According to the DSM-V (American Psychiatric Association, 2013) obsessive-compulsive disorder (OCD) is characterized by obsessions and compulsions that interfere with a person’s normal life. OCD is suffered not only by adult people, but also by children and adolescents, and its impact on the patients’ lives can be severe. OCD causes considerable interference in children’s activities (play, academic tasks, social life, etc.) due to the enormous amount of time lost that compulsions generate (Taylor, Reference Taylor2011; Valderhaug & Ivarsson, Reference Valderhaug and Ivarsson2005). Prevalence rates reported by some studies in the child and adolescent population have reached figures around 2%, some even reaching 4% (Rapoport et al., Reference Rapoport, Inoff-Germain, Weissman, Greenwald, Narrow, Jensen and Canino2000; Zohar, Reference Zohar1999). In addition, OCD is often associated with other psychological disorders, such as tics, attention deficit-hyperactivity disorder, or depression, which increase the degree of discomfort and complicate its treatment and prognosis (Storch, Larson et al., Reference Storch, Lehmkuhl, Ricketts, Geffken, Marien and Murphy2010).
In recent years, pediatric OCD has received increased attention from clinicians and researchers, leading to an improvement of assessment measures and treatments (Krebs & Heyman, Reference Krebs and Heyman2010). Cognitive-behavioral therapy (CBT) has been the most investigated treatment model, exposure with response prevention (ERP) being the main component. The efficacy of ERP seems to be similar whether it is applied alone or in combination with other techniques, at least in adults (Rosa-Alcázar, Sánchez-Meca, Gómez-Conesa, & Marín-Martínez, Reference Rosa-Alcázar, Sánchez-Meca, Gómez-Conesa and Marín-Martínez2008). The treatment components that most frequently accompany ERP are psychoeducation (March & Mulle, Reference March and Mulle1998), family-based treatments with parent training (Barrett, Healy-Farrell, & March, Reference Barrett, Healy-Farrell and March2004; Freeman et al., Reference Freeman, Garcia, Coyne, Ale, Przeworski, Himle and Leonard2008), intervention in narrative context (March & Mulle, 1998; Wagner, Reference Wagner2003), and cognitive or anxiety management techniques with the use of age appropriate metaphors to facilitate cognitive restructuring (Barrett et al., Reference Barrett, Healy-Farrell and March2004; March & Mulle, 1998; Pediatric OCD Treatment Study [POTS] Team, 2004; Piacentini & Langley, Reference Piacentini and Langley2004).
Empirical studies conducted on pediatric OCD have examined the efficacy of treatments in different modalities. For example, there have been no relevant differences observed between individual and group CBT, with efficacy figures ranging between 61% and 65% for both modalities (Barrett et al., Reference Barrett, Healy-Farrell and March2004). Similarly, intensive CBT seems to be as efficacious as CBT applied in a longer format (Franklin et al., Reference Franklin, Kozak, Cashman, Coles, Rheingold and Foa1998; Storch, Geffken et al., Reference Storch, Geffken, Merlo, Mann, Duke, Munson and Goodman2007). CBT has been investigated with the inclusion of certain modifications, such as telephone format (Turner, Heyman, Futh, & Lovell, Reference Turner, Heyman, Futh and Lovell2009), community-based CBT (Farrell, Schlup, & Boschen, Reference Farrell, Schlup and Boschen2010), or web-camera delivered CBT (Storch et al, Reference Storch, Caporino, Morgan, Lewin, Rojas, Brauer and Murphy2011). However, the differential efficacy between the components of CBT has not received much attention. Only the study by Simons, Schneider, and Herpertz-Dahlmann, (2006) has compared the benefits of ERP and meta-cognitive therapy, finding non-significant differences.
Some studies have examined the efficacy of family-based programs, finding improvement percentages of around 25–65% (Barrett et al., Reference Barrett, Healy-Farrell and March2004; Farrell et al., 2010; Piacentini & Langley, Reference Piacentini and Langley2004; Scahill, Vitulano, Brenner, Lynch, & King, Reference Scahill, Vitulano, Brenner, Lynch and King1996; Valderhaug, Larsson, Götestam, & Piacentini, Reference Valderhaug, Larsson, Götestam and Piacentini2007; Waters, Barrett, & March, Reference Waters, Barrett and March2001). In addition, some reviews point towards the existence of significant differences between fathers and mothers according to gender, age of children (Bögels & Phares, Reference Bögels and Phares2008), and parental style dimensions (McLeod, Wood, & Weisz, Reference McLeod, Wood and Weisz2007). Creswell and Cartwright-Hatton (Reference Creswell and Cartwright-Hatton2007) indicated the convenience of family-based CBT for child anxiety when parents show high levels of this problem.
Several qualitative reviews on pediatric OCD treatment have tried to classify psychological interventions according to Evidence-Based-Treatment criteria proposed by Chambless, Baker, Baumon, Beutler, and Calhoun (Reference Chambless, Baker, Baucom, Beutler and Calhoun1998) and Chambless and Hollon (Reference Chambless and Hollon1998). Thus, Barrett, Farrell, Pina, Peris, and Piacentini (Reference Barrett, Farrell, Pina, Peris and Piacentini2008) concluded that individual exposure-based CBT can be considered as a probably efficacious treatment and that family-based CBT, both in individual or group format, can be considered as a possibly efficacious treatment as well. Barrett et al. (Reference Barrett, Farrell, Pina, Peris and Piacentini2008) also pointed some limitations of the primary studies, such as the comorbidity and the heterogeneity and small size of the samples. Krebs and Heyman (Reference Krebs and Heyman2010) reported that in cases with refractory OCD relevant variables such as comorbidity, family factors and symptom-related characteristics must be addressed, since these may hinder the treatment efficacy. Finally, in the American Academy of Child and Adolescent Psychiatry (AACAP) Committee on Quality Issues (2012) CBT is recommended as the first choice when OCD presents mild to moderate severity, whereas selective serotonin reuptake inhibitors (SSRIs) combined with CBT are indicated for moderate to severe cases.
Review of previous meta-analyses
There have been published four meta-analyses on the efficacy of psychological interventions in pediatric OCD (Abramowitz, Whiteside, & Deacon, Reference Abramowitz, Whiteside and Deacon2005; Freeman et al., Reference Freeman, Choate-Summers, Moore, Garcia, Sapyta, Leonard and Franklin2007; O’Kearney, Reference O'Kearney2007; Watson & Rees, Reference Watson and Rees2008). Abramowitz et al. (Reference Abramowitz, Whiteside and Deacon2005) identified 18 articles, published between 1983 and 2004, that included 10 ERP groups, 10 pharmacotherapy groups, and seven placebo control groups. The effect size index was the standardized pretest-posttest mean change for each group. For the obsessive-compulsive measures, a mean effect d = 1.98 was obtained for the ERP groups and d = 0.48 for the placebo control groups, both of them reaching statistical significance. Following Cohen’s (Reference Cohen1988) criterion to interpret the magnitude of the d indices, ERP treatment exhibited a large magnitude (over 0.8), whereas the placebo control showed a medium magnitude (about 0.5). In addition, a combined effect size was calculated for the anxiety and depression measures, obtaining a mean d = 0.48 for ERP (four groups) and d = 0.06 for control groups (four groups), none of which were statistically significant.
