Prescribing of antidepressants in Europe increased by an average of 20% per year between 2000 and 2010. Reference Gusmão, Quintão, McDaid, Arensman, Van Audenhove and Coffey1 However, the quantity of antidepressant prescribing varies widely between countries, with 6.4 times as many antidepressants prescribed per person in Iceland than in Estonia in 2010. 2 A large body of research into the epidemiology of depression and anxiety disorders shows higher prevalence among women, individuals in late middle age and those of lower socioeconomic status, Reference McManus, Meltzer, Brugha, Bebbington and Jenkins3,Reference Wittchen and Jacobi4 but no substantial difference between European countries. Reference Wittchen, Jacobi, Rehm, Gustavsson, Svensson and Jönsson5 Little is known about the reasons for the inter-country variation in antidepressant use. Variations in treatment-seeking, availability of providers, spending on healthcare services and other differences between healthcare systems are likely important factors. Societal attitudes towards mental illness may also play a role, as is the case for help-seeking for mental health problems. Reference Evans-Lacko, Brohan, Mojtabai and Thornicroft6,Reference Mojtabai7 In this study, we investigated individual- and country-level factors associated with: (a) any anti-depressant use; and (b) regularity of antidepressant use among those who reported antidepressant use, as a quality indicator for treatment regimens. Regularity is important because clinical guidelines recommend that antidepressants be taken regularly for a minimum period of a few months, Reference Anderson, Ferrier, Baldwin, Cowen, Howard and Lewis8 and adherence has been shown to be low in community settings. Reference Lingam and Scott9 We hypothesised that antidepressant use patterns would reflect the sociodemographic characteristics associated with affective disorders, and that higher levels of healthcare spending and lower levels of mental health-related stigma in each country would be associated with higher levels of antidepressant use and greater regularity.
Method
Data source
The key data source was Eurobarometer 2010. This is a cross-sectional survey of residents of 27 European Union Member States, with approximately 1000 individuals from each country interviewed. Participants were recruited via multistage random probability sampling and were representative of residents of each country aged 15 years or older. Data were collected via face-to-face interviews (n = 26 800). Full details of the design and sampling are given elsewhere. 10,11
As this study was based on fully anonymised, publicly available data, ethical approval was not needed.
Dependent variables
Two dichotomous dependent variables derived from Eurobarometer 2010 were examined.
Any use of antidepressants in the past 12 months
Participants were asked: ‘Have you taken any antidepressants in the last 12 months?’ Responses were: (a) ‘Yes, regularly for a period of at least 4 weeks’; (b) ‘Yes, regularly for a period of less than 4 weeks’; (c) ‘Yes, from time to time when I felt the need’; and (d) ‘No, not at all’. These responses were combined into ‘any use’ versus ‘no use’.
Regularity of use among antidepressant users
The first two responses from the previous question were combined into an indicator variable for regular use versus non-regular use.
Independent variables
Individual-level variables were taken from Eurobarometer 2010. The sources of country-level variables were taken from various sources and these are described below.
Sociodemographic information
Sociodemographic information included age (grouped into 15–39, 40–54 and 55+ years), gender and employment status. To assess employment status, participants were asked: ‘What is your current occupation?’ Students and employed participants were categorised as ‘employed’. Participants looking after the home, and those who were ill or retired were categorised as ‘economically inactive’, and the remainder were rated as ‘unemployed’. Self-perceived social class was assessed by asking the participants to place themselves on a ladder, step 1 of which corresponded to the lowest level in society and step 10 to the highest. Individuals placing themselves on levels 1–4 were categorised as ‘low’, 5–6 as ‘medium’ and 7–10 as ‘high’; 3.1% of individuals refused to answer this question. Data for these individuals were imputed from their occupation and whether they had difficulty paying bills.
Mental health symptoms
Mental health symptoms were assessed using the five-item Mental Health Inventory (MHI-5). The MHI-5 is a valid and reliable measure of common mental disorders derived from the Short Form 36 (SF-36). Reference McCabe, Thomas, Brazier and Coleman12,Reference Ware and Gandek13 Higher scores indicate worse mental health. As a validated cut-point has not been established for this scale, Reference Kelly, Dunstan, Lloyd and Fone14 individuals were categorised into three groups: those with the worst mental health, scoring in the top 5% on the MHI-5; those with poorer than average mental health, scoring above the median score but excluding the top 5%; and those with better than average mental health, scoring lower than the median value; 1.3% of individuals answered ‘don't know’ to some MHI-5 items, and for these cases the mean score from other items was used; 0.2% of individuals answered ‘don't know’ to all MHI-5 items, and their scores were imputed from their gender and occupation.
