Depressive and anxiety disorders are highly prevalent in the general population, Reference Kessler, McGonagle, Zhao, Nelson, Hughes and Eshleman1 and have an enormous impact on physical, social and occupational functioning. Reference Judd, Akiskal, Zeller, Paulus, Leon and Maser2–Reference Ormel, Petukhova, Chatterji, Aguilar-Gaxiola, Alonso and Angermeyer6 These severe impairments may be long-lasting because depressive and anxiety disorders frequently have a persistent course. Reference Piccinelli and Wilkinson7–Reference Rhebergen, Beekman, De Graaf, Nolen, Spijker and Hoogendijk11 Identification of risk factors that predict unfavourable outcomes may provide important insights into processes involved in the natural course of these disorders and is essential for optimising treatment strategies. Alcohol use disorders (abuse and dependence) are highly prevalent in people with depression and/or anxiety, Reference Burns and Teesson12–Reference Boschloo, Vogelzangs, Smit, Van den Brink, Veltman and Beekman15 and have been suggested to be important predictors of a poor outcome. However, few prospective studies have examined the effects of alcohol use disorders on the natural course of depressive and anxiety disorders, and these have reported conflicting results. For example, people with comorbid alcoholism have a decreased risk of remission of major depressive disorder, Reference Mueller, Lavori, Keller, Swartz, Warshaw and Hasin16 and in addition remission of generalised anxiety disorder is less likely in people with comorbid substance use disorders. Reference Bruce, Yonkers, Otto, Eisen, Weisberg and Pagano17 However, other studies failed to find alcohol use disorders to be significant predictors of the persistence of disorder among people who had depression or anxiety. Reference Rhebergen, Beekman, De Graaf, Nolen, Spijker and Hoogendijk11,Reference Kushner, Sher and Erickson18 These inconsistent findings may be partly explained by these studies’ lack of power owing to small sample sizes (n = 588, n = 473, n = 400 and n = 92 respectively). Reference Rhebergen, Beekman, De Graaf, Nolen, Spijker and Hoogendijk11,Reference Mueller, Lavori, Keller, Swartz, Warshaw and Hasin16–Reference Kushner, Sher and Erickson18 Therefore, we prospectively examined the 2-year course of depressive and/or anxiety disorders in a large sample of participants with current depression and/or anxiety (n = 1369).
Another possible explanation for the inconsistent results is the heterogeneity of alcohol use disorders. Previous studies have shown that alcohol dependence has strong cross-sectional associations with depressive and/or anxiety disorders, whereas alcohol abuse has not. Reference Hasin, Stinson, Ogburn and Grant14,Reference Boschloo, Vogelzangs, Smit, Van den Brink, Veltman and Beekman15 It may, therefore, be important to examine the unique associations of each condition on the natural course of depressive and anxiety disorders. In addition, it may be necessary to take into account the severity of alcohol abuse and dependence, since these conditions have a dimensional aspect. Reference Muthen, Hasin and Wisnicki19–Reference Hasin, Liu, Alderson and Grant21 Consequently, our study not only examined whether the presence of an alcohol use disorder predicts the course of depressive and/or anxiety disorders, but also explored whether this association is conditional on the type of alcohol use disorder (abuse or dependence) or the severity of each condition. In addition, we examined whether found associations might be due to or independent of baseline severity of depressive and/or anxiety disorders, and of psychosocial and treatment factors.
Method
Study sample
Data were derived from the Netherlands Study of Depression and Anxiety (NESDA), an ongoing cohort study aimed at examining the long-term course and consequences of depressive and anxiety disorders in the adult population (aged 18–65 years). A total of 2981 persons were included at the baseline assessment in 2004–7, consisting of a healthy control group, people with a history of depressive or anxiety disorder and people with current depressive and/or anxiety disorder. Participants were recruited from community (19%), primary care (54%) and out-patient mental healthcare services (27%). Community-based participants had previously been identified in a population-based study. Primary care participants were identified through a three-stage screening procedure, involving the 10-item Kessler questionnaire and the Short Form Composite International Diagnostic Interview (CIDI), Reference Kessler, Andrews, Colpe, Hiripi, Mroczek and Normand22,Reference Wittchen, Robins, Cottler, Sartorius, Burke and Regier23 conducted by telephone among a random sample of patients of 65 general practitioners. Mental healthcare participants were recruited consecutively when newly enrolled at one of the 17 participating mental health organisation locations. People with insufficient command of the Dutch language or a primary clinical diagnosis of bipolar disorder, obsessive–compulsive disorder, severe substance use disorder, psychotic disorder or organic psychiatric disorder, as reported by them or their mental health practitioner, were excluded. The research protocol was approved by the ethical committee of participating universities and all participants provided written informed consent. A detailed description of the NESDA study design, sampling procedures and response rates can be found elsewhere. Reference Penninx, Beekman, Smit, Zitman, Nolen and Spinhoven24,Reference Van der Veen, Van der Meer and Penninx25 In our earlier research we examined non-response at the baseline interview: in participants recruited from primary care (the majority), mainly sociodemographic factors – namely younger age and male gender – but not mental health status predicted higher non-response. Reference Van der Veen, Van der Meer and Penninx25 Similar observations were found in the community and mental healthcare settings. Reference Penninx, Beekman, Smit, Zitman, Nolen and Spinhoven24 This suggests that our overall sample is generalisable to the sample from which it was recruited, although younger men may be slightly underrepresented.
The baseline assessment included a face-to-face assessment of demographic and personal characteristics as well as a standardised diagnostic psychiatric interview among all 2981 NESDA participants. After 2 years, another face-to-face assessment including the same standardised diagnostic psychiatric interview was conducted, with a response of 87.1% (n = 2596; see Lamers et al also for sociodemographic and psychiatric determinants of non-response). Reference Lamers, Hoogendoorn, Smit, Van Dyck, Zitman and Nolen26 For this study we selected all participants with major depressive disorder, dysthymia, social phobia, panic disorder and/or generalised anxiety disorder that was present within the 6 months prior to the baseline assessment (n = 1641). Of these, 1369 persons (83.4%) had complete data at the 2-year follow-up assessment and formed the sample for the analyses presented here. The non-response group was significantly younger (P = 0.03), less educated (P<0.001) and more often had a current depressive disorder (P = 0.003) at baseline compared with the responder group, whereas gender (P = 0.16), alcohol abuse/dependence status (P = 0.74) and current anxiety disorder (P = 0.07) were not associated with failure to respond.