Freeman et al. (Reference Freeman, Choate-Summers, Moore, Garcia, Sapyta, Leonard and Franklin2007) integrated 12 CBT groups, published between 1983 and 2005, and calculated the same effect size index as that used in Abramowitz et al. (Reference Abramowitz, Whiteside and Deacon2005) to estimate treatment efficacy in reducing obsessive-compulsive symptoms. Assuming a random-effects model, they obtained a mean d = 1.55, which was statistically significant. They also calculated mean effects separately for individual CBT, d = 1.77 (seven groups), group CBT, d = 0.76 (three groups), and family-based CBT, d = 1.88 (two groups), concluding that individual and family-based CBT seem to be the most promising treatments of pediatric OCD.
O’Kearney (Reference O'Kearney2007) recovered 19 articles, published between 1983 and 2007, five of which were comparison studies and 14 were one-group studies. For the one-group studies, the same d index defined in the two previous meta-analyses was calculated, with d indices for obsessive-compulsive measures ranging between 0.78 and 3.49. Due to the large variability shown by the effect estimates, a mean effect was not calculated in the study. O’Kearney (Reference O'Kearney2007) considered the effect estimates obtained from the one-group studies as overestimations of the true treatment effect due to the low internal validity of these designs. In order to correct the effect estimates, he adjusted the d indices of the one-group studies by the mean d index obtained with the control groups, concluding that, on average, the mean effect of CBT is around d = 1. Due to the large number of internal validity threats of the one-group studies, Watson and Rees (Reference Watson and Rees2008) selected only randomized controlled studies that applied some psychological or pharmacological treatment to children and adolescents with OCD. They selected 12 articles and one unpublished paper (1985–2008) that produced 15 comparisons between a treatment group and a control group, although only five of them engaged CBT. The high methodological quality of the studies included in this meta-analysis allowed the use of an effect size index that controlled the internal validity threats. This effect size was defined as the difference between the pretest-posttest mean changes of the treatment and control groups, divided by the pooled standard deviation of the two groups in the posttest. For the five CBT comparisons, the mean effect was d = 1.45, statistically significant and exhibiting a large magnitude following Cohen’s (Reference Cohen1988) criteria.
In summary, the results obtained in the four meta-analyses carried out to date about the efficacy of CBT for pediatric OCD point towards ERP as the main treatment component and towards individual and family-based CBT as the most promising treatment modalities.
Objectives of the study
The previous meta-analyses have shown that CBT exhibits great efficacy in children and adolescents with OCD, although their effect estimates vary depending on the effect size index used. The scarce number of controlled studies that assess the efficacy of CBT on pediatric OCD led us to include one-group studies in the meta-analysis, in spite of their internal validity problems. As a consequence, assessments of the risk of bias in the effect estimates need to be addressed. The purpose of this research was to carry out a meta-analysis on the efficacy of psychological treatments in pediatric OCD to determine the current status and future directions in the field. Our meta-analysis offers some improvements to those previously published on this topic. First, one objective not addressed in the previous meta-analyses was to tentatively explore the differential efficacy of the different components that CBT can include, such as ERP, cognitive restructuring, psychoeducation, anxiety management training, problem-solving strategies, relapse prevention, behavioral experiments, etc. With this purpose, a tentative model was proposed in order to explore the most relevant treatment components on pediatric OCD with the aim to guide future experimental research on this topic. Second, in addition to obsessive-compulsive symptoms, we have examined the treatment effects on other outcome measures, such as anxiety, depression, family adaptation, functional impairment, and other measures. Only Abramowitz et al. (Reference Abramowitz, Whiteside and Deacon2005) computed a combined effect size for anxiety and depression symptoms. Third, the effect sizes were calculated in the posttest and in the follow-up, allowing us to study both the short-term and the long-term efficacy of the treatments. Fourth, efforts were made to analyze a wide range of treatment, participant, context, methodological, and extrinsic moderator variables that could account for the effect size variability.
Method
Study Selection Criteria
In order to be included in the meta-analysis, studies had to fulfill the following criteria: a) to examine the efficacy of a psychological treatment on a sample of participants younger than 19 years old with a diagnosis of OCD according to standardized diagnostic criteria (e.g., DSM or ICD) and clinician-administered structured clinical interviews (e.g., SCID, ADIS-III, ADIS-IV); b) to include at least one treatment group with pretest and posttest measures and, optionally, follow-up measures; c) the sample size in the posttest should be greater than four participants; therefore, single-case designs were excluded; d) statistical data reported in the study had to allow us to compute the effect sizes, and e) to be written in English or Spanish.
Search strategy
Several literature search procedures were used to locate the studies that could fulfill our selection criteria. First, several electronic databases were consulted: Medline, PsycINFO, PsycARTICLES, Psychology and Behavioral Sciences Collection (PBSC), ERIC, and Google Scholar, as well as the Spanish database CSIC (ISOC). The following keywords were combined, in English and Spanish, in the electronic searches: ([obsessive-compulsive] or [OCD]) and ((treatment) or (cognitive behavioral therapy) or (CBT) or ([exposure response prevention] or [ERP]) and ([pediatric] or [child*] or [adolesce*]), which should be in the title or the abstract. Second, the references of four meta-analyses cited above and six systematic reviews were consulted (Barrett et al., Reference Barrett, Farrell, Pina, Peris and Piacentini2008; Himle, Reference Himle2003; March, Reference March1995; March, Franklin, Nelson, & Foa, Reference March, Franklin, Nelson and Foa2001; Turner, Reference Turner2006; Wolff & Wolff, Reference Wolff and Wolff1991). Third, the references of the located studies were also reviewed. Finally, emails were sent to 22 experts in this area in order to locate unpublished studies. A flow chart of the literature search process is showed in Figure 1.
