Individuals undergoing assessment for dangerous and severe personality disorder (DSPD) are likely to be a heterogenous group, with divergent psychological and treatment requirements. Clinical assessment should, therefore, make provision for distinguishing between individuals with different personality characteristics and cognitive difficulties. Individuals with borderline personality disorder constitute an important subgroup within the DSPD service. In our studies of 31 prisoners from the initial sample assessed for DSPD at HMP Whitemoor, 17 had a definite diagnosis of borderline personality disorder according to DSM–IV criteria (American Psychiatric Association, 1994). Several sources of evidence attest to a link between borderline personality disorder and serious antisocial behaviour. Borderline personality disorder is highly comorbid with antisocial personality disorder (Reference Becker, Grilo and EdellBecker et al, 2000), and may involve common psychological mechanisms such as affective instability and impulsiveness (Reference ParisParis, 1997). Second, it is over-represented in surveys of forensic psychiatric services (Reference Coid, Kahtan and GaultCoid et al, 1999) and, third, its most prominent characteristics –unstable, intense relationships and affective instability – are exaggerated in individuals with histories of extreme violence (Reference RaineRaine, 1993).
Other evidence suggests that borderline personality disorder is mediated by disturbances within neural (Reference Driessen, Herrman and StahlDriessen et al, 2000; Reference Donegan, Sanislow and BlumbergDonegan et al, 2003) and neurochemical systems (Reference Hollander, Stein and DeCariaHollander et al, 1994; Reference Soloff, Meltzer and GreerSoloff et al, 2000) that support cognitive and emotional functions, although the specificity of these phenomena remains uncertain. Neuropsychological investigations suggest that borderline personality disorder is associated with memory disturbances, including difficulties in the encoding and retrieval of complex multi-modal information (Reference O'Leary, Brouwers and GardnerO'Leary et al, 1991; Reference BurgessBurgess 1992; Reference Judd and RuffJudd & Ruff, 1993; Reference Kurtz and MoreyKurtz & Morey, 1999). However, to date positive results have been demonstrated only in comparisons of patients with borderline personality disorder and non-clinical healthy controls, again raising the question as to whether such impairments tell us anything about the disorder itself or are merely indicative of the non-specific consequences of psychological distress. Similarly, there have been no studies of memory function in prisoners with borderline as compared with other personality disorders.
In this study, we used traditional pencil-and-paper neuropsychological instruments to investigate visual and verbal memory function in prisoners undergoing assessment for DSPD. All prisoners were screened for neurological illness, learning disability, current mood disorder, and current or previous psychoses. We sought to compare the performance of prisoners with DSM–IV borderline personality disorder with that of prisoners with other DSM–IV personality disorders.
METHOD
Participants
Thirty-six male prisoners participated, 18 fulfilled DSM–IV criteria for borderline personality disorder (borderline group) and 18 had other personality disorders (non-borderline group). Thirty-one prisoners were voluntarily undergoing assessment at a maximum security prison (Whitemoor) as part of the UK government's DSPD policy initiative. Five prisoners were undergoing assessment at a medium secure unit (Arnold Lodge, RSU) as a part of an assessment for prisoners with clear personality difficulties. All provided written, informed consent.
Clinical assessment
Participants underwent a full psychiatric assessment of DSM–IV Axis I and Axis II disorders. Axis I disorders were assessed using the Structured Clinical Interview for DSM–IV Axis I Disorders (SCID–I; Reference First, Spitzer and GibbonFirst et al, 1996). One participant from the borderline group and 4 from the non-borderline group were screened for Axis I disorders using the Schedule of Affective Disorders and Schizophrenia (Reference Endicott and SpitzerEndicott & Spitzer, 1979). Exclusion criteria were as follows: previous or current neurological illness or injury; previous or current psychotic illness (including schizoaffective disorder and bipolar I or II disorder); current unipolar depression; any evidence of learning disability. Of the 18 participants with borderline personality disorder, 1 received a comorbid diagnosis of gender identity dysphoria, 1 had an adjustment disorder, 1 had a history of attention-deficit hyperactivity disorder (ADHD) and 1 had alcohol dependency. Of the non-borderline participants, 1 was diagnosed with ADHD, and 1 with polydrug misuse and generalised anxiety disorder. Significant previous alcohol or substance misuse was reported by 3 men with borderline and 1 with other personality disorders. The number of participants who had been dependent upon alcohol, stimulants (i.e. amphetamine) or opiates was 4 and 3 respectively.