Individual attitudes towards people with mental health problems
The attitudes of individual Eurobarometer 2010 participants were assessed by the question, ‘Which of the following two statements best describe how you feel?’: (1) ‘You would find it difficult talking to someone with a significant mental health problem’; (2) ‘You would have no problem talking to someone with a significant mental health problem’. Individuals answering ‘don't know’ were grouped with option (2).
Difficulty paying bills
This measure was used as an indicator of financial difficulties. Participants were asked: ‘During the last 12 months, would you say you had difficulties to pay your bills at the end of the month?’ The responses ‘from time to time’ and ‘most of the time’ were grouped as indicating difficulty, and the responses ‘never’ and ‘refused to answer’ were grouped as no difficulty.
Country-level healthcare spending
World Bank data provided annual healthcare spending per capita in US$ in 2010, which ranged from US$457 in Romania to US$8193 in Luxembourg. 15 The 27 European countries are distributed across this range, and were therefore assigned to four equally sized groups: those spending US$457–1002, US$1402–2872, US$2895–4618 and U$4658–8193 per capita.
Country prevalence of stigmatising attitudes towards people with mental health problems
This was assessed in Eurobarometer 2006 11 using four statements about various stigmatising beliefs. People with psychological or emotional health problems: (1) constitute a danger to others; (2) are unpredictable; (3) have themselves to blame; and (4) never recover. Participants rated their agreement on a 4-point Likert scale from ‘totally disagree’ to ‘totally agree’. Those responding ‘totally agree’ or ‘tend to agree’ were grouped together as endorsing the statement. The country-level measures were computed as the proportion of respondents endorsing each statement in each country. Each country-level attitude variable was standardised and a z-score was computed as an indicator of how far away (in standard deviations) the country prevalence was from the mean prevalence.
Statistical analysis
