Late-life depression
With the current trends of ageing in the worldwide population, health problems associated with ageing have become an issue. Depression among the elderly populations has become an important public health problem which is associated with increased morbidity and risk of suicide; decreased physical, cognitive and social functioning; and self-neglect.Reference Fiske, Wetherell and Gatz1,Reference Blazer2 A previous study has shown that, compared with older people without depression, the total ambulatory costs are 43–52% higher and total ambulatory and in-patient costs were 47–51% higher in older people with depression.Reference Katon, Lin, Russo and Unutzer3 The severity of depression among older adults is associated with poor quality of life.Reference Sivertsen, Bjorklof, Engedal, Selbaek and Helvik4 However, depression is largely undetected and untreated among community-dwelling older adults in primary care,Reference Klap, Unroe and Unutzer5 which suggests a particularly great burden of late-life depression in the community. Previous studies have shown that the prevalence of clinically significant depressive symptoms among community-dwelling older adults range from approximately 8 to 16%.Reference Blazer6
Late-life depression is considered a geriatric syndrome with multiple aetiologies.Reference Kennedy7 Compared with depression in younger adults, late-life depression is associated with a higher prevalence of somatic depressive symptoms (e.g. fatigue)Reference Fiske, Wetherell and Gatz1 which may reflect poor physical condition. In particular, the proposed ‘vascular depression hypothesis’ states that vascular disease may predispose, precipitate or perpetuate depressive syndromes among older adults.Reference Alexopoulos, Bruce, Silbersweig, Kalayam and Stern8 This is supported by the evidence that vascular disease and its risk factors are associated with lesions in white matter, which is an established risk factor for late-life depression.Reference Glassman9 These factors could contribute to a poor prognosis, even death, which includes all-cause and cardiovascular mortality. A number of studies have examined the associations between late-life depression and risk of mortality, but they used a variety of definitions for late-life depression and populations that were heterogeneous in terms of region, age and gender.
Late-life depression and mortality
A previous systematic review in 2001 demonstrated that diagnosed depression in community-resident older people is associated with increased mortality, with an odds ratio of 1.73 (95% CI 1.53, 1.95).Reference Saz and Dewey10 However, the literature is now far more up to date after almost 20 years. We therefore aimed to conduct an updated systematic review and meta-analysis to summarise the existing evidence of the association between late-life depression and all-cause mortality in older adults living in the community. We hypothesised that late-life depression is associated with higher risk of both all-cause and cardiovascular mortality, and therefore also conducted a meta-analysis of late-life depression with all-cause and cardiovascular mortality in community-dwelling older adults.
Method
Literature selection
We followed MOOSE (Meta-analysis Of Observational Studies in Epidemiology) guidelines to conduct our systematic review and meta-analysis.Reference Stroup, Berlin, Morton, Olkin, Williamson and Rennie11 We included original studies with full text that were: (a) published in peer-reviewed journals from January 1966 to February 2018; (b) used prospective cohort studies; (c) included community-dwelling participants ≥60 years; (d) ascertained depression according to a physician diagnosis, use of antidepressant or based on a specified cut-off of a standardised depressive symptoms scale; (e) examined all-cause and/or cardiovascular mortality; and (f) followed participants for at least 1 year. We excluded studies with participants identified in clinical settings or with specific comorbidities, studies that assessed depression together with other mental disorders and studies that only reported depressive symptoms as a continuous variable without a clinical cut-off point. If there were multiple studies based on the same cohort, we retained the study with longest follow-up duration for the main analysis and the other studies may be used for subgroup/sensitivity analysis.
We systematically searched PubMed, Embase, Web of Science and PsycINFO for prospective cohort studies on the association of late-life depression with all-cause and cardiovascular mortality. Search terms included ‘depression’, ‘depressive’, ‘mortality’, ‘death’, ‘survival’ and ‘late life’ (Supplementary Appendix available at https://doi.org/10.1192/bjp.2019.74). The electronic search was supplemented by examination of secondary references of previously published original articles and review papers. The search was limited to articles written in English.
Study selection was conducted in two steps. First, titles and abstracts of studies identified in the literature search were independently reviewed by three investigators (J.W., R.H. and X.Z.). Second, the full texts of studies that remained after the first step were reviewed by the same three investigators and disagreements were again reconciled (J.W., R.H. and X.Z.). Data from studies that met inclusion criteria were then extracted and tabulated by the same three investigators and disagreements were reconciled. Information obtained from each study included effect size and the corresponding measure of statistical dispersion, e.g. a 95% confidence interval, region, sample size, age of participants, percentage females, follow-up length, assessment of depression, effect sizes and covariates included in the analysis.