Personality disorders
Personality disorder was assessed with the International Personality Disorder Examination (IPDE; Reference Loranger, Sartorius and AndreoliLoranger et al, 1994), which is a semi-structured interview that provides diagnostic information about DSM–IV personality disorders and indicates both ‘definite’ and ‘probable’ diagnoses within the personality disorders specified in Axis II. The participants with borderline personality disorder had more definite diagnoses of personality disorder than the non-borderline participants (2.06±0.29 v. 1.33±0.27;F (1, 34)=3.40, P=0.074). The distribution of ‘definite’ and ‘probable’ diagnoses is shown in Table 1.
Table 1 Number and types of concurrent DSM–IV personality disorders diagnosed in 18 prisoners with borderline personality disorder and 18 with other personality disorders.

| Borderline participants | Non-borderline participants | |||||
|---|---|---|---|---|---|---|
| Definite diagnosis | Probable diagnosis | Definite diagnosis | Probable diagnosis | |||
| Cluster A | ||||||
| Paranoid | 6 | 3 | 4 | 2 | ||
| Schizoid | 0 | 3 | 0 | 2 | ||
| Schizotypal | 1 | 2 | 1 | 0 | ||
| Cluster B | ||||||
| Antisocial | 14 | 2 | 11 | 4 | ||
| Borderline | 18 | 0 | 0 | 1 | ||
| Histrionic | 4 | 0 | 2 | 1 | ||
| Narcissistic | 5 | 2 | 3 | 0 | ||
| Cluster C | ||||||
| Avoidant | 6 | 1 | 2 | 2 | ||
| Dependent | 0 | 2 | 0 | 0 | ||
| Obsessive–Compulsive | 1 | 4 | 2 | 0 | ||
Each participant was also rated for severity of personality disturbance according to the procedure described by Tyrer & Johnson (Reference Tyrer and Johnson1996) in which the number of diagnoses within and between DSM–IV clusters is transformed into four levels of severity: no personality disorder, personality difficulty, simple personality disorder and diffuse personality disorder (Psychiatric Assessment Schedule (PAS)). The PAS has been used to specify the presence, cluster type and severity of personality disorders in a variety of clinical settings (Reference Cuesta, Peralta and ZarzuelaCuesta et al, 2001; Reference Seivewright, Tyrer and JohnsonSeivewright et al, 2002). It has been shown to have adequate interrater and test–retest reliability (Reference Tyrer and AlexanderTyrer &Alexander, 1979; Reference Tyrer, Strauss and CicchettiTyrer et al, 1983; Reference Hill, Fudge and HarringtonHill et al, 2000) and to predict treatment outcome (Reference Tyrer, Seivewright and TyrerTyrer & Seivewright, 1988). The participants with borderline personality disorder were rated as having a significantly greater breadth of personality disturbance than the non-borderline participants (2.56±0.12 v. 2.00±0.20); F (1, 34)=5.743, P<0.05). Specifically, in the non-borderline group, 1 participant was classified as having no personality disorder but had a total score on the Psychopathy Checklist–Revised (PCL–R; Reference HareHare, 1991; Reference Hart, Hare, Harpur, McReynolds and RosenHart et al, 1992) of 32.6, indicating a very high degree of psychopathy, 3 were classified as having a personality disturbance, 9 as having a simple personality disorder and 5 as having a diffuse personality disturbance. Eight participants in the borderline group were classified by the PAS as having a simple personality disorder and 10 as having a diffuse personality disorder.