Measures
Depressive and anxiety disorders
Diagnoses of psychiatric disorders according to DSM-IV criteria 27 were established with the CIDI version 2.1, administered by specially trained research staff. Reference Wittchen, Robins, Cottler, Sartorius, Burke and Regier23 The CIDI has shown high interrater and test–retest reliability and high validity for depressive and anxiety disorders. Reference Wittchen, Robins, Cottler, Sartorius, Burke and Regier23 To examine the course of depressive and/or anxiety disorders, we considered the persistence of the disorder as well as the course of symptoms.
Persistence. Participants were considered to have persistent disorder if they met DSM-IV criteria for a depressive and/or anxiety disorder in the 6 months prior to the 2-year follow-up assessment.
Symptoms. To assess the robustness of findings regarding the persistence of these disorders, the course of symptoms during the 2-year follow-up was used as a secondary outcome. Depressive symptoms were defined as the total score on the 30-item self-report Inventory of Depressive Symptomatology (IDS); Reference Rush, Gullion, Basco, Jarret and Trivedi28 anxiety symptoms were defined as the total score on the 21-item self-report Beck Anxiety Inventory (BAI). Reference Beck, Epstein, Brown and Steer29 Both questionnaires related to symptoms in the week prior to assessment. In addition to the baseline and 2-year follow-up interviews, the IDS and BAI were also administered at an intermittent 1-year follow-up assessment.
Alcohol use disorder
Diagnoses of alcohol use disorder (DSM-IV criteria) were established at baseline with the CIDI, which is a reliable and valid instrument for assessing alcohol dependence, but with more variable results for alcohol abuse. Reference Cottler, Grant, Blaine, Mavreas, Pull and Hasin30 A DSM-IV diagnosis of alcohol abuse requires one or more of the four abuse criteria to be met, whereas a diagnosis of alcohol dependence requires three or more of the seven dependence criteria. The CIDI hierarchy criteria for diagnosing DSM-IV alcohol use disorders exclude the possibility of a diagnosis of alcohol abuse when a lifetime diagnosis of alcohol dependence is present. A distinction was made between alcohol use disorders that were present in the 6 months prior to the baseline assessment (current disorder) v. before this period (remitted disorder). Various alcohol use disorder measures were assessed to examine the exact effects of this disorder on the course of depressive and/or anxiety disorders.
Alcohol use disorder status. Alcohol use disorder status – no lifetime alcohol use disorder (reference category), remitted disorder or current disorder – was used to examine whether these categories predicted the course of depressive and/or anxiety disorders.
Alcohol abuse/dependence status. To determine whether DSM-IV alcohol abuse and dependence have differential effects on the course of depressive and/or anxiety disorders, we distinguished between participants with no lifetime alcohol use disorder (reference category), remitted alcohol abuse, current abuse, remitted dependence and current dependence.
Alcohol abuse/dependence severity. The severity of current alcohol abuse and dependence diagnoses was defined by the number of criteria met, i.e. one to four criteria for alcohol abuse and three to seven criteria for dependence. Previous studies have shown that alcohol abuse and dependence have a dimensional aspect, Reference Muthen, Hasin and Wisnicki19,Reference Harford and Muthen20 and that the count of alcohol dependence criteria constitutes a linear dimension of alcohol dependence severity. Reference Hasin, Liu, Alderson and Grant21
Covariates
Basic covariates comprised gender, age (in years) and smoking status (never smoked, former smoker, current smoker) at baseline. To examine the role of baseline severity of depressive and/or anxiety disorders, psychosocial factors and treatment factors in the association between alcohol use disorders and the course of depressive and/or anxiety disorders, analyses were additionally adjusted for the following covariates.
Severity of depression and anxiety
Severity of depression and anxiety was defined as the severity of symptoms at baseline assessed with the IDS and BAI respectively.
Psychosocial factors
Psychosocial factors included education (in years), employment status (no/yes) and partner status (no/yes) at the baseline assessment.
Treatment factors
Treatment factors consisted of frequent use of antidepressants, frequent use of benzodiazepines and psychological treatment at the baseline interview and/or during follow-up. Frequent use of psychoactive medication was assessed by drug container inspection of medication used in the month before the baseline or 2-year follow-up assessment, classified according to the World Health Organization Anatomical Therapeutic Chemical (ATC) classification, 31 and was considered to be present when the medication was taken daily or on at least half of the days. We distinguished between use of antidepressants – selective serotonin reuptake inhibitors (ATC code N06AB), tricyclic antidepressants (N06AA) and other antidepressants (N06AF/N06AX) – and use of benzodiazepines (ATC codes N03AE, N05BA, N05CD and N05CF). The receipt of psychological treatment (formal psychotherapy, counselling or skills training) in the 6 months prior to the baseline or 2-year follow-up assessment was based on self-reported information.
Statistical analysis
Analyses were conducted using SPSS version 15.0 for Windows. First, baseline characteristics of the sample were summarised using descriptive statistics. To examine whether alcohol use disorder status (no lifetime disorder, remitted disorder or current disorder) predicted the presence of depressive and/or anxiety disorders at the 2-year follow-up, logistic regression analyses were used. We then focused on the type of alcohol use disorder by examining the associations across alcohol abuse/dependence status: no lifetime alcohol use disorder (reference category), remitted alcohol abuse, current abuse, remitted dependence and current dependence.
We further explored the relationships of current alcohol abuse and dependence with the presence of depressive and/or anxiety disorders at the 2-year follow-up by focusing on the severity of the current alcohol use disorder. A graph was plotted based on logistic regression analyses with variables representing all separate levels of abuse severity (one to four criteria) or dependence severity (three to seven criteria) as predictors. We used the Wald statistic to test whether a model based on alcohol abuse or dependence severity better predicted the presence of depressive and/or anxiety disorders at 2-year follow-up than the model based on DSM-IV alcohol use disorder diagnoses, an analytic method used previously by others. Reference Hasin, Liu, Alderson and Grant21 All analyses were adjusted for gender, age and smoking status.
