Research is consistently showing a significant generational shift, as young adults are now taking longer than in past decades to reach educational, financial and social developmental milestones (Arnett, Reference Arnett2000). Youngsters now take longer to finish their education, access to the job market and commit to stable relationships and have children (e.g., Arnett, Reference Arnett2000, Reference Arnett2014; Furstenberg, Reference Furstenberg2015; Settersten & Ray, Reference Settersten and Ray2010). This developmental pathway has led to acknowledge that emerging adulthood is currently an important transitional and developmental period (Arnett et al., Reference Arnett, Žukauskienė and Sugimura2014), where completing education and building stable life structures often comprises significant developmental challenges. Emerging adulthood (Arnett, Reference Arnett2000) is thus an important developmental period characterized by different life changes and demands, that puts youngsters at risk to develop multiple emotional and behavioral disturbances (Arnett et al., Reference Arnett, Žukauskienė and Sugimura2014). Not surprisingly, current research also points to a parallel alarming increase in the rate of behavioral difficulties and mental health issues among young adults in the last decade. Twelve-month prevalence estimates of mood and anxiety disorders before the COVID–19 pandemic ranged between 8.3 and 12.4% and between 19.4 and 22.3%, respectively, among emerging adults between 18 and 33 years (Moffitt et al., Reference Moffitt, Caspi, Taylor, Kokaua, Milne, Polanczyk and Poulton2010; Ormel et al., Reference Ormel, Raven, van Oort, Hartman, Reijneveld, Veenstra, Vollebergh, Buitelaar, Verhulst and Oldehinkel2015). Gustavson et al. (Reference Gustavson, Knudsen, Nesvåg, Knudsen, Vollset and Reichborn- Kjennerud2018) indicated a 12-month prevalence of mental disorders among this developmental period of 27.8%, among which mood and anxiety disorders are the most common problems, with prevalence estimates of 7.3% and 20.4%, respectively. Elevated depression and anxiety levels are thus highly common currently among young adults and the occurrence of affective dysfunctions during emerging adulthood confers increased risk for continuing suffering them during mid adulthood (i.e., Gustavson et al., Reference Gustavson, Knudsen, Nesvåg, Knudsen, Vollset and Reichborn- Kjennerud2018).
There is thus a critical need to prioritize research that facilitates a better understanding of risk and protective factors against depression and anxiety disturbances during emerging adulthood and to translate this information to enhance well-being and to promote developmental success in young populations. Previous research has been mostly focused on the study of risk factors contributing to affective disorders’ onset in young adults. For instance, individual cognitive styles, especially those characterized by a need of control, relatedness, and approval, have been found to predict the development of depression in young adults (e.g., Mazure & Maciejewski, Reference Mazure and Maciejewski2003).
Previous research has also found that high anxiety sensitivity, poor emotion regulation, and looming parental styles predict the development of anxiety disorders during emerging adulthood (Kashdan et al., Reference Kashdan, Zvolensky and McLeish2008; Riskind et al., Reference Riskind, Sica, Bottesi, Ghisi and Kashdan2017). However, current views claim that this focus is incomplete, and that a comprehensive approach in developmental psychopathology research needs to include a further focus on predictors of positive adaptation in response to developmental challenges (e.g., Miret et al., Reference Miret, Cabello, Marchena, Mellor-Marsá, Caballero, Obradors-Tarragó, Haro and Ayuso-Mateos2015; Schönfeld et al., Reference Schönfeld, Brailovskaia and Margraf2017). Within this view, it is essential to study protective factors that contribute to resilience in young adults, namely the ability to flexibly adapt to situational demands (Bonanno & Burton, Reference Bonanno and Burton2013), to resist to psychopathology (Ingram & Price, Reference Ingram, Price, Ingram and Price2001) and to enable positive adaptation despite the experience of adversity or trauma (Luthar, Reference Luthar, Cicchetti and Cohen2006).
There are still important gaps in the study of resilience in emerging adulthood, as resilience developmental research has been mostly conducted with children and adolescent populations (e.g., Masten, Reference Masten2001). Nonetheless, initial research on resilience factors during developmental transitions (Grotberg, Reference Grotberg2003; Lee et al., Reference Lee, Nam, Kim, Kim, Lee and Lee2013; Murray, Reference Murray2003), have commonly identified two main types of factors that may be relevant in the promotion of resilient functioning in young adults: One referred to personal psychological characteristics, namely individual capacities to cope with stressful and/or challenging demands, to generate positive self-appraisals and to establish good interpersonal relationships (Carbonell et al., Reference Carbonell, Reinherz, Giaconia, Stashwick, Paradis and Beardslee2002; Gooding et al., Reference Gooding, Hurst, Johnson and Tarrier2012), and another one referred to dimensions of perceived social support and perceived quality of established relationships (Luthar, Reference Luthar, Cicchetti and Cohen2006).
In terms of personal factors, resilient adaptation has been related to resilience factors such as inner strength, competence, and optimism (Wagnild, Reference Wagnild2009), personal coping capacities, perceived control and goal-oriented behavior, positive appraisals of stress and others’ trust (Connor & Davidson, Reference Connor and Davidson2003), among others. Extensive research in the context of adolescence highlights how several of these factors are predictive of resistance to the development of depression and anxiety (e.g., Dumont & Provost, Reference Dumont and Provost1999; Gariépy et al., Reference Gariépy, Honkaniemi and Quesnel-Vallée2016; Herman-Stahl & Petersen, Reference Herman-Stahl and Petersen1996; Seligman, Reference Seligman, Routh and DeRubeis1998). However, in the context of young adults, existing research has mostly focused on determining how overall levels of resilience relate to individual differences in emotional symptoms (e.g., Campbell-Sills et al., Reference Campbell-Sills, Cohan and Stein2006), rather than examining associations between specific personal resilience factors and specific forms of emotional symptomatology (i.e., depression, anxiety). Thus, in the present study we aimed to conduct an initial examination on how different personal factors of resilience (i.e., coping and persistence during stress, tolerance to negative affect, positive appraisals, trust) might uniquely be associated to different dimensions of emotional psychopathology that are relevant during emerging adulthood (i.e., depression and anxiety), above and beyond other central protective factors during this developmental period such as dimensions of perceived social support.