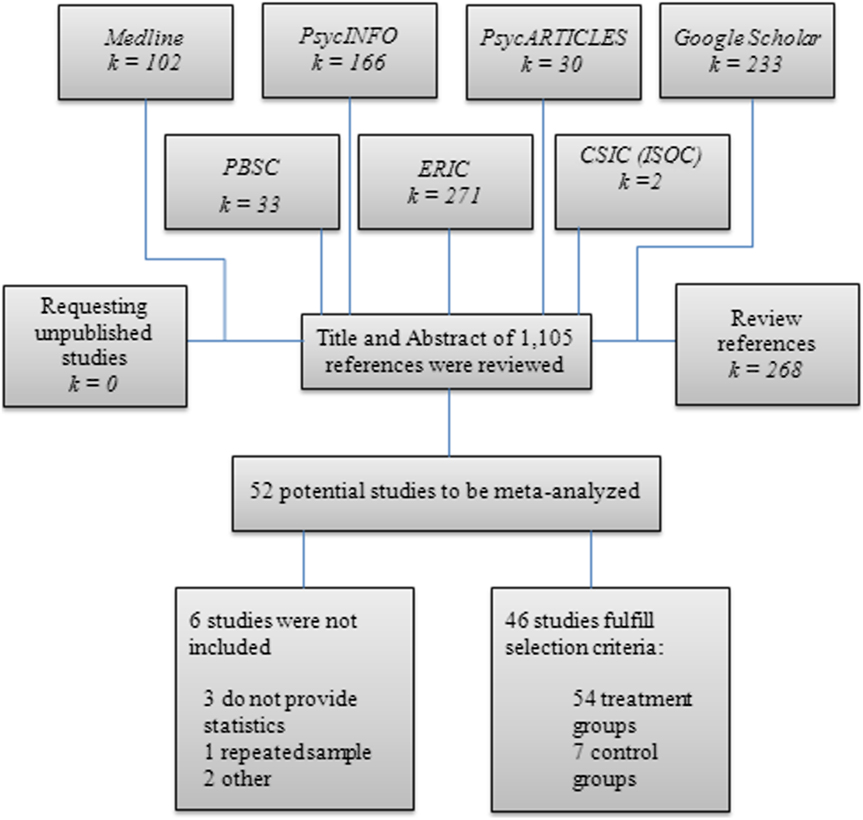
Figure 1. Flow chart of the search strategy and study selection process.
The search strategy produced a total of 1,105 references, finding 46 articles that fulfilled the selection criteria, all of them written in English and published between 1983 and February of 2014. Out of the 46 articles, 28 were one-group studies, 17 were comparison studies with random assignment (seven studies with a control group, ten with alternative CBT groups and medication group,) and one comparison two-groups study. The 46 articles produced a total of 62 groups: 54 groups of participants that received some kind of CBT, one group of psychodynamic therapy, and seven control groups (six nonactive groups and one pill-placebo group). In total, 1,164 participants were included in the posttest measurements (1,051 in the treatment groups and 113 in the control groups), with a median sample size of 15 participants. The studies came from USA (58.7%), United Kingdom (15.2%), Australia (10.9%), Canada (4.3%), Germany (2.2%), Brazil (2.2%), Netherlands (2.2%), Norway (2.2%), and Iran (2.2%). Although we endeavored to locate unpublished studies, all those included in the meta-analysis were published papers.
The degree of overlap, in terms of the number of articles of our meta-analysis that were already been included in each one of the previous ones was 26% with Freeman et al. (Reference Freeman, Choate-Summers, Moore, Garcia, Sapyta, Leonard and Franklin2007) and 34.8% with O´Kearney (Reference O'Kearney2007). In these two meta-analyses only psychological treatments were included. The overlap was even lower when compared our meta-analysis with other meta-analyses that also included pharmacological treatments, such as Watson and Rees (Reference Watson and Rees2008) with 6.5%, or Abramowitz et al. (Reference Abramowitz, Whiteside and Deacon2005) with 19.6%. The minor overlap between our meta-analysis and the previous ones guarantees the originality of our results.
Coding of moderator variables
In order to examine the potential influence of characteristics of the studies on the effect sizes, potential moderator variables were coded. The treatment variables coded were: a) the type of group (treatment versus control); b) the behavioral techniques applied to the participants (psychoeducation, ERP, cognitive restructuring, relapse prevention, behavioral experiments, etc.); c) the type of exposure (in vivo versus in imagination); d) the mode of applying the exposure (therapist-guided, parent-guided, self-exposure, therapist-guided with audiovisual support, parent-guided with audiovisual support, and self-exposure with audiovisual support); e) the treatment duration (number of weeks); f) the treatment intensity (number of weekly hours); g) the treatment magnitude (total number of intervention hours per participant); h) the homogeneity of the treatment (if it was similar for all subjects); i) the inclusion of homework; j) the inclusion of a follow-up program; k) the degree of parental involvement (minimal: parents only received information; moderate: parents attended some sessions, or high: parents attended almost all sessions and were trained to assist children); l) the focus of the intervention (the OCD child or the whole family); m) the mode of CBT (individual versus in group); n) the utilization of a manualized protocol; o) the therapist’s training (psychologist versus psychiatrist); and p) the therapist’s experience (low: graduate students with no experience; moderate: postgraduate students with experience, or high: professionals or faculty members with experience).
Several participant characteristics were also coded: a) the mean age of the sample (in years); b) the gender distribution (percentage of males); c) the mean duration of the OCD (in years); d) whether they had received any previous treatment (somebody versus nobody); and e) the presence of comorbidity (< 50% versus ≥ 50% of the sample). The methodological variables coded were: a) the diagnostic criteria (any version of DSM, ICD or others); b) the control of medication consumption; c) the inclusion of follow-up measures (in months); d) the attrition from pretest to posttest, and e) the methodological quality of the study (on a scale of 0–6 points) Footnote 1 .
The coding process was carried out in a standardized and systematic way since a codebook and a protocol for registering the variables Footnote 2 had been produced previously. To assess the reliability of the coding process, 20% of the studies were randomly selected and subjected to a double coding process by two previously trained coders. The results showed very satisfactory inter-coder reliability, with kappa coefficients ranging from 0.85 to 1 for the qualitative variables, and intra-class correlations between 0.99 and 1 for the continuous ones.
Computation of effect sizes
The type of designs used in the studies conditioned the selection of the effect size index in our meta-analysis. Only seven of the 46 articles included a control group. As a consequence, our analysis unit was the group, not the study, and the effect size index was the standardized change scores index, defined as the difference between the pretest and the posttest means divided by the pretest standard deviation:
![]() $$d = c(m)(\overline y _{Post} - \overline y _{\Pr e} )/S_{Pre} $$
, with c(m) being a correction factor for small sample sizes (Hedges & Olkin, Reference Hedges and Olkin1985).
$$d = c(m)(\overline y _{Post} - \overline y _{\Pr e} )/S_{Pre} $$
, with c(m) being a correction factor for small sample sizes (Hedges & Olkin, Reference Hedges and Olkin1985).
The d index was calculated for the 55 treatment groups and for the seven control groups. To calculate effect sizes in the follow-ups, the same formula was used with the follow-up mean instead of the posttest mean. Positive values for d indicated a favorable change in the group from the pretest to the posttest (or the follow-up), and vice versa.