To test the robustness of our findings, we additionally examined the course of depressive symptoms as well as anxiety symptoms using linear mixed models (LMM) analyses. Alcohol abuse/dependence status, time of assessment (baseline, 1-year follow-up, 2-year follow-up) and covariates were entered as fixed factors, participants were treated as a random effect and a random intercept was estimated. To determine whether groups based on alcohol abuse/dependence status differed in their overall levels of depressive and anxiety symptoms, we considered the direct effects of alcohol use disorder groups. In addition, we added a group × time interaction term to examine whether the trajectories of depressive and anxiety symptoms differed across the groups. Similarly, we used LMM analyses to examine whether the alternative model based on abuse/dependence severity predicted the course of depressive and anxiety disorders. To examine the role of other factors in the association between alcohol use disorders and the persistence of depressive and/or anxiety disorders, analyses were additionally adjusted for covariates involving baseline severity of depression and anxiety (IDS and BAI total scores), psychosocial factors (education, employment status and partner status) and treatment factors (use of antidepressants, use of benzodiazepines and psychological treatment).
Results
Our sample (n = 1369) had a mean age of 41.3 years (s.d. = 12.3) and two-thirds (66.3%) were women; 935 persons (68.3%) had never had an alcohol use disorder, 307 (22.4%) had a remitted alcohol use disorder and 127 (9.3%) had a current alcohol use disorder (Table 1).
Alcohol use disorder status
We examined whether alcohol use disorder status predicted the presence of depressive and/or anxiety disorders after 2-year follow-up, adjusted for basic covariates. Neither remitted nor current alcohol use disorder was a significant predictor of an unfavourable course of depressive disorder and/or anxiety disorder compared with those with no lifetime alcohol use disorder (Table 2).
Type of alcohol use disorder
We tested whether alcohol abuse and dependence had differential effects on the course of depressive and/or anxiety disorders, adjusted for basic covariates (Table 2). Participants with depression and/or anxiety with remitted alcohol dependence (persistence: 62.4%; odds ratio (OR) = 1.42, 95% CI 1.02–1.97, P = 0.04) and those with current alcohol dependence (persistence: 66.7%; OR = 1.69, 95% CI 1.04–2.75, P = 0.04) had a significantly
TABLE 1 Sample characteristics at baseline (n = 1369)

| Basic covariates | |
|---|---|
| Gender, female, n (%) | 907 (66.3) |
| Age, years: mean (s.d.) | 41.3 (12.3) |
| Smoking, n (%) | |
| Non-smoker | 363 (26.5) |
| Former smoker | 430 (31.4) |
| Current smoker | 576 (42.1) |
| Severity of depression and anxiety | |
| Depressive symptoms (IDS total score): mean (s.d.) | 28.9 (12.2) |
| Anxiety symptoms (BAI total score): mean (s.d.) | 16.7 (10.4) |
| Psychosocial factors | |
| Education, years: mean (s.d.) | 11.9 (3.3) |
| Employment (yes), n (%) | 758 (55.4) |
| Partner (yes), n (%) | 890 (65.0) |
| Treatment, n (%) | |
| Use of antidepressants (yes) | 632 (46.2) |
| Use of benzodiazepines (yes) | 239 (17.5) |
| Psychological treatment (yes) | 915 (66.8) |
| AUD measures, n (%) | |
| AUD status | |
| No lifetime AUD | 935 (68.3) |
| Remitted AUD | 307 (22.4) |
| Current AUD | 127 (9.3) |
| AA/AD status | |
| No lifetime AUD | 935 (68.3) |
| Remitted AA | 113 (8.3) |
| Current AA | 46 (3.4) |
| Remitted AD | 194 (14.2) |
| Current AD | 81 (5.9) |
| Number of current AA criteria, n (%) | |
| One | 44 (3.2) |
| Two | 2 (0.1) |
| Three | 0 (0.0) |
| Four | 0 (0.0) |
| Number of current AD criteria, n (%) | |
| Three | 26 (1.9) |
| Four | 22 (1.6) |
| Five | 13 (0.9) |
| Six | 12 (0.9) |
| Seven | 8 (0.6) |
AA, alcohol abuse; AD, alcohol dependence; AUD, alcohol use disorder; BAI, Beck Anxiety Inventory; IDS, Inventory of Depressive Symptomatology.
TABLE 2 Alcohol use disorder measures predicting the persistence of depressive and/or anxiety disorder at 2-year follow-up
| Persistence of depressive/anxiety disorder | |||
|---|---|---|---|
| Baseline AUD measure | Rate, % | OR a (95% CI) | P |
| AUD status | |||
| No lifetime AUD | 53.2 | Reference | |
| Remitted AUD | 58.3 | 1.21 (0.92–1.60) | 0.17 |
| Current AUD | 59.1 | 1.27 (0.86–1.86) | 0.23 |
| AA/AD status | |||
| No lifetime AUD | 53.2 | Reference | |
| Remitted AA | 51.3 | 0.94 (0.63–1.40) | 0.75 |
| Current AA | 45.7 | 0.79 (0.43–1.45) | 0.45 |
| Remitted AD | 62.4 | 1.42 (1.02–1.97) | 0.04 |
| Current AD | 66.7 | 1.69 (1.04–2.75) | 0.04 |
| AD severity | |||
| No lifetime AUD | 53.2 | Reference | |
| Moderate current AD (3–5 criteria) | 57.4 | 1.11 (0.65–1.89) | 0.69 |
| Severe current AD (6 or 7 criteria) | 95.0 | 17.15 (2.27–129.51) | 0.006 |
AA, alcohol abuse; AD, alcohol dependence; AUD, alcohol use disorder; OR, odds ratio.
a Based on logistic regression analyses, adjusted for basic covariates (gender, age and smoking status).
increased risk of having a persistent depressive and/or anxiety disorder at the 2-year follow-up compared with participants with no lifetime alcohol use disorder (persistence: 53.2%). In contrast, neither remitted nor current alcohol abuse significantly predicted the presence of depressive and/or anxiety disorders after 2 years.
