Depressive disorders are one of the most important mental health problems world-wide (Reference LepineLepine, 2001). Over the past decades, effective biological and psychological treatments have been developed, and various treatment guidelines have been compiled to improve the quality of treatment (American Psychiatric Association, 2000; Deutsche Gesellschaft für Psychiatrie, Psychotherapie und Nervenheilkunde, 2000). Adherence to guidelines has been shown to enhance treatment outcome (Reference Melfi, Chawla and CroghanMelfi et al, 1998) but is still variable in clinical practice (Reference Ackerman, Unutzer and GreenlandAckerman et al, 2002; Reference Härter, Sitta and KellerHärter et al, 2004; Reference Schneider, Kratz and BermejoSchneider et al, 2004). The aim of this study is to describe the status of treatment of in-patients for depression in Germany and to compare treatment routines with guideline recommendations in order to identify starting points for quality management. Owing to increasing medical costs and tight budgets, there is a growing need for quality management to assure effective and high standards of care.
METHOD
Design
This was conducted as a multicentre study. For each patient, data were collected at admission, during in-patient treatment and at discharge. Within the first 3 days of admission patients were asked to rate their level of depression. The psychiatrists documented the patients’ socio-demographic characteristics, history of depression and psychopathology, and rated the patients’ levels of depression. During in-patient treatment they noted treatment characteristics (e.g. diagnostic and therapeutic procedures) as well as psychopathology (Psychiatric Basic Documentation System, BADO; Reference Cording, Gaebel and SpenglerCording et al, 1995) on a weekly basis. At discharge the patients rated their level of depression and satisfaction with treatment. The psychiatrists rated the patients’ level of depression and noted other variables (e.g. subsequent treatment, changes in job situation).
Assessment tools
In order to take into account the complexity of treatment for depression, we assessed structure, process and outcome quality aspects (Reference DonabedianDonabedian, 1966; Fig. 1). For assessing psychopathology, we chose the self-rating Beck Depression Inventory (BDI; Reference Beck, Ward and MendelsonBeck et al, 1961), the expert-rating Hamilton Rating Scale for Depression (HRSD, 21-item version; Reference HamiltonHamilton, 1967) and the Global Assessment of Functioning Scale (GAF; American Psychiatric Association, 1994). The ZUF–8 (Reference Schmidt, Lamprecht and WittmannSchmidt et al, 1989) measures patients’ satisfaction with treatment. Interactive video-based rater training on use of the HRSD was conducted in every hospital, with an average intraclass coefficient of 0.63 (F=2.7, d.f.=19,418; P < 0.001). To assess general information about patients and the treatment process we modified the German documentation system BADO according to the special needs of care of in-patients with depression. The BADO is a standard instrument for quality assurance of psychiatric in-patient care developed by the German Association of Psychiatry, Psychotherapy and Neurology (DGPPN) (Reference Cording, Gaebel and SpenglerCording et al, 1995). The modified version consists of three forms: admission (27 items) course of treatment (7 items) and discharge (29 items).
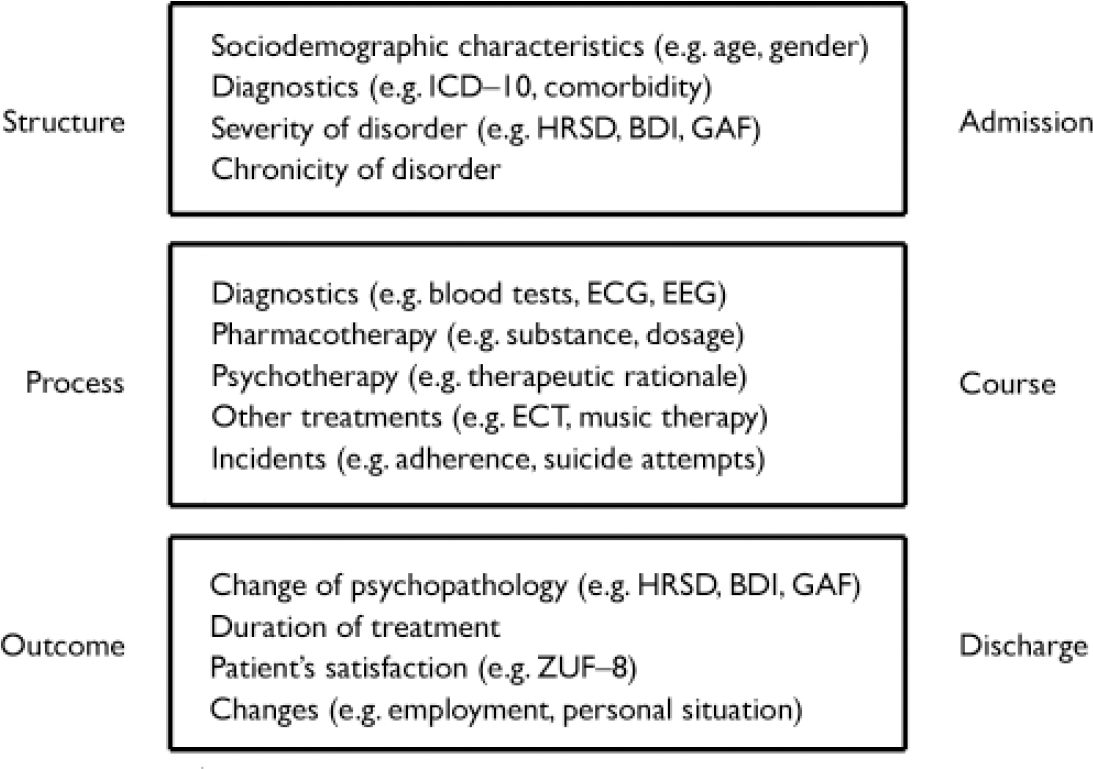
Fig. 1 Structure, process and outcome quality aspects of the treatment of depression in in-patients. HRSD, Hamilton Rating Scale for Depression; BDI, Beck Depression Inventory; GAF, Global Assessment of Functioning scale; ECG, electrocardiogram; EEG, electroencephalogram; ECT, electroconvulsive therapy.