In order to control some of the validity threats of this effect size index, we computed the d index for both treatment and control groups. In this way, the difference between the mean d indices for the treatment and the control groups can offer a more realistic estimate of the true effect.
Separate effect sizes were calculated for obsessive-compulsive symptoms, anxiety, depression, family adaptation, functional impairment, and other outcome measures. In order to measure obsession and compulsion symptoms, the most frequent clinician instruments were the Children´s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS; Scahill et al., Reference Scahill, Riddle, McSwiggin-Hardin, Ort, King, Goodman and Leckman1997) and the Obsessive-Compulsive Subscale of National Institute of Mental Health Diagnostic Interview Schedule for Children (NIMH-OCS; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, Reference Shaffer, Fisher, Lucas, Dulcan and Schwab-Stone2000). Self-reports for measuring obsession and compulsion symptoms were the Leyton Obsessional Inventory – Child Version (LOI-CV; Berg, Rapoport, & Flament, Reference Berg, Rapoport and Flament1986) and the Children’s Obsessional Compulsive Inventory (CHOCI; Shafran et al., Reference Shafran, Frampton, Heyman, Reynolds, Teachman and Rachman2003). General anxiety was measured mainly by means of the Multidimensional Anxiety Scale for Children (MASC; March, Parker, Sullivan, Stallings, & Conners, Reference March, Parker, Sullivan, Stallings and Conners1997) and the Revised Children’s Manifest Anxiety Scale (RCMAS; Reynolds & Richmond, Reference Reynolds and Richmond1978). Depression symptoms were measured with the Children’s Depression Inventory (CDI; Kovacs, Reference Kovacs1992), the Children´s Depression Rating Scale-Revised (CDRS-R; Poznanski, Freeman, & Mokros, Reference Poznanski, Freeman and Mokros1985), and the Hamilton Rating Scale for Depression (HAM-D; Hamilton, Reference Hamilton1960). Functional impairment was measured basically with the Child Obsessive Compulsive Impact Scale-Child/Parent for functional impairment (COIS-C/P; Piacentini & Jaffer, Reference Piacentini and Jaffer1999) and the Clinical Global Impression-Severity/Improvement (CGI-S/I; Guy, Reference Guy1976; National Institute of Mental Health, 1985). Family adaptation was measured with the McMaster Family Assessment Device (FAD; Epstein, Balwin, & Bishop, 1983). Included in the category ‘other outcomes’ were such tests as the Global Assessment of Functioning Scale (GAF; Startup, Jackson, & Bendix, Reference Startup, Jackson and Bendix2002) and the Children’s Global Assessment Scale (C-GAS; Shaffer et al., Reference Shaffer, Gould, Brasic, Ambrosini, Fisher, Bird and Aluwahlia1983).
For the assessment of the reliability of the effect size calculations, the same random sample of studies used in the coding reliability study was subjected to a double process of effect size calculations, obtaining excellent inter-coder reliability, with intra-class correlations of over 0.99.
Statistical Analysis
Separate meta-analyses were carried out with the effect sizes for each outcome measure. In order to accommodate the variability exhibited by the effect sizes, random-effects models were assumed (Borenstein, Hedges, Higgins, & Rothstein, Reference Borenstein, Hedges, Higgins and Rothstein2009). To assess the heterogeneity of the effect sizes, the Q statistic and the I Footnote 2 index were calculated. For each outcome measure, a weighted mean effect size with its confidence interval was calculated separately for the treatment groups and for the control groups (Sánchez-Meca & Marín-Martínez, Reference Sánchez-Meca and Marín-Martínez2008). Given that our meta-analysis did not include any unpublished papers, an analysis of publication bias was carried out. The influence of moderator variables on the effect sizes was carried out by assuming a mixed-effects model. Both random- and mixed-effects models applied in this meta-analysis implied to weight each study as a function of its precision, and the precision is mainly a function of the sample size: the larger the sample size, the larger the precision of the effect size. The statistical analyses were carried out with the SPSS macros developed by David B. Wilson Footnote 3 , with the exception of the forest plot, which was constructed with the program RevMan 5.3.
Results
Distribution of effect sizes
A table with the main moderator variables and effect sizes for each group is presented in the Appendix. For each outcome measure a separate meta-analysis was carried out in order to estimate the mean effect size and its 95% confidence interval. Table 1 presents the results obtained separately for the treatment groups and for the control groups in each outcome measure, and Figure 2 presents a forest plot for the obsessive-compulsive symptoms.
Table 1. Results for the effect sizes as a function of the outcome measure for the treatment and control groups
Note: *p < .05. **p < .01. ***p < .001. 95% C.I.: 95% confidence interval. k: number of studies. Q: heterogeneity statistic. I 2: heterogeneity index (%). d +: mean effect size. d l and d u: lower and upper confidence limits.

Figure 2. Forest plot of the effect size for the obsessive-compulsive symptoms classified a as function of the treatment groups and the control groups. Tau Footnote 2 = estimate of the between-studies variance. Chi Footnote 2 = heterogeneity Q test. df = degrees of freedom of the Q test. Z = statistical test for contrasting the mean effect size.
Focusing on the most important outcome measure in the treatment of pediatric OCD, the obsessive-compulsive symptoms, the results showed a statistically significant mean effect for the 55 treatment groups (d + = 1.860), whereas the mean effect for the seven control groups did not reach statistical significance (d + = 0.232). Furthermore, an ANOVA applied to compare the two mean effects showed statistically significant differences and a large proportion of variance explained of 0.48, Q B(1) = 32.411, p ≤ .0001. Due to its low internal validity, the mean d index obtained for the treatment groups may be overestimating the true effect. A reasonable strategy for controlling the testing effects suffered by these d indices is to define an adjusted mean effect, d adj, as the difference between the mean effect of the treatment groups, d T, and the mean effect of the control groups, d C: d adj = d T - d C. Thus, for the global measures of obsessive-compulsive symptoms an estimate of the true treatment effect was d adj = 1.860 – 0.232 = 1.628, an effect estimate that can still be considered of large magnitude (Cohen, Reference Cohen1988).
Regarding obsessive-compulsive symptoms, Table 1 also presents separately the mean effect obtained for clinician-administered instruments and for self-reports. One noteworthy result is the large mean effect size obtained for clinician-administered instruments (d + = 2.022) in comparison to that of self-reports (d + = 0.816), although in both cases the mean effect was statistically significant, as well as their corresponding adjusted mean effect sizes (clinician-administered: d adj = 2.022 – 0.358 = 1.664; self-reports: d adj = 0.816 – 0.073 = 0.743).
Effect sizes for the 23 treatment groups that measured anxiety symptoms showed a medium, statistically significant mean effect for the treatment groups (d + = 0.603), whereas the four control groups that reported anxiety measures obtained a positive but non statistically significant mean effect (d + = 0.133). When the two mean effects were statistically compared, the difference between them led to a statistically significant difference, Q B(1) = 4.158, p = .041; R 2 = .139. The difference between the two mean effects gave an adjusted effect size of a medium magnitude: d adj = 0.603 – 0.133 = 0.470.