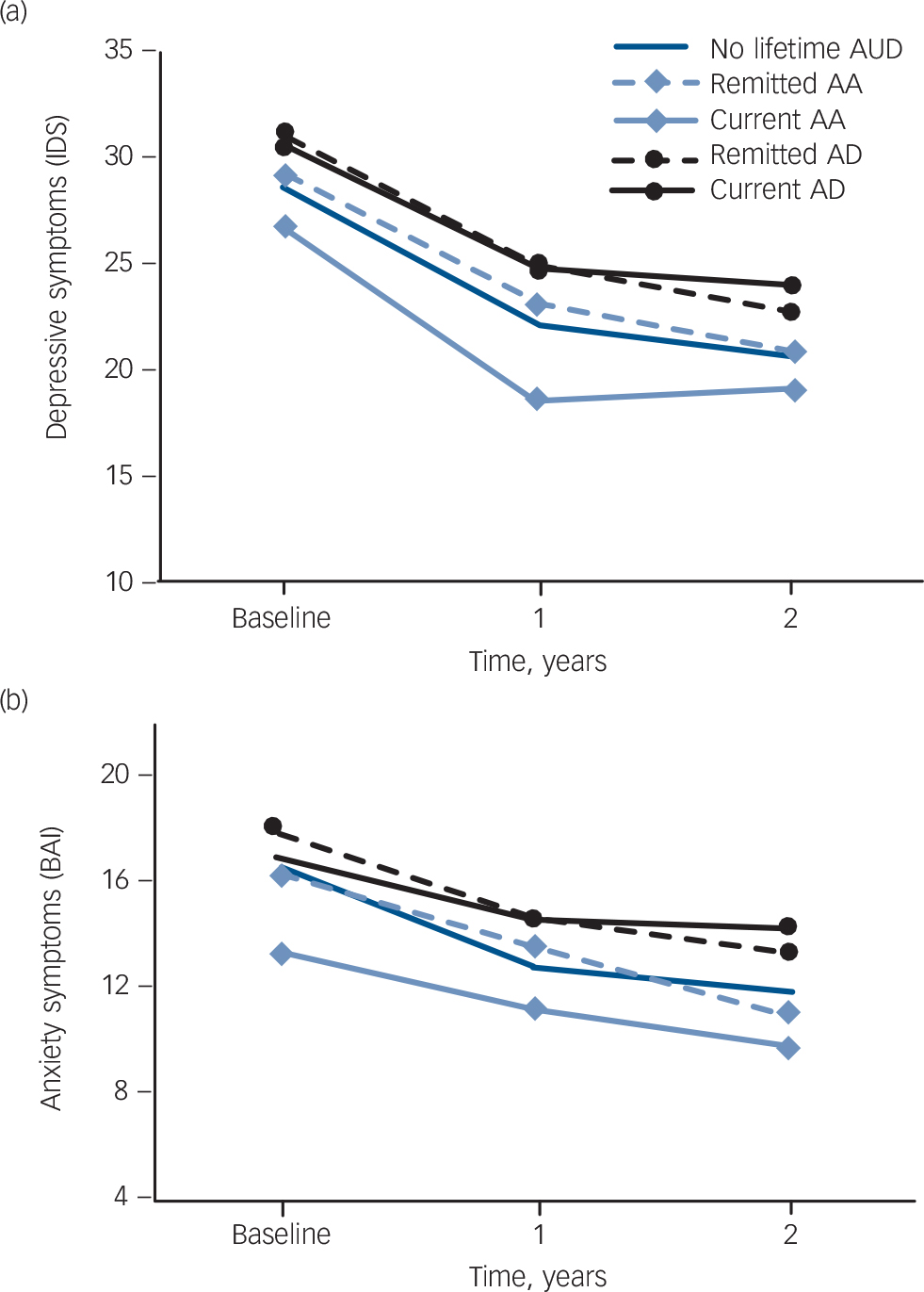
Fig. 1 Alcohol abuse and dependence status predicting the course of (a) depressive symptoms and (b) anxiety symptoms.
Based on linear mixed model analyses, adjusted for basic covariates (gender, age and smoking status). Probability values are given in Table 3. AA, alcohol abuse; AD, alcohol dependence; AUD, alcohol use disorder; BAI, Beck Anxiety Inventory; IDS, Inventory of Depressive Symptomatology.
We tested the robustness of these findings with LMM analyses adjusted for basic covariates (Fig. 1). Over the entire follow-up period, participants with remitted and current alcohol dependence had significantly higher overall levels of depressive symptoms and a trend was found for anxiety symptoms (see Table 3 for probability values), with similar course trajectories over time (P≥0.10 for all interactions remitted dependence ×time or current dependence ×time), compared with participants with no lifetime alcohol use disorder. Neither the overall levels nor the course trajectories of depressive and anxiety symptoms were significantly worse for people with remitted or current alcohol abuse.
Severity of alcohol abuse and dependence
A third aim of our study was to examine whether the associations of current alcohol abuse and dependence with the course of depressive and/or anxiety disorders were conditional on the severity of each condition. Analyses of alcohol abuse severity appeared to be impossible, since of the 46 participants in the current alcohol abuse group, 44 met only one DSM-IV abuse criterion (see Table 1), so further analyses were restricted to the severity of current alcohol dependence. A graph of the association between the number of current alcohol dependence criteria and the presence of depressive and/or anxiety disorders at the 2-year follow-up (Fig. 2) indicated that this association was conditional on the severity of dependence. Only people meeting six or seven alcohol dependence criteria, and not those meeting three, four or five criteria, were at an increased risk. To test this directly, we
TABLE 3 Probability values for prediction of course of symptoms by alcohol abuse and dependence status (see Fig. 1)
| Depressive symptoms | Anxiety symptoms | |||
|---|---|---|---|---|
| Direct effect | Time interaction | Direct effect | Time interaction | |
| P | P | P | P | |
| Remitted AA | 0.80 | 0.91 | 0.70 | 0.26 |
| Current AA | 0.03 | 0.25 | 0.02 | 0.24 |
| Remitted AD | 0.02 | 0.91 | 0.07 | 0.67 |
| Current AD | 0.04 | 0.54 | 0.18 | 0.10 |
AA, alcohol abuse; AD, alcohol dependence.