Participants were also assessed using the PCL–R which is a 20-item checklist that measures the personality traits and behaviours characteristic of psychopathy. All items are scored on the basis of a file review and semi-structured interview. Notwithstanding recent controversy surrounding the psychometric structure of the PCL–R (Reference Cooke and MichieCooke & Michie, 2001; Reference Cooke, Michie and HartCooke et al, 2004; Reference Neumann, Vitacco and HareNeumann et al, 2005), total scores on the PCL–R in this study were taken to represent the composite of just 2 factors: Factor 1 relates to interpersonal and emotional deficits characteristic of psychopathy whereas Factor 2 relates to a history of criminality and a propensity towards an antisocial lifestyle. Generally, participants PCL–R scores were rated in the high range but were matched between the borderline and non-borderline groups (26.34±1.23 v. 24.96±2.06; F<1.00). There were 11 participants from the non-borderline group and 10 from the borderline group with a PCL–R of 27 or above. The two groups were comparable for Factor 1 (9.62±0.70 v. 10.06±1.22; F<1.00) and Factor 2 scores (12.91± 0.69 v. 11.84±0.81;F<1.10).
Medication
Twelve participants in the non-borderline group were unmedicated; 2 were prescribed atypical antipsychotics; 2 selective serotonin reuptake inhibitors (SSRI) antidepressants, 1 a tricyclic antidepressant, 3 mood stabilisers, 1 beta-blockers, 1 hypnotics and 1 a stimulant. Six participants from the borderline group were not being prescribed any medication; 1 was being prescribed a standard antipsychotic, 6 atypical antipsychotics, 2 SSRI anti-depressants, 8 tricyclic antidepressants, 4 mood stabilisers, 3 beta-blockers and 2 hypnotics. Significantly more participants with borderline personality disorder were receiving antidepressants (χ2=5.9, d.f.=1, P=<0.05) and there was a tendency for a greater proportion to be prescribed antipsychotics (χ2= 3.704, d.f.=1, P=0.054). However, the two groups were well-matched in terms of mood stabilisers (χ2=0.177, d.f.=1, P=0.674), beta-blockers (χ2=1.125, d.f.=1, P=0.289), hypnotics (χ2=0.364, d.f.=1, P=0.546), and stimulants (χ2=1.029, d.f.=1, P=0.31).
Psychometric assessments and self-report measures of mood and impulsivity
All participants were assessed for general cognitive ability using the Wechsler Abbreviated Scale of Intelligence (WASI; Reference WechslerWechsler, 1999). They also completed the Welsh Anxiety Scale (WAS; Reference Welsh, Welsh and DahlstromWelsh, 1956), which is a measure of anxiety/negative affect and is derived from the Minnesota Multiphasic Personality Inventory (MMPI; Reference Hathaway and McKinleyHathaway & McKinley, 1943). High scores on the WAS are thought to relate to a dysthymic and dysphoric nature in which anxiety is a prominent feature. Depressive symptoms were assessed using the short form of the Beck's Depression Inventory (BDI; Reference Beck, Ward and MendelsonBeck et al, 1961). Impulsivity was assessed using the Barratt Impulsiveness Scale (Version 11) (BIS–11; Reference Patton, Stanford and BarrattPatton et al, 1995). The BIS–11 has been used to distinguish between violent and non-violent parolees (Reference Cherek, Moeller and DoughertyCherek et al, 1997), and has been reported to be a reliable measure of impulsivity in inmate populations (Reference Patton, Stanford and BarrattPatton et al, 1995).
Neuropsychological instruments
Verbal memory
Logical Memory and Word Lists sub-tests of the Wechsler Memory Scale–III (Reference WechslerWechsler, 1998) were administered to assess retention of verbal material under immediate and delayed conditions.
Visual memory/Rey–Osterrieth Complex Figure Test
The Complex Figure Test (CFT; Reference OsterriethOsterrieth, 1944) was used to assess visual memory. Participants were scored according to the strict marking scheme described by Bennett-Levy (Reference Bennett-Levy1984) on the quality of their copy, immediate recall (3 min after copy) and delayed recall (25–30 min after copy). Additional measures of the participants' recall of features with good continuation and symmetry were also derived. Previous results have found that recall deficits in the non-verbal tasks, such as the CFT, have been associated with right-sided temporal damage (Reference LezakLezak, 1983).
Statistical analysis
Age, WASI scores, WAS, BDI, BIS–11 and WMS–III subtest scores were analysed using one-way ANOVA with the between-participant factor of group (borderline and non-borderline). Scaled WMS–III scores were derived from the raw scores adjusted for age according to published norms (Reference WechslerWechsler, 1998). Scores on CFT were analysed by repeated-measures ANOVA with the between-participant factor of group and the within-participant factor of trial (copy, immediate and delayed recall score).