Perceived social support has been identified as a second central protective factor in developmental transitions (Luthar, Reference Luthar, Cicchetti and Cohen2006). It is referred to how individuals perceive friends, family members and significant others as available sources to provide support during demanding times. Extant empirical evidence suggests that for social support to facilitate resilient development during emerging adulthood, youngsters must perceive their social relations as supportive ones, in other words, having the sense that one can reach to their social support system (e.g., Goyette, Reference Goyette, Mann-Feder and Goyette2019). Perceived social support has been consistently related to higher well-being and better psychological health (Cohen et al., Reference Cohen, Underwood and Gottlieb2000). There is consistent accumulating evidence on its protective effects to promote resilient functioning in different populations and development stages. This body of evidence has been collected especially in children and adolescents (see, for instance, the meta-analysis of Rueger et al., Reference Rueger, Malecki, Pyun, Aycock and Coyle2016), although recent research also points to a similar protective role in young adults (e.g., Ioannou et al., Reference Ioannou, Kassianos and Symeou2019). Further, some research shows evidence that personal resilience and social support are highly correlated and that they both are associated to higher mental health rates in young adults (Dumont & Provost, Reference Dumont and Provost1999; Peng et al., Reference Peng, Zhang, Li, Li, Zhang, Zuo, Miao and Xu2012). Importantly, recent studies go beyond the study of associations between these social and personal protective factors and point to a mediating role of personal resilience factors (i.e., coping and persistence during stress, tolerance to negative affect, positive appraisals, trust) on the protective effects of perceived social support on mental health. For instance, Brailovskaia et al. (Reference Brailovskaia, Schönfeld, Zhang, Bieda, Kochetkov and Margraf2018) recently showed that overall resilience levels mediated the association between higher perceived social support and lower rates of stress, depression and anxiety. Research with young adults has also started to provide some indirect support for this type of mediational effects. Specifically, there is initial evidence showing that perceived social support may improve psychological health in young adults through the mediating effect of individual factors of self-worth, sense of security and belonging, related to personal resilience factors (Cano et al., Reference Cano, González Castro, De La Rosa, Amaro, Vega, Sánchez, Rojas, Ramírez-Ortiz, Taskin, Prado, Schwartz, Córdova, Salas-Wright and de Dios2020; Ioannou et al., Reference Ioannou, Kassianos and Symeou2019; Lee et al., Reference Lee, Dickson, Conley and Holmbeck2014).
Thus, whether perceived social support is related to better resilient outcomes, in terms of better psychological health (i.e., lower depression and anxiety levels), through their association with higher levels of different personal resilience factors during emerging adulthood is a plausible pathway with multiple potential implications for prevention programs. The present proof-of-concept study aimed to study the associations between different social support dimensions and personal resilience factors and to test their hypothetical pathways of relation to existing levels of depression and anxiety rates in young adults, comprising a mediating role of personal resilience factors in accounting for the association between social support dimensions and mental health (i.e., perceived social support → resilience factors → mental health outcomes).
Perceived social support is not a unitary construct but includes multiple dimensions (perceived support from the family, friends, and a significant other, Zimet et al., Reference Zimet, Dahlem, Zimet and Farley1988), that must be considered for the present research purposes. Some initial studies indicate that the strength of associations between different social support dimensions and resilience factors depend on the developmental stage. For instance, some studies with adolescents (between 14 to 18 years) have shown that perceived support from family members and from friends both influences the promotion of resilience (Stumblingbear-Riddle & Romans, Reference Stumblingbear-Riddle and Romans2012; Wills & Bantum, Reference Wills and Bantum2012). In contrast, in later development stages (i.e., young adults), results from extant research are not that consistent regarding the contribution of all these social support dimensions. Some studies have only considered perceived social support in general when studying its paths of relation with resilience factors to account for better mental health outcomes (Malkoç & Yalçin, Reference Malkoç and Yalçin2015). Other studies considering separate social support dimensions have pointed to a higher relevance of perceived social support from friends or family as the main protective social support factors buffering against stress in young adults (Lee & Dik, Reference Lee and Dik2017; Lee & Goldstein, Reference Lee and Goldstein2016; Tam & Lim, Reference Tam and Lim2009; Wilks & Spivey, Reference Wilks and Spivey2010).
The main aim of the present study was thus going beyond previous existing research that have considered either single general measures of perceived social support and/or resilience in the study of paths of promotion of mental health in young adults.
We examined the relationships between different social support dimensions and personal resilience factors, and their hypothetical pathways of influence to account for individual differences in mental health (depression and anxiety levels) in young adults. Thus, although previous research has typically assessed resilience in a global manner, in our study we considered different personal resilience factors (i.e., coping and persistence abilities in stressful situations, tolerance of negative affect and capacity for goal-oriented focus, positive appraisal of stress situations, and others’ trust) in relation to different social support dimensions (i.e., family, friends and significant other). Using this approach, this study is a first step to try to understand how different social support dimensions may distinctly relate to different forms of personal resilience factors during a challenging and demanding developmental period such as emerging adulthood.