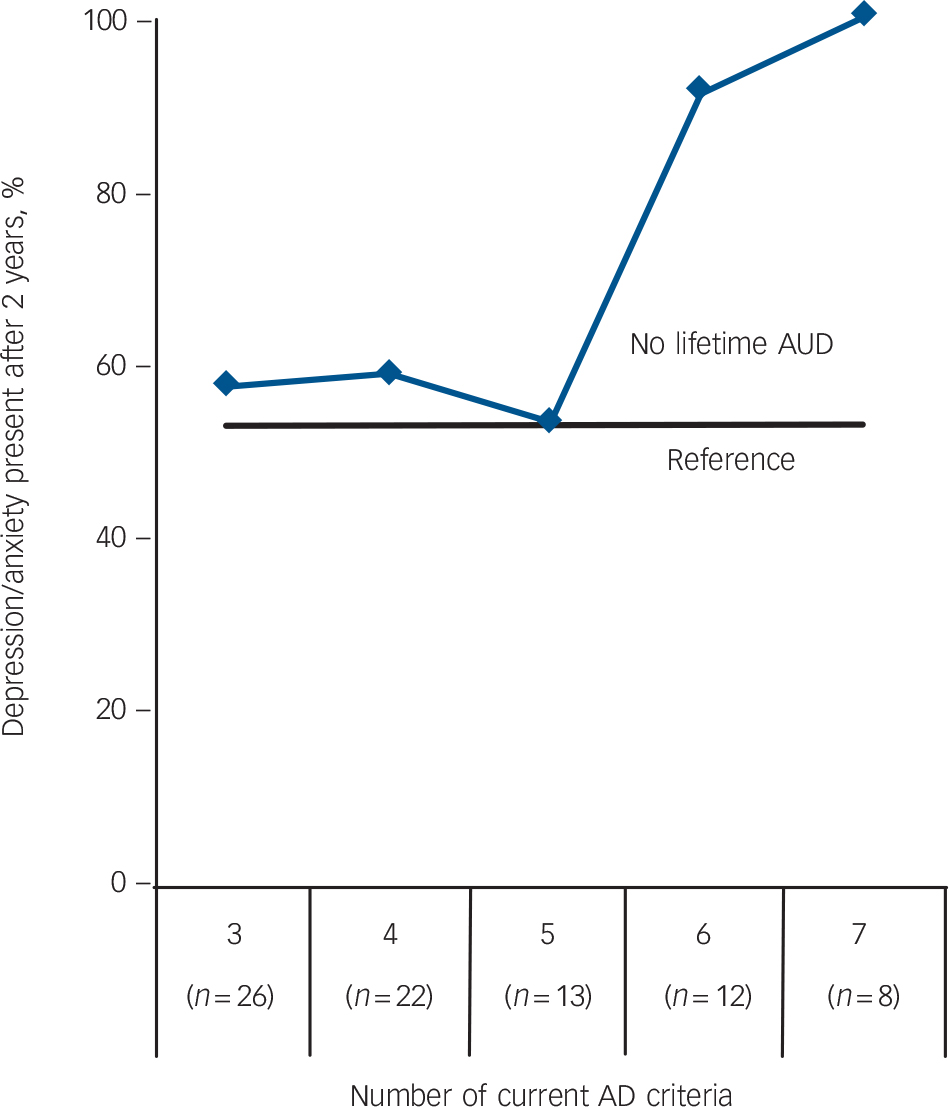
Fig. 2 Number of current alcohol dependence criteria predicting the persistence of depressive and/or anxiety disorder at 2-year follow-up. AD, alcohol dependence; AUD, alcohol use disorder.
used a model distinguishing no lifetime alcohol use disorder, ‘moderate’ current alcohol dependence (meeting three to five criteria) and ‘severe’ current alcohol dependence (six or seven criteria). This two-level model explained the relationship with the persistence of depressive and/or anxiety disorders better than the original DSM-IV model which made no distinction based on severity of alcohol dependence (χ2 = 7.10, d.f. = 1, P = 0.008). Additional analyses, taking moderate alcohol dependence as the reference group, showed a significant difference between people with severe alcohol dependence and those with moderate dependence (unadjusted OR = 14.11, 95% CI 1.77–112.29, P = 0.01), indicating that severe alcohol dependence had a significantly stronger effect on the persistence of depressive and/or anxiety disorders.
Table 2 shows that 95.0% of participants with severe alcohol dependence still had a depressive and/or anxiety disorder after the 2-year follow-up, which was significantly higher than in those with no lifetime alcohol use disorder (basic adjustment: OR = 17.15, 95% CI 2.27–129.51, P = 0.006). No significant association was found for participants with moderate alcohol
TABLE 4 Probability values for persistence of depressive and/or anxiety disorder predicted by severity of current alcohol dependence (see Fig. 3)
| Depressive symptoms | Anxiety symptoms | |||
|---|---|---|---|---|
| Direct effect | Time interaction | Direct effect | Time interaction | |
| P | P | P | P | |
| Moderate current AD (3–5 criteria) | 0.33 | 0.89 | 0.63 | 0.61 |
| Severe current AD (6 or 7 criteria) | 0.01 | 0.02 | 0.06 | 0.02 |
AD, alcohol dependence.