With depression measures the results were slightly less favorable than with the anxiety: the treatment groups obtained a mean effect d + = 0.448, but larger than the one obtained with the control groups (d + = 0.129), a difference that was statistically significant, Q B(1) = 4.445, p = .035; R 2 = .889. The adjusted mean effect was of low-medium magnitude: d adj = 0.448 – 0.129 = 0.319.
For family adaptation outcomes, the treatment groups obtained a mean effect of d + = 0.494, whereas the mean effect for the control groups was practically null (d + = 0.025). The difference between these two mean effects was not statistically significant, Q B(1) = 1.445, p = .229; R 2 = .048. However, the adjusted mean effect size was of medium magnitude: d adj = 0.494 – 0.025 = 0.469.
For other outcome measures, the treatment groups exhibited a mean effect of d + = 1.466, whereas the mean effect of the control groups was d + = 0.083. The statistical comparison between these two mean effects reached statistical significance, Q B(1) = 5.520, p = .019; R 2 = .281, and the adjusted mean effect size was of a large magnitude: d adj = 1.466 – 0.083 = 1.383.
Finally, for functional impairment measures, the mean effect for the 16 groups that reported data about this type of outcomes was statistically significant and of a large magnitude (d + = 0.743). In this case, it was not possible to calculate an adjusted mean effect due to the absence of data for control groups.
Since all the studies included in the meta-analysis were published papers, we calculated the fail-safe N, which involved calculating the number of unpublished studies averaging a null effect that must exist in order for the mean effect obtained in a meta-analysis to become zero (Becker, Reference Becker, Rothstein, Sutton and Borenstein2005). In our meta-analysis this safe number was N fs = 5k + 10 = 5 x 55 + 10 = 285. Taking the adjusted mean effect for obsessive-compulsive measures, d adj = 1.628, the tolerance number for null results was equal to N = 895. As N > N fs, we can discard publication bias as a threat for our meta-analysis.
Analysis of Moderator Variables
As Table 1 shows, effect sizes for the treatment groups exhibited large heterogeneity in obsessive-compulsive symptoms, general anxiety, family adaptation, and other outcome measures. Consequently, an analysis of the characteristics of the studies that could affect the effect size variability was carried out. For this purpose, however, we focused only on obsessive-compulsive measures, as these are the main symptoms that the treatments intend to reduce. Out of the 55 treatment groups, 54 applied some type of CBT with only one group applying a non-cognitive-behavioral treatment (Rezvan et al., Reference Rezvan, Bahrami, Abedi, Macleod, Doost and Ghasemi2013). Thus, the non-CBT study was excluded from the analyses of moderator variables, due to its scarce representativeness. Therefore, the analyses of moderator variables were based on the 54 groups that applied CBT.
(A) Treatment Characteristics
One of the main objectives of this meta-analysis was to examine the differential effects of the different treatment techniques included in CBT. The 54 CBT groups included psychoeducation, 47 groups applied ERP, 44 groups cognitive restructuring, 44 groups relapse prevention, six groups behavioral experiments, eight groups problem solving, and three groups biofeedback techniques.
The various techniques found in the cognitive-behavioral interventions were not mutually exclusive categories. Therefore, the only possible analytical strategy was to apply a multiple meta-regression analysis, taking the d index for obsessive-compulsive measures as the dependent variable, and the predictors were a set of dummy variables (0, absent; 1, present) representing the different techniques found in the studies: ERP, cognitive restructuring, relapse prevention, behavioral experiments, and problem solving. Biofeedback techniques were excluded from the analysis because of their limited use, and psychoeducation was also excluded because all treatment groups included it. The seven control groups were included in the analysis with zero values in all predictors. The full model reached the statistical significance with a large proportion of variance explained of 58.7%, Q R(5) = 45.171, p < .0001. With the exception of problem solving, the remaining techniques obtained positive partial regression coefficients, but only relapse prevention reached statistical significance once the influence of the remaining treatment techniques was controlled (p = .002).
Table 2. Results of the ANOVAs for the influence of qualitative variables related with the treatment implementation on the effect sizes for obsessive-compulsive symptoms
Note: k: number of studies. d +: mean effect size for each category. 95% C.I.: 95% confidence interval for d +. d l and d u : lower and upper confidence limits around d +. Q B : between-categories statistic. Q W : within-categories statistic. R 2 : proportion of variance explained.
Table 2 shows the ANOVAs carried out to analyze the influence of other characteristics related with the treatments. One of the most relevant treatment characteristics in pediatric OCD is the degree of parental involvement in the therapeutic process. In our meta-analysis, the parental involvement level was coded as low (parents only received information from the therapist about the therapeutic progress of the child), moderate (parents attended several treatment sessions), and high (parents were trained as co-therapists to develop the treatment techniques at home). As Table 2 shows, parental involvement had a positive, statistically significant association with the effect size (p = .002), exhibiting a large percentage of variance explained of 34%. Another variable that had a statistically significant result was the treatment protocol used (p = .010) with 31% of variance explained. The most effective manualized protocols were those of Lewin, Storch, Adkins, Murphy, and Geffken (Reference Lewin, Storch, Adkins, Murphy and Geffken2005) and the FOCUS protocol (Barrett et al., Reference Barrett, Healy-Farrell and March2004), with mean effects of 3.198 and 3.188, respectively. Although Lebowitz et al. (Reference Lebowitz2013) obtained a large effect size (d = 3.747), it was based in only one study with a very small sample size (n = 6 participants) and, in fact, this effect was not statistically significant. Other protocols with very good results were those of Simons et al. (2006; d + = 2.728) and Piacentini et al. (2002; d + = 2.530). The training level of the therapist showed a negative, marginally significant relationship with the effects sizes (p = .065), with 11.8% percentage of variance explained. The inclusion of a follow-up program after the treatment seemed to positively affect treatment efficacy, although the difference between the mean effects for studies with (d + = 2.391) and without (d + = 1.772) follow-up programs only reached a marginally statistically significant difference (p = .056). The remaining moderator variables in Table 2 did not have a significant relation with the effect sizes.
Table 3 presents the results of simple meta-regressions applied on continuous moderator variables. As Table 3 shows, the median duration of the treatments was 12 weeks, with an intensity of 1.5 hours a week, and a total magnitude of about 15.5 hours. Simple meta-regression analyses with each of these three moderator variables revealed non-statistically significant relationships with the effect sizes.
Table 3. Results of the simple meta-regressions of the continuous variables on the effect sizes for obsessive-compulsive measures
Note: k = number of studies. Mdn : median. b j = regression coefficient. Q R = statistic for testing the significance of the moderator variable. Q E = statistic for assessing the model misspecification. R 2 = proportion of variance explained. **p < .01. ***p < .001.