To investigate which criteria had the largest impact on neuropsychological test performance, we performed backward regression analyses, including both variables expected to influence memory performance – age (except where the dependent measure was scaled), full WASI score and current mood (BDI score) – and other personality-related variables such as the breadth of personality disorder (PAS score), Factor 1 score of the PCL–R and IPDE ratings of impulsiveness and affective instability (scored as absent, present at a sub-criteria level and present at full criteria level). There were no significant differences between the ages, full WASI scores and current mood ratings for participants rated with the IPDE for different levels of trait impulsivity (all F (2, 35), s<1.8) or for different levels of trait affective instability (F (2, 35) s<1.90). Correlations between ratings of impulsiveness and affective instability and other regressors included in the models were, in the main, modest (-0.10 to -0.19 and 0.01 to 0.28). However, affective instability was significantly correlated with the Factor 2 score of the PCL–R, so the latter was dropped. We report only regressors retained in the final model for the dependent measures.
RESULTS
The participants from the non-borderline group were marginally younger than those from the borderline group (F (1, 34)=1 (Table 2)); but were closely matched in terms of general level of cognitive functioning (F<1). Table 2 shows that although WASI performance IQ scores were within the normal range, the verbal IQ scores tended to be towards the lower end. There was a wide range of ability, with full-scale IQ scores ranging from 70 to 117 in participants with borderline personality disorder, and from 74 to 123 in the non-borderline group.
Table 2 Demographic and psychometric characteristics of 18 prisoners diagnosed with borderline personality disorder and 18 diagnosed with other personality disorders

| Borderline participants | Non-borderline participants | |
|---|---|---|
| Age, years: mean (s.d.) | 34.44 (1.70) | 37.61 (2.25) |
| Full-scale IQ (WASI) score: mean (s.d.) | 93.28 (3.06) | 95.44 (3.64) |
| Verbal IQ (WASI) | 90.67 (3.25) | 91.00 (3.71) |
| Performance IQ (WASI) | 97.17 (2.76) | 100.50 (3.24) |
| Beck's Depression inventory score: mean (s.d.) | 15.11 (2.26) * | 7.44 (1.82) |
| Welsh's Anxiety Scale score: mean (s.d.) | 15.39 (1.35) *** | 7.39 (1.21) |
| BIS-II total score: mean (s.d.) | 77.44 (3.48) ** | 61.83 (2.68) |
| Motor impulsiveness | 27.28 (1.46) ** | 21.61 (1.16) |
| Attentional impulsiveness | 18.89 (1.04) ** | 15.28 (1.01) |
| Planning impulsiveness | 31.83 (1.45) ** | 24.94 (1.10) |
| PAS score: mean (s.d.) | 2.56 (0.12) ** | 2.00 (0.20) |
| PCL–R total score: mean (s.d.) | 26.43 (1.21) | 24.96 (2.06) |
| Factor 1 | 9.62 (0.70) | 10.06 (1.22) |
| Factor 2 | 12.91 (0.69) | 11.84 (0.81) |
WASI, Wechsler Abbreviated Scale of Intelligence; BIS–II, Barratt Impulsiveness Scale (version II); PAS, Psychiatric Assessment Schedule;PCL–R, Psychopathy Checklist–Revised
* P<0.05
** P<0.01
*** P<0.001
Participants with borderline personality disorder reported significantly greater levels of anxiety on the WAS (F (1, 34)=19.612, P<0.001) and depressive/anxious symptoms on the BDI compared with participants without borderline personality disorder (F (1, 34)=6.987, P<0.05) (Table 2). Different aspects of impulsiveness were also increased, as reflected in higher scores on the attentional (F (1, 34)=6.183, P<0.05), motor (F (1, 34)= 9.201, P<0.01) and planning impulsiveness scores of the BIS–11 (F (1, 34)= 14.357, P<0.01) The total impulsiveness score of the BIS–11 was also increased (F (1, 34)=12.668, P<0.01).