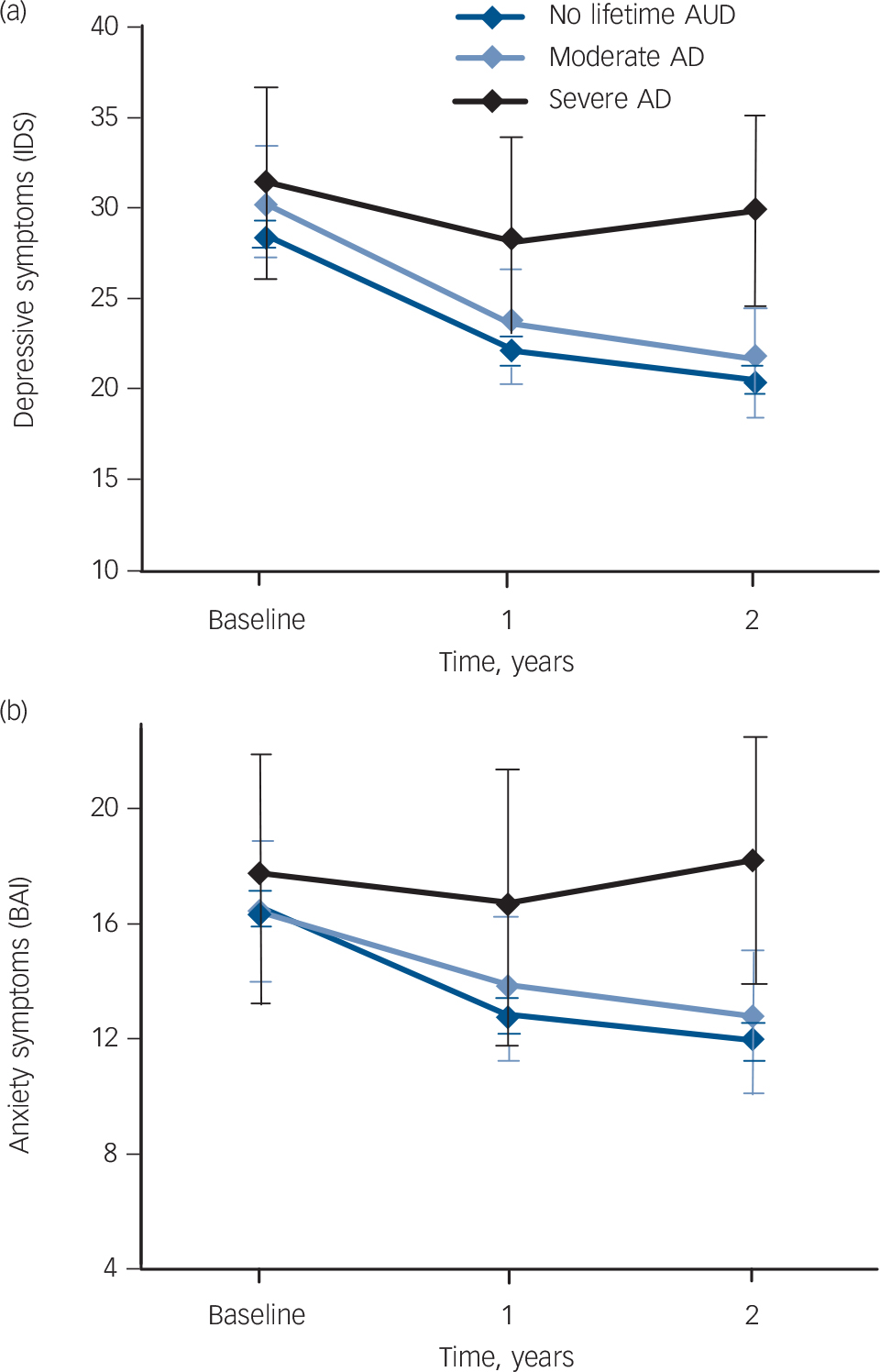
Fig. 3 Moderate and severe current alcohol dependence predicting the course of (a) depressive symptoms and (b) anxiety symptoms.
Based on linear mixed model analyses, adjusted for basic covariates (gender, age, and smoking status). Probability values are given in Table 4. AD, alcohol dependence; AUD, alcohol use disorder; BAI, Beck Anxiety Inventory; IDS, Inventory of Depressive Symptomatology.
dependence (basic adjustment: OR = 1.11, 95% CI 0.65–1.89, P = 0.69). To verify our findings regarding the persistence of depressive and/or anxiety disorders at 2 years follow-up, we additionally tested whether moderate alcohol dependence and severe alcohol dependence predicted the course of depressive and anxiety symptoms using LMM analyses (Fig. 3). These results showed that the overall levels of depressive and anxiety symptoms were higher for those with severe current alcohol dependence and that, in addition, the course trajectories for depressive and anxiety symptoms were poorer compared with those with no lifetime alcohol use disorder (P values are summarised in Table 4). No significant difference in the course of depressive or anxiety symptoms was found for moderate alcohol dependence.
Role of other factors
To explore the role of other factors in the association between severity of alcohol dependence and the persistence of depressive and/or anxiety disorders, the analyses were additionally adjusted for baseline severity of depression and anxiety (Table 5, second column), psychosocial factors (third column) and treatment factors (fourth column). In the analyses adjusted for basic covariates, severe current alcohol dependence was a significant predictor of the persistence of depressive and/or anxiety disorders (OR = 17.15, 95% CI 2.27–129.51, P = 0.006). Although the association was slightly decreased after additional adjustment for severity of depressive and anxiety symptoms (OR = 15.88, 95% CI 2.09–120.87, P = 0.008), psychosocial factors (OR = 15.22, 95% CI 1.99–116.16, P = 0.009) and treatment factors (OR = 13.50, 95% CI 1.77–102.96, P = 0.01), the association remained significant (Table 5).