(B) Participant characteristics
Two qualitative participant characteristics were analyzed: whether the participants had received previous treatments for OCD (≥ 50% of the sample versus < 50% in the sample) and the presence of comorbidity in the participants (≥ 50% of the sample with comorbidity versus < 50% in the sample). As Table 4 shows, the results of the ANOVAs applied on these moderator variables were not statistically significant. Table 3 presents three other (continuous) variables related to the participants: the mean age (median = 13 years), the percentage of males (median = 53.8%), and the years suffering from OCD (median = 3.1 years). None of these characteristics presented a significant relationship with the effect sizes.
Table 4. Results of the ANOVAs for the influence of qualitative variables related with the samples of participants on the effect sizes for obsessive-compulsive symptoms
Note: k = number of studies. d + = mean effect size for each category. 95% C.I. = 95% confidence interval for d +. d l and d u = lower and upper confidence limits around d +. Q B = between-categories statistic. Q W = within-categories statistic. R 2 = proportion of variance explained.
(C) Methodological characteristics
The analysis of the influence of methodological variables on the effect sizes has a central role in meta-analysis, since it allows us to discover any deficiencies in the method that might lead to biased estimates of the true treatment effect. Surprisingly, in this case, none of the methodological characteristics analyzed reached a significant result (random allocation, sample size, use of intent-to-treat analysis, use of blinded assessors, control of medication consumption, etc). However, it is worth highlighting some results. As may be expected, when the researchers used intent-to-treat analyses the mean effect (d + = 1.807) was slightly lower than when a completers analysis was carried out (d + = 2.361). On the other hand, an unexpected result was to find a larger mean effect when using blinded assessors (d + = 2.146) than when they were not used (d + = 1.749). However, this result is explained by the confounding between the variables ‘blinded assessors’ and ‘type of measure’ (self-reports vs. clinician assessments). Most of the studies included in the category ‘no blinded assessors’ used self-report measures and, as mentioned above, self-reports systematically showed lower effect sizes than clinician measures.
Two continuous methodological variables were also analyzed: attrition in the posttest and methodological quality, neither of which reaching a statistically significant relationship with the effect sizes (see Table 3).
A Predictive Model
The analyses of the moderator variables revealed that some characteristics of the studies were influencing the magnitude of the treatment effects on obsessive-compulsive symptoms. However, the specification tests (Q W for ANOVAs and Q E for meta-regressions) revealed that none of the models was correctly specified. In order to propose a subset of studies characteristics that could explain a large quantity of the variance, a multiple meta-regression analysis was applied on the effect sizes for obsessive-compulsive symptoms as the dependent variable. The predictors in the model were selected both on a conceptual and a statistical basis. Thus, the different treatment techniques applied in the groups were included in the model, as one of our main objectives was to assess the differential efficacy of the techniques used in CBT. In addition, the parental involvement in the treatment was also included, as it exhibited a statistically significant relationship with the effect size and is a very relevant conceptual characteristic of the treatments. Therefore, the meta-regression model included two clusters of predictor variables: a) a cluster of parental involvement coded as two dummy variables (0, absent; 1, present) for the categories ‘high involvement’ and ‘moderate involvement’; and b) a cluster of treatment techniques with five dichotomous predictors (0, absent; 1, present) for the techniques ERP, cognitive restructuring, relapse prevention, behavioral experiments, and problem solving. The 54 treatment effect sizes and the seven control ones were included in the multiple meta-regression model, with the control groups being coded as zero in all of the predictor variables.
Table 5 presents the results of the multiple meta-regression. The cluster of parental involvement reached a statistically significant result (p ≤ .001), with 56.7% of variance explained. The cluster of treatment techniques also showed a statistically significant result (p < .001), with a percentage of variance explained of 58.7%. When both clusters were introduced in the meta-regression model, the full model reached statistical significance (p < .001) and its percentage of variance explained reached 68.9%. Out of the seven predictors included in the model, only four exhibited a statistically significant relationship with the effect sizes: the categories ‘high parental involvement’ (p = .0006) and ‘moderate parental involvement’ (p = .031), and the techniques ‘relapse prevention’ (p = .006) ‘solving problems’ (p = .020). With the exception of ‘solving problems’, the remaining significant predictors exhibited positive partial regression coefficients, indicating the benefits of including them in the treatments.
Table 5. Results of the multiple meta-regression applied on the effect sizes for obsessive-compulsive symptoms
Note: * p < .05. ** p < .01. *** p < .001. b j partial regression coefficient. Z = statistic for testing the significance of b j. Q R = statistic for assessing the significance of the meta-regression model. Q E = statistic for assessing the model misspecification. R 2 = proportion of variance explained. df = degrees of freedom. ΔQ R and ΔR 2 = increase in the Q R statistic and in R 2, respectively, as a consequence of including in the model the cluster once the other cluster had already been introduced.
Table 5 also shows the increases in statistical significance and in the proportion of variance accounted for by each cluster of predictors when it was included once the other one had already been introduced in the meta-regression model. The increase in R Footnote 2 when the parental involvement cluster was included in the model was 10.2%, and statistically significant (p < .001). Adding the cluster of treatment techniques provided an increase in R 2 of 12.2%, which was also statistically significant (p < .001).
Meta-analysis in the Follow-Up
Thirty of the 54 CBT groups analyzed reported data in the follow-up, but anyone study reported data for the control groups. In order to examine if the benefits of the therapy maintained over time, the standardized mean difference was computed between the pretest and the longest follow-up reported in the study. With regard to the distribution of the effect sizes, the results showed a greater improvement than in the posttest in the majority of the outcome measures. For global obsessive-compulsive measures, the mean effect was of very large magnitude and statistically significant (d + = 2.189; 95% C.I.: 1.808, 2.570; k = 30). Results of a large magnitude were also found for anxiety measures (d + = 0.938; 95% C.I.: 0.597, 1.278; k = 13), depression (d + = 0.662; 95% C.I.: 0.461, 0.862; k = 11), functional impairment (d + = 1.153; 95% C.I.: 0.764, 1.541; k = 9), and other measures (d + = 1.845; 95% C.I.: 1.209, 2.481; k = 12). The only exception was family adaptation, whose mean effect was very low and non statistically significant (d + = 0.150; 95% C.I.: -0.396, 0.696; k = 5).