Secondly, the study aimed to determine unique associations of each of these social and personal resilience factors with better mental health outcomes during emerging adulthood. Previous studies have supported negative associations of global measures of both social support and resilience with depression and anxiety levels in young adults (e.g., Catabay et al., Reference Catabay, Stockman, Campbell and Tsuyuki2019; Haroz et al., Reference Haroz, Murray, Bolton, Betancourt and Bass2013; Sim et al., Reference Sim, Bowes and Gardner2019), presumably due to social withdrawal and the presence of negative cognitive schemas (Ibarra-Rovillard & Kuiper, Reference Ibarra-Rovillard and Kuiper2011). The present study aimed to provide an integrative initial test of the separate associations of each of these social support and personal resilience variables with lower depression and anxiety levels in a sample of Spanish young adults. In line with the most recent evidence pointing to a mediational role of resilience factors in accounting for the influence of social support dimensions on mental health outcomes (Brailovskaia et al., Reference Brailovskaia, Schönfeld, Zhang, Bieda, Kochetkov and Margraf2018, Cano et al., Reference Cano, González Castro, De La Rosa, Amaro, Vega, Sánchez, Rojas, Ramírez-Ortiz, Taskin, Prado, Schwartz, Córdova, Salas-Wright and de Dios2020), we aimed to test these hypothetical mediational models in our sample of young adults. Thus, when analyses supported (a) an association between a given social support dimension and a given personal resilience factor, and (b) an association between that personal resilience factor and one of the mental health outcomes, indirect effect models were conducted to test the main hypothesis that social support dimensions are indirectly related to lower levels of depression and/or anxiety through their relation with personal resilience factors (i.e., social support → resilience factor → depression and anxiety).
Significant negative correlations were expected between depression and anxiety levels and all resilience factors and social support dimensions. Social support dimensions were further expected to predict individual differences in resilience factors. Specifically, in line with previous research in young adults (Stumblingbear-Riddle & Romans, Reference Stumblingbear-Riddle and Romans2012; Wills & Bantum, Reference Wills and Bantum2012), higher levels of perceived social support from friends were expected to have the highest predictive power in accounting for higher levels of resilience factors. Social support dimensions and personal resilience factors reflecting effective coping (Malkoç & Yalçin, Reference Malkoç and Yalçin2015) and a positive appraisal style (Kalisch et al., Reference Kalisch, Müller and Tüscher2015; see also Veer et al., Reference Veer, Riepenhausen, Zerban, Wackerhagen, Puhlmann, Engen, Köber, Bögemann, Weermeijer, Uściłko, Mor, Marciniak, Askelund, Al-Kamel, Ayash, Barsuola, Bartkute- Norkuniene, Battaglia, Bobko and Kalisch2021) were hypothesized to demonstrate the highest predictive power to account for lower levels of depression and anxiety.
Ultimately, mediational models were tested, according to which the effects of social support dimensions in mental health outcomes were expected to be mediated by their association with protective personal factors of resilience.
Method
Participants
Spanish young adults with ages ranging from 18 to 29 years old were screened and recruited from the general population using internet postings and public advertisement. The final sample was composed by 500 participants (72.2% female, 26.8 male and 1% other (i.e., non-binary). The study was conducted between March and April 2021 and the data collection period comprised four weeks. The participation in this study was entirely voluntary, and no financial compensation was given to the participants.
Participants comprised a representative sample of the population under study (57.8% students, 3.2% unemployed, 2.4% neither studying nor working, 15.2% active workers, 21.4% both studying and working). The mean age was 21.57 years (SD = 2.7) and ranged from 18 to 29 years. The marital status of the respondents was of 59.4% single not in a relationship, 39.6% single in a relationship, 0.8% married, and 0.2% divorced. Other relevant sociodemographic data collected included educational level (0.4 % primary education, 5.6% secondary education, 9 % high school education, 7% vocational training, 14.8% higher degree vocational training, 51.8% college bachelor’s degree, 11 % master’s degree, 0.4% PhD), and number of cohabitants with whom the participants lived with (86% living with one or more relatives, 13.21% living with non-relatives -friends, house mates, etc.-, and 0.8% living alone).
Measures
Resilience Factors
The Connor-Davidson Resilience Scale (CD-RISC) (Connor & Davidson, Reference Connor and Davidson2003) was used to measure personal resilience factors. This scale includes a series of 25 items, each rated on a 5-point scale (0 = not at all true to 4 = nearly all the time), reflecting several individual factors of resilience, including a sense of personal competence, tolerance of negative affect, positive acceptance of change, trust in one’s instincts, sense of social support, spiritual faith, and an action-oriented approach to problem solving.
The scale is typically scored as an overall single index, with higher scores reflecting greater general resilience levels. For this study we used the Spanish adaptation of the CD-RISC (Crespo et al., Reference Crespo, Fernández-Lansac and Soberón2014; 21 items) which has demonstrated good reliability and validity and its feasibility to be used with both adult psychiatric and general populations. The factorial validation of the Spanish adaptation of the instruments (Crespo et al., Reference Crespo, Fernández-Lansac and Soberón2014) identified four separate resilience factors that can be derived from the overall index: 1- Abilities of coping and persistence in stress situations (8 items); 2- tolerance of negative affect and capacity for goal-oriented focus (5 items); 3- positive appraisal of stress (6 items); and 4- others’ trust (2 items). Based on this, the present study also analyzed these separate resilience subfactors identified in the previous Spanish validation, as they were theoretically relevant for our hypotheses. In our study, internal consistencies for each resilience factor were comparable with the ones reported by Crespo et al. (Reference Crespo, Fernández-Lansac and Soberón2014): Coping and persistence in stress situations, Cronbach’s alpha = .77; tolerance of negative affect and capacity for goal-oriented focus (α = .65), positive appraisal (α = .56), and trust (α = .28) respectively.