Recruitment procedure
Recruitment started in December 2001 and finished either as soon as 150 patients had been recruited per hospital or at the latest by the end of February 2003. Each adult patient (> 18 years) was included prospectively if they had received in-patient treatment for at least 3 days and had depressive symptoms meeting one of the following ICD–10 diagnostic criteria (World Health Organization, 1993): depressive episode, bipolar (F31.3–F31.5), depressive episode, unipolar (F32.0–F32.2), depressive episode, recurrent (F33.0–F33.9), dysthymia (F34.1), other chronic depressive disorders (F34.8–F34.9), other affective disorders (F38–F39) and adjustment disorders with depressive symptoms (F43.20–F43.21). Data were anonymised and sent to the study centre for statistical analysis. Since the analysis of routine data for quality assurance reasons is a legal obligation according to German healthcare laws, it was not necessary to obtain informed consent from every patient.
Hospital sample
To draw representative conclusions, hospitals in different regions, of various type and size were chosen (Table 1). Owing to differences in average number of admissions and for internal organisational reasons, the number of recruited patients differed between hospitals. Half of the patients (50.2%, n=603) were treated in state psychiatric hospitals, 28.6% (n=344) in general hospitals and 21.2% (n=255) in university hospitals. About half of the sample (48.3%) was treated in north Germany and about half (51.7%) in south Germany.
Table 1 Hospital sample chosen for inclusion in the study
| Hospital type | Town | Region | Patients included in the study, n (% of total sample) |
|---|---|---|---|
| University hospital | Freiburg | South | 163 (13.6) |
| Münster | North | 92 (7.7) | |
| State psychiatric hospital | Bayreuth | South | 123 (10.2) |
| Düsseldorf1 | North | 144 (12.0) | |
| Offenburg | South | 94 (7.8) | |
| Weinsberg | South | 150 (12.5) | |
| Wiesloch | South | 92 (7.7) | |
| General hospital | Gelsenkirchen | North | 150 (12.5) |
| Gummersbach | North | 118 (9.8) | |
| Oberhausen | North | 76 (6.3) |
Hospitals were invited to cooperate voluntarily in this study. They were asked to use the documentation tools to recruit 150 patients. They had the benefit of detailed comparative feedback (‘benchmarking’) on their treatment routine.
Adherence to guidelines
To evaluate adherence to guidelines, we selected some high-priority guideline recommendations for treatment of in-patient depression (Table 2) and compared these with treatment routine as assessed in this study. Since there are a variety of national and international guidelines for treatment of depression, we chose the internationally accredited American Psychiatric Association guidelines (American Psychiatric Association, 2000) as well as the nationally accepted German DGPPN guidelines (Deutsche Gesellschaft für Psychiatrie, Psychotherapie und Nervenheilkunde, 2000). To ensure that we had specified updated recommendations, we also considered current literature (Reference Furukawa, Steiner and YoungFurukawa et al, 2002; Reference Smith, Dempster and GlanvilleSmith et al, 2002; Reference Benkert and HippiusBenkert & Hippius, 2003; Reference Guaiana, Barbui and HotopfGuaiana et al, 2003; UK ECT Review Group, 2003). Psychotherapy was defined as at least one individual or group session with a psychotherapeutic rationale.