Quality assessment of individual studies
Each study included in the review underwent a formal quality assessment using the Newcastle–Ottawa Scale.Reference Wells, Shea, O'Connell, Peterson, Welch and Losos12 The Newcastle–Ottawa Scale evaluates quality of cohort studies in three domains: selection of exposed and non-exposed cohorts (representativeness of the exposed cohort, selection of the non-exposed cohort, ascertainment of exposure and demonstration of absence of outcome at the beginning of studies), comparability of exposed and non-exposed cohorts (analysis appropriately adjusted for potential confounding factors, such as medications, history of other chronic diseases and lifestyle factors) and outcome ascertainment (adequacy of outcome assessment, length of follow-up and adequacy of follow-up). A study was awarded a maximum of one point for each variable within each assessment domain (selection, comparability and outcome) for a possible maximum total score of nine. The quality assessment was conducted independently by three reviewers (J.W., R.H. and X.Z.) and the results were reconciled by a consensus.
Statistical analysis
Risk ratios or similar estimates were obtained along with 95% confidence intervals for each eligible study. If available, the results of fully adjusted models were used. If effect sizes were not reported, risk ratios were calculated using the data reported in the articles. Other effect measures (odds ratios, incidence rate ratios, hazards ratios) were considered equivalent to risk ratios.Reference Symons and Moore13 The pooled risk ratios across studies were calculated using generic inverse variance weighting in random-effects meta-analysis models.Reference DerSimonian and Laird14,Reference Reeves, Deeks, Higgins, Wells, Higgins and Green15 We considered a pooled risk ratio to be statistically significant if its 95% confidence interval did not contain one. Heterogeneity among studies was assessed with χ2-test and the I 2 statistic, with a significant heterogeneity defined as I 2 > 50%. Forest plots were created to illustrate individual and pooled risk estimates. Subgroup analyses were conducted according to study characteristics, including regions of studies (USA, Europe, Asia, Australia), mean age of participants (≥75 years or not), percentage of female participants (≥50% or not), assessment of depression (measured with standardised scales/physician diagnosis or use of antidepressants) and time of study published (before or after 2001). Funnel plots were created to examine potential publication bias. If evidence of publication bias existed, a sensitivity analysis was conducted after excluding all outlying studies in a ‘trim-and-fill’ manner, which uses simple rank-based data augmentation techniques to estimate the number of studies missing from a meta-analysis due to the suppression of the most extreme results on one side of the funnel plot.Reference Duval and Tweedie16 Sensitivity analysis was conducted on studies that scored eight or above for quality assessment, as well as on those that examined the associations between late-onset depression with all-cause mortality and cardiovascular mortality. All analyses were conducted using Stata 14 for Windows (Stata Corp, College Station, USA).
Results
Qualitative analysis
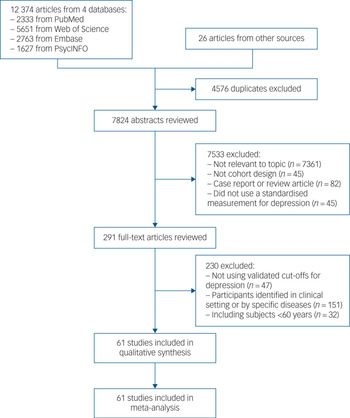
The database search yielded 12 374 citations (Fig. 1). An additional 26 studies were identified from the bibliography of relevant reports and reviews. After eliminating duplicates, 7824 publications remained. Of these, 7533 papers were excluded because they described studies that were irrelevant, did not use prospective cohort design or they focused on participants younger than 60 years. The 291 remaining reports were retrieved and examined in detail. Of these, 230 were ultimately excluded for not meeting other inclusion criteria. A total of 61 publications presenting data on 53 separate cohorts met the eligibility criteria and were included in the systematic review and meta-analysis.

Fig. 1 Flow chart showing the selection of study reports for the meta-analysis.
Among the 53 cohorts, there were 17 from the USA, 21 from Europe (France, Finland, Greece, Italy, Netherlands, UK, Sweden, Norway, Spain and Germany), 8 from Asia (China [Hong Kong, Taiwan], Japan, South Korea and Singapore), 5 from Australia, 1 from Brazil and 1 from Canada. The pooled sample included 198 589 participants with range of 281–62 839 per study. The main characteristics of the studies included in the meta-analysis are summarised in Supplemental Table 1. The minimum age of included participants ranged from 60 to 85 years. The proportion of women ranged from 0 to 100%. The follow-up period ranged from 4 to 15 years. The prevalence of depression ranged from 2.7 to 54.6%, although three studies reported no prevalence estimates.