Perceived Social Support Dimensions
The Multidimensional Scale of Perceived Social Support (MSPSS) (Zimet et al., Reference Zimet, Dahlem, Zimet and Farley1988) was used to measure social support dimensions. This is a 12-item measure of perceived adequacy of social support from three different sources: Family, friends, and a significant other (4 items each); rated using a 7-point Likert scale (0 = very strongly disagree, 7 = very strongly agree’). For this study, the Spanish adaptation of Ruiz Jiménez et al., (Reference Ruiz Jiménez, Saiz Galdós, Montero Arredondo and Navarro Bayón2017) was used. The MSPSS measure has demonstrated good reliability and validity (Zimet et al., Reference Zimet, Powell, Farley, Werkman and Berkoff1990). It can be scored as a total sum sore, reflecting general perceived support, or as separate social support dimensions, adding the scores of each subscale and dividing them by four. In this study, we used the three separate dimensions of perceived social support, in order to test our hypotheses. All the subscales demonstrated good internal consistencies in this study: support from family (α = ~92), friends (α = .91), and a significant other (α = .84).
Depressive Symptoms
The Center for Epidemiologic Studies Depression Scale (CES-D) (Radloff, Reference Radloff1977; Spanish adaptation: Vázquez et al., Reference Vázquez, Blanco and López2007) is an original 20-item measure designed to assess symptoms of depression in the general population, with items phrased as self-statements (e.g., “I felt hopeful about the future”). Respondents rate how frequently each item applied to them over the course of the past week. Ratings are based on a 4-point Likert scale ranging from 0 (rarely or none of the time -less than 1 day-) to 3 (most or all of the time -5 to 7 days-). For the purposes of the current study, we used the 8-item brief version of the CES-D (Radloff, Reference Radloff1977), as it is oriented for its use in the general population for purposes of symptoms’ screening and risk factors detection. Scores in the 8-item version range from 8 to 32. The CES-D has demonstrated good reliability and validity in different populations and sociocultural contexts (Radloff, Reference Radloff1977). In this study, internal consistency showed a Cronbach’s alpha = .89.
Anxiety Symptoms
The Generalized Anxiety Disorder Scale (GAD–7) (Spitzer et al., Reference Spitzer, Kroenke, Williams and Löwe2006, Spanish adaptation: García-Campayo et al., Reference García-Campayo, Zamorano, Ruiz, Pardo, Pérez-Páramo, López- Gómez, Freire and Rejas2010) is a brief self-report measure to assess symptomatology and severity related to Generalized Anxiety Disorder over the course of the last two weeks. The scale has 7 items with 4-point Likert scale responses (0 = Never to 3 = almost every day). Scores range from 0 to 21. The GAD–7 has excellent reliability and validity (Spitzer et al., Reference Spitzer, Kroenke, Williams and Löwe2006). In this study internal consistency was also good, Cronbach’s alpha = .88. Beyond its intended use for GAD screening, this instrument has demonstrated high sensitivity to estimate individual differences in general anxiety symptomatology, showing high convergent validity with other measures of general anxiety levels (Kertz et al., Reference Kertz, Bigda-Peyton and Bjorgvinsson2013). This made the GAD highly suited for the purposes of anxiety levels screening in the present study.
Procedure
All participants completed the measures in a digital survey using Google Forms. Before taking part in the online data collection, participants were first informed on the purposes of the study, their anonymity and the confidentiality of all their responses. They were also provided with a contact email in case they had any further question before taking part in the study. Then, they signed a digital informed consent and completed the instruments (i.e., CD-RISC, MSPSS, CES-D and GAD–7), which were presented with clear instructions on how to respond to each of them. Participants’ identity was blinded to the researchers, who only had access to individuals’ anonymous responses, without accessing to any data that allowed personal identification of respondents. The study was approved by the Faculty Ethical Committee and was conducted in accordance with the Declaration of Helsinki.
Data Analytic Plan
Description of each variable and their psychometric properties were first computed. After determining that normality was met for all measures and the absence of multicollinearity between them, the main analyses were conducted. First, Pearson’s bivariate correlations were performed to test the associations between the different factors of the CD-RISC (i.e., coping and persistence, tolerance of negative affect and capacity for goal-oriented focus, positive appraisal, and trust factors) and the MSPSS dimensions (i.e., social support from family, friends, and a significant other), as well as, and the associations between these variables and the mental health outcomes (i.e., depression and anxiety levels).
In order to determine the explained variance of mental health outcomes by social support and personal resilience variables, a series of linear regression analysis were made, considering: (a) The contribution of each social support dimension to each of the personal resilience factors; and then (b) the specific contribution of each of these factors (i.e. social support and personal resilience variables) to account for individual differences in each mental health outcome (i.e. depression and anxiety), using stepwise regression models. Consequently, social support dimensions were entered as predictors in the regression models in the first step, and personal resilience factors were entered in the second step. Given the number of combined dependent tests concerning associations between social support dimensions, resilience factors and mental health outcomes, Benjamini-Hochberg p-value correction was applied to avoid false discovery rates (FDR) in all the models. This procedure computes the ratio of false positive (FP) classifications, that is, the false discoveries to the total of true positive (TP) classifications, known as rejection of the null. This method provides a helpful tool to control for the chance appearance of small significant p-values, and consequently diminishes the probability of appearance of Type I errors (Benjamini & Hochberg, Reference Benjamini and Hochberg1995). The reported p-values in the manuscript thus refer to those after applying Benjamini-Hochberg p-value corrections.