Verbal memory/logical memory
Participants with borderline personality disorder recalled significantly fewer story elements when recalling the stories immediately compared with participants without borderline personality disorder (F (1, 33)= 4.54, P<0.05) (Table 3). This was particularly evident when recalling the stories for the very first time (F (1, 33)=10.21, P<0.005). They also performed significantly worse when recalling thematic elements of the test, both immediately (F (1, 33)=9.65, P<0.005) and after a delay of 25–35 min (F (1, 33)=6.03, P<0.05). There were no significant differences between groups in the improvement in immediate recall when hearing the stories for the second time compared with the first time (F<1.00), in the total number of story elements recalled after 25–30 min (F (1, 33)=1.57), or the proportion of information retained in delayed recall (F<1.00). However, the participants with borderline personality disorder showed significantly poorer recognition of story elements (F (1, 32)=6.21, P<0.05).
Table 3 Performance on verbal memory (WMS–II; Reference WechslerWechsler, 1998) tests by 18 prisoners diagnosed with borderline personality disorder and 18 prisoners diagnosed with other personality disorders.

| Mean (s.d.) | |||
|---|---|---|---|
| Borderline participants | Non-borderline participants | ||
| Logical memory (WMS–III) | |||
| Immediate recall | |||
| Immediate recall total score | 8.28 (0.91) * | 10.47 (0.43) | |
| Immediate first recall score | 8.06 (0.78) ** | 11.00 (0.46) | |
| Immediate recall learning slope | 10.06 (0.54) | 9.12 (0.82) | |
| Immediate thematic score ** | 7.72 (0.68) ** | 9.88 (0.55) | |
| Delayed recall | |||
| Delayed recall total score | 8.78 (0.75) | 9.94 (0.52) | |
| Delayed recall percentage retention | 8.89 (0.82) | 9.47 (0.73) | |
| Delayed thematic score | 7.72 (0.68) * | 9.88 (0.54) | |
| Recognition score | 23.89 (0.86) * | 26.41 (0.50) | |
| Word Lists (WMS–III) | |||
| Immediate recall | |||
| List A first recall | 8.33 (0.86) | 10.50 (0.83) | |
| List A recall total score | 8.72 (0.78) | 10.78 (0.87) | |
| Learning slope | 10.39 (0.85) | 9.56 (0.69) | |
| Interference from List A (List B) | 11.72 (0.64) * | 10.00 (0.54) | |
| Delayed recall | |||
| Recall total score | 11.61 (0.67) | 12.89 (0.51) | |
| Recognition score | 10.78 (0.48) | 11.11 (0.58) | |
| Percentage retention | 11.72 (0.59) * | 13.33 (0.51) | |
WMS–III, Wechsler Memory Scale–III
* P<0.05
** P<0.005
Backward regression indicated that both clinical ratings of breadth of personality disorder (PAS score) and affective instability (IPDE criterion score) were significant or near-significant predictors of poor immediate story recall (R 2=0.28; standardised β=-0.32, t=-2.03, P=0.05 and standardised β=-0.37, t=-2.37, P<0.05, respectively). Affective instability alone was a significant predictor of poor immediate recall after hearing the stories for the first time (R 2=0.29; standardisedβ=-0.54, t=-3.53, P<0.001; see Fig. 1), immediate thematic recall (R 2=0.41; standardised β=-0.64, t=-4.56, P<0.001; see Fig. 1) and recognition of story items (R 2= 0.20; standardised β=-0.44, t=-2.77, P<0.01). Cognitive ability (WASI full IQ) predicted better delayed thematic recall scores (R 2=0.44;standardised β=-0.49, t=-3.51, P<0.005) whereas higher Factor 1 scores from the PCL–R and affective instability both predicted worse delayed thematic scores (standardised β=0.32, t=-2.21, P<0.05 and standardised β= 0.35, t=-3.51, P<0.05 respectively; see Fig. 1).
Verbal memory/word lists
Participants with borderline personality disorder tended to show poorer scores on the verbal list learning test compared with participants without borderline personality disorder. Specifically, they tended to recall fewer words after the first learning trial (F (1, 34)=3.29, P=0.08) and after four learning trials (F (1, 34)=3.10, P=0.09). However, there was no difference in terms of the improvement in recall over the course of the four learning trials (F<1). In addition, the participants with borderline personality disorder showed greater levels of interference from the first list (List A) while recalling the second list (List B) (F (1, 35)=4.29, P<0.05; see Table 3). They showed only modest and non-significant reductions in recall scores after a delay of 25–30 min but showed significantly poorer retention at delayed recall compared with the non-borderline group (F (1, 34)=4.28, P<0.05).