Heterogeneity of depressive and anxiety disorders
At the baseline assessment, 60.4% of all the participants who had current depression also had a current anxiety disorder. Similarly, 57.4% of participants with current anxiety also had a current depressive disorder. Given the high comorbidity of depressive and anxiety disorders, previous analyses were based on a mixed group of people with a depressive and/or anxiety disorder. To assess the robustness of our findings, a set of sensitivity analyses was conducted. First, we tested whether alcohol abuse/dependence status predicted the presence of a depressive and/or anxiety
TABLE 5 Alcohol use disorder measures predicting the persistence of depressive and/or anxiety disorders at 2-year follow-up
| Persistence of depressive/anxiety disorder after 2 years | ||||||||
|---|---|---|---|---|---|---|---|---|
| Basic adjustment a | Additionally adjusted for symptom severity b | Additionally adjusted for psychosocial factors c | Additionally adjusted for treatment factors d | |||||
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |
| AD severity | ||||||||
| No lifetime AUD | Reference | Reference | Reference | Reference | ||||
| Moderate current AD | 1.11 (0.65–1.89) | 0.71 | 1.03 (0.59–1.80) | 0.92 | 1.00 (0.57–1.75) | 1.00 | 0.97 (0.55–1.72) | 0.93 |
| Severe current AD | 17.15 (2.27–129.51) | 0.006 | 15.88 (2.09–120.87) | 0.008 | 15.22 (1.99–116.16) | 0.009 | 13.50 (1.77–102.96) | 0.01 |
| Basic covariates | ||||||||
| Gender (female) | 1.11 (0.83–1.48) | 0.49 | 1.13 (0.83–1.53) | 0.43 | 1.12 (0.83–1.52) | 0.46 | 1.12 (0.82–1.52) | 0.48 |
| Age | 1.01 (1.00–1.02) | 0.01 | 1.01 (1.00–1.02) | 0.08 | 1.01 (1.00–1.02) | 0.08 | 1.01 (1.00–1.03) | 0.02 |
| Smoking status | ||||||||
| Non-smoker | Reference | Reference | Reference | Reference | ||||
| Former smoker | 1.36 (0.98–1.88) | 0.06 | 1.21 (0.86–1.70) | 0.27 | 1.19 (0.84–1.67) | 0.33 | 1.17 (0.83–1.65) | 0.37 |
| Current smoker | 1.65 (1.21–2.25) | 0.002 | 1.43 (1.03–1.98) | 0.03 | 1.42 (1.02–1.98) | 0.04 | 1.43 (1.02–1.99) | 0.04 |
| Severity of depression and anxiety | ||||||||
| Depressive symptoms (IDS score) | 1.05 (1.04–1.07) | <0.001 | 1.05 (1.03–1.07) | <0.001 | 1.05 (1.03–1.06) | <0.001 | ||
| Anxiety symptoms (BAI score) | 1.01 (0.99–1.02) | 0.37 | 1.01 (0.99–1.03) | 0.32 | 1.01 (0.99–1.02) | 0.38 | ||
| Psychosocial factors | ||||||||
| Education in years | 1.01 (0.97–1.06) | 0.53 | 1.00 (0.96–1.05) | 0.84 | ||||
| Employment (yes) | 0.90 (0.69–1.18) | 0.46 | 0.91 (0.69–1.20) | 0.51 | ||||
| Partner (yes) | 0.91 (0.69–1.21) | 0.53 | 0.91 (0.68–1.21) | 0.51 | ||||
| Treatment factors | ||||||||
| Use of antidepressants (yes) | 1.00 (0.76–1.32) | 1.00 | ||||||
| Use of benzodiazepines (yes) | 0.91 (0.64–1.30) | 0.62 | ||||||
| Psychological treatment (yes) | 1.63 (1.20–2.20) | 0.002 | ||||||
AD, alcohol dependence; AUD, alcohol use disorder; BAI, Beck Anxiety Inventory; IDS, Inventory of Depressive Symptomatology; OR, odds ratio.
a Adjusted for basic covariates (gender, age, smoking status).
b Adjusted for basic covariates and depressive/anxiety symptoms (baseline IDS and BAI scores).
c Adjusted for basic covariates, depressive/anxiety symptoms and psychosocial factors (education, employment status, partner status).
d Adjusted for basic covariates, depressive/anxiety symptoms, psychosocial factors and treatment factors (use of antidepressants, use of benzodiazepines and psychological treatment).
disorder at the 2-year follow-up in a subsample of participants with depressive disorders (n = 946) v. those with anxiety disorders (n = 994). We found consistent associations for remitted alcohol abuse (unadjusted OR = 0.69, P = 0.12 v. unadjusted OR = 1.06, P = 0.80), current alcohol abuse (unadjusted OR = 0.58, P = 0.14 v. unadjusted OR = 0.74, P = 0.43), remitted alcohol dependence (unadjusted OR = 1.26, P = 0.25 v. unadjusted OR = 1.67, P = 0.04) and current alcohol dependence (unadjusted OR = 1.47, P = 0.16 v. unadjusted OR = 1.75, P = 0.05). In addition, severe current alcohol dependence was a significant predictor in participants with depressive disorders (unadjusted OR = 11.26, P = 0.02) and anxiety disorders (unadjusted OR = 10.29, P = 0.03), whereas moderate current alcohol dependence was not significant in either subsample (unadjusted OR = 0.99, P = 0.96 v. unadjusted OR = 1.28, P = 0.43).
Discussion
To our knowledge this is the first study showing that the association between alcohol use disorders and the course of depressive and/or anxiety disorders is conditional on the type (abuse or dependence) and severity of the alcohol use disorder. Our results show that current dependence as well as a history of alcohol dependence, but not abuse, predicts an unfavourable course of depressive and/or anxiety disorders. People with severe current alcohol dependence (six or seven alcohol dependence criteria) have an especially poor course since 95% have a persistent depressive and/or anxiety disorder, in contrast to 53% of those with no lifetime alcohol use disorder. In addition, depressive and anxiety symptoms remain significantly higher in people with severe current alcohol dependence, whereas they generally improve in those with no lifetime alcohol use disorder. The inconsistent findings of previous studies reporting that alcohol use disorders predicted an unfavourable course of depressive or anxiety disorders, Reference Mueller, Lavori, Keller, Swartz, Warshaw and Hasin16,Reference Bruce, Yonkers, Otto, Eisen, Weisberg and Pagano17 or did not, Reference Rhebergen, Beekman, De Graaf, Nolen, Spijker and Hoogendijk11,Reference Kushner, Sher and Erickson18 may therefore be explained by the differential effects of alcohol use disorders depending on the type and severity.
Possible mechanisms
Our study further demonstrated that severe current alcohol dependence predicted the persistence of depressive and/or anxiety disorders, even after taking into account the effects of other risk factors. Although baseline severity of depressive and anxiety symptoms, psychosocial factors and treatment partly explained the association, severe alcohol dependence remained a strong predictor. Previous studies have proposed that interpersonal and social problems, as characteristics of alcohol use disorders, cause the persistence of depressive and/or anxiety disorders. Reference Swendsen and Merikangas32 This may be supported by our finding that the risk of persistent depressive and/or anxiety disorders was increased only in people with severe alcohol dependence. Previous studies have found that the alcohol dependence criterion involving interpersonal and social problems (criterion 6: giving up or reducing occupational, social and/or recreational activities to drink) is one of the most severe criteria and is mainly present in those with severe alcohol use disorders. Reference Dawson, Saha and Grant33 This was supported by some additional analyses showing that this specific criterion was present in 85% of participants with severe alcohol dependence v. 15% of those with moderate alcohol dependence. Similarly, DSM-IV alcohol abuse criteria involving interpersonal and social problems (criterion 1: failure to fulfil major role obligations; criterion 4: persistent social or interpersonal problems) are more likely in people with severe alcohol use disorders; Reference Mechanic34 the prevalence rates of alcohol abuse criteria 1 and 4 in participants with severe alcohol dependence in our sample were 60% and 100% respectively. Although factors involving general psychosocial status (level of education, employment status and partner status) did not explain the association between severe current alcohol dependence and the persistence of depressive and/or anxiety disorders, factors involving the quality of interpersonal and social life (giving up activities, failure to fulfil roles, and persistent social or interpersonal problems), as characteristics of severe alcohol dependence, may have a more important role. Further research is needed to unravel the exact mechanisms through which (severe) current alcohol dependence leads to an unfavourable course of depressive and/or anxiety disorders.