In order to test the hypothesized mediation models considering personal resilience factors as potential mediators of the associations between social support dimensions and mental health outcomes (see Figure 1), indirect effect models were finally conducted. To establish specific direct and indirect effects of each social support dimension, analyses were performed controlling for the covariance of the rest of social support dimensions under study, thus, entering them in the models as covariates. All the analyses were conducted using IBM SPSS Statistics 25. For the indirect effect models, we used the PROCESS SPSS macro (Hayes, Reference Hayes2022).

Figure 1. Hypothesized Mediation Models
Results
Preliminary Analyses
Mean and standard deviations of the variables evaluated in the study are shown in Table 1. Asymmetry and kurtosis tests were carried out for all the variables included in the study. All measures showed asymmetry and kurtosis lower to ±2, showing a normal distribution of the data (Lomax & Schumacker, Reference Lomax and Schumacker2012). Furthermore, bivariate correlations (see Table 2) showed that neither of the correlations between the resilience factors, the social support dimensions or between them were > .9, indicating absence of multicollinearity between these factors in the study.
Table 1. Mean and Standard Deviations of the Variables Included in the Study

Note. CD-RISC = Connor-Davidson Resilience Scale; MSPSS = Multidimensional Scale of Perceived Social Support; CES-D = Center for Epidemiologic Studies Depression scale; GAD–7 = Generalized Anxiety Disorder scale; M = Mean; SD = Standard deviation.
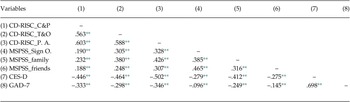
Table 2. Bivariate Correlations among Variables in the Study

Note. C&P = coping and persistence; T&O = tolerance of negative affect and capacity for goal-oriented focus; P.A. = Positive Appraisal; CD-RISC = Connor-Davidson Resilience scale; Sign O. = significant other; MSPSS = Multidimensional Scale of Perceived Social Support; CES-D = Center for Epidemiologic Studies Depression Scale; GAD–7 = Generalized Anxiety Disorder scale.
* p < .05.
** p < .01.
Bivariate Correlations
Bivariate correlations between all the variables evaluated in the study are shown in Table 2. As it can be seen in Table 2, all correlation coefficients between the variables in the study were statistically significant, all p’s < .05.
Correlation analysis showed high positive associations between the different personal resilience factors as well as between the different social support dimensions. Regarding the associations between personal resilience and social support variables, all these associations were positive and significant. Analyses also showed that all social support dimensions and personal resilience factors were negatively correlated with both depression and anxiety levels.
Regression Models
Social Support Dimensions Accounting for Individual Differences in Personal Resilience Factors
Regression models were used to test the predictive role of each social support dimension (i.e., friends, family, and significant others, as predictors in the model) on each personal resilience factor (i.e., coping and persistence, tolerance of negative affect and capacity for goal-oriented focus, positive appraisal), as dependent variables. Due to low reliability of the trust factor of the resilience scale (α = .28), this variable was no longer considered in regression and mediation analyses.
Coping and persistence during stress. As for the factor referred to coping and persistence, the equation explained 7.3% of the variance (R 2 corrected, p < .01). The social support dimension corresponding to support from family showed significant predictive power (β =.17, p < .01). In contrast, support from friends and from a significant other did not show predictive power (β = .09, p = .04; β = .07, p = .12, respectively).
Tolerance of negative affect and capacity for goal-oriented focus. Results showed that the equation explained a 17.9% of the variance (R 2 corrected, p < .01), with social support from family and a significant other being significant predictors for this variable (β = .29 and β = .15 respectively, both p’s < .01). Social support from friends did not show significant predictive power (β = .08; p = .07).
Positive appraisal. The equation explained a 22.8% of the variance (R 2 corrected, p < .01), with all social support dimensions demonstrating significant predictive power (β=.13 (significant other), β = .33 (family), β = .13 (friends), all p’s < .01).
Social Support Dimensions and Personal Resilience Factors Accounting for Individual Differences in Depression and Anxiety Levels
To establish the explained variance of social support dimensions, and personal resilience factors on mental health outcomes, we conducted a series of stepwise regression analyses separately for each mental health variable (i.e., depression, anxiety) as outcome variables. The social support dimension measures were entered in the first step of the equation model. In the second step, we entered the set of the three personal resilience factors separately (i.e., coping and persistence, tolerance of negative affect and capacity for goal-oriented focus, positive appraisal) as predictors.
Depression levels. Step 1 (social support dimensions) explained a 19.4% of the variance in depression levels (R 2 corrected, p < .01), with all the of social support dimensions being significant predictors (β = –.09 (other significant), β = –.33 (family) and β = –.12 (friends); all p’s < .05). When the three resilience factors were entered in Step 2 of this model, they accounted for another 16% of variance, with the full model explaining a total of 35.4% of variance in depression levels (R 2 corrected, p < .01). The dimension of social support from friends and significant other did not longer reach significance in Step 2 (β = –.07 and β = –.02, respectively, all p’s < .05) and the family dimension was the only social support significant predictor (β = –.20, p’s < .01). As for resilience factors, coping and persistence, tolerance and goal orientation and positive appraisal were all significant predictors (β = –.18; β = –.14; β = –.18, respectively, all p’s < .001) in step 2.