Cognitive ability and current mood (BDI score) showed significant but opposing relationships with the number of words recalled after the first learning trial (R 2= 0.46; standardised β=0.45, t=3.337, P<0.005; standardised β=-0.42, t=-3.05, P<0.01, respectively). Current mood alone predicted poorer list recall after the fourth learning trial (R 2=0.14; standardised β=-0.37, t=-2.27, P<0.05).
Visual memory/Rey–Osterrieth Complex Figure Test
Participants with borderline personality disorder obtained significantly lower scores on all aspects of performance compared with participants without borderline personality disorder (F (1,33)=8.11, P<0.01;see Fig. 2). Planned comparisons indicated significantly lower scores on the copy component of the CFT (F (1,33)= 6.86, P<0.05). Specifically, the copies of the two groups showed comparable evidence of good continuation (12.00±0.84 v. 11.22±0.86; F<1) but those with borderline personality disorder tended to show poorer reproduction of the symmetrical components of the CFT (9.61±0.87 v. 12.06±0.82; F (1,35)=4.29, P<0.05). In addition, they produced lower scores on the immediate recall (F (1,33)=5.93, P<0.05) and delayed recall measures (F (1,33)=5.52, P<0.05).

Fig. 1 Performance (and standardised β) on complex verbal (logical memory) and complex visual (Rey–Osterrieth Complex Figure Test (CFT)) memory as a function of clinician-rated trait affective instability as scored on the International Personality Disorder Examination.
Cognitive ability and affective instability were significant predictors of good and poor copy scores (R 2=0.52; standardisedβ=0.40, t=3.19, P<0.005; standardised β=-0.47, t=-3.59, P<0.005; see Fig. 1). Breadth of personality also tended to show some association with poorer copy scores (standardisedβ=-0.22, t=-1.73, P<0.10). However, affective instability was the single best predictor of poor immediate recall score of the CFT (R 2=0.13; standardised β=-0.36, t=-2.18, P<0.05; Fig. 1).
DISCUSSION
These results indicate that a sample of prisoners being assessed for DSPD who were given a diagnosis of DSM–IV borderline personality disorder exhibited significant impairments in the recall of thematic and complex information from verbal and visuospatial memory. These impairments cannot be attributed to a greater incidence of previous or current psychotic disorder, or current mood disorders, since these were exclusion criteria for our study. Neither are they attributable to a lack of motivation since the pattern of test performance did not show the kind of generalised impairment consistent with a motivational deficit. Therefore, since we have identified significant memory impairments in comparison with age and IQ-matched controls with other forms of personality disturbance, these data confirm and extend the findings of O'Leary et al (Reference O'Leary, Brouwers and Gardner1991) and other investigators (Reference BurgessBurgess, 1992; Reference Kurtz and MoreyKurtz & Morey, 1999), by demonstrating that memory impairments have some specificity for borderline personality disorder.
We acknowledge that our two groups of prisoners were inevitably different in ways that may have influenced cognitive function. First, the participants with borderline personality disorder scored significantly higher on the BDI;therefore, their greater ratings of depressive symptomology may account for some of the deficits observed here. However, although BDI scores predicted poorer recall of items from the word lists test on the first and fourth presentations across the entire sample, there was no indication of state mood effects in the case of the logical memory or the Rey–Osterrieth CFT tests. Rather, these impairments seemed most closely tied to the presence or otherwise of a diagnosis of borderline personality disorder and the presence of trait affective instability scored as part of the IPDE assessment. Second, we also note that participants with borderline pesonality disorder were receiving more antipsychotic and antidepressant medication. Previous studies have shown that such medications tend to have mixed effects on cognitive measures (Reference Markovitz and WagnerMarkovitz &Wagner, 1995), depending upon participants' baseline performance, their dose and the treated psychopathology. However, in the present study, the differences in drug regimens between the two groups were relatively modest and unlikely to account for the pattern of our observations.