Separate multivariable logistic regression models were used to examine predictors of the two outcome variables – any use of anti-depressants and regularity of use. The model for any use of antidepressants included the full sample (n = 26 800), and the model for regular use was limited to those who reported any use (n = 1995). Eurobarometer 2010 post-stratification weights, based on gender, age, region and size of locality, were used in all analyses to estimate the country-level averages. All analyses were carried out using R version 3.0.3 (www.r-project.org).
Results
Prevalence of antidepressant use
Of the adults in our sample, 7.2% (unweighted frequency, n = 1995) reported taking antidepressants at some time in the past year. There was wide variation between countries in the prevalence of antidepressant use, from 15.7% in Portugal to 2.7% in Greece (Fig. 1). Overall prevalence of antidepressant use, sociodemographic and mental health-related characteristics is presented in Table 1.
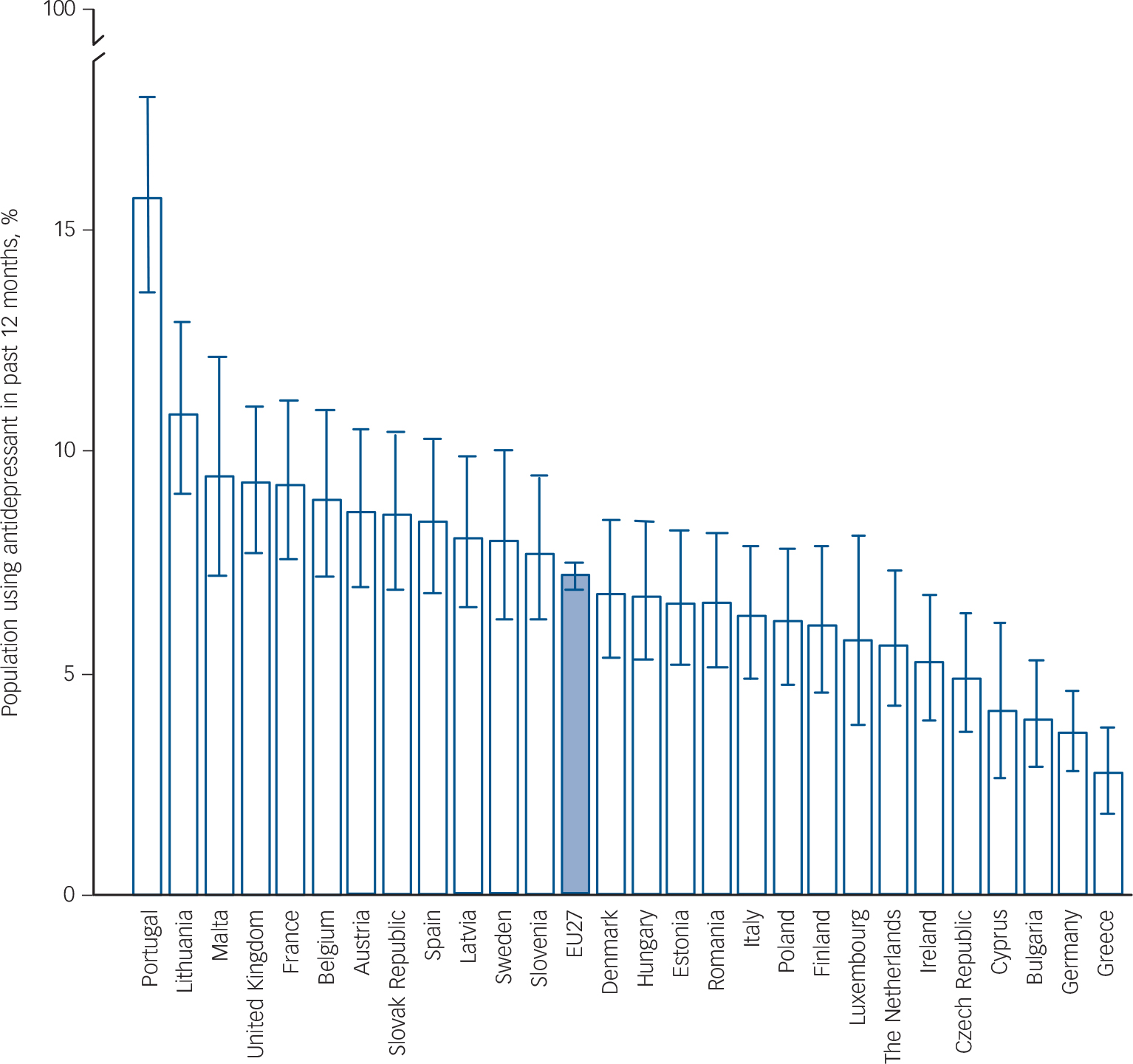
Fig. 1 Percentage of general population that have used antidepressants in the past 12 months by country, with 95% confidence intervals (note maximum value of 15.7%).
TABLE 1 Prevalence of antidepressant use and regular antidepressant use among those who use antidepressants

| Any use of antidepressants in past 12 months (general population) % (95% CI) |
Taking regularly (antidepressant users only) % (95% CI) |
|
|---|---|---|
| MHI-5 | ||
| 5–10 | 2.0 (1.7–2.2) | 60.5 (54.1–66.6) |
| 11–17 | 9.5 (9.0–10.0) | 54.5 (51.6–57.3) |
| 18+ | 34.6 (32.1–37.2) | 66.8 (62.4–71.0) |
| Comfortable talking to someone with a mental health problem |
||
| Yes | 6.9 (6.5–7.3) | 63.3 (60.5–66.1) |
| No | 7.9 (7.3–8.4) | 49.7 (46.0–53.4) |
| Gender | ||
| Female | 9.4 (8.9–9.9) | 58.2 (55.5–60.9) |
| Male | 4.9 (4.5–5.3) | 58.1 (54.0–62.1) |
| Age | ||
| 15–39 | 4.5 (4.1–5.0) | 64.8 (60.2–69.3) |
| 40–54 | 8.6 (8.0–9.3) | 60.8 (56.7–64.8) |
| 55+ | 9.5 (8.9–10.1) | 52.3 (49.1–55.6) |
| Employment status | ||
| Employed | 4.5 (4.2–4.9) | 61.0 (57.2–64.7) |
| Economically inactive | 11.0 (10.4–11.7) | 55.6 (52.5–58.7) |
| Unemployed | 10.4 (9.2–11.7) | 60.2 (53.6–66.5) |
| Self-perceived social class | ||
| Low | 12.4 (11.6–13.3) | 56.0 (52.2–59.7) |
| Medium | 6.5 (6.1–7.0) | 58.7 (55.2–62.0) |
| High | 4.8 (4.3–5.3) | 62.1 (56.9–67.2) |
| Difficulty paying bills | ||
| No | 5.1 (4.8–5.5) | 62.6 (59.2–65.8) |
| Yes | 10.6 (10.0–11.2) | 54.7 (51.7–57.7) |
MHI-5, five-item Mental Health Inventory.