Anxiety levels. Step 1 (social support dimensions) explained 6.8% of the variance in anxiety levels (R 2 corrected, p < .01), with the dimension of social support from family being the only significant predictor (β = –.23; p < .05), while neither social support from friends nor from a significant other reached significance (β = –.08; and β = .03, respectively, both p’s > .05). When the three resilience factors were entered in the Step 2 of this model, they accounted for another 9.7% of variance, with the full model explaining a total of 16.5% of variance in anxiety levels (R 2 corrected, p < .001). The dimensions of social support from family did again reach significance in Step 2 (β = –.13; p < .01), whereas two resilience factors, coping and persistence and positive appraisals of stress, emerged as significant predictors in Step 2 (β = –.17 (coping and persistence), β = –.15 (positive appraisal) both p’s < .01). Tolerance of negative affect and capacity for goal–oriented focus did not reach significance (β = .07; p = .25).
Mediation Models
To evaluate the possible mediating role of personal resilience factors on the associations between social support dimensions and mental health outcome levels (i.e., depression and anxiety), we conducted a series of indirect effect models using the PROCESS macro for SPSS to estimate total, direct and indirect effects. Provided that preliminary assumptions to test indirect effect models (i.e., significant associations between the predictor and the mediator, as well as between the mediator and the outcome) were supported for all variables tested (see Table 2), we decided to restrict indirect effect models to those pathways with the most consistent statistical support, in accordance with the p-value corrected regression models. First, as for social support, we only considered social support dimensions that demonstrated significant predictive power to account for individual differences in each mental health outcome, after controlling for the variance explained by personal resilience factor: i.e., Social support from family. Second, as for potential mediators in the relations between those social support dimensions and mental health outcomes, we considered those resilience factors that were supported as significant predictors, after controlling for the influence of social support dimensions, of either depression and anxiety levels (i.e., coping and persistence, tolerance and goal orientation and positive appraisal for depression, and only the first and the latter for anxiety). Thus, two multiple-mediation models were finally tested, one considering 3 potential mediators (i.e., coping and persistence, tolerance and goal-oriented focus, and positive appraisal) in the association between social support from family and depression, and one considering 2 potential mediators (i.e., coping and persistence, and positive appraisal) in the association between social support from family and depression. The results from these models are summarized in Table 3.
Table 3. Analyses of Total, Direct and Indirect Effects for Each Multiple-Mediation Model

Note. IV = independent variable; M = mediator; DV = dependent variable.
As it can be seen in Table 3, all indirect effects were statistically supported, both for depression and anxiety outcomes. However, the direct effects of social support from family also remained significant in all models, thus supporting partial mediation effects of the personal resilience factors (coping and persistence, tolerance and goal-oriented focus and positive appraisal) in the relation between higher social support from family and lower depression and anxiety levelsFootnote 1.
Discussion
In the present study, we aimed to investigate the relation between social support dimensions (i.e., perceived social support from friends, family, and a significant other) and personal resilience factors, as well as the hypothetical pathways of association between these two types of protective variables and mental health outcomes (i.e., depression and anxiety levels) in a sample of Spanish young adults. Thus, this study was designed to provide an initial comprehensive view of the inter-relations among multidimensional social and personal protective factors that are thought to be relevant in a developmental stage marked by multiple challenges (Arnett et al., Reference Arnett, Žukauskienė and Sugimura2014) and characterized by high risk for depression and anxiety (Gustavson et al., Reference Gustavson, Knudsen, Nesvåg, Knudsen, Vollset and Reichborn- Kjennerud2018).
Previous research has supported the existence of positive relations between perceived social support and general resilience levels during emerging adulthood (e.g., Howard-Sharp et al., Reference Howard-Sharp, Schwartz, Barnes, Jamison, Miller-Graff and Howell2017; Malkoç & Yalçin, Reference Malkoç and Yalçin2015; Peng et al., Reference Peng, Zhang, Li, Li, Zhang, Zuo, Miao and Xu2012; Taylor et al., Reference Taylor, Doane and Eisenberg2014). However, there is a paucity with research examining how specific dimensions of social support relate to different personal factors of resilience. In the current study, we examined the associations of dimensions of perceived social support from friends, family and a significant other with a set of personal resilience factors, derived from previous studies testing the factorial structure of the Spanish version of the CD-RISC (Crespo et al., Reference Crespo, Fernández-Lansac and Soberón2014). We found significant positive relations between specific social support dimensions and personal resilience factors. Specifically, social support from family emerged as a dimension related to individual differences in all the three analyzed resilience factors, whereas support from a significant other was specifically related to tolerance of negative affect and goal-oriented focus and positive appraisal factor and, social support from friends was specifically related to positive appraisal.
Our results not only confirm previously observed relations between social support and general resilience levels (e.g., Howard-Sharp et al., Reference Howard-Sharp, Schwartz, Barnes, Jamison, Miller-Graff and Howell2017; Peng et al., Reference Peng, Zhang, Li, Li, Zhang, Zuo, Miao and Xu2012; Taylor et al., Reference Taylor, Doane and Eisenberg2014), but also show that certain dimensions of social support may be associated with specific personal factors of resilience. Thus, in line with extensive evidence in other developmental stages (see, for instance, the review of Smith & Carlson, Reference Smith and Carlson1997), our results, fully discussed below, indicate that perceived social support can be framed as series of potentially protective dimensions to promote resilience not only at earlier stages but also during emerging adulthood.
