Introduction
The international community must now recognise that, despite their differences, the planet’s and humans' health are inextricably linked to one another and, taken as a whole, offer a critical path for mitigation (Demaio and Rockström, Reference Demaio and Rockström2015). Considering these two aspects, which, as stated prima facie, look unrelated, human health is possibly the best recognised. Regarding planetary health, this one is more likely to be identified with global health. By contrast, global health per se does not fully contemplate the setting we live in, the Earth itself (Horton, Reference Horton2013). In this context, the Rockefeller Foundation–Lancet Commission on Planetary Health defined planetary health as the accomplishment of the utmost achievable level of healthiness, welfare and fairness at the global level via thoughtful attentiveness to the social–political–economic systems that outline humanity’s future as well as the Earth’s natural systems, which outline the healthy environmental limits within which humanity may prosper. In simpler words, the state of human civilisation and the natural systems it depends on is called planetary health (Horton and Lo, Reference Horton and Lo2015; Jones et al., Reference Jones, Reid and Macmillan2022). Alternatively, the Canmore Declaration understands planetary health as the inter-dependent vitality of all natural and anthropogenic ecosystems, emphasising that achieving planetary health depends on the interconnected systems of life and our approach to living (Jones et al., Reference Jones, Reid and Macmillan2022). The philosophy of planetary health relies on the understanding that thriving natural systems and intelligent governance of such systems are essential for human health and civilisation. Nonetheless, natural systems are being degraded to a certain extent, which has never been seen in human history (Whitmee et al., Reference Whitmee, Haines, Beyrer, Boltz, Capon, de Souza Dias, Ezeh, Frumkin, Gong, Head, Horton, Mace, Marten, Myers, Nishtar, Osofsky, Pattanayak, Pongsiri, Romanelli, Soucat, Vega and Yach2015).
Planetary health emphasises the effects of anthropogenic disruptions on Earth’s natural systems, that is limited resources, land-use changes, climate change and biodiversity loss. Food insecurity, the spread of vector-borne diseases and high heat- and air-related mortality rates are just a few of the effects of these disturbances. According to the World Health Organization (WHO), environmental degradation is responsible for nearly one-fourth of all deaths and diseases worldwide (Hampshire et al., Reference Hampshire, Islam, Kissel, Chase and Gundling2022).
The 2016 UN Climate Change Conference highlighted that climate affects disease patterns, death rates, human living conditions, nutrition, water and hygiene, resulting in an upward trend in temperatures, sea levels and extreme events. Flooding, which can increase the risk of water-related illnesses and vector-borne illnesses; food manufacturing – both in terms of lengthened dry spell cycles and decreased micronutrients in staple crops – and the contaminants linked to carbon emissions – all of which are detrimental to human health (COP22, ). Climate change also influences human and animal health by altering the conditions for pathogens and vectors of zoonotic diseases, posing new challenges to maintaining human and animal health (Leal Filho et al., Reference Leal Filho, Ternova, Parasnis, Kovaleva and Nagy2022).
Regarding zoonosis, it is an infectious disease that has jumped from a non-human animal to humans (WHO, 2021). In other words, it is a direct infection acquired naturally from animals causing disease. Zoonotic diseases can be caused by pathogens that can spread to humans through direct or indirect contact with animals, vector-borne transmission, foodborne transmission or waterborne transmission (CDC, 2021). A zoonotic pathogen can undergo replication and mutation under selective pressure within a human host, enabling the pathogen to acquire the ability to efficiently transmit from person to person, subsequently leading to an emerging infectious disease in human populations unrelated to its zoonotic origins (Escudero Pérez et al., Reference Escudero-Pérez, Lalande, Mathieu and Lawrence2023). Noteworthy recent examples include the 2022 global outbreak of Mpox (formerly known as Monkeypox) and likely the COVID-19 pandemic (Haider et al., Reference Haider, Rothman-Ostrow, Osman, Arruda, Macfarlane-Berry, Elton and Kock2020; Orviz et al., Reference Orviz, Negredo, Ayerdi, Vázquez, Muñoz-Gomez, Monzón, Clavo, Zaballos, Vera, Sánchez, Cabello, Jiménez, Pérez-García, Varona, del Romero, Cuesta, Delgado-Iribarren, Torres, Sagastagoitia, Palacios, Estrada, Sánchez-Seco, Ballesteros, Baza, Carrió, Chocron, Fedele, García-Amil, Herrero, Homen, Mariano, Martínez-Burgoa, Molero, Navarro, Núñez, Perez-Somarriba, Puerta, Rodríguez-Añover, Pastrana, Jiménez, de la Vega, Vergas and Zarza2022; Sharif et al., Reference Sharif, Sharif, Alzahrani, Halawani, Alzahrani, Díez and Dey2023). The complex links between human, animal and environmental health require coordinated multidisciplinary and multipronged collaboration to address the threats from zoonotic diseases, and the global public health community needs to act decisively now. Therefore, the importance of One Health, defined by the quadripartite WHO-WOAH-FAO-UNEP as an integrated, unifying approach that aims to sustainably balance and optimise the health of people, animals and ecosystems – It recognises the health of humans, domestic and wild animals, plants and the wider environment (including ecosystems) are closely linked and inter-dependent. The approach mobilises multiple sectors, disciplines and communities at varying levels of society to work together to foster well-being and tackle threats to health and ecosystems while addressing the collective need for clean water, energy and air, safe and nutritious food, taking action on climate change and contributing to sustainable development (WOAH, 2021). Hence, One Health is critical to addressing zoonotic public health threats, environmental issues and neglected tropical diseases to attain sustainable development goals (WHO, 2022).
However, implementing planetary health initiatives at the local level presents many challenges, some overlapping with those encountered in implementing One Health programmes (Bordier et al., Reference Bordier, Uea-Anuwong, Binot, Hendrikx and Goutard2020). In this regard, Mwatondo et al. (Reference Mwatondo, Shepherd, Hollmann, Chiossi, Maina, Kurup, Hassan, Coates, Khan, Spencer, Mutono, Thumbi, Muturi, Mutunga, Arruda, Akhbari, Ettehad, Ntoumi, Scott, Nel, Ellis-Iversen, Wolff Sönksen, Onyango, Ismail, Simachew, Wolking