Table 2 Guideline recommendations for the treatment of depression in in-patients
| Aspect of treatment | Recommendation |
|---|---|
| General treatment strategy | Pharmacotherapy: patients with moderate-to-severe depression, recurrent depressive disorder1,2 |
| Additional psychotherapy: psychosocial stressors, comorbid axis II disorder1,2 | |
| Prescription of antidepressants | First choice: tricyclic antidepressants, SSRIs or antidepressants such as mirtazapine, venlafaxine and reboxetine1,2 |
| MAOIs only for non-responders (side-effects, dietary restrictions) Venlafaxine > SSRIs, tricyclics3 | |
| SSRIs=tricyclics4 | |
| Antidepressant dosage1,5 | Tricyclics and tetracyclics |
| Amitriptyline 180-300 mg/day, clomipramine 100-250 mg/day, doxepine, imipramine, trimipramine, desipramine 100-300 mg/day, nortriptyline 50-200 mg/day, maprotiline 100-400 mg/day | |
| SSRIs | |
| Citalopram, fluoxetine, paroxetine 20-60 mg/day, fluvoxamine 50-300 mg/day, sertraline 50-200 mg/day | |
| Other antidepressants | |
| Mirtazapine 15-45 mg/day, venlafaxine 75-375 mg/day, reboxetine 8-12 mg/day | |
| MAOIs | |
| Phenelzine 15-90 mg/day, tranylcypromine 30-60 mg/day, moclobemide 300-600 mg/day | |
| Prescription of benzodiazepines | Benzodiazepines only for acute treatment (risk of dependence, accident proneness)1,2,6 |
| No benzodiazepines for patients with comorbid drug addiction1 | |
| Application of ECT | ECT as an effective treatment for patients with depression with severe or psychotic symptoms1,2,7 |
| Psychotherapeutic rationale | First choice: cognitive—behavioural therapy or interpersonal therapy1,2 |
Statistical analysis
We used different measures to analyse therapy outcome. Individual effect sizes d were calculated for the expert-rated level of depression (HRSD) by taking individual differences in scores before and after treatment and then dividing them by the pooled standard deviation. According to Cohen (Reference Cohen1988), effect sizes can be classified into small (d < 0.40), medium (0.40 < d < 0.80) and high (d > 0.80). Response to treatment was defined according to Jacobson et al (Reference Jacobson, Follette and Revenstorf1984) with the reliable change index (RCI). We calculated RCIs for each patient by dividing the difference between expertrated level of depression (HRSD) at admission and discharge by the standard error of measurement
![]() \batchmode \documentclass[fleqn,10pt,legalpaper]{article} \usepackage{amssymb} \usepackage{amsfonts} \usepackage{amsmath} \pagestyle{empty} \begin{document} \(\mathrm{S}_{\mathrm{E}}(\mathrm{S}_{\mathrm{E}}=\mathrm{s}.\mathrm{d}._{1}{\surd}(1-r_{\mathrm{xx}^{{^\prime}}})\) \end{document}
, with s.d.1=standard deviation of HRSD score at admission and r
xx′=test–retest reliability of the HRSD). An RCI score > 1.96 indicates statistically reliable improvement (response).
\batchmode \documentclass[fleqn,10pt,legalpaper]{article} \usepackage{amssymb} \usepackage{amsfonts} \usepackage{amsmath} \pagestyle{empty} \begin{document} \(\mathrm{S}_{\mathrm{E}}(\mathrm{S}_{\mathrm{E}}=\mathrm{s}.\mathrm{d}._{1}{\surd}(1-r_{\mathrm{xx}^{{^\prime}}})\) \end{document}
, with s.d.1=standard deviation of HRSD score at admission and r
xx′=test–retest reliability of the HRSD). An RCI score > 1.96 indicates statistically reliable improvement (response).
Group differences of categorical data were assessed using the χ2 statistic. Group differences of continuous data were examined using analysis of variance (ANOVA). The frequency distribution of length of stay, ZUF–8, HRSD and BDI scores did not follow a normal distribution. Therefore non-parametric tests such as the Mann–Whitney U-test, Wilcoxon and Kruskal–Wallace H-test were used to analyse differences between groups.
Since a considerable number of BDI self-ratings were lacking (BDI at admission, 15.4%; BDI at discharge, 28.6%), we quoted the number of missing cases separately (Table 3). For the same reason we used the HRSD expert ratings as the main measure of depression.
Table 3 Psychopathology of the patients (n=1202)
| Assessment of depression | Admission | Discharge |
|---|---|---|
| Self-rated level of depression (BDI) | ||
| Mean (s.d.) | 26.9 (11.7)1 | 11.5 (10.0)2 |
| Median | 27.0 | 9.0 |
| None (BDI < 11): n (%) | 84 (7.0) | 495 (41.2) |
| Mild to moderate (BDI 11-17): n (%) | 158 (13.1) | 190 (15.8) |
| Severe (BDI > 18): n (%) | 782 (65.1) | 179 (14.9) |
| Missing data: n (%) | 178 (14.8) | 338 (28.1) |
| Expert-rated level of depression (HRSD) | ||
| Mean (s.d.) | 22.8 (8.9) | 7.1 (6.3) |
| Median | 22.0 | 6.0 |
| None (HRSD < 7): n (%) | 20 (1.8) | 696 (63.4) |
| Mild (HRSD 7-17): n (%) | 308 (27.7) | 323 (29.4) |
| Moderate (HRSD 18-24): n (%) | 345 (31.1) | 55 (5.0) |
| Severe (HRSD > 24): n (%) | 437 (39.4) | 24 (2.2) |
| Global functioning (GAF)3 | ||
| Mean (s.d.) | 45.8 (13.5) | 70.1 (13.9) |
| Median | 48.0 | 70.0 |
RESULTS
Patients
Socio-demographic characteristics
Data were collected from 1202 patients. The mean age was 50.8 years (s.d.=15.8); 64.0% of the patients were female. Most patients were married or living with a partner (53.8%); 87.0% had German as a first language. Most patients had 9 years of school education (47.0%); 24.0% had 10 years and 20.9% had 13 years. There were significant differences between hospitals concerning age (ANOVA, F=13.2, d.f.=9,1174, P < 0.001), marital status (χ2=123.8, d.f.=45, P < 0.001), first language (χ2=58.8, d.f.=18, P < 0.001) and level of school education (χ2=190.2, d.f.=45, P < 0.001).