Stepwise regression models pointed to the specific importance of perceived support from family in young adults, being a significant predictor of the analyzed resilience factors (coping and persistence during stressful situations, tolerance of negative affect and goal-oriented focus and positive appraisal of stress). Interestingly, these results are in line with evidence from studies testing adolescents, where different dimensions of perceived support, from friends and from family, seem to have relative importance and unique contributions to adaptive functioning markers, such as well-being, related to resilience (Armstrong et al., Reference Armstrong, Birnie-Lefcovitch and Ungar2005; Milgram & Palti, Reference Milgram and Palti1993; Ringdal et al., Reference Ringdal, Bjørnsen, Espnes, Bradley Eilertsen and Moksnes2020). Yet, our findings also suggest that perceived social support from family may have a particular relevance in terms of resilience promotion when individuals reach emerging adulthood. In this case, this contrasts with previous studies indicating that perceived social support from family tend to decrease in its relevance during emerging adulthood, compared to childhood and adolescence (Gariépy et al., Reference Gariépy, Honkaniemi and Quesnel-Vallée2016; Gooding et al., Reference Gooding, Hurst, Johnson and Tarrier2012). Nonetheless, it is important to note the temporal context in which our study was conducted. Data collection of this study was performed during the COVID–19 pandemic (March-April 2021), a period comprising several restrictions limiting social contact with non-cohabitants, namely for instance, friends or non-cohabitating sentimental partners of the young adults. This might have influenced the subjective perception of support from these social sources, thus reducing their influence in resilience levels. In contrast, an increased perception of social support provided by the family during this period might have consequently had higher associations with individual differences in resilience levels during this period. In our study, 85.3% of the participants where cohabitating with one or more relatives at the time of completing the assessments. Therefore, it is plausible that the ongoing social restrictions due to the COVID–19 during the period in which the study was conducted and the resulting increased time and shared space with relatives might have had an influence in the results, in comparison to previous studies (Coventry et al., Reference Coventry, Gillespie, Heath and Martin2004). In line with this, there is already some initial evidence showing that restrictions due to the COVID–19 may have modulated social experiences and perceptions of support of young adults, shifting their social support seeking pathways from friends to family (Li et al., Reference Li, Luo, Mu, Li, Ye, Zheng, Xu, Ding, Ling, Zhou and Chen2021).
Previous studies have supported negative associations of global measures of both social support and resilience factors with mental health markers of depression and anxiety (e.g., Catabay et al., Reference Catabay, Stockman, Campbell and Tsuyuki2019; Haroz et al., Reference Haroz, Murray, Bolton, Betancourt and Bass2013; Sim et al., Reference Sim, Bowes and Gardner2019). The present study aimed to conduct a first analysis of the unique contributions of specific social support dimensions and personal resilience factors to account for individual differences in both depression and anxiety levels. First, our results supported significant negative bivariate correlations between social support and resilience variables with both depression and anxiety levels. These results are consistent with previous literature supporting the potentially protective effect of both social dimensions and personal resilience factors in mental health (e.g., Brailovskaia et al., Reference Brailovskaia, Schönfeld, Zhang, Bieda, Kochetkov and Margraf2018). However, stepwise regression analyses also indicated that both for social support dimensions and for resilience factors, different specific variables emerged as unique factors associated to each mental health outcome. In the case of social support dimensions, initial regression analyses indicated that perceived support from family, friends and a significant other were all significantly associated with lower depression. However, when the different resilience factors were entered in the Step 2 of regression models, only the dimension of social support from family remained as a factor significantly associated to lower depression levels, whereas social support from friends and a significant other did not longer reach significance. Individual differences in coping and persistence, tolerance goal- oriented focus and positive appraisal were all significantly and uniquely associated to lower depression levels. As for anxiety, only social support for family and personal resilience factors of coping and persistence, and positive appraisal emerged as significant associated to lower anxiety levels. These findings extend the support for a central role of perceived support from family in mental health in our sample as well as the relevance of personal resilience characteristics as potentially protective factors during emerging adulthood. Results highlight the particular relevance of cognitive processes comprising primary appraisals of stress intensity and secondary appraisals of coping abilities as central resilience factors for the promotion of mental health in young adults. This is in line with conceptual models of psychological stress and coping (Lazarus & Folkman, Reference Lazarus and Folkman1984; for an update review see Biggs et al., Reference Biggs, Brough, Drummond, Cooper and Quick2017), but also with current resilience frameworks that highlights adaptive processes of coping and cognitive appraisal as the ultimate mechanisms involved in the generation of resilience outcomes in response to challenges and adversities (Kalisch et al., Reference Kalisch, Müller and Tüscher2015). Furthermore, in line with predictions from current resilience frameworks (Kalisch et al., Reference Kalisch, Müller and Tüscher2015), and congruent with our hypotheses, results from stepwise regression pointed to a potential mediating role of these cognitive resilience factors in the associations between perceived social support dimensions and depression and anxiety outcomes in young adults.