Ten studies relied on the DSM-III (1980) or DSM-IV (1994) criteria, four studies used Automated Geriatric Examination for Computer Assisted Taxonomy (AGECAT) and one study used Geriatric Mental State Examination. A total of 38 studies employed standardised scales for depressive symptoms, including Center for Epidemiologic Studies Depression Scale (CES-D) of 8, 10 and 20 items; Zung Self-Rating Depression Scale and the 15- or 30-item Geriatric Depression Scale (GDS). As shown in Supplemental Table 1, the cut-offs for defining depression differed across scale-based studies. In the 53 included cohorts, 49 reported all-cause mortality and 15 reported cardiovascular mortality. All-cause mortality in the included studies was defined in at least one of the following sources: medical records, registry records, death certificate, obituaries and interview with relatives. Mortality from cardiovascular disease was ascertained from medical records, death certificates, ICD codes, obituaries or interviews with relatives and contacts. Time-to-event analysis was applied in 19 out of the 53 cohorts.
Quantitative analysis
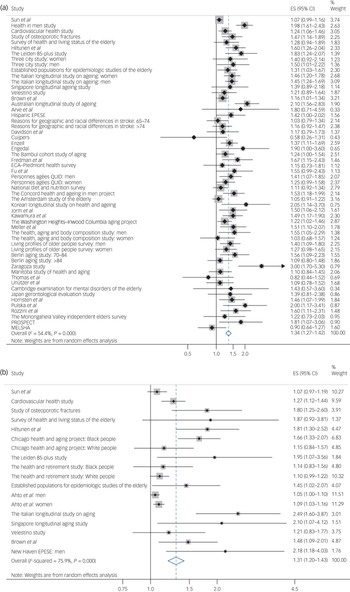
The meta-analysis of the 49 cohort studies indicated that there was a significantly higher risk of all-cause mortality among older adults with depression (risk ratio 1.34; 95% CI 1.27, 1.42; Fig. 2a) compared with people of the same age but without evidence of depression. The corresponding meta-analysis of 15 studies reporting cardiovascular mortality produced a similar result (risk ratio 1.31; 95% CI 1.20, 1.43; Fig. 2b). There was significant heterogeneity across studies with I 2 estimates of 54.4% for all-cause mortality analyses and 75.9% for analyses of cardiovascular mortality.

Fig. 2 Pooled association between late-life depression and risk of (a) all-cause mortality and (b) cardiovascular mortality.
Late-life depression is associated with all-cause mortality among different subgroups. Among the different regions, the pooled risk ratio was largest in Australia and smallest in North America. Furthermore, the pooled risk ratio is larger among studies with an average age ≥75 years, studies with at least 50% male participants, studies assessing depression with physician diagnosis and studies published before 2001; however the results were similar for studies with follow-up time <5 years and those with follow-up time ≥5 years. Heterogeneity across studies was observed in studies conducted in Asia and Australia, studies with mean age ≥75 years, studies with majority of either male or female, studies with follow-up period ≥5 years, studies that assessed depression using a standardised scale (particularly those using GDS) and studies published after 2001. For late-life depression and cardiovascular mortality, the associations were significant among studies in North America and Europe, but not in Asia, and the pooled risk ratio was larger for studies in Europe. Risk ratio was statistically significant among studies that were majority female but not among those that were majority male. Risk ratios were larger among studies with an average age ≥75 years, studies with follow-up time <5 years, studies assessing depression with physician diagnosis and studies published before 2001. Heterogeneity across studies was observed in studies conducted in North America, Europe and Asia; studies with mean age ≥75 years and <75 years; studies with a majority of either male or female; studies with follow-up period ≥5 years; studies that assessed depression using standardised scales and studies published after 2001 (Table 1).
Table 1 Subgroup meta-analysis of the associations between late-life depression and risk of all-cause mortality and cardiovascular mortality (pooled risk ratios and 95% confidence intervals)

Bold terms indicate 95% CIs that do not include 1, and P-values for I 2 < 0.05. AGECAT, Automated Geriatric Examination for Computer Assisted Taxonomy.
a. Eleven cohorts reported late-life depression and all-cause mortality by gender; two cohorts reported late-life depression and cardiovascular mortality by gender.
b. Three cohorts used both physician diagnosis and standardised scales for assessment of depression.