Psychopathology
Average levels of depression at admission were high according to self-ratings (BDI, mean=26.9, s.d.=11.7, median=27.0) and moderate according to expert ratings (HRSD, mean=22.8, s.d.=8.9, median=22.0; Table 3).
The levels of self-rated and expert-rated depression at admission were correlated (Spearman's r=0.43, P < 0.001). The level of depression at admission differed significantly between hospitals, with the mean HRSD score ranging from 15 to 29 (χ2=151.2, d.f.=9, P < 0.001). Global functioning (GAF) was restricted at admission (mean=45.8; s.d.=13.5, median=48.0; Table 3) and also differed between hospitals (range 38.3–53.5; χ2=111.2, d.f.=9, P < 0.001). Of those included in the study, 27.3% had fallen ill in the year of admission.
The two most frequent diagnoses were single depressive episode (42.0%) and depressive episode within recurrent depressive disorder (40.0%), followed by adjustment disorder (12.2%), depressive episode within bipolar depressive disorder (4.8%) and dysthymia (1.1%). Psychiatric comorbidity was reported for 25.1% of patients, with drug addiction problems (12.0%), axis II disorders (6.3%) and anxiety disorders (6.0%) as the largest diagnostic groups (World Health Organization, 1993). The highest rate of psychiatric comorbidity was found for patients with dysthymia (58.3%), followed by patients with recurrent depressive disorder (28.5%). Comorbid physical illness was found in 33.5% of the total sample, with the highest rate for patients with recurrent depressive disorder (40.5%), followed by patients with bipolar depressive disorder (37.9%). Vascular disease (17.7%) was the most frequent reported category, followed by nutritional and metabolic disorders (10.2%) and orthopaedic diseases (5.6%; World Health Organization, 1993).
Treatment process
General treatment strategy
Most patients (n=982, 81.7% of the total sample) were treated with a combination of pharmacotherapy and psychotherapy. A combination of pharmacotherapy, psychotherapy and electroconvulsive therapy (ECT) was used for 53 patients (4.4% of the total sample). Of the 782 patients with moderate-to-severe depression (HRSD > 17), 95.8% received pharmacotherapy; 91.9% of the 160 patients with severe acute stressors and 93.4% of the 76 patients with comorbid axis II disorder were treated with psychotherapy.
Prescription of antidepressants
A total of 93.4% of the sample received pharmacotherapy during in-patient treatment. Of those, 94.1% were discharged with antidepressant medication. As shown in Table 4, the most frequently prescribed antidepressants were mirtazapine, venlafaxine and reboxetine (47.8% of patients receiving pharmacotherapy), followed by selective serotonin reuptake inhibitors (SSRIs) (30.2%) and tri- and tetracyclics (26.6%). Monoamine oxidase inhibitors (MAOIs) were prescribed rarely (2.8%) and not to first-episode patients. For 17.5% of patients, more than one antidepressant had been prescribed.
Table 4 Antidepressive medication at discharge (multiple answers possible)
| Group of antidepressants | Generic name | Patients receiving pharmacotherapy, % (n=1123) | Adequate dosage decisions, % |
|---|---|---|---|
| Tri-/tetracyclics | Amitriptyline, clomipramine, imipramine, trimipramine, desipramine, doxepin, lofepramine, dosulepin, opipramol, dibenzepine, maprotiline, mianserin | 26.6 | 76 |
| SSRIs | Fluoxetine, fluvoxamine, sertraline, paroxetine, citalopram | 30.2 | 98 |
| Other antidepressants | Reboxetine, nefazodone, mirtazapine, venlafaxine | 47.8 | 81 |
| MAOIs | Moclobemide, tranylcypromine | 2.8 | 67 |
The proportion of patients discharged with antidepressants (χ2=23.0, d.f.=9, P=0.006) and the prescription of different antidepressant groups differed between hospitals (tricyclics: χ2=54.5, d.f.=9, P < 0.001 (Fig. 2); SSRIs: χ2=135.9, d.f.=9, P < 0.001; other antidepressants: χ2=44.4, d.f.=9, P < 0.001; MAOIs: χ2=51.8, d.f.=9, P < 0.001).

Fig. 2 Proportion of patients taking tri-/tetracyclic antidepressants at discharge.