In line with recent evidence pointing to a mediational role of personal resilience factors in accounting for the influence of social support dimensions in mental health (Brailovskaia et al., Reference Brailovskaia, Schönfeld, Zhang, Bieda, Kochetkov and Margraf2018; Cano et al., Reference Cano, González Castro, De La Rosa, Amaro, Vega, Sánchez, Rojas, Ramírez-Ortiz, Taskin, Prado, Schwartz, Córdova, Salas-Wright and de Dios2020), and supporting our mediational hypothesis, indirect effect models supported a mediating role of the personal resilience factors in accounting for the association between perceived support from family and depression and anxiety levels. These mediating effects were found when considering specific personal factors of coping and persistence, tolerance and goal-oriented focus and positive appraisal as mediators. However, these resilience factors only partially mediated the effects of social support from family in accounting for better mental health outcomes (i.e., both lower depression and anxiety levels). These results point out that perceived support from family seems to be the most relevant social support dimension for young adults, indirectly contributing to both depression and anxiety resistance through its association with personal factors of resilience (i.e., cognitive components of positive stress appraisals, goal-oriented focus and coping and persistence capacities), but also showing direct associations with mental health above and beyond these mediators.
These findings have interesting conceptual but also practical implications. One of the main goals for the promotion of resilience at developmental stages characterized by high risk for affective disturbances (Gustavson et al., Reference Gustavson, Knudsen, Nesvåg, Knudsen, Vollset and Reichborn- Kjennerud2018) is to design adequate social policies and applied protocols to prevent psychopathology onset. The focus on relevant dimensions of social support and personal resilience factors identified in this study can thus be useful as an applied approach to improve better coping with adverse situations in young adults facing multiple adversities and increased risk to develop affective and anxiety disorders. There is empirical evidence supporting the effectiveness of prevention approaches based on the promotion of resilience both in non-clinical (Hirani et al., Reference Hirani, Norris, van Vliet, van Zanten, Karmaliani and Lasiuk2018) and clinical populations (Chandler et al., Reference Chandler, Roberts and Chiodo2015; Steinhardt & Dolbier, Reference Steinhardt and Dolbier2008). As for similar future approaches for young adults, results from this study allow to identify a set of personal factors of resilience with potential to be included in psychological interventions for resilience promotion. This includes training on positive reappraisals of stress, goal-orientation and promotion of abilities to cope with and persist during stressful experiences. Of note, these are mainly primary targets in many psychological treatments for affective disorders (Berking et al., Reference Berking, Ebert, Cuijpers and Hofmann2013; Clark et al., Reference Clark, Beck and Alford1999) and thus cognitive-behavioral techniques could be efficiently adapted and integrated into new programs for the purpose of resilience promotion in young adults. Similarly, recent cognitive training methods targeting attention and interpretation processes involved in these forms of primary and secondary stress appraisals have been shown to improve emotion regulation capacities (Sanchez-Lopez et al., Reference Sanchez-Lopez, De Raedt, van Put and Koster2019) and could thus be used as promising add-ons to standardized programs of stress resilience promotion. Further, social support from family has been identified as a social protective factor for young adults, closely linked to the facilitation of these resilience factors. Thus, future prevention programs for young adults should consider integrating strategies to promote adaptive forms of family relations and integrate them in ways that facilitate adaptive cognitive appraisals and coping with stress. Ultimately, interventions that include social networking with friends and significant others might also contribute to these programs, although further research would be required to first establish their potential relevance at other contexts different to the one at which the present study was conducted (i.e., during a period characterized by high social restrictions due to COVID–19).
The above discussed implications are derived from an initial integrative approach to study the interplays of multidimensional social and personal resilience variables, and thus require further replications. The cross-sectional nature of our study does not allow us to infer causal pathways in our data. Nonetheless, as for the direction of interplays among social support dimensions and personal resilience factors, statistical findings were robust for our hypothetical models and did not support alternative models where social support dimensions might act as mediators of the associations between personal resilience factors and mental health outcomes. In any case, causal temporal links between these social and personal protective factors and depression and anxiety outcomes should be examined in future research using appropriate longitudinal designs. Future prospective studies should test the protective effects of social support and resilience factors across time and integrate these pathways in relation to individual differences in the degree of experience of stress among young adults. Further research is also warranted to establish the protective effects of these factors beyond resilience outcomes of psychopathology resistance (i.e., low levels of depression and/or anxiety in the face of stress), further considering its role in promoting other relevant resilience outcomes such as maintained psychological well-being levels in the face of stress and the frequency of use of adaptive behaviors to reach adult-related goals during emerging adulthood (Arnett, Reference Arnett2000, Reference Arnett2014; Furstenberg, Reference Furstenberg2015; Settersten & Ray, Reference Settersten and Ray2010). Furthermore, another potential limitation that must be addressed is the fact that the selection of the sample was based on a purposive sampling method, increasing risk of a selection bias and of a not representative sample of Spanish emerging adults. However, taking into account the temporal moment where the sample was collected (as noted above, during the COVID–19 pandemic: March-April 2021), it is important to note that similar results in mental health rates to the ones found in our study have been reported in other contemporaneous studies. For instance, in a systematic review and meta-analysis conducted by Zhang et al. (Reference Zhang, Chen, Xu, Yin, Dong, Chen, Delios, Miller, McIntyre, Ye and Wan2022), indicate similar rates of anxiety and depression in young adult samples as the ones in our study, showing, for instance, that the overall anxiety rates in young adults across studies conducted during that period were at 39%, 95% CI [18, 62] compared to the 38.2% reported in our study. Similarly, the systematic review and meta-analysis showed that the levels of depression in young adults during that period were at 59%, 95% CI [58, 61], compared the 53.4% reported in our study.
In conclusion, despite the above-mentioned limitations, this study represents an important initial step to study the multifactorial nature of social and personal variables that may help to promote resilience outcomes during a challenging developmental period, such as emerging adulthood. Future research extending this approach to disentangle the full network of interplays among social support dimensions and personal resilience factors and their contributions to mental health outcomes has a large potential to inform new effective social policies and prevention programs for young adults.