Characteristics associated with antidepressant use
The multivariable regression results presented in Table 2 show that individuals had higher odds of taking antidepressants if they: (a) had higher MHI-5 scores; (b) were female; (c) were aged over 40 years; (d) were not employed or looking after the home (compared with those employed or studying); (e) perceived themselves to be of lower social class; and (f) reported difficulty paying their bills. Comfort with talking to someone with a mental health problem was not associated with the odds of taking anti-depressants. Individuals had higher odds of taking antidepressants if they lived in a country that spent more on healthcare (but the relationship did not show a clear gradient and unadjusted odds ratios were not statistically significant – see online Table DS1), lived in a country where residents were more likely to consider people with mental illness to be dangerous, or lived in a country where residents were less likely to consider people with mental illness to never recover or to have themselves to blame for their illness.
TABLE 2 Results of the multivariable logistic regression models for predictors of antidepressant use in Eurobarometer 2010

| Any use of antidepressants in past 12 months (sample N = 26,800; users n = 1995) adjusted OR (95% CI) |
Taking regularly (sample N = 1995; regular users n = 1154) adjusted OR (95% CI) |
|
|---|---|---|
| Individual-level variables | ||
| MHI-5 score (ref.: Reference Wittchen, Jacobi, Rehm, Gustavsson, Svensson and Jönsson5–10) | ||
| 11–17 | 4.77 (4.11–5.52)Footnote *** | 1.14 (0.83–1.57) |
| 18+ | 19.43 (16.11–23.43)Footnote *** | 2.51 (1.72–3.66)Footnote *** |
| Uncomfortable talking to someone with a mental health problem | 0.98 (0.88–1.09) | 0.71 (0.58–0.88)Footnote *** |
| Male | 0.62 (0.55–0.69)Footnote *** | 0.93 (0.75–1.16) |
| Age, years (ref.: 15–39) | ||
| 40–54 | 1.69 (1.47–1.94)Footnote *** | 0.74 (0.56–0.99)Footnote * |
| 55+ | 1.45 (1.24–1.71)Footnote *** | 0.58 (0.42–0.78)Footnote *** |
| Labour status (ref.: employed) | ||
| Economically inactive | 1.76 (1.51–2.04)Footnote *** | 1.10 (0.85–1.43) |
| Unemployed | 1.53 (1.28–1.83)Footnote *** | 0.92 (0.65–1.30) |
| Perceived SES (ref.: = low) | ||
| Mid | 0.75 (0.66–0.85)Footnote *** | 0.88 (0.70–1.11) |
| High | 0.71 (0.60–0.84)Footnote *** | 0.85 (0.62–1.16) |
| Difficulty paying bills | 1.44 (1.28–1.62)Footnote *** | 0.84 (0.67–1.05) |
| Country-level variables | ||
| Health spend per capita, US$ (ref.: <1000) | ||
| 1000–2999 | 1.58 (1.35–1.87)Footnote *** | 1.48 (1.06–2.06)Footnote * |
| 3000–4499 | 1.77 (1.47–2.13)Footnote *** | 2.34 (1.62–3.37)Footnote *** |
| 4500+ | 1.79 (1.45–2.20)Footnote *** | 4.75 (3.01–7.48)Footnote *** |
| Stigmatising attitudes: z-score of % agreeing with statement | ||
| Mentally ill people are unpredictable | 1.06 (0.97–1.15) | 1.27 (1.06–1.53)Footnote * |
| Mentally ill people are dangerous | 1.27 (1.16–1.38)Footnote *** | 1.15 (0.96–1.38) |
| Mentally ill people never recover | 0.87 (0.79–0.95)Footnote *** | 0.56 (0.46–0.69)Footnote *** |
| Mentally ill people have selves to blame | 0.79 (0.71–0.87)Footnote *** | 0.81 (0.66–1.01) |
MHI-5, five-item Mental Health Inventory; ref., reference value; SES, socioeconomic status.