Dosage of antidepressants
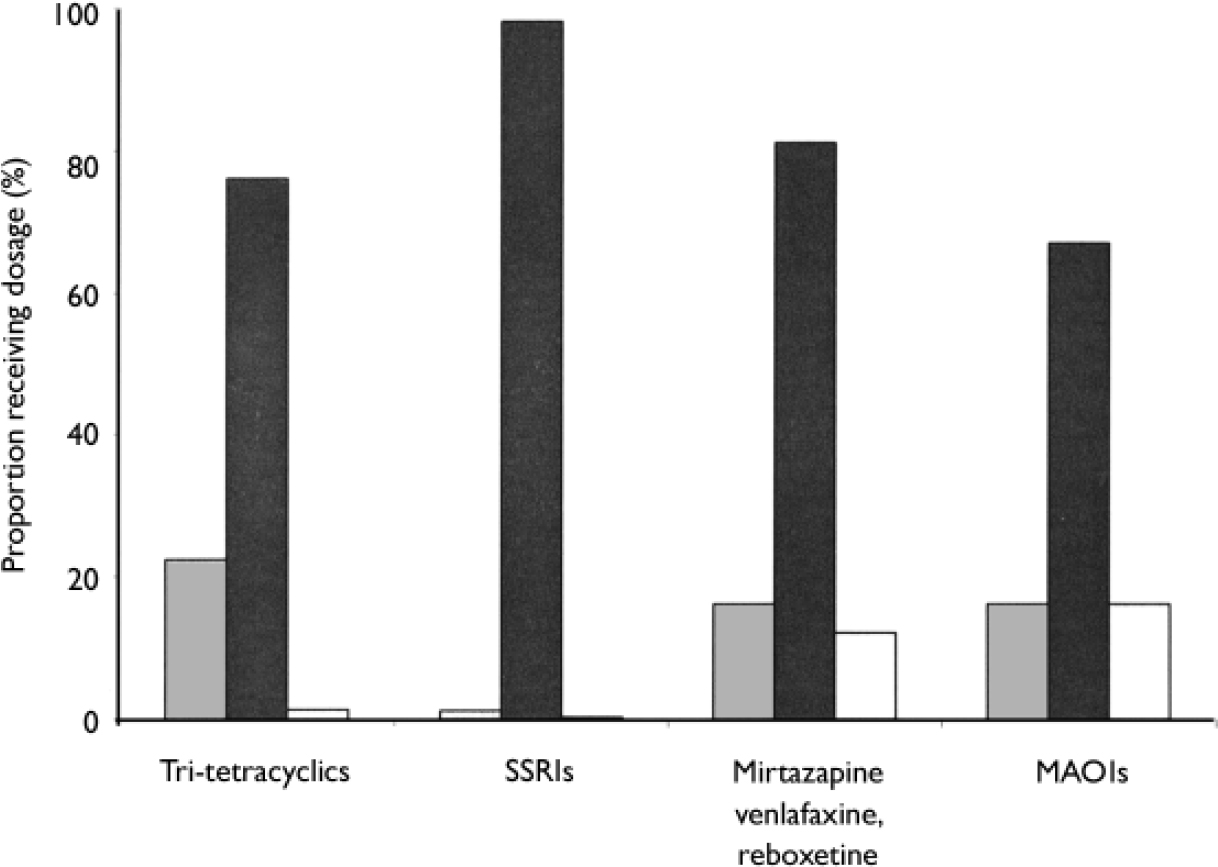
Following guideline recommendations (Table 2), we classified each antidepressant dosage decision at discharge into either adequate, below recommendation or above recommendation. In 85% of cases antidepressant dosage at discharge was in line with guideline recommendations. Nearly every SSRI dosage decision (98.0%) was adequate, whereas adherence to guidelines for dosage was lower for antidepressants such as mirtazapine, venlafaxine and reboxetine (81.0%), tri-/tetracyclics (76.0%) and MAOIs (67.0%; Table 4). As shown in Fig. 3, tri-/tetracyclics tended to be prescribed below recommended doses (22.4%), antidepressants such as mirtazapine, venlafaxine and reboxetine tended to be prescribed above recommended doses (12.1%). Monoamine oxidase inhibitors were prescribed both below and above guideline recommendations (16.1% respectively). The average percentage of guideline-adherent dosage decisions for antidepressants differed between hospitals (ANOVA, F=2.9, d.f.=9,1045, P=0.002).