The funnel plots suggested that the results from some cohorts appeared asymmetric for the associations of late-life depression with all-cause mortality (Supplemental Figure 1A) and cardiovascular mortality (Supplemental Figure 1B). After excluding cohorts outside the range, the trim-and-fill analysis showed significant pooled association of late-life depression with all-cause mortality (risk ratio 1.22; 95% CI 1.15, 1.30) and cardiovascular mortality (risk ratio 1.11; 95% CI 1.01, 1.22).
The quality of the methodology of the 62 studies included in the meta-analysis, as scored with the Newcastle–Ottawa Scale, is presented in Supplemental Table 2. The average total score was 7.2 out of a maximum score of 9 (range 5–9), indicating that the quality was good overall. The sensitivity analysis based on studies with a total score of eight or above showed consistent associations between late-life depression and all-cause mortality (risk ratio 1.44; 95% CI 1.30, 1.60) and cardiovascular mortality (risk ratio 1.42; 95% CI 1.16, 1.75), and heterogeneity across studies was present for both outcomes (Table 2).
Table 2 Sensitivity meta-analysis of the associations between late-life depression and risk of all-cause mortality and cardiovascular mortality (pooled risk ratios and 95% confidence intervals)

Bold terms indicate 95% CIs that do not include 1, and P-values for I 2 < 0.05.
In addition, sensitivity analysis indicated that late-onset depression was associated with both all-cause (risk ratio 1.51; 95% CI 1.15, 1.97) and cardiovascular mortality (risk ratio 1.40; 95% CI 1.01, 1.94) among studies that specifically identified late-onset depression (Table 2).
Discussion
The present systematic review and meta-analysis of prospective cohort studies suggests that late-life depression is associated with 34 and 31% higher risk of all-cause mortality and cardiovascular mortality, respectively; although the observed associations in our study were subject to considerable heterogeneity across studies.
Only one previous systematic review published in 2001 summarised the association between late-life depression and all-cause mortality among community-dwelling old adults.Reference Saz and Dewey10 Similar to our study, the systematic review included studies with participants ≥60 years of age from community samples. However, the systematic review also included studies measuring specific depressive symptoms, in addition to overall depressive symptoms measured using scales and diagnostic methods. Our results are consistent with this previous systematic review: diagnosed depression in community-resident older people is associated with increased all-cause mortality and longer follow-up predicted smaller effect sizes. However, this systematic review only quantified the associations based on clinically diagnosed depression, and the definition of depression in the systematic review did not include cut-off points based on established depression scales. In addition, many studies on the associations between late-life depression and all-cause and cardiovascular mortality were published after 2001. To the best of our knowledge, our systematic review and meta-analysis is the latest and most comprehensive study to summarise existing literature on the prospective association of late-life depression with all-cause mortality, as well as the first meta-analysis on late-life depression and cardiovascular mortality among older adults living in the community.
From our analysis, the heterogeneity across studies may be caused by regions of studies, age and gender of study participants, length of follow-up and assessment of late-life depression. It is worth noting that studies published after – but not before – 2001 showed heterogeneity. This may be because more studies were conducted outside of North America and Europe in this time period, using more novel and diverse assessment tools for depression. The number of studies published after 2001 was much larger, which also increases the possibility of heterogeneity. In addition, the newly published studies may be subject to heterogeneity by involving more stratified analysis and various adjustment factors. Despite the heterogeneity, the associations are statistically significant across most subgroups with similar effect sizes and the trim-and-fill analysis also yielded significant results, which suggests that our results were valid and reliable.
Another potentially important factor that may be related to heterogeneity is the onset of depression, which is not identified in most studies. Previous studies have shown that late-onset depression (with the first episode of depression occurring during late life) has a distinctive aetiology compared with early-onset depression (with the first episode of depression occurring before late life), and that late-onset depression is highly correlated to vascular pathology.Reference Papazacharias, Logroscino, Barulli and Nardini17 Compared with older adults with early-onset depression and age-matched controls, those with late-onset depression show more severe structural brain abnormalities and cerebrovascular pathology,Reference Papazacharias, Logroscino, Barulli and Nardini17 which is consistent with the vascular depression hypothesis. Vascular depression may manifest as areas of white matter hyperintensity on the magnetic resonance imaging studies and/or present as executive dysfunction; both these clinical manifestations are, in turn, associated with risk factors for cardiovascular disease and cardiovascular mortality.Reference Sheline, Pieper, Barch, Welsh-Boehmer, McKinstry and MacFall18,Reference Taylor, Aizenstein and Alexopoulos19 Therefore, late-onset depression may predict a higher risk of mortality, particularly cardiovascular mortality. This is consistent with our sensitivity analysis on late-onset depression, which showed larger effect sizes than those in general, although very few studies included in our analysis specifically examined late-onset depression.Reference Teng, Yeh, Lee, Lin and Lai20,Reference Penninx, Guralnik, Mendes de Leon, Pahor, Visser and Corti21 This calls for future studies to compare early-onset with late-onset depression for prediction of mortality, which could help improve prevention and treatment of different subtypes of depression as well as prevention of all-cause and cardiovascular mortality.