* P<0.05,
** P<0.01,
*** P<0.001.
Characteristics associated with regularity of antidepressant use
Fifty-eight per cent of antidepressant users reported regular use of antidepressants. There was wide variation between countries, from 89% in Sweden to 19% in Bulgaria (Fig. 2).
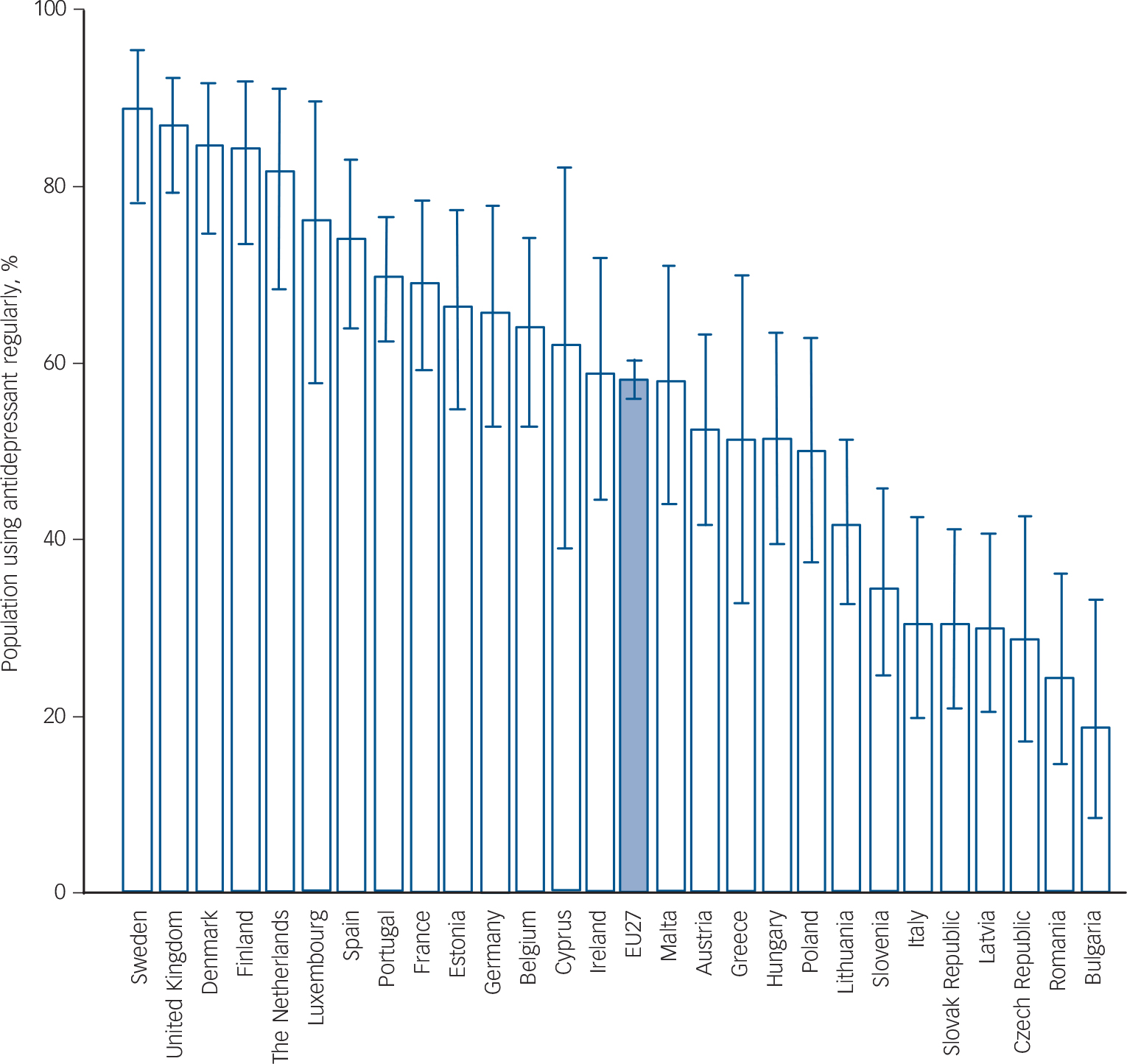
Fig. 2 Percentage of antidepressant users that report taking them regularly by country, with 95% confidence intervals.