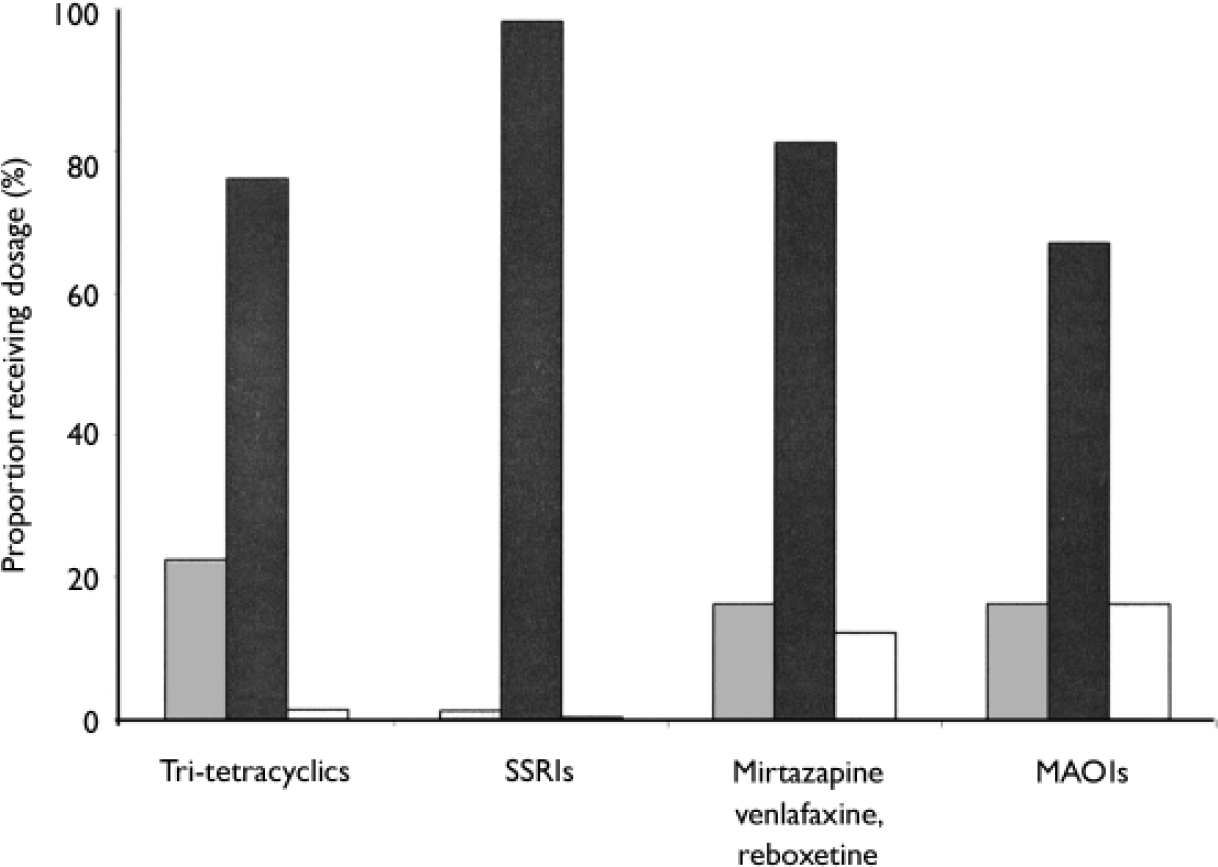
Fig. 3 Adherence to guidelines for antidepressant dosage. ![]() , Below recommendation; ▪, adequate; □, above recommendation; SSRI, selective serotonin reuptake inhibitor; MAOI, monoamine oxidase inhibitor.
, Below recommendation; ▪, adequate; □, above recommendation; SSRI, selective serotonin reuptake inhibitor; MAOI, monoamine oxidase inhibitor.
Prescription of benzodiazepines
Of the patients receiving pharmacotherapy, 189 (16.8%) were discharged with benzodiazepines; the proportion receiving benzodiazepines differed between hospitals (range 1.1–56.0%, χ2=325.6, d.f.=9, P < 0.001). One-fifth of the patients with comorbid substance misuse were prescribed benzodiazepines at discharge (19.4%). For 42.9% of those with comorbid substance misuse discharged with benzodiazepines, subsequent out-patient psychiatric treatment was arranged.
Electroconvulsive therapy
Electroconvulsive therapy was given to 5.2% of patients. Of the 437 with severe depressive symptoms at admission (HRSD > 24), 24 (5.5%) received ECT. Out of 108 psychotic patients, 9 (8.3%) were treated with ECT. There is a difference between hospitals concerning the application of ECT (χ2=286.5, d.f.=9, P < 0.001): four of the ten participating hospitals did not use ECT at all. Further investigation revealed that three of those four hospitals have ECT facilities but do not offer this treatment to patients with depression because of ethical considerations and low demand by patients.
Psychotherapeuqtic rationale
A total of 1105 patients (91.9% of the total sample) received psychotherapy during inpatient treatment. Cognitive–behavioural therapy was most frequently applied (57.1% of psychotherapy patients), followed followed by psychodynamic therapy (22.8%), client-centred therapy (9.9%) and interpersonal therapy (8.8%). The ten hospitals differed with respect to the proportion of patients receiving psychotherapy (χ2=118.3, d.f.=9, P < 0.001) as well as psychotherapeutic rationale (χ2=137.0, d.f.=9, P < 0.001).
Outcome
The mean duration of in-patient treatment was 49.5 days (s.d.=40.5, range 3–385), with significant differences between hospitals (χ2=81.7, d.f.=9, P < 0.001). The average level of global functioning (GAF) of the patients increased significantly during in-patient treatment from 45.8 (s.d.=13.5) to 70.2 (s.d.=13.8) at discharge (Z=-28.2, P < 0.001). The mean self-rated level of depression (BDI) decreased from 27.0 (s.d.=11.6) to 11.4 (s.d.=10.0, Z=-23.2, P < 0.001), the mean expertrated level of depression (HRSD) from 22.8 (s.d.=8.9) to 7.1 (s.d.=6.3, Z=-28.2, P < 0.001; Table 3). The response ratio for the level of depression (RCI (HRSD) > 1.96) was 76.9%. Two patients (0.2%) deteriorated during treatment (RCI (HRSD) < -1.96). The average effect size d for expert-rated level of depression (HRSD) was 2.1 (s.d.=1.2). Hospitals differed with respect to the mean level of depression at discharge (HRSD range 4.5–9.7, χ2=120.4, d.f.=9, P < 0.001) and the depression effect sizes (χ2=88.1, d.f.=9, P < 0.001). Only 866 out of 1202 patients (72%) rated their satisfaction with treatment at discharge. Of those patients, 85.9% were satisfied.