Discussion
The purpose of this research was to investigate the differential efficacy of psychological treatments for pediatric OCD. With this aim, a meta-analysis was conducted with a total of 62 groups reported in 46 studies. Fifty-four groups tested the efficacy of CBT and seven were control groups. The effect size index was the standardized mean of the pretest-posttest (follow-up) change scores. The problems with the internal validity of the d index obtained from one-group designs, led us to propose an adjusted mean effect, d adj, computing the difference between the mean d indices of the treatment, d T, and the control, d C, groups (d adj = d T - d C). The adjusted index allowed us to control the testing effects and, as a consequence, it offered a more appropriate estimate of the true treatment effect. With regard to obsessive-compulsive symptoms, the adjusted mean effect was d adj = 1.628, very similar to that obtained by Abramowitz et al. (Reference Abramowitz, Whiteside and Deacon2005) if we calculate the difference between the treatment and the control mean ds reported by them: d adj = d T - d C = 1.98–0.48=1.50. A similar estimate was obtained by Watson and Rees (Reference Watson and Rees2008) with the five CBT-control comparisons included in their meta-analysis: d adj = 1.45. The effect estimates for CBT obtained by O’Kearney (Reference O'Kearney2007) and Freeman et al. (Reference Freeman, Choate-Summers, Moore, Garcia, Sapyta, Leonard and Franklin2007) were slightly lower than ours. O’Kearney (Reference O'Kearney2007) reported a mean effect d adj = 1, and Freeman et al. (Reference Freeman, Choate-Summers, Moore, Garcia, Sapyta, Leonard and Franklin2007) obtained an unadjusted mean effect d = 1.55. Freeman et al. (Reference Freeman, Choate-Summers, Moore, Garcia, Sapyta, Leonard and Franklin2007) did not offer a mean d for the control groups, but if we take the mean d obtained with our control groups (or those from Abramowitz et al., Reference Abramowitz, Whiteside and Deacon2005), then their adjusted estimation is similar to that offered by O’Kearney (Reference O'Kearney2007): d adj = d T - d C = 1.55–0.48 = 1.07. An analysis of publication bias enabled us to discard this as a threat to the validity of our results.
A result not found in previous meta-analyses on pediatric OCD was the larger effect size obtained with clinician assessments in comparison with those from self-reports. Another result not addressed previously concerns the effect estimates of the treatments on other related outcome measures. Our results showed statistically significant differences between the mean effects of CBT and control groups for anxiety and depression measures, with low-to-medium adjusted mean effect sizes (d adj = 0.470 and 0.319, respectively).The lower effect of CBT on general anxiety and depression symptoms in comparison with that of obsessive-compulsive ones can be due to the fact that the treatments did not directly target these symptoms. Concerning family adaptation, the adjusted mean effect was of a medium magnitude (d adj = 0.469), but not statistically significant. A statistically significant adjusted mean effect and of a large magnitude was obtained for other outcome measures (d adj = 1.383). Regarding functional impairment, the studies did not report data from control groups; so, it was not possible to obtain an adjusted effect size of the benefits achieved by CBT on these measures. Therefore, although the standardized pretest-posttest change scores index exhibited statistically significant improvements for the treatment groups in functional impairment, these results do not enable us to offer an accurate estimate of the benefits of CBT on these symptoms. The follow-up data showed large, statistically significant mean effects for obsessive-compulsive, anxiety, depression, functional impairment, and other measures. However, the absence of data from control groups did not allow us to obtain adjusted effect sizes. Therefore, follow-up results must be interpreted with caution.
The large heterogeneity exhibited by the effect sizes for obsessive-compulsive outcomes led us to examine the influence of the study characteristics. With regard to treatment characteristics, parental involvement in the therapy and the inclusion of relapse prevention techniques seem to be the most relevant components to improve the benefits of CBT in reducing obsessive-compulsive symptoms. These characteristics were included in the two treatment protocols that reached the largest effect sizes, the one applied by Barrett et al. (Reference Barrett, Healy-Farrell and March2004), with d = 3.188, and the intensive CBT applied by Lewin et al. (Reference Lewin, Storch, Adkins, Murphy and Geffken2005), with d = 3.198. Following the same line, our predictive model showed statistically significant increases in the variance accounted for when both the cluster of parental involvement (10.2%) and the cluster of treatment techniques (12.2%) were added to the model. Although previous research has found ERP as the main component of CBT to benefit patients with pediatric OCD, the results of our multiple meta-regression did not find a statistically significant result for ERP, being relapse prevention the only treatment component than exhibited a positive, statistically significant result. One reason for not finding a statistical association between ERP and effect size is that the majority of the CBT groups (47 out of the 54 CBT groups) included ERP as a treatment component, making it difficult to achieve statistical significance. Another tentative explanation of this counterintuitive result is that the studies that reported using relapse prevention were also the better-conducted ones, hence explaining the significant finding in the meta-regression.
Previous meta-analyses on the efficacy of CBT for pediatric OCD did not present data about the differential efficacy due to treatment techniques. Only Freeman et al. (Reference Freeman, Choate-Summers, Moore, Garcia, Sapyta, Leonard and Franklin2007) found greater effect sizes for family-based CBT (d = 1.88) and individual CBT (d = 1.77) in comparison with group CBT (d = 0.76). The mean effects obtained by Freeman et al. (Reference Freeman, Choate-Summers, Moore, Garcia, Sapyta, Leonard and Franklin2007) were based on the standardized pretest-posttest difference for the CBT groups. Our results with the same effect size index were clearly larger than those obtained by Freeman et al. (Reference Freeman, Choate-Summers, Moore, Garcia, Sapyta, Leonard and Franklin2007): d = 2.035 for family-based CBT, d = 2.017 for individual CBT, and d = 1.781 for group CBT (see Table 3). If we adjust our mean effect for these three CBT categories by subtracting the mean effect for the control groups (d = 0.232), we can obtain a more realistic benefit of CBT for family-based (d adj = 1.803), individual (d adj = 1.785), and group CBT (d adj = 1.549).
The training level of the therapists showed a negative, marginally statistically significant relationship with the effect sizes (p = .065), with 11.8% of variance accounted for. This was an unexpected result, as previous research has found a null relationship between therapist’s experience and treatment efficacy. Thus, van Oppen et al. (Reference van Oppen, van Balkom, Smit, Schuurmans, van Dyck and Emmelkamp2010) found that clinically inexperienced master’s students with no post-graduate training can be as capable as experienced behavior therapists in treating OCD patients, as long as therapists adhere to a manualized treatment and adequate training and supervision is provided. In addition, Webb, DeRubeis, and Barber (Reference Webb, DeRubeis and Barber2010) conducted a meta-analysis about the relationship between therapist competence and outcome treatment and they found a practically null correlation between them (r = .07). A tentative explanation for the negative relationship found in our meta-analysis between therapist’s training and effect size might be that young clinicians often work harder than senior clinicians and pay more attention to details. Another explanation is the existence of a correlation between the training level of therapists and the treatment techniques applied in the studies, but this possible relationship was not explored due to the large number of techniques included in the studies. And another explanation of this unexpected result is the ambiguity in the studies to describe the therapist’s experience.