The multivariable regression results showed that individuals who reported taking antidepressants had higher odds of taking them regularly if they had a higher MHI-5 score, were more comfortable talking to someone with a mental health problem and were younger (Table 2). There were no significant associations with gender, employment status, perceived social class or difficulty paying bills. At the country level, individuals had higher odds of taking antidepressants regularly if they resided in a country that spent more on healthcare per capita, where residents were more likely to consider people with mental illness to be unpredictable, and where residents were less likely to consider people with mental illness to never recover. At a country level, there was no statistically significant correlation between prevalence of antidepressant use and the proportion of antidepressant users reporting regular use (r = 0.15, P = 0.44).
Discussion
This study provides new insights into how societal attitudes and spending on healthcare are associated with antidepressant use. These findings explain some of the variation in antidepressant use across Europe and provide further evidence for the relationship between stigma and treatment for mental illness. The findings also contribute substantively to the study of the epidemiology of anti-depressant use in Europe, which to date provides limited insight into the sociodemographic and contextual correlates of variations across countries.
The 12-month prevalence of antidepressant use of 7.2% in 2010 is double a previous estimate of 3.7% in 2000, Reference Alonso, Angermeyer, Bernert, Bruffaerts, Brugha and Bryson16 which reflects a doubling in prescription rates over the same period in 18 European countries. 2 The demographic associations with anti-depressant use in Europe have not been investigated in detail in previous research. One study in Europe Reference Ohayon and Lader17 showed that women and those in middle age are more likely to use antidepressants, which is consistent with our findings. Our findings are also broadly consistent with studies from the USA, which show that older people, women and people with worse mental health are more likely to take antidepressants. Reference Mojtabai and Olfson18–Reference Stagnitti20
The sociodemographic characteristics associated with anti-depressant use in this study were similar to those typically found to be associated with affective disorders in community surveys. Reference McManus, Meltzer, Brugha, Bebbington and Jenkins3,Reference Wittchen, Jacobi, Rehm, Gustavsson, Svensson and Jönsson5 At the country level, health spending and stigmatising attitudes were associated with antidepressant use to some extent. Interestingly, different aspects of stigma had opposite effects on the likelihood of taking antidepressants.
The prevalence of regular use of antidepressants is low in view of practice guideline recommendations that they should be taken regularly for effective treatment, with only 58% of the participants reporting that they take them regularly. This is also consistent with existing research, which shows low adherence to antidepressant regimens. An international review of studies showed a median adherence rate of only 40%. Reference Lingam and Scott9 Low adherence may be due to prescriber factors. For example, in a study of prescribing between 1992 and 1997 in the UK, Reference Dunn, Donoghue, Ozminkowski, Stephenson and Hylan21 only 33% of selective serotonin reuptake inhibitor prescriptions were consistent with guidelines. Patients' concerns about dependence, toxicity and stigma may also contribute to the low rate of regular use. Reference Pound, Britten, Morgan, Yardley, Pope and Daker-White22 Finally, patients may discontinue antidepressants early because they start to feel better.
The results regarding the regularity of use within demographic groups are relevant to clinical practice. In particular, we found that middle-aged and older adults are less likely to take anti-depressants regularly. Clinicians may thus want to pay greater attention to monitoring medication use in this age group.
One of the most striking results from this study was the strong association of healthcare spending with regular use of antidepressants. A possible explanation is that physicians in better-funded healthcare systems have more time, training and support and make more accurate diagnoses and prescribe more effective drug regimens. Alternatively, better-funded healthcare systems may provide more guidance to patients on the use of drugs or make drugs more affordable. A study in Australia found that an increase in co-payments (transferring some of the cost of drugs to patients) reduced dispensing. Reference Hynd, Roughead, Preen, Glover, Bulsara and Semmens23
We found no correlation at a country level between prevalence of antidepressant use and the proportion of antidepressant users reporting regular use. We might have expected countries with higher prevalence to have more people with less severe symptoms taking antidepressants, and therefore lower regularity of use. However, this did not appear to be the case. Regularity of use appears to be low in Eastern European countries and high in Scandinavian countries. As these countries tend to have lower and higher per capital income respectively, it is difficult to tease out the contribution of economic factors and regional cultural factors. We included proxies for both of these variables in our analyses and the results suggest that economic and cultural factors may independently contribute to the likelihood of individuals taking antidepressants regularly.