Adherence to guidelines and outcome
There are significant differences between responders (RCI (HRSD) > 1.96) and non-responders (RCI (HRSD) < 1.96) with respect to adherence to treatment guidelines (Table 2). Patients with a comorbid axis II disorder who received psychotherapy were more likely to respond to treatment (84% responders) than axis II patients who had not received psychotherapy (61.1% responders, χ2=4.0, d.f.=1, P < 0.05). Adherence to treatment guidelines for tricyclic antidepressant dosage made a difference to treatment response among patients receiving tricyclic medication (χ2=6.6, d.f.=1, P < 0.05), with a higher rate of correct tricyclic dosage decisions in the response group (78.3%) than in the non-response group (60.8%). The mean duration of treatment of those with comorbid substance misuse given benzodiazepines at discharge was significantly shorter (n=28, mean=32.1 days, range=5–124) than the mean duration of treatment of similar patients not receiving benzodiazepines at discharge (n=116, mean=49.1 days, range 4–163, U=1030.0, P=0.003). The response rates among patients given psychotherapy were higher for interpersonal therapy (84.5%) and cognitive–behavioural therapy (83.2%) than for client-centred therapy (70.7%) or psychodynamic therapy (69.1%, χ2=25.2, d.f.=8, P=0.001).
DISCUSSION
The large sample of patients is comparable to other national and international samples of in-patients with depression in terms of socio-demographic variables and psychopathology at admission (Reference Keller, Lavori and RiceKeller et al, 1986; Reference Simon, Lin and KatonSimon et al, 1995; Reference Ackerman, Unutzer and GreenlandAckerman et al, 2002; Reference Härter, Sitta and KellerHärter et al, 2004). The investigation was carried out in the German in-patient healthcare system, which is especially well suited for the study of this question since hospital admission is free of any direct cost to the patient in Germany.
Treatment outcome
The mean treatment outcome was high: the effect sizes (d=1.5) for BDI expert rating and for HRSD self-rating (d=2.3) can be considered large (Reference CohenCohen, 1988). Most patients showed a significant decrease in the level of depression during treatment (76.9%) and only two patients deteriorated. The results are comparable with other evaluation studies of depression treatment in Germany (Reference Hautzinger and de Jong-MeyerHautzinger & deJong-Meyer, 1996; Reference Härter, Sitta and KellerHärter et al, 2004). The decrease in psychopathology and in global functioning during in-patient treatment is not only statistically but also clinically significant. The average global functioning at discharge (GAF=70.2) can be described as having ‘some mild symptoms or some difficulty in social, occupational or school functioning, but generally functioning pretty well…’ (American Psychiatric Association, 1994, p. 759), justifying discharge from in-patient treatment. The mean depression score at discharge was on a threshold towards a non-clinical level of depression (BDI=11.5, HRSD=7.1). Many patients were satisfied with treatment (85.9%). Nevertheless, since self-report data on patients’ satisfaction are missing for 28.1% of patients, interpretation is limited. There might have been a selection effect of extraordinarily compliant patients.
Adherence to treatment guidelines
General therapeutic strategies have mainly been chosen according to guideline recommendations (Table 2). Most patients with moderate-to-severe depression received pharmacotherapy (95.8%). Psychotherapy can be considered a second core element of German in-patient treatment of depression. Most patients with a comorbid axis II disorder (93.4%) or acute stressors (91.9%) were treated with psychotherapy, according to guideline recommendations.
The results also reflect a routine of antidepressant prescribing which is highly concordant with guideline recommendations (Table 2). Only 2.8% of the sample and no first-episode patients were prescribed MAOIs but a large number of patients received at least one of the recommended antidepressants – SSRIs, tri-/tetracyclics or antidepressants such as mirtazapine, venlafaxine and reboxetine (Table 4). The preference for antidepressants such as mirtazapine, venlafaxine and reboxetine over SSRIs and tri-/tetracylics corresponds to the prescription trends in the USA (Reference Ackerman, Unutzer and GreenlandAckerman et al, 2002).
The results concerning dosage of antidepressants give an optimistic picture for the in-patient setting compared with international and out-patient findings. Only 15% of decisions regarding antidepressant dosage did not satisfactorily meet guideline recommendations (Table 2, Fig. 3). Studies from the USA (e.g. Reference Dawson, Lavori and CoryellDawson et al, 1999) have reported that up to 50% of antidepressant dosages were not in accordance with recommendations. For out-patient settings, similar rates were reported (44%), with worse treatment outcome for patients receiving too low a dosage of antidepressants (Reference Simon, Lin and KatonSimon et al, 1995).
The high rate of benzodiazepine prescribing at discharge (up to 56%) is a point for discussion. Combination therapy with benzodiazepines is said to decrease dropout rates but at the same time there are concerns about dependence and accident proneness (Reference Furukawa, Steiner and YoungFurukawa et al, 2002). Treatment guidelines advise clearly against benzodiazepines for patients with comorbid drug addiction. In contrast, almost 20% of this subgroup were still taking benzodiazepines at discharge. The duration of treatment may account for this deviation from guideline recommendations. Possibly benzodiazepine withdrawal had not yet been completed and benzodiazepines may have been continued in subsequent out-patient treatment. The fact that only half of the patients with comorbid drug addiction and benzodiazepine prescription at discharge continued out-patient treatment does not support this assumption.
