes between the ages of 18 and 52 years, and given that the majority of male suicides occur by this age, 19,20 these results are applicable to the population age group in which suicide is a major concern. However, this cohort was not set up to examine risk factors for suicide, and there is no information on suicide attempts, suicidal ideation, family history of suicide or detailed information on mood and personality throughout the life-course that might have allowed a more detailed examination of the association between cannabis use and subsequent risk of suicide. This study could also have benefited from more detailed information on frequency of cannabis use, because the category of heaviest use in this study (used more than 50 times) does not allow us to distinguish between people who used cannabis once a week for a year, and those using cannabis many times each day or those dependent on the drug, who are most likely to be at risk of adverse outcomes relating to its use. Unfortunately cohorts that have such detailed information and that are large enough to study rare outcomes such as suicide do not currently exist. Furthermore, although the large increase in frequency of cannabis use that has occurred since 1969 should not affect the interpretation of our results, the average concentration of delta-9-tetrahydrocannabinol has also changed since then, and the effect of these more potent forms of cannabis on suicide is not known.
Comparison with other studies
Few longitudinal studies examining suicide exist, as it is such a rare outcome, and most previous studies have addressed suicidal behaviours such as suicidal ideation or suicide attempt rather than completed suicides. Some previous studies have found an association between cannabis and suicidal behaviour, even after controlling for some of the characteristics adjusted for in our study. Reference Fergusson, Horwood and Swain-Campbell11,Reference Borowsky, Ireland and Resnick21–Reference Lynskey, Glowinski, Todorov, Bucholz, Madden and Nelson25 The longitudinal design and long duration of follow-up in our study meant that we were able to control for many variables reflecting life circumstances and mental health in childhood and early adolescence. The studies by Wilcox & Anthony and by Beautrais et al, for example, were able – much like us – to control for a more comprehensive set of confounding variables, Reference Wilcox and Anthony23,Reference Beautrais, Joyce and Mulder26 and the risk of suicidal behaviours in relation to cannabis use reported in these studies is more modest than in studies that have not been able to control so well for markers of adversity during childhood and adolescence.
Some studies have also found evidence of age-related variation in the strength of the association between cannabis use and suicidal behaviours, with younger users being more affected, Reference Fergusson, Horwood and Swain-Campbell11,Reference Wilcox and Anthony23 although we found no evidence of such an age-dependent effect.
Although suicidal ideation and suicide attempt are likely to differ from completed suicide in their aetiology, nevertheless our findings highlight the concern that many studies of suicidal behaviour have not adequately adjusted for confounding, and that at least part of the observed associations between cannabis use and suicidal attempts or ideation may be due to alternative, non-causal explanations. Reference Moore, Zammit, Lingford-Hughes, Barnes, Jones and Burke2
Implications of the study
There exists little epidemiological research regarding the health effects of long-term cannabis use. In this cohort there was no evidence of association between cannabis use and risk of suicide after controlling for confounding social and personal factors, indicating that cannabis use is unlikely to be an important risk factor for suicide, either directly or as a consequence of mental health problems secondary to its use.
Funding
S.Z. is funded through a Clinician Scientist Award funded by the National Assembly for Wales.






eLetters
No eLetters have been published for this article.