With regards to the participants’ characteristics, it was not possible to analyze some of these (e.g., family history of the disorder and type of obsessions/compulsions) due to the lack of information on these characteristics reported in the studies. None of the variables analyzed in our meta-analysis about the characteristics of the participants reached a statistical relationship with the effect sizes (age, gender, OCD history, previous treatments, comorbidity). These results must be interpreted cautiously, due to the low sensitivity of meta-analytic techniques in examining the influence of these characteristics. Previous meta-analyses did not explore the moderating effect of participant variables.
In our meta-analysis the effect size was not affected by methodological variables such as attrition of treatment groups in the posttest or the methodological quality of the studies. On the contrary, O’Kearney (Reference O'Kearney2007) found that the studies with low risk of bias (according to methodological quality) tended to obtain lower effect sizes than the studies with high risk. In this respect, differences in how the study quality was assessed may explain the discrepant results between the meta-analyses.
One of the clearest implications for clinical practice is the convenience of using CBT for treating children and adolescents with OCD, since the improvements are very notable in reducing obsessive-compulsive symptoms and, in a lesser extent, anxiety, depression, family adaptation, functional impairment, and other symptoms.
Concerning the treatment techniques, our findings suggest that the most promising treatments are those based on multicomponent programs comprising ERP, cognitive strategies, and relapse prevention. With the use of ERP children are exposed to feared objects, preventing them from performing avoiding responses (compulsions). Through this method, consecution of negative reinforcement is avoided, and the anxiety levels are reduced through the habituation process. Cognitive training intends to change beliefs and cognitive bias that maintain the obsessive-compulsive disorder, such as exaggerated sense of responsibility (Salkovskis et al., Reference Salkovskis, Wroe, Gledhill, Morrison, Forrester, Richards and Thorpe2000), thought-action fusion (Rachman, Reference Rachman1993) or externalizing OCD (March & Mulle, 1998). The latter refers to the ability of children to think about the disorder as an enemy separated from themselves. In relapse prevention sessions the therapist provides the child and family with coping techniques for future problems. In this sense, the factor that plays the most important role in the treatment is parental involvement. Parents can actively participate, on the one hand, in the assessment and reporting of more objective data and information and, on the other hand, in the implementation of the treatment, reducing accommodation to symptoms, applying exposure at home, and modifying beliefs and attitudes toward OCD (AACAP Committee on Quality Issues, 2012; Barrett et al., Reference Barrett, Farrell, Pina, Peris and Piacentini2008). Currently, there are several standardized protocols that present the mentioned characteristics. Three of them present the highest effect sizes in our meta-analysis: Lewin et al.’s (Reference Lewin, Storch, Adkins, Murphy and Geffken2005) intensive CBT, Barrett’s (Reference Barrett, Healy-Farrell and March2004) FOCUS protocol, and Lebowitz et al.’s (Reference Lebowitz2013) intervention. In spite of the empirical support for these protocols, their application in clinical practice is not very common, with only one third of clinicians applying them routinely (AACAP Committee on Quality Issues, 2012). Our findings strongly recommend the routine application of these protocols by professionals.
Finally, the assessment of OCD requires an exhaustive collection of information by the therapist. Therefore, the use of validated measures and systematic observation constitute key elements for achieving this goal. At present, the most representative instrument for the assessment of pediatric OCD is the CY-BOCS.
Despite the great advances achieved in this field, there are still few experimental studies with control groups. The absence of control groups in the studies force meta-analysts to use an effect size index with low internal validity, conditioning the scope of the results of the primary studies and of the meta-analyses. In this sense, including two (or more) group designs with random allocation of the participants to the groups, as well as psychological placebo control conditions in the primary studies will allow the estimation of the nonspecific effects of the interventions for pediatric OCD. In addition, follow-up measurements should be carried out in the control groups in order to obtain a valid estimate of the long-term effects of the treatments.
Our recommendation on which treatment components are the most relevant to reduce obsessive-compulsive symptoms in pediatric OCD must be taken very cautiously, as meta-analysis is not an experimental research, but an observational one. The results of our multiple meta-regression model to examine the relative contributions of different treatment components are not based on an experimental design that dismantles CBT components. Multiple regression models applied in the context of a meta-analysis allow us to find a subset of study characteristics that can be statistically associated to the effect sizes taking into account the multicollinearity among them. However, regression models in meta-analysis cannot be employed to establish cause-effect relationships, but only statistical associations between the predictors and the effect sizes (López-López, Marín-Martínez, Sánchez-Meca, Van den Noortgate, & Viechtbauer, Reference López-López, Marín-Martínez, Sánchez-Meca, Van den Noortgate and Viechtbauer2014; Raudenbush, Reference Raudenbush, Cooper, Hedges and Valentine2009). Following the same line, the results obtained in our multiple meta-regression model are only tentative, requiring caution throughout their interpretation, and should be used to guide future research on this topic. Thus, future experimental research should assess the differential effectiveness of the protocols and treatment techniques with the goal of improving the cost-effectiveness trade-off. This goal can be addressed by dismantling the treatments or by conducting face-to-face studies (e.g., ERP alone vs. ERP + cognitive training). In this sense, it would have been interesting to analyze differences depending on the kind of cognitive techniques used in the studies, but the scarce information reported by the majority of the empirical studies did not allow us to do so. Furthermore, family-based treatments must be studied in greater depth, as they seem to be very promising. In addition, the differential efficacy of the standardized protocols such as FOCUS, POTS, or Lewin et al.’s intensive CBT, should be examined by designing controlled studies that directly compare their efficacy. On the other hand, as Barrett et al. (Reference Barrett, Farrell, Pina, Peris and Piacentini2008) suggested, treatments must present enough flexibility to address the differing needs of individual families coming for treatment. It is also necessary to conduct studies analyzing differential efficacy according to variables indicated by some studies such as anxiety of parents, age or gender of participants (Böguels & Phares, Reference Bögels and Phares2008; Creswell & Cartwright-Hatton, Reference Creswell and Cartwright-Hatton2007; McLeod et al., Reference McLeod, Wood and Weisz2007). It is also relevant to develop strategies for treating non-responders, taking into account such factors as comorbidity or family functioning (Krebs & Heyman, Reference Krebs and Heyman2010).
Finally, the information provided by primary studies should be more exhaustive and should report variables such as comorbidity, family history of the disorder, or type of obsessions/compulsions, among others. Moreover, the studies did not report all of the information needed to code all moderator variables included in our meta-analysis. A more comprehensive reporting of the relevant variables in the primary studies would not only facilitate the conducting of meta-analyses, but also the replication of empirical studies. Missing information about moderator variables in the studies limits the scope and generalizability of our meta-analytic findings. Although the results of our moderator analyses must be interpreted cautiously, they can help to guide the design and reporting of future research on this topic.
Appendix. Some of the moderator variables of the studies included in the meta-analysis.