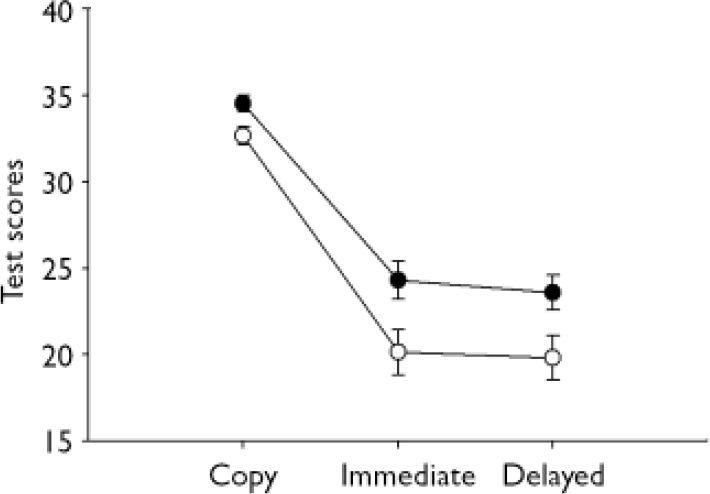
Fig. 2 Performance on the Rey–Osterrieth Complex Figure Test of 18 participants with borderline personality disorder (—○—) and 18 with non-borderline personality disorders (—•—). Delayed recall is at 25-20 min.
Finally, participants with borderline personality disorder had a higher number of ‘definite’ and ‘probable’ comorbid personality disorders so that the increased multiplicity of personality disorders associated with borderline personality disorder (Reference Becker, Grilo and EdellBecker et al, 2000) might also account for the observed memory impairments. However, our analyses indicated that breadth of personality disorder – as measured by the PAS (Reference Tyrer and JohnsonTyrer & Johnson, 1996)– accounted for only a very modest amount of the variance of memory performance, being a significant predictor only of the immediate recall scores of the logical memory test. We did not find that individuals with a diffuse pattern of personality disorder scored consistently worse than those with a simple personality disorder. Finally, it is unlikely that gross differences in clinical ratings of psychopathy can explain our results as these were comparable between our two groups. Instead, the data indicate that poor recall was more closely associated with the presence of borderline personality disorder and its diagnostic features.
Verbal and visuospatial mnemonic function
Prisoners with borderline personality disorder demonstrated significant reductions in the total recall, the first recall and the immediate and delayed thematic recall measures of the WMS–III Logical Memory test, and on the copy, immediate and delayed recall of Rey–Osterrieth CFT. Performance of the WMS–III Word Lists test was more equivocal, showing statistically unreliable impairments in immediate and delayed recall but a significant reduction in the delayed recall of words successfully reproduced at immediate recall. This pattern is broadly similar to those reported previously in community samples, and is consistent with the proposal that the memory impairment in borderline personality disorder is most strongly expressed in the recall of complex material (Reference O'Leary, Brouwers and GardnerO'Leary et al, 1991). Extensive evidence indicates that declarative memory is supported by functionally dissociable sub-systems supported by overlapping neural substrates (Reference SchacterSchacter, 1996). The present data suggest that borderline personality disorder in individuals with significant histories of antisocial behaviour is associated with relatively generalised memory impairments, perhaps reflecting dysfunction in some of these sub-systems.
These data do not tell us too much about whether memory problems relate primarily to the encoding of information, the consolidation or the recall of already sampled information. On the one hand, deficits were most marked in the immediate story recall of the Logical Memory and Rey–Osterrieth CFT tests and there was little sign that these differences were increased at delayed recall (the single exception being the poorer retention of previously remembered items of word lists). This indicates that the prisoners with borderline personality disorder did not show greater forgetting of material that has been successfully recalled earlier, at least over relatively brief intervals. Similarly, there were no significant between-group differences in the improvement seen in performance over the successive learning trials of the WMS–III Word Lists test. However, the participants with borderline personality disorder did show evidence of greater susceptibility to interference while recalling word lists, indicating that the retrieval of verbal information might also be compromised (see Reference Della Rocchetta and MilnerDella Rocchetta & Milner, 1993).