The data reflect a restricted routine use of ECT in Germany. This is not in line with guideline recommendations and research findings that showed ECT to be an effective treatment for patients with severe and psychotic symptoms and those not responding to antidepressant medication (American Psychiatric Association, 2000; UK ECT Review Group, 2003). These results are in accordance with Müller et al (Reference Müller, Klimke and Janner1998), who showed that the application of ECT in German hospitals was much more influenced by social factors and psychiatrists’ attitudes than by medical factors.
According to guideline recommendations (Table 2), cognitive–behavioural therapy and interpersonal therapy are the most effective specific treatment strategies for major depressive disorder. While cognitive–behavioural therapy was the most applied therapeutic modality in the present study, interpersonal therapy still seems to be relatively unknown in German psychiatric hospitals.
Our results emphasise the importance to outcome of adherence to treatment guidelines. Adherence to guidelines for tricyclic antidepressant dosage, psychotherapeutic treatment and cognitive–behavioural and interpersonal therapy as main therapeutic rationales seems to correspond to higher response rates.
Methodological issues
There was a difference between self- and expert-rated levels of depression in this study, indicating the importance of different methods of assessment in the treatment of depression. As in out-patient settings, patients seemed to rate themselves as more depressed than their therapists did (Reference Schneider, Kratz and BermejoSchneider et al, 2004). Unfortunately many self-rating data are missing and hence the validity is restricted.
Significant differences between hospitals were found with respect to patients’ characteristics at admission (‘case mix’) as well as variables of treatment process and outcome. This corresponds with a number of other studies (e.g. Reference Härter, Sitta and KellerHärter et al, 2004) and suggests that fair comparisons of treatment process and outcome between hospitals can only be conducted by statistically considering the case mix.
There are different definitions of adherence to guidelines in the current literature. In a Dutch study by Tiemeier et al (Reference Tiemeier, de Vries and van het Loo2002), adherence to guidelines for psychiatric treatment was assessed using vignettes. Adherence was defined by an expert panel based on the three leading Dutch guidelines, resulting in 73% guideline-adherent intentions-to-treat by the participating psychiatrists. Fortney et al (Reference Fortney, Rost and Zhang2001) found only 29% of an American sample of out-patients with depression to be treated according to guidelines. In that study adherence to guidelines was defined as antidepressant medication corresponding with Agency for Healthcare Research and Quality guidelines or as a certain number of visits to a specialist health provider. Since psychiatric treatment is a complex phenomenon, with many variables influencing treatment process and outcome (Reference Frick, Rehm and KrischkerFrick et al, 1999; Reference Sitta, Härter and BrandSitta et al, 2003), and the specificity of guideline recommendations is limited, a single score for adherence to guidelines seems too restrictive. For that reason we selected single guideline recommendations to verify the recommendations in real clinical settings. Even this method does not compare with real-life settings since differences between hospitals became obvious. The question ‘To what extent is in-patient depression treatment adherent to guidelines?’ should be rephrased as ‘How does a psychiatric hospital deal with specific guideline recommendations with respect to specific groups of patients?’ Our results as well as the results of Tiemeier et al (Reference Tiemeier, de Vries and van het Loo2002) and Fortney et al (Reference Fortney, Rost and Zhang2001) may be a useful starting point for quality management since they focus on single treatment aspects.
In order to effectively improve the quality of treatment for in-patients with depression, there is a need to:
-
(a) assess various aspects of treatment quality;
-
(b) provide individual feedback for single hospitals;
-
(c) compare with other hospitals (‘benchmarking’) by statistically considering differences in the case mix to allow hospitals to orient themselves towards models of best practice;
-
(d) develop individual quality management strategies.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
• German treatment of depression in in-patients is of a high standard.
-
• Areas of improvement include the dosage of tricyclic antidepressants, the prescription of benzodiazepines, the application of electroconvulsive therapy and interpersonal therapy.
-
• Since hospitals differ with respect to treatment process and outcome, quality management strategies should be individualised.
LIMITATIONS
-
• Self-ratings of depression are missing for a considerable number of patients.
-
• Interpretation of treatment outcome is restricted since we did not collect follow-up data.
-
• We describe general trends for treatment of depression in German in-patients with respect to single guideline recommendations. Further analyses of therapeutic strategies for certain subgroups of patients or combinations of strategies are overdue.
Acknowledgements
This study was supported by the German Ministry for Education and Research (BMBF; 01GI9922 and 01GI9923) and the German Research Network on Depression and involved the collaboration of ten German psychiatric hospitals. We thank R.-D. Stieglitz (Basel), E. Klieser (Gelsenkirchen), H. Mecklenburg (Gummersbach), V. Arolt (Münster), H. Bongardt (Oberhausen), T. Gollik (Offenburg), H.-J. Luderer (Weinsberg) and M. Schwarz (Wiesloch) for support.









eLetters
No eLetters have been published for this article.