In addition to vascular depression, other mechanisms which are not fully understood may be involved in the association between late-life depression and mortality. It is plausible that depression may lead to death through unhealthy behaviours.Reference Khawaja, Westermeyer, Gajwani and Feinstein22 Depression may lead to poor health risk-related behaviours (e.g. tobacco use, alcohol use, binge drinking, physical inactivity, poor eating habits), which may further lead to worsened health conditions.Reference Verger, Lions and Ventelou23 Older adults with depression are likely to have poor adherence to prescribed treatment,Reference Carney, Freedland, Eisen, Rich and Jaffe24 which may worsen the health conditions and increase the risk of death. The risk may be particularly higher among community-dwelling older adults who live independently without access to special care. In addition, depression may result in higher risk of comorbidities through delayed immune responses and the triggering of pro-inflammatory responses, which in turn may influence mortality from various causes.Reference Goodwin25,Reference Morimoto and Alexopoulos26
The results of our study may have clinical and public health implications. Given the high prevalence of late-life depression and its association with mortality, interventions aimed at prevention of depression among older adults should also help with reducing mortality. A number of risk factors for late-life depression have been identified, including disease precursors such as cardiovascular disease, obesity, cerebral infarction; social factors such as loneliness and reduced independence; and certain psychological problems such as bereavement and certain personality traits.Reference Aziz and Steffens27,Reference Allan and Ebmeier28 Moreover, unfavourable lifestyle choices such as smoking, physical inactivity, heavy or binge drinking have been found to be prevalent among older adults with depression.Reference Chang, Pan, Kawachi and Okereke29 Literature has shown that targeting older adults with these risk factors may be effective in preventing depression.Reference Hall and Reynolds-Iii30 Studies have also shown that the total number of points on a depression scale such as GDS-15, even without a depression diagnosis, may be associated with higher mortality.Reference Kamphuis, Kalmijn, Tijhuis, Geerlings, Giampaoli and Nissinen31–Reference Piña-Escudero, Navarrete-Reyes and Ávila-Funes34 This suggests that each increment of depressive symptoms is associated with increased risk of mortality, without a clear threshold.
Taken together, these data underscore that prevention and timely treatment of depression may play an important role in maintaining optimal health and reducing mortality in older patients. Studies have shown that managed depression care in primary practice reduces mortality in older adults with major depression.Reference Gallo, Bogner, Morales, Post, Lin and Bruce35,Reference Gallo, Morales, Bogner, Raue, Zee and Bruce36 Pharmacotherapy for late-life depression may be effective; however, antidepressant use in this population may present its own set of challenges.Reference Allan and Ebmeier28 For example, antidepressants may negatively affect health by disrupting adaptive processes, such as in the immune system.Reference Andrews, Thomson, Amstadter and Neale37 In addition, among different subtypes of late-life depression, vascular depression is resistant to antidepressant treatment.Reference Aizenstein, Baskys, Boldrini, Butters, Diniz and Jaiswal38 For all of the above reasons, proper management of mental health in the elderly should also consider a variety of psychotherapeutic approaches. These may include problem-solving, cognitive and interpersonal psychotherapy, all of which may be helpful in managing late-life depression among older people who are resistant to antidepressant medications.Reference McGovern, Kiosses, Raue, Wilkins and Alexopoulos39
The strengths of this study involve the large number of included studies and the ability to explore sources of heterogeneity. On the other hand, the limitation of the available literature and consequently of this review is the relative paucity of studies that used physician diagnoses to assess depression. Although standardised scales of depressive symptoms are validated and have been used in population studies, there appears to be discordance between diagnosis-based and scale-based results, especially with respect to cardiovascular mortality. Moreover, even among the studies that defined depression based on standardised scales, the cut-off points varied. This calls for a standardised way of categorising depression.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2019.74.





eLetters
No eLetters have been published for this article.