Further information about the nature of the mnemonic deficits is provided by the observation that participants with borderline personality disorder were most clearly impaired on the thematic elements of the Logical Memory test. These relate to the ability to remember the gist of the stories, which is more general than the specific and literal information required by other components of the test. This finding may have real consequences for assessment and treatment in centres such as those in the DSPD initiative. In these and other forensic settings, treatment intervention might involve exposure to sets of concepts, organised around one single theme, relevant to a particular treatment target (e.g. stop-and-think in cognitive skills training). The present results suggest that some prisoners may find it difficult to assimilate even such general ideas when delivered in a verbal format. Treatment development might involve assessing memory for both the themes and the details of treatment programmes over the short and longer-term to optimise delivery in different individuals.
In addition, it was notable that the participants with borderline personality disorder were impaired in the copy component of the Rey–Osterrieth CFT. Previous results involving patients with borderline personality disorder have been equivocal, with two studies reporting that community patients were impaired relative to non-clinical controls (Reference Judd and RuffJudd & Ruff, 1993; Reference Dinn, Harris and AycicegiDinn et al, 2004) but three reporting no differences (Reference O'Leary, Brouwers and GardnerO'Leary et al, 1991; Reference Driessen, Herrman and StahlDriessen et al, 2000; Reference Sprock, Rader and KendallSprock et al, 2000). Given that the participants with borderline personality disorder in the present study also reproduced significantly fewer symmetrical elements of the CFT, further investigations in antisocial populations should at least explore the possibility that memory impairments are accompanied by more basic deficits in visuospatial construction, as well as using tailored tasks to probe the cognitive mechanisms that underlie problems in mnemonic function related to borderline personality disorder.
Our analyses sought to provide a preliminary test of the extent to which state or trait factors were most closely associated with memory dysfunction. We found only limited effects of current mood or trait impulsiveness but more consistent evidence for the involvement of affective instability in poor memory performance. Thus, these data suggest an association between failing regulation of emotion and generalised multi-modal memory deficits in prisoners with a diagnosis of DSM–IV borderline personality disorder. This is consistent with the findings of a complementary study –conducted in an overlapping sample of prisoners assessed for DSPD –demonstrating that affective instability was associated with reduced attention towards emotional cues while making risky choices (Reference Kirkpatrick, Joyce and MiltonKirkpatrick et al, 2007). This, and the present study, utilised clinical ratings of affective instability – scored across a relatively restricted range– but future studies should exploit more recently developed and multi-faceted structured clinical measures of emotional regulation (Reference Koenigsberg, Harvey and MitropoulouKoenigsberg et al, 2002) to examine its influence upon altered cognition in borderline personality disorder.
Finally, the selection of neuropsychological instruments provides only poor information about dysfunction within underlying neural systems. However, the pattern of memory impairments observed is broadly consistent with the proposal that borderline personality disorder involves dysfunction of bilateral frontotemporal systems. The Logical Memory test and Rey–Osterrieth CFT are sensitive to anterior left-sided anterior temporal lobe damage (Reference Trenerry, Jack and CascinoTrenerry et al, 1996; Reference Griffith, Pyzalski and SeidenbergGriffith et al, 2004) and right-sided hippocampal and association cortex damage (Reference Bohbot, Kalina and StepankovaBohbot et al, 1998) respectively. Recent research has also suggested that the amygdala plays a significant role in memory for themes or gist, particularly for emotionally salient information (Reference Adolphs, Denburg and TranelAdolphs et al, 2001). This is consistent with the finding that higher Factor 1 scores, indicative of more marked interpersonal and affective deficits in psychopathy, were associated with impaired thematic memory on the Logical Memory test. Intriguingly, Donegan et al (Reference Donegan, Sanislow and Blumberg2003) have demonstrated altered neuronal activity within the amygdala in response to emotional facial expressions in individuals with borderline personality disorder. Therefore, the observed memory impairment might be mediated by dysfunction within association cortices that subserve learning, memory and visuospatial capabilities, and limbic circuits that route emotional information into other forms of cognitive processing.
Acknowledgements
We thank Dr Val Hawes, Psychology Department, and the prison officers on Red-Spur, HMP Whitemoor, as well as the staff at Arnold Lodge RSU. This study was supported by a 2-year grant from the Home Office, UK.








eLetters
No eLetters have been published for this article.