The results relating to stigmatising attitudes are complex and merit some discussion. It is clear that individual- and country-level attitudes play an important role in whether and how people use antidepressants. At an individual level, comfort talking to someone with a mental health problem does not appear to make people more or less likely to use antidepressants, but does appear to make people less likely to use these medications regularly.
As has been shown previously, different types of social stigma vary in their association with outcomes for people with mental illness. Reference Evans-Lacko, Brohan, Mojtabai and Thornicroft6 The findings from our study suggest that individuals living in a country where a higher proportion of the public believes that people with mental illnesses are ‘dangerous’ is associated with a greater likelihood of using antidepressants. Other research has shown that a belief that people with mental illnesses are dangerous is associated with greater likelihood of help-seeking, Reference Mojtabai7 more support for coercive treatment Reference Corrigan, Markowitz, Watson, Rowan and Kubiak24,Reference Mossakowski, Kaplan and Hill25 and a biogenetic explanation for mental illness. Reference Kvaale, Gottdiener and Haslam26 It may be that a ‘medicalised’ concept of mental illness in which mental illness is considered ‘a disease like any other’, Reference Pescosolido, Martin, Long, Medina, Phelan and Link27 which can be treated with effective medical therapy, contributes to greater use of medical treatments such as antidepressants. Conversely, living in a country with stronger beliefs that people with mental illness ‘have themselves to blame’ or ‘never recover’ was associated with a lower likelihood of using antidepressants and lower regularity of use. The view that people with mental illnesses ‘never recover’ has particularly strong and significant inverse associations with antidepressant use and regular use. Viewing mental illness as a personality fault or an incurable illness may contribute to lower likelihood of use of medical therapies. Other research has also shown that attitudes regarding blame are associated with lower rates of willingness to seek help and are often inversely associated with endorsement of a biogenetic model. These results support the idea that medicalised views of mental illness may act as a ‘double-edged sword’, leading to higher rates of treatment but also greater social distance Reference Pescosolido, Martin, Long, Medina, Phelan and Link27–Reference Schomerus, Schwahn, Holzinger, Corrigan, Grabe and Carta29 and social exclusion, for example from employment. Reference Evans-Lacko, Knapp, McCrone, Thornicroft and Mojtabai30
Strengths and limitations
This study was based on a large and representative sample and included both individual and contextual variables from 27 diverse European countries, providing powerful models. Nevertheless, the study had a number of limitations. First, Eurobarometer is a cross-sectional survey, thus limiting causal inference. Second, many of the variables used are based on self-report and may be vulnerable to recall bias. It was not possible to verify antidepressant use with medical records; however, past research has shown good agreement between self-reports of medication use and pharmacy records and low risk of bias. Reference Cotterchio, Kreiger, Darlington and Steingart31,Reference Kwon, Bungay, Pei, Rogers, Wilson and Zhou32 Third, mental health status was determined via a brief self-report measure and not verified by a clinician. Furthermore, specific mood and anxiety disorders could not be assessed based on these data. However, mean MHI-5 scores were highest for women and people aged 40–54, which corresponds with patterns of common mental disorders and supports validity of the data. Additionally, some of the effect sizes are small and thus we have tried to emphasise the magnitude of the association in addition to statistical significance given the relatively large sample size. Finally, the data are based on European countries only, which have specific healthcare systems and attitudes towards mental health and medications, and therefore the results may not be generalisable to other regions.
Implications
In the context of these limitations, these findings provide a broad view of both individual and sociocultural correlates of antidepressant use. Some of the wide variation in antidepressant use across Europe is explained by differences in healthcare spending and attitudes towards mental illness. Healthcare spending in this study is likely a proxy for many variables, including availability of medical care, training of healthcare staff and affordability of drugs. Our study shows that healthcare spending is strongly associated with regularity of antidepressant use. In addition, attitudes towards people with mental illness are associated with both use and regularity of use. Policy aiming to achieve appropriate prescribing and use of antidepressants will need to consider individual and societal attitudes as well as medical practices. Variations in the association of various attitudinal factors with antidepressant use points to the need for a more nuanced approach to messages incorporated in public mental health campaigns. The view that people with mental illness cannot recover or are blameworthy for their illness appears to be a strong barrier to the appropriate and regular use of antidepressants. Countering these beliefs through public health campaigns and interventions may thus help to improve access to and more appropriate use of antidepressant medications.







eLetters
No eLetters have been published for this article.