Clinical implications
Our finding that (severe) current alcohol dependence leads to an unfavourable course of depressive and/or anxiety disorders stresses the importance of integrating addiction treatment in general mental health services to optimise treatment for patients with depression and/or anxiety with comorbid alcohol dependence. This has the potential to be highly effective, since 95% of our sample with severe current alcohol dependence had a persistent depressive and/or anxiety disorder after 2 years. Integrated care has also been advocated by others as a means of enhancing communication between care providers, reducing stigma and avoiding artificial separation of various psychiatric problems that otherwise could result in substandard care. Reference Mechanic34,Reference Bartels, Coakley, Zubritsky, Ware, Miles and Areán35 To identify individuals with alcohol dependence, time-efficient screening instruments such as the Alcohol Use Disorder Identification Test (AUDIT) could be helpful. Reference Saunders, Aasland, Babor, Fuente and Grant36 This test has been shown to be accurate in detecting alcohol dependence in individuals with depression and anxiety, Reference Boschloo, Vogelzangs, Smit, Van den Brink, Veltman and Beekman37 and therefore may be effective in identifying patients with depression and/or anxiety who need additional addiction treatment.
Alcohol use disorder in DSM-5
We showed that alcohol abuse, unlike dependence, does not predict the course of depressive and/or anxiety disorders. A similar pattern of results was found in other studies reporting that alcohol abuse was not more prevalent in people with anxiety and/or depression, in contrast to dependence. Reference Hasin, Stinson, Ogburn and Grant14,Reference Boschloo, Vogelzangs, Smit, Van den Brink, Veltman and Beekman15 Since others found that the reliability and validity were excellent for a DSM-IV diagnosis of alcohol dependence but not for a diagnosis of alcohol abuse, Reference Beck, Epstein, Brown and Steer29,Reference Saunders, Aasland, Babor, Fuente and Grant36 this raises the question whether alcohol abuse as diagnosed by DSM-IV criteria (i.e. hierarchically assessed based on one or more criteria) should be considered a genuine psychiatric disorder. This may be supported by our finding that of the 46 persons with current alcohol abuse in our sample, all but 2 met only one criterion. Although the reliability and validity of a diagnosis of alcohol abuse were low, studies have shown that the individual criteria of alcohol dependence as well as abuse are reliable and valid, and represent a single latent dimension with dependence and abuse criteria interspersed across an underlying severity spectrum. Reference Boschloo, Vogelzangs, Smit, Van den Brink, Veltman and Beekman37–Reference Saha, Chou and Grant39 Together, these findings have motivated the DSM-5 work group to propose one diagnosis of an alcohol use disorder that is based on alcohol abuse as well as dependence criteria, with different levels of severity. The importance of using severity indicators rather than categorical diagnoses is also highlighted by our finding that only those with severe alcohol dependence (meeting six or seven criteria) and not those with moderate alcohol dependence (meeting three to five criteria) have an unfavourable course of depressive and/or anxiety disorders. Severity of disorder may therefore be more informative than pure diagnosis, as has already been indicated by others. Reference Boschloo, Vogelzangs, Smit, Van den Brink, Veltman and Beekman37–Reference Boschloo, Van den Brink, Penninx, Wall and Hasin41
Strengths and limitations
Methodological strengths of our study include that we prospectively examined whether DSM-IV alcohol abuse and alcohol dependence predicted the course of disorders in a large sample of people with a DSM-IV diagnosis of a depressive and/or anxiety disorder. This sample consisting of 1369 persons was much larger than the 92 to 588 persons who participated in previous studies on this topic. Reference Rhebergen, Beekman, De Graaf, Nolen, Spijker and Hoogendijk11,Reference Mueller, Lavori, Keller, Swartz, Warshaw and Hasin16–Reference Kushner, Sher and Erickson18 In addition, our main findings regarding the persistence of depressive and/or anxiety disorders were all supported by additional analyses on the course of depressive and anxiety symptoms. Despite the large sample size, a limitation of our study is the small number of participants with severe alcohol use disorders. In addition, people with a primary diagnosis of a severe substance use disorder were not included in this study. Therefore, reported associations between alcohol use disorders and the course of depressive and/or anxiety disorders are likely to be underestimates and may not be generalised to severe alcohol use disorders. Studies in clinical samples of patients with severe alcohol use disorders, with or without comorbid substance use disorders, should provide important additional information. Although consistent findings were found for participants with a depressive disorder v. an anxiety disorder, further research is needed to assess associations between alcohol use disorders and specific depressive and anxiety disorders.
Concluding remarks
The effects of comorbid alcohol use disorders on the course of depressive and/or anxiety disorders are conditional on the type as well as severity of the former disorders. Alcohol dependence, especially severe current dependence, predicts an unfavourable course of depressive and/or anxiety disorders, whereas alcohol abuse does not. Of the group with severe current alcohol dependence, 95% had a persistent depressive and/or anxiety disorder without symptomatic improvement. This stresses the importance of integrating addiction treatment in general mental health services as a means of optimising treatment outcomes for patients with depression and/or anxiety.
Funding
The infrastructure for The Netherlands Study of Depression and Anxiety (http://www.nesda.nl) is funded through the Geestkracht programme of The Netherlands Organisation for Health Research and Development (Zon-Mw, grant number ) and is supported by participating universities and mental healthcare organisations: VU University Medical Centre, GGZ inGeest, Arkin, Leiden University Medical Centre, GGZ Rivierduinen, University Medical Centre Groningen, Lentis, GGZ Friesland, GGZ Drenthe, Scientific Institute for Quality of Health Care (IQ Healthcare), Netherlands Institute for Health Services Research (NIVEL) and Netherlands Institute of Mental Health and Addiction (Trimbos). Data analyses were supported by grant from The Netherlands Organisation for Health Research and Development.











eLetters
No eLetters have been published for this article.