In both younger and older adults, anxiety disorders are the most common form of psychiatric illness. Reference Byers, Yaffe, Covinsky, Friedman and Bruce1,Reference Kessler, Berglund, Demler, Jin, Merikangas and Walters2 The consequences of anxiety disorders in later life can be severe, including increased risk of cardiovascular disease, Reference Roest, Martens, de Jong and Denollet3 other serious medical illness Reference El-Gabalawy, Mackenzie, Shooshtari and Sareen4 and cognitive impairment. Reference Beaudreau and O'Hara5 Although treatment for anxiety disorders is generally effective, some data suggest that older people respond less well than younger people do. Reference Hendriks, Oude Voshaar, Keijsers, Hoogduin and van Balkom6-Reference Covin, Ouimet, Seeds and Dozois12 Most studies of anxiety treatment in ‘adult’ populations have excluded elderly individuals, however, precluding a direct comparison of treatment outcome across age groups within a single trial. In the present investigation, we examine age differences in outcomes from the Coordinated Anxiety Learning and Management (CALM) study (clinicaltrials. gov identifier: NCT00347269), an effectiveness trial comparing usual care to a collaborative care intervention for primary care patients with panic disorder, generalised anxiety disorder, post-traumatic stress disorder (PTSD) or social anxiety disorder. Reference Roy-Byrne, Craske, Sullivan, Rose, Edlund and Lang13 We hypothesised that older adults would show a poorer response to the intervention than younger adults. We examined findings for the overall sample, as well as within each diagnostic group.
Method
Participants
The development and details of the methodology used in the CALM study have been described elsewhere. Reference Roy-Byrne, Veitengruber, Bystritsky, Edlund, Sullivan and Craske14,Reference Sullivan, Craske, Sherbourne, Edlund, Rose and Golinelli15 Primary care patients diagnosed with panic disorder, generalised anxiety disorder, PTSD and social anxiety disorder (as single disorders or in combination) were referred by primary care professionals (internists and family physicians) from 17 clinics at four sites in the USA: Little Rock, Arkansas; Los Angeles County and San Diego, California; and Seattle, Washington. The 1004 randomised participants ranged in age from 18 to 75. Clinical inclusion was based on meeting DSM-IV diagnostic criteria, as assessed by trained interviewers who administered the Mini International Neuropsychiatric Interview, Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs and Weiller16 and also at least moderate anxiety severity and impairment as assessed by the Overall Anxiety Severity and Impairment Scale. Reference Campbell-Sills, Norman, Craske, Sullivan, Lang and Chavira17 Written informed consent was obtained from all participants after study procedures were explained.
Measures
Outcome assessments were conducted via telephone by raters masked to treatment assignment at baseline, 6 months, 12 months and 18 months. The primary outcome of interest was the Brief Symptom Inventory (BSI) Anxiety subscale. Reference Derogatis18 This self-report instrument consists of six Likert-scored items measuring symptoms of worry and autonomic arousal. Internal consistency as measured by Cronbach's alpha at baseline in the present sample was 0.84 for both younger and older adults.
Somatic symptoms were assessed with the BSI Somatic subscale, Reference Derogatis18 which also comprises six Likert-scored items and measures cardiac, gastrointestinal and other bodily sensations. Cronbach's alpha was 0.78 for the younger adults and 0.73 for the older adults. Depressive symptoms were measured with the Patient Health Questionnaire (PHQ). Reference Kroenke, Spitzer and Williams19 The nine-item PHQ was administered at baseline; an eight-item version (with the suicide item omitted) was administered at the 6-, 12- and 18-month follow-up periods. Outcome analyses were based on the eight-item score. The Cronbach's alpha of the eight-item PHQ at baseline was 0.85 for both younger and older adults.
Among the subset of participants with generalised anxiety disorder, the Generalized Anxiety Disorder Severity Scale (GADSS) Reference Shear, Belnap, Mazumdar, Houck and Rollman20 was used to assess symptoms. The Cronbach's alpha of the GADSS at baseline was 0.82 among the younger adults and 0.81 among the older adults. The Panic Disorder Severity Scale (PDSS) was administered to patients with panic disorder. Reference Houck, Spiegel, Shear and Rucci21 Cronbach's alpha was 0.87 for both younger and older adults. Patients with social phobia completed the Social Phobia Inventory (SPIN). Reference Connor, Davidson, Churchill, Sherwood, Weisler and Foa22 Cronbach's alphas were 0.91 for the younger adults and 0.93 for the older adults. Finally, the PTSD Checklist (PCL) measured PTSD symptoms among patients with that diagnosis. Reference Weathers, Litz, Huska and Keane23 Cronbach's alphas in the present sample were 0.88 for the younger adults and 0.89 for the older adults.
Usual care
Patients in the usual care condition received their usual treatment from their physician. At the baseline assessment, 62.1% of the patients in this condition were receiving any psychotropic medication, and 46.7% were receiving counselling. However, only 30.6% of the patients were receiving an adequate dose (i.e. either the maximum dose tolerated or the maximum suggested by the manufacturer) of an appropriate psychotropic medication (usually an selective serotonin reuptake inhibitor (SSRI) or serotonin-noradrenaline reuptake inhibitor (SNRI)) for at least 2 months and only 4.6% were receiving consistent cognitive-behavioural therapy (CBT, i.e. usually or always received three or more essential CBT elements, such as exposure, cognitive restructuring and homework) for their anxiety at baseline.
Collaborative care
The collaborative care intervention was modelled on an intervention that was effective for older primary care patients with major depression. Reference Unützer, Katon, Callahan, Williams, Hunkeler and Harpole24 It was managed by anxiety clinical specialists (ACSs). The ACSs were 11 women and 3 men, including 6 social workers, 5 registered nurses and 3 psychologists (2 master's level and 1 doctoral level). All ACSs had experience working with patients in a primary care setting for an average of 12 years. Eight had mental health experience, four with CBT, and seven had experience managing medications.
Patients in the collaborative care condition were able to choose pharmacotherapy, CBT or both. The ACSs managed the pharmacotherapy, which was prescribed by primary care physicians, to patients who preferred it and for whom it was not contraindicated. A manual for CALM pharmacotherapy included the medication algorithm, strategies for discussing medications with patients, protocols for monitoring medications, managing side-effects and indications for choosing specific medications. The ACS received didactic training and ongoing weekly supervision from a local study psychiatrist in which cases were reviewed and further training was provided on medication management.
The first-line pharmacological treatment for most patients was an SSRI or an SNRI, chosen based on the patient's psychopharmacological history and potential interactions with other medications. For patients who had not responded to SSRI or SNRI medications in the past, a benzodiazepine or GABAergic agent (such as gabapentin or pregabalin) was prescribed initially. Doses of all medications were titrated to the maximal tolerated dose over a period of 4-6 weeks. Each pharmacological treatment was maintained for at least 10-12 weeks; non-responders to first-line SSRIs were switched to another SSRI, an SNRI, a benzodiazepine or a GABAergic, or in some cases to CBT. Treatment for partial responders to first-line SSRI or SNRI pharmacotherapy could be augmented with benzodiazepines, a GABAergic or CBT. Third-line pharmacological strategies included other classes of antidepressants such as mirtazapine or tricyclics, with atypical antipsychotics as a fourth-line option, in all cases with or without CBT.
The ACSs, under weekly supervision from a psychologist, also delivered the CBT intervention, usually in 6-8 weekly sessions. Prior to delivering study treatments, the ACSs received intensive training in CBT, motivational interviewing and outreach strategies. The ACSs delivered treatment following the CALM model, which included a web-based symptom monitoring system and a computer-assisted programme for delivering the CBT. The training included role-playing and successful completion of two to six training cases, which were audiotaped, reviewed by supervisors and rated for adherence and competence. The ACSs were not permitted to see randomised patients until they demonstrated adequate proficiency on at least 50% of their training cases. Although the web-based system allowed supervisors to monitor treatment elements delivered, patient progress and potential problems with the treatment process, adherence and competence were not rated on an ongoing basis.
Statistical analyses
Analyses were conducted by using SAS version 9.1 for Windows 7. Sample characteristics were computed for the older (aged 60-75) and younger adult (aged 18-59) groups. Age differences were examined using chi-squared tests for categorical variables and t-tests for continuous variables. Outcomes were examined both as dichotomous and as continuous variables for the older and younger samples separately, with appropriate covariates included in the models. Logistic regression analyses were used to predict treatment response, as defined by a reduction in BSI Anxiety score of 50% or more relative to baseline, and remission, as defined by BSI Anxiety score less than three. Mixed-model analyses were conducted to examine change in the outcome variables. The restricted maximum likelihood approach was used to fit the models. This approach allows for the use of all available data and accounts for missing data at subsequent time points. Reference Little and Rubin25,Reference Brick and Kalton26 Each model included time (baseline, 6 months, 12 months, 18 months), treatment condition (intervention v. usual care), and the time × treatment interaction. Time was treated as a categorical variable. The intercept and time were also included as random effects in the model. The proposed model was fit using a restricted maximum likelihood approach. The estimated means for each treatment group at each time point were generated. In addition to examining the significance of the overall model, we compared the means scores for the intervention and usual care at each time point. We performed analyses with the BSI Anxiety and Somatic subscales and PHQ as dependent variables using the overall sample. We also performed separate analyses for each diagnostic subgroup using the appropriate diagnosis-specific measure (GADSS for those with generalised anxiety disorder; PDSS for those with panic disorder, etc.).
Results
Of the 1004 participants in the CALM study, 134 (13.3%) were 60-75 years of age. Demographic and baseline clinical information for the sample is displayed in Table 1. Not surprisingly, older adults had on average a higher number of chronic medical conditions and more visits to medical specialists than did younger adults, although the groups did not differ significantly on primary care visits. Older adults also had lower levels of education, were more likely to be White, and were less likely to be working. They did not differ from younger adults by gender or marital status. In terms of diagnoses, a significantly lower proportion of older than younger individuals met criteria for social anxiety disorder (26.1% v. 42.3%, χ2 = 12.65, P<0.001) and panic disorder (35.8% v. 49.5%, χ2 = 8.76, P = 0.003); age differences in rates of generalised anxiety disorder (74.6% v. 75.3%, χ2 = 0.27, P = 0.87), PTSD (23.1% v. 17.2%, χ2 = 2.73, P = 0.10) and major depression (70.1% v. 63.6%, χ2 = 2.20, P= 0.14) were not statistically significant. Scores on symptom scales did not differ by age. Older adults had, on average, fewer anxiety disorders than did younger adults. All analyses controlled for education, number of chronic medical conditions, the presence of more than one anxiety disorder diagnosis and the presence of comorbid major depression.
Table 1 Demographics and baseline clinical variables for the overall sample
| Age group, years | Total, n | |||||
|---|---|---|---|---|---|---|
| 18-59 | 60-75 | 18-59 | 60-75 | χ2 or t-test | P | |
| Gender, n (%) | 870 | 134 | <0.01 | 0.95 | ||
| Male | 251 (28.9) | 39 (29.1) | ||||
| Female | 619 (71.1) | 95 (70.9) | ||||
| Hispanic, n (%) | 174 (20.0) | 22 (16.4) | 870 | 134 | 0.95 | 0.33 |
| Ethnicity, n (%) | 870 | 134 | ||||
| American Indian | 51 (5.8) | 7 (5.2) | 0.90 | 0.76 | ||
| Asian | 39 (4.4) | 1 (0.7) | 4.25 | 0.03 | ||
| Pacific Islander | 19 (2.2) | 1 (0.7) | 1.23 | 0.50 | ||
| African American | 109 (12.5) | 7 (5.2) | 6.37 | 0.01 | ||
| White | 482 (55.4) | 86 (64.2) | 7.65 | 0.01 | ||
| Other | 105 (12.1) | 19 (14.2) | 0.14 | 0.71 | ||
| Education, n (%) | 870 | 134 | 7.80 | 0.02 | ||
| <12 years 42 (4.8) | 13 (9.8) | |||||
| 12 years | 138 (15.9) | 27 (20.3)Footnote a | ||||
| >12 years | 689 (79.3)Footnote a | 93 (69.9)Footnote a | ||||
| Married or cohabiting, n (%) | 466 (53.6) | 73 (54.9)Footnote a | 870 | 134 | 0.08 | 0.78 |
| Employed, n (%) | 655 (75.5)Footnote b | 53 (39.6) | 870 | 134 | 72.20 | <0.001 |
| Major chronic medical conditions, n (s.d.) | 2.1 (1.9) | 3.7 (2.2) | 870 | 134 | –8.26 | <0.001 |
| Primary care visits | 4.3 (4.2) | 5.0 (5.8) | 870 | 134 | –1.69 | 0.09 |
| Medical specialist visits | 1.0 (2.4) | 1.7 (2.8) | 870 | 134 | –2.60 | 0.01 |
| Number of anxiety disorders, n (%) | 870 | 134 | 11.4 | 0.01 | ||
| One | 346 (39.8) | 73 (54.5) | ||||
| Two | 345 (39.7) | 44 (32.8) | ||||
| Three | 147 (16.9) | 15 (11.2) | ||||
| Four | 32 (3.7) | 2 (1.5) | ||||
| Measures, n (s.d.) | ||||||
| Brief Symptom Inventory Anxiety subscale T-score | 65.2 (8.6) | 65.7 (8.4) | 870 | 134 | –0.66 | 0.51 |
| Brief Symptom Inventory Somatic subscale T-score | 60.4 (9.7) | 60.8 (9.1) | 870 | 134 | –0.42 | 0.68 |
| Patient Health Questionnaire | 12.7 (6.3) | 13.4 (6.5) | 870 | 134 | –1.19 | 0.23 |
| Generalized Anxiety Disorder Severity Scale | 13.9 (3.9) | 13.9 (3.7) | 655 | 100 | –0.06 | 0.96 |
| Panic Disorder Severity Scale | 13.5 (5.8) | 13.2 (5.8) | 428 | 47 | 0.37 | 0.71 |
| Social Phobia Inventory | 38.2 (13.3) | 39.7 (14.6) | 368 | 35 | –0.62 | 0.54 |
| PTSD Checklist | 55.6 (12.3) | 57.5 (13.2) | 150 | 31 | –0.78 | 0.44 |
a. Missing data for one person.
b. Missing data for two people.
Statistically equivalent proportions of younger (n = 442, 50.8%) and older adults (n = 61, 45.5%, χ2 = 1.30, P = 0.26) were randomised to the collaborative care intervention. Among the younger adults, 11.3% (n = 50) in the collaborative care condition and 15.0% (n = 64) in the usual care condition, χ2 = 2.53, P = 0.12, were missing data at the 6-month assessment period.
Comparable data for the 12- and 18-month periods were 19.2% (n = 85) v. 20.8% (n = 89), χ2 = 0.33, P = 0.56, and 19.7% (n = 87) v. 22.2% (n = 95), χ2 = 0.83, P = 0.36. Among the older adults, rates of missing data at the 6-, 12- and 18-month assessment for the collaborative care and usual care arms, respectively, were 11.5% (n = 7) v. 9.6% (n = 7), χ2 = 0.13, P = 0.73; 13.1% (n = 8) v. 12.3% (n = 9), χ2 = 0.02, P = 0.90; and 13.1% (n = 8) v. 15.1% (n = 11), χ2 = 0.10, P = 0.75. Across both treatment conditions, a higher proportion of younger adults (20.0%, n = 174) than older adults (12.7%, n = 17) were missing data at the 12-month assessment period, χ2 = 4.03, P = 0.05. Differences were not statistically significant at the 6-month time period, 13.1% (n = 114, younger) v. 10.5% (n = 14, older), χ2 = 0.74, P = 0.39 or 18-month assessment period, 20.9% (n = 182) v. 14.2% (n = 19), χ2 = 3.29, P = 0.07. It should be noted that some participants who missed the 6- or 12-month assessments did provide data at subsequent assessments.
Among those randomised to collaborative care, 6.6% (n = 4) of older adults received medication only, 34.4% (n = 21) received CBT only and 59.0% (n = 36) received combined treatment. Comparable data for the younger adults were 8.8% (n = 39), 32.8% (n = 145), and 53.6% (n = 237) respectively, with another 21 (4.8%) receiving neither CBT nor medications. Treatment type did not differ by age, χ2(3) = 3.55, P = 0.31. Of those receiving CBT, 68.4% (n = 39) of older adults and 75.7% (n = 289) of younger adults completed at least 6 sessions, χ2 = 1.37, P = 0.24. Detailed information on medications by age group and treatment condition at each time point is presented in Table 2.
Among younger adults, those receiving the intervention were more likely to respond and remit at all time points than were those who received usual care (Table 3). Among older adults, the intervention was associated with higher response rates at 12 months, but not at 6 or 18 months. The intervention was not associated with significantly higher remission rates than usual care at any time point for the older adults. These analyses were also run with participants with missing data assumed to be non-responders and not remitted; results did not change substantially.
With respect to anxiety symptoms as measured by the BSI Anxiety subscale, the overall treatment × time interaction was significant among both younger (F(3,862) = 6.39, P = 0.0003) and older (F(3,127) = 3.21, P = 0.03) participants. Among the younger adults, the CALM intervention was equivalent to usual care at baseline and superior to usual care at all subsequent time points (Fig. 1). Among older adults, the CALM intervention was superior to usual care at 12 months but not at 6 or 18 months. For somatic symptoms, the CALM intervention was superior among the younger adults (F(3,862) = 5.35, P = 0.001) but not among the older adults overall or at any time point (F(3,127) = 0.79, P = 0.50; Fig. 2). For depressive symptoms as measured by the PHQ, the treatment × time interaction was significant in the younger (F(3,862) = 8.24, P<0.0001) and older groups (F (3,127) = 3.36, P = 0.02), with the intervention superior to usual care at all follow-up points among the younger adults and at 12 months among the older individuals (Fig. 3).
Table 2 Proportion of patients taking various classes of anxiolytic medications at an appropriate dose for at least 2 months by age and treatment condition at each time pointFootnote a
| % (n) | χ2 (P) | |||||||
|---|---|---|---|---|---|---|---|---|
| Class of drug, at appropriate dose for 2 months or more |
Younger CALM |
Younger usual care |
Older CALM |
Older usual care |
Younger CALM v. younger usual care |
Older CALM v. older usual care |
Younger CALM v. older CALM |
Younger usual care v. older usual care |
| Baseline | ||||||||
| Any appropriate agent | 27.7 (120) | 29.5 (124) | 37.9 (22) | 36.6 (26) | 0.37 (0.55) | 0.23 (0.88) | 2.63 (0.11) | 1.44 (0.23) |
| Antidepressant | 25.7 (112) | 26.3 (111) | 27.1 (16) | 31.5 (23) | 0.04 (0.84) | 0.30 (0.58) | 0.06 (0.82) | 0.85 (0.36) |
| Benzodiazepine | 2.8 (12) | 5.4 (23) | 10.0 (6) | 4.2 (3) | 3.88 (0.05) | 1.69 (0.19) | 7.83 (<0.01) | 0.18 (0.67) |
| Other anti-anxiety agent | 2.0 (9) | 0.9 (4) | 5.0 (3) | 5.5 (4) | 0.37 (0.55) | 0.02 (0.90) | 1.99 (0.16) | 8.20 (<0.01) |
| 6 months | ||||||||
| Any appropriate agent | 46.1 (178) | 42.3 (151) | 51.0 (26) | 37.5 (24) | 1.10 (0.30) | 2.10 (0.15) | 0.43 (0.51) | 0.51 (0.47) |
| Antidepressant | 44.3 (172) | 37.3 (134) | 43.4 (23) | 36.9 (24) | 3.78 (0.52) | 0.51 (0.48) | 0.02 (0.90) | 0.01 (0.95) |
| Benzodiazepine | 4.4 (17) | 8.3 (30) | 11.3 (6) | 1.5 (1) | 4.94 (0.03) | 5.01 (0.03) | 4.62 (0.04) | 3.71 (0.06) |
| Other anti-anxiety agent | 1.8 (7) | 0.8 (3) | 3.9 (2) | 1.5 (1) | 1.36 (0.24) | 0.62 (0.43) | 0.95 (0.33) | 0.30 (0.58) |
| 12 months | ||||||||
| Any appropriate agent | 41.4 (146) | 35.5 (117) | 55.1 (27) | 38.7 (24) | 2.51 (0.12) | 2.96 (0.09) | 3.31 (0.07) | 0.24 (0.62) |
| Antidepressant | 40.4 (143) | 31.6 (105) | 45.1 (23) | 38.7 (24) | 5.71 (0.02) | 0.47 (0.50) | 0.41 (0.52) | 0.19 (0.28) |
| Benzodiazepine | 4.3 (15) | 6.6 (22) | 11.5 (6) | 3.1 (2) | 1.79 (0.18) | 3.16 (0.08) | 4.84 (0.03) | 1.14 (0.29) |
| Other anti-anxiety | 1.1 (4) | 0.9 (3) | 3.9 (2) | 3.9 (2) | 0.10 (0.76) | 0.05 (0.83) | 2.38 (0.13) | 2.23 (0.14) |
| 18 months | ||||||||
| Any appropriate agent | 39.6 (140) | 36.4 (118) | 49.0 (25) | 40.0 (24) | 0.70 (0.40) | 0.91 (0.34) | 1.66 (0.20) | 0.28 (0.60) |
| Antidepressant | 38.1 (135) | 32.8 (107) | 39.2 (20) | 40.0 (24) | 2.09 (0.15) | 0.01 (0.93) | 0.02 (0.88) | 1.16 (0.28) |
| Benzodiazepine | 4.8 (17) | 5.7 (19) | 9.6 (5) | 3.2 (2) | 0.29 (0.59) | 2.00 (0.16) | 2.03 (0.15) | 0.65 (0.42) |
| Other anti-anxiety | 1.4 (5) | 1.2 (4) | 3.9 (2) | 3.2 (2) | 0.05 (0.82) | 0.03 (0.86) | 1.59 (0.21) | 1.41 (0.24) |
CALM, Coordinated Anxiety Learning and Management.
a. Results in bold are statistically significant.
Table 3 Adjusted odds ratios associated with response and remission to a collaborative care intervention for anxiety disorders relative to usual care by age groupFootnote a
| Response (BSI Anxiety decrease ⩾50%), OR (95% CI) | Remission (BSI Anxiety score <3), OR (95% CI) | |||||
|---|---|---|---|---|---|---|
| 6 months | 12 months | 18 months | 6 months | 12 months | 18 months | |
| Younger | 2.15 (1.60-2.89) | 2.24 (1.64-3.04) | 1.83 (1.34-2.49) | 2.37 (1.69-3.33) | 1.86 (1.35-2.56) | 2.16 (1.56-2.98) |
| Older | 1.47 (0.69-3.12) | 4.04 (1.81-9.00) | 1.70 (0.79-3.65) | 1.94 (0.78-4.80) | 1.75 (0.80-3.83) | 1.08 (0.49-2.38) |
BSI, Brief Symptom Inventory.
a. Controlled for education, number of chronic medical conditions, presence of more than one anxiety disorder and major depression at baseline. Results in bold are statistically significant.
Among the patients with generalised anxiety disorder, the intervention was significantly better than usual care for generalised anxiety disorder symptoms as measured by the GADSS in the younger group (F(3,648) = 6.93, P<0.0001) but not in the older group (F(3,93) = 2.26, P = 0.09; Fig. 4). Similarly, for patients with panic disorder, the intervention was significantly better than usual care for panic symptoms among the younger adults (F(3,420) = 3.84, P = 0.01), but not among the older adults (F(3,41) = 2.06, P = 0.12; Fig. 5). Results favoured the collaborative care intervention relative to usual care for older adults with social phobia (F(3,28) = 5.22, P = 0.006; Fig. 6) and PTSD (F(3,25) = 3.02, P<0.05; Fig. 7); results for younger adults favoured the collaborative care intervention for those with social phobia (F(3,363) = 8.81, P<0.0001) but not for those with PTSD (F(3,143) = 2.15, P = 0.10).
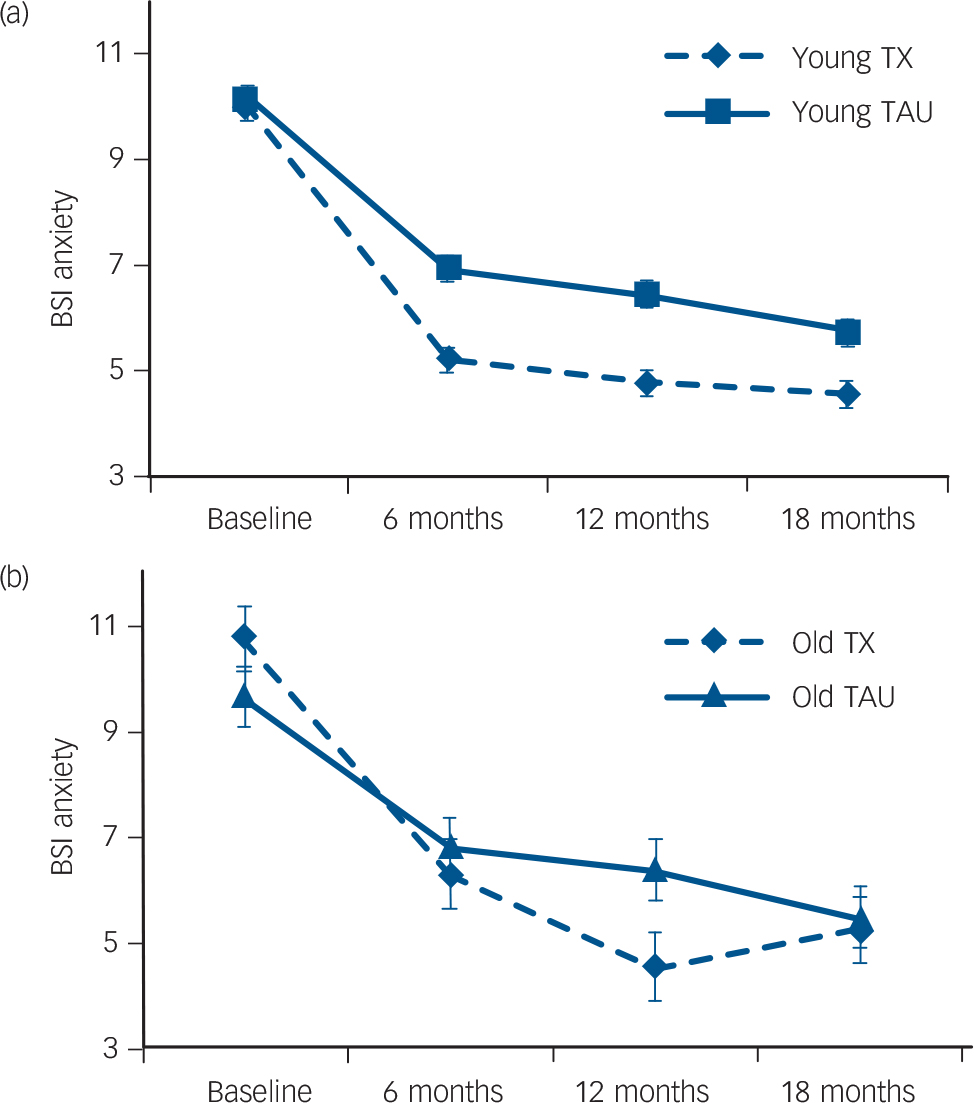
Fig. 1 Anxiety symptoms in (a) younger (n = 870) and (b) older (n = 134) primary care patients with anxiety disorders receiving a collaborative care intervention (TX) or usual care (TAU).
Controlled for education, number of chronic medical conditions, presence of more than one anxiety disorder and comorbid major depression. BSI, Brief Symptom Inventory.
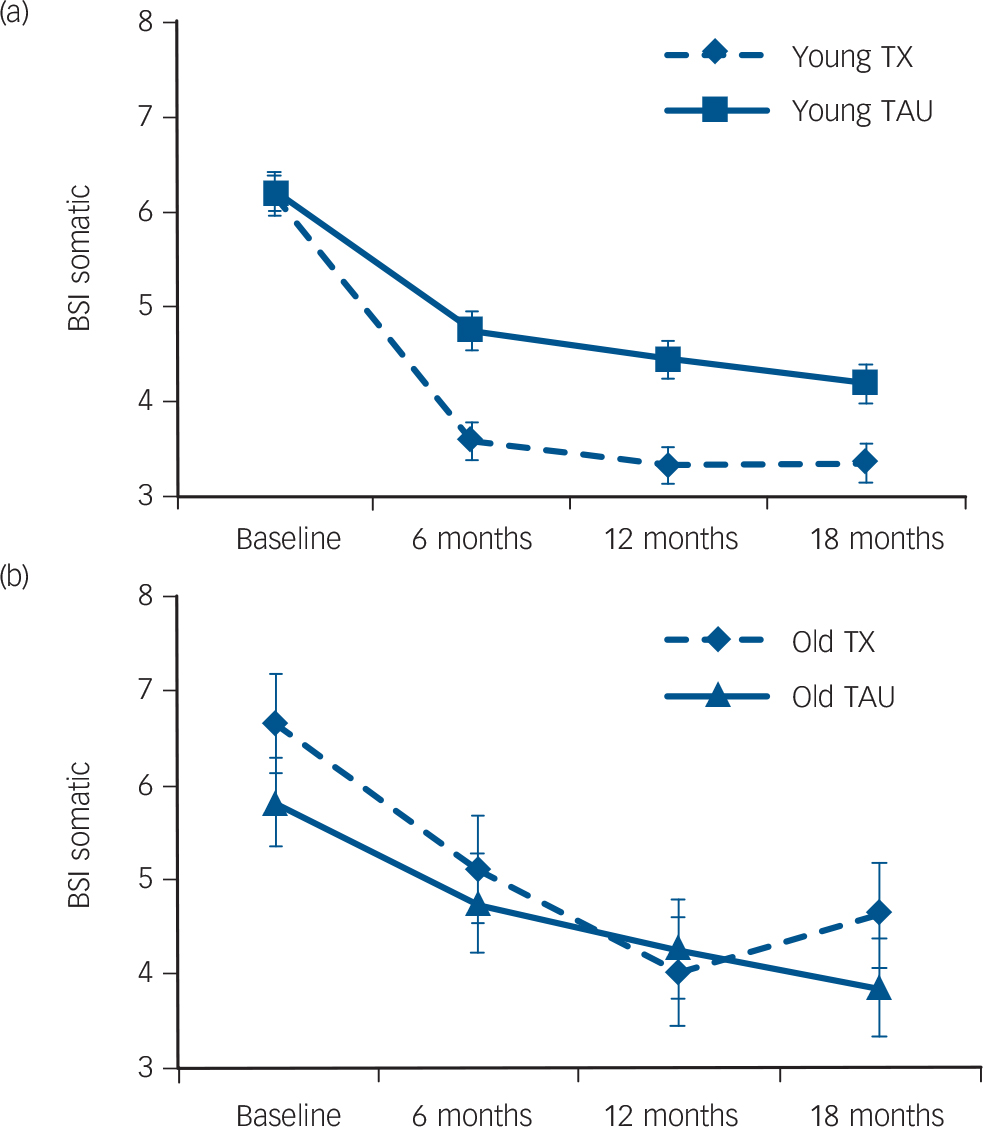
Fig. 2 Somatic symptoms in (a) younger (n = 870) and (b) older (n = 134) primary care patients with anxiety disorders receiving a collaborative care intervention (TX) or usual care (TAU).
Controlled for education, number of chronic medical conditions, presence of more than one anxiety disorder and comorbid major depression. BSI, Brief Symptom Inventory.
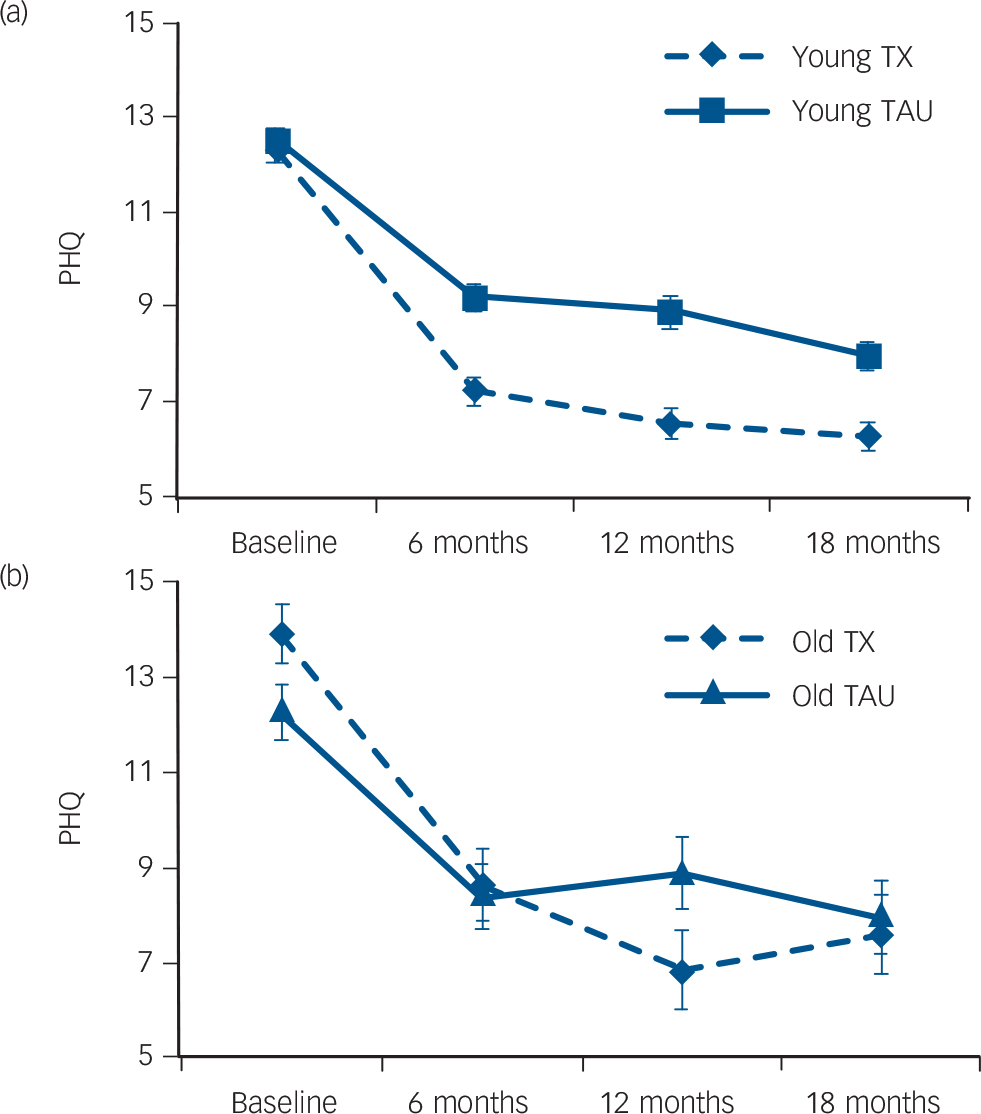
Fig. 3 Depressive symptoms in (a) younger (n = 870) and (b) older (n = 134) primary care patients with anxiety disorders receiving a collaborative care intervention (TX) or usual care (TAU).
Controlled for education, number of chronic medical conditions, presence of more than one anxiety disorder and comorbid major depression. PHQ, Patient Health Questionnaire.
Discussion
Main findings
The CALM collaborative care intervention was more effective than usual care in younger adults overall and among those with generalised anxiety disorder, panic disorder and social phobia, although not among those with PTSD. This was true for almost all measures at all follow-up time points, in terms of symptom levels and responder and remitter status. In older adults, however, the intervention was only significantly better on anxiety and depressive symptoms than usual care at 12 months, effects appeared to erode by the 18-month follow-up, and there were no significant effects on remission at any time point. Effects were not significant for somatic symptoms in older adults, but the somatic subscale may have reflected medical illness rather than emotional distress. Among patients with generalised anxiety disorder and panic disorder, the collaborative care intervention was not more effective than usual care among the older adults at any time point, but results in the older panic disorder subsample may have been influenced by the low sample size. Overall, these findings are consistent with those of other investigators suggesting that medications Reference Préville, Vasiliadis, Bossé, Dionne, Voyer and Brassard10,Reference Tedeschini, Levkovitz, lovieno, Ameral, Nelson and Papakostas11 and CBT for anxiety disorders Reference Goncalves and Byrne8,Reference Gould, Coulson and Howard9,Reference Covin, Ouimet, Seeds and Dozois12 may not be as effective for older individuals as they are for younger people.
Although neither the type of care received nor the attrition rates differed between older and younger adults, older adults took longer to respond to the collaborative care intervention than did younger adults, and they were more likely to experience a recurrence of symptoms at 18-month follow-up. Age-related pharmacodynamic and learning factors may be responsible for the delayed and less robust treatment response among older adults.
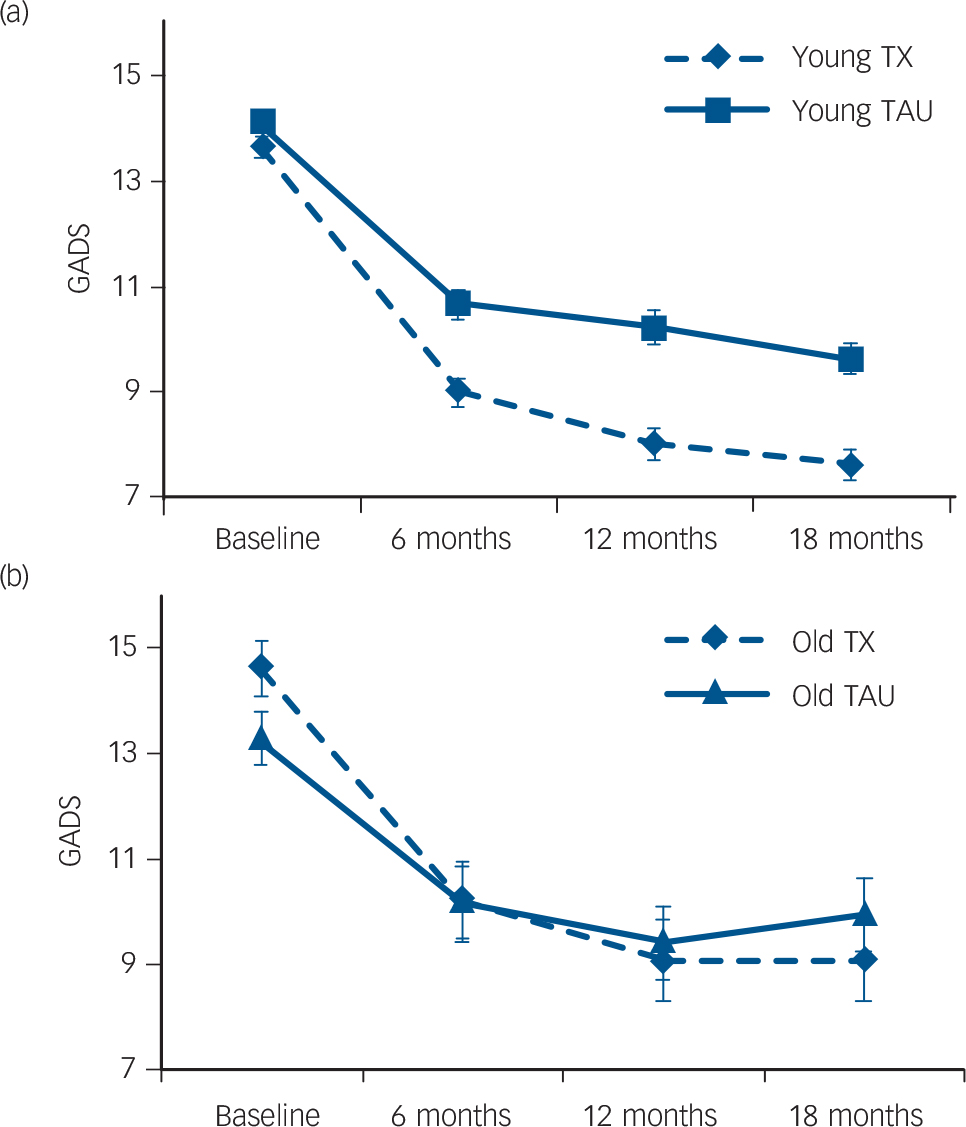
Fig. 4 Generalised anxiety disorder symptoms in (a) younger (n = 655) and (b) older (n = 100) primary care patients with generalised anxiety disorder receiving a collaborative care intervention (TX) or usual care (TAU).
Controlled for education, number of chronic medical conditions, presence of more than one anxiety disorder and comorbid major depression. GADSS, Generalized Anxiety Disorder Severity Scale.
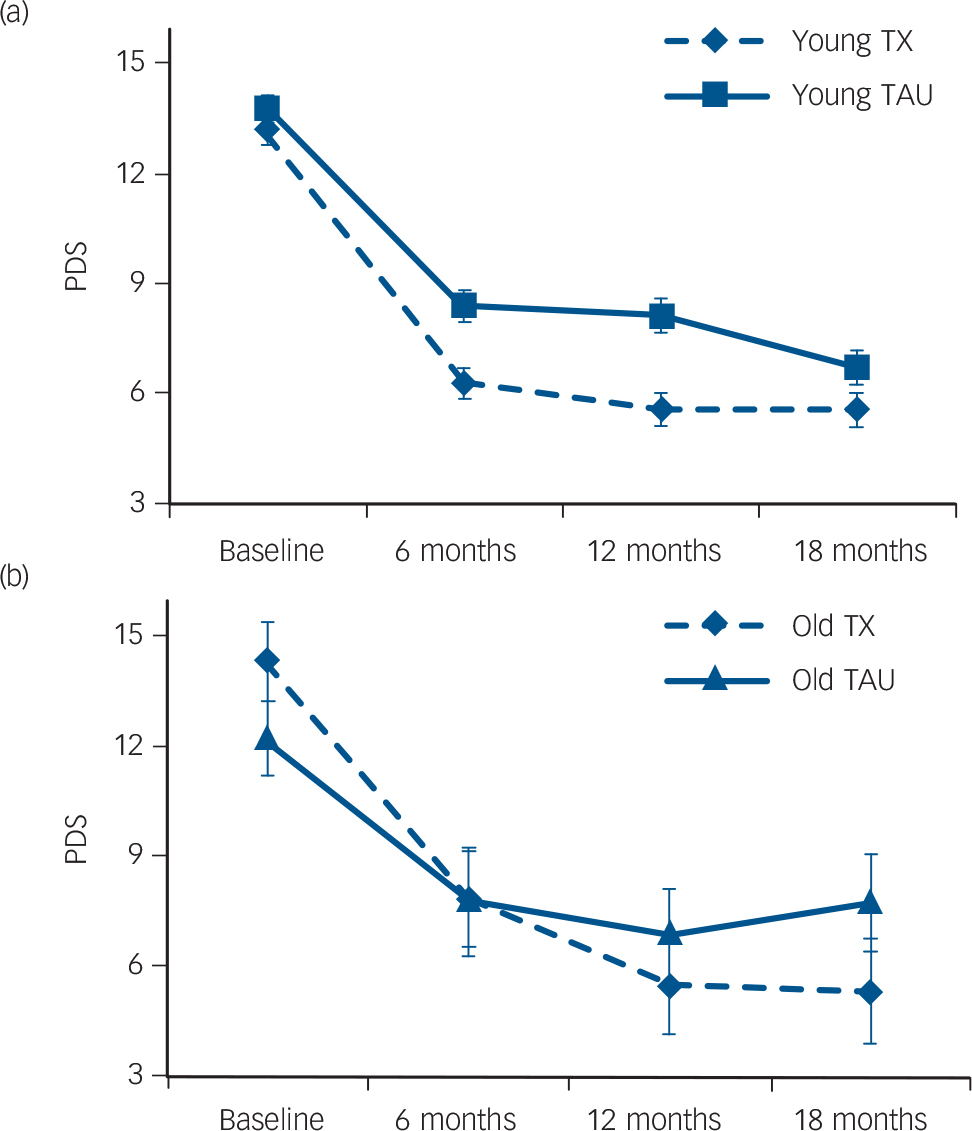
Fig. 5 Panic disorder symptoms in (a) younger (n = 428) and (b) older (n = 47) primary care patients with panic disorder receiving a collaborative care intervention (TX) or usual care (TAU).
Controlled for education, number of chronic medical conditions, presence of more than one anxiety disorder and comorbid major depression. PDSS, Panic Disorder Severity Scale.
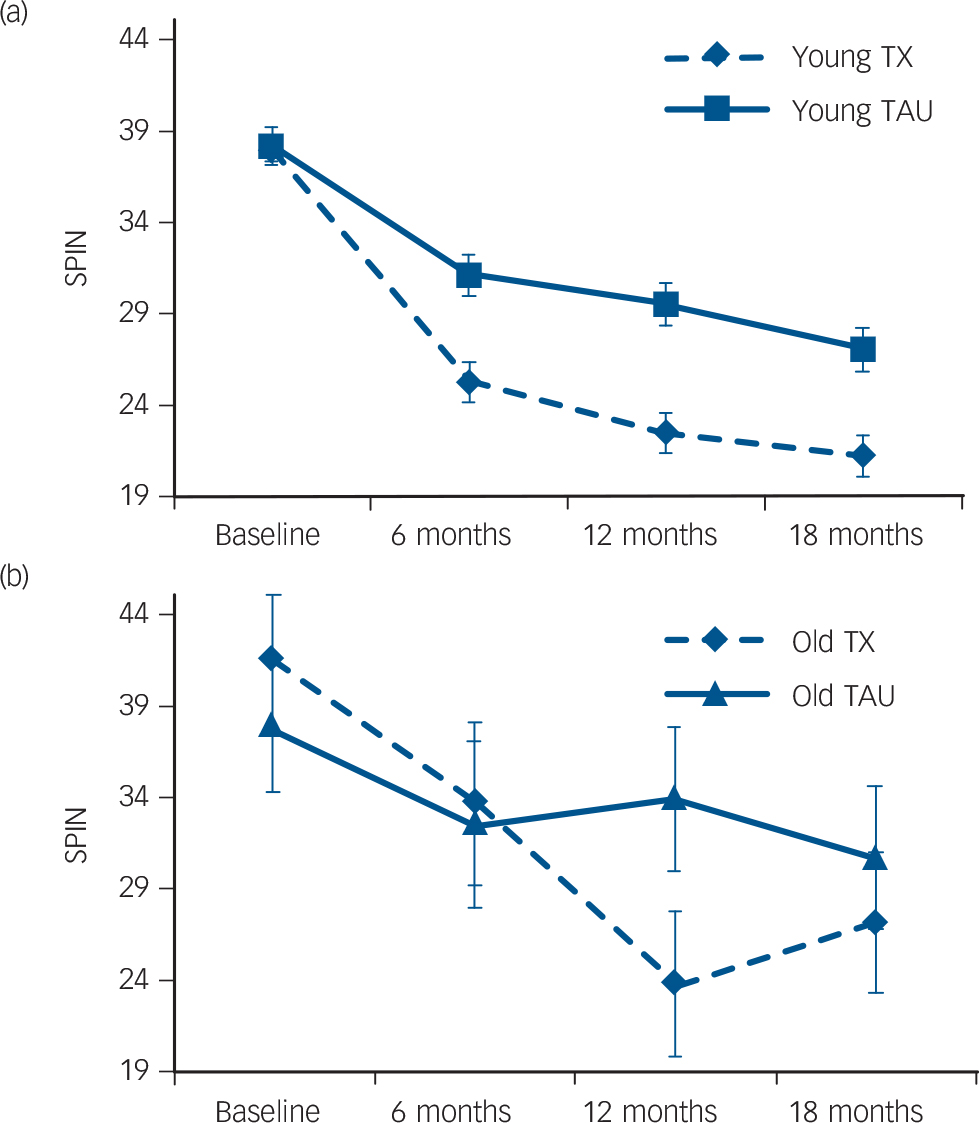
Fig. 6 Social phobia symptoms in (a) younger (n = 368) and (b) older (n = 35) primary care patients with panic disorder receiving a collaborative care intervention (TX) or usual care (TAU).
Controlled for education, number of chronic medical conditions, presence of more than one anxiety disorder and comorbid major depression. SPIN, Social Phobia Inventory.
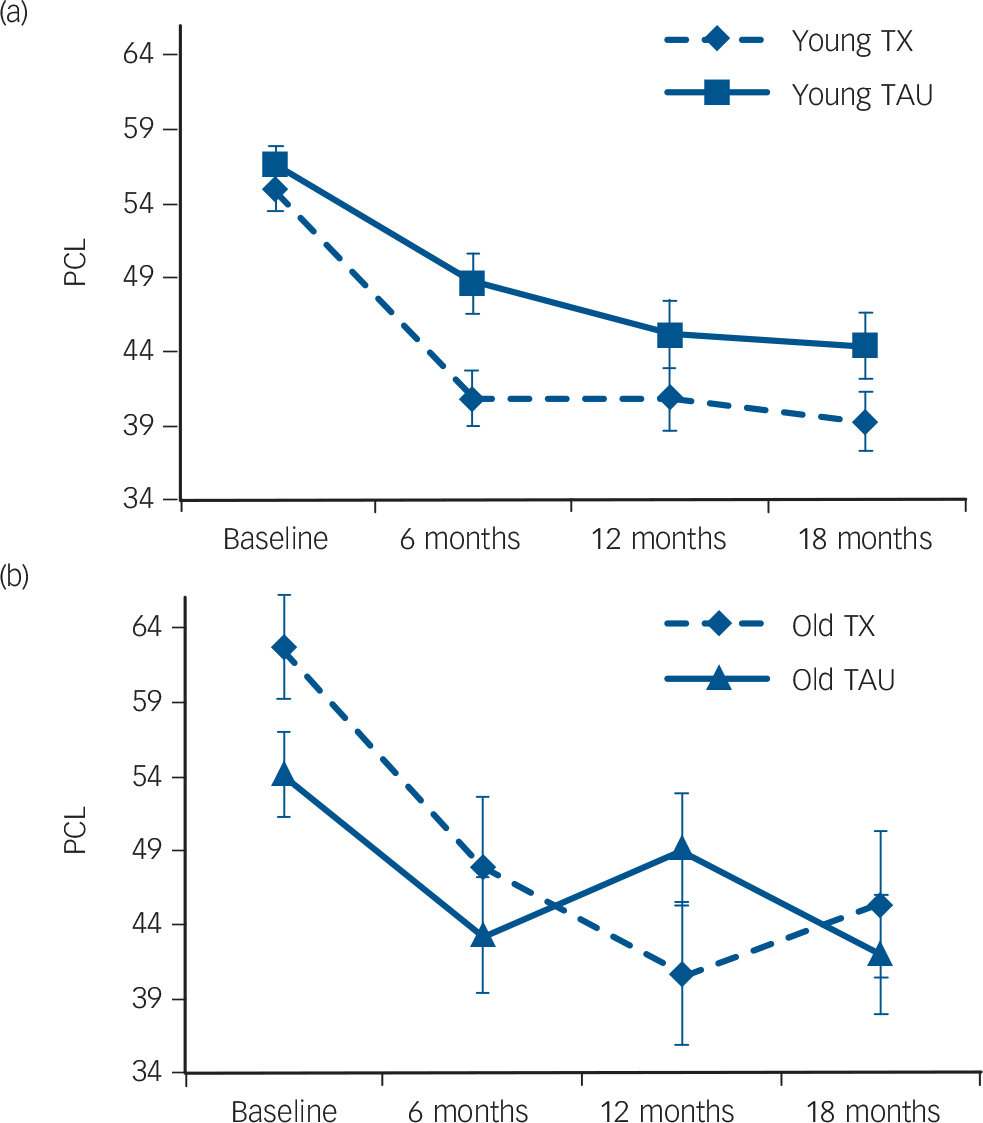
Fig. 7 Post-traumatic stress disorder (PTSD) symptoms in (a) younger (n = 150) and (b) older (n = 31) primary care patients with panic disorder receiving a collaborative care intervention (TX) or usual care (TAU).
Controlled for education, number of chronic medical conditions, presence of more than one anxiety disorder and comorbid major depression. PCL, PTSD Checklist.
Because pharmacological Reference Kok, Nolen and Heeren27,Reference Pinquart, Duberstein and Lyness28 and behavioural Reference Arean, Raue, Mackin, Kanellopoulos, McCulloch and Alexopoulos29,Reference Serfaty, Haworth, Blanchard, Buszewicz, Murad and King30 treatments are effective for depression in older adults, it is unlikely that factors directly related to ageing such as medical illness, medication use or cognitive impairment are completely responsible for the decreased efficacy of treatment for anxiety in older adults. It is plausible that the chronic nature of anxiety disorders may account for their resistance to treatment in later life. Generalised anxiety disorder in particular is a highly chronic condition, which in older adults has an average duration of 20 years or more before presentation for treatment. Reference Chou31,Reference Goncalves and Byrne32 By contrast, depression in older adults is both more episodic and more likely to develop for the first time in old age. Reference Kessler, Berglund, Demler, Jin, Merikangas and Walters2,Reference Penninx, Nolen, Lamers, Zitman, Smit and Spinhoven33 Unfortunately, age at onset data were not collected in the present study to allow us to test for the effects of duration in this sample.
It is possible that some features of the collaborative care intervention are responsible for its relative lack of effectiveness among older adults. For example, it was delivered by primary care healthcare workers, many of whom had limited experience delivering mental health services before the trial, the CBT was limited to 6-8 sessions, and it was not modified for older individuals. It may be that older adults with anxiety disorders, unlike those with major depression, require specialty care from seasoned mental health professionals, modified CBT and/or a longer course of treatment. These are empirical questions that should be addressed in future research.
It is also possible that characteristics of the older adults enrolled in this trial influenced the results. Older individuals with anxiety disorders presenting in primary care may differ in important ways from anxious older adults presenting to mental health clinics or those participating in clinical trials of anxiety treatments. Moreover, because cognitive performance was not assessed, some participants in the present study may have had cognitive impairment that affected their response to the intervention.
This study represents, to our knowledge, the first investigation to examine the efficacy of a collaborative care intervention in a sample that included both younger and older adults with anxiety disorders. As such, it represents a methodological advance over meta-analyses that attempt to compare effect sizes across studies. The CALM study was a large-scale, well-designed, and carefully conducted investigation. Moreover, the setting was in primary care, where most older (and younger) adults with anxiety disorders present for treatment, Reference Klapow, Kroenke, Horton, Schmidt, Spitzer and Williams34-Reference Rollman, Belnap, Mazumdar, Houck, Zhu and Gardner36 suggesting that the findings are likely generalisable to the broader population of individuals seeking help for anxiety.
Collaborative care models are more common in other high-income nations than in the USA, where the reimbursement system poses obstacles to the practice of non-mental health providers performing mental health interventions. Therefore, it is possible that anxious older adults would fare better in countries with well-established collaborative care networks employing highly experienced care management specialists. Collaborative care for depression in older adults does appear to work in the USA, however, Reference Unützer, Katon, Callahan, Williams, Hunkeler and Harpole24 suggesting that the nationality of the current trial cannot completely explain the results.
Limitations
The present study has several limitations. First, this is a secondary analysis of data from an effectiveness study of a collaborative care intervention in primary care. Because it was a secondary analysis, participants were not randomised stratified by age, although no significant differences were found in the proportion of younger and older adults randomised to the intervention. Effectiveness studies differ from efficacy studies in that they attempt to assess how well a treatment works in real-world settings, as opposed to a tightly controlled research setting in which, for example, therapy sessions are videotaped and rated for adherence and competence throughout the duration of the trial and blood samples are drawn to measure adherence to pharmacotherapy. It is not uncommon for treatments that work in efficacy trials to fail when exported outside of the laboratory. This may explain the fact that although prior studies have shown CBT and pharmacotherapy to be efficacious relative to pill placebo, waiting list or usual care for generalised anxiety disorder and panic disorder in older adults, Reference Lenze, Rollman, Shear, Dew, Pollock and Ciliberti37-Reference Hendriks, Keijsers, Kampman, Oude Voshaar, Verbraak and Broekman39 such was not the case here. Additionally, studies of collaborative care interventions are intended to answer questions about care delivery models rather than specific treatments. As such, important issues such as the comparative efficacy of various types of treatments and the appropriate dose (including the optimal number of CBT sessions) are not addressed. Future research should investigate age differences in response to medications, psychotherapy and their combination for anxiety disorders in a more tightly controlled efficacy trial.
Although the CALM study is the third largest investigation of anxiety treatment in older adults ever conducted, the number of elderly individuals was still relatively small. A fourfold increase in the sample size needed for adequate power to detect a significant two-way interaction is required to detect a significant three-way interaction (i.e. including age as a factor along with time and treatment condition), Reference Heo and Leon40 which is why we modelled data from younger and older participants separately. People older than 75 were excluded from participation; if ageing does diminish the effects of anxiety treatment, the exclusion of the very old may have biased the results away from a finding of significant age differences. Finally, the comparison condition consisted of treatment as usual in the primary care setting, rather than a consistent alternative treatment or active control condition.
Implications
The most positive message from this study is that people as old as 75 with anxiety disorders do appear to benefit from a collaborative care intervention, relative to usual care, albeit not as much as younger adults do. Another clinical implication of these findings is that older adults with generalised anxiety disorder or panic disorder may require closer monitoring and more intensive treatment than do younger people with these disorders or than older adults with other anxiety disorders. Additionally, older people with anxiety disorders may benefit from periodic booster sessions to ensure that treatment gains are maintained.
Funding
This work was supported by grants U01 MH057858 and K24 MH065324 (P.R.-B.), U01 MH058915 (M.G.C.), U01 MH070022 (G.S.), U01 MH070018 (C.S.) and U01MH057835 and K24 MH64122 (M.B.S.) from the National Institute of Mental Health.













eLetters
No eLetters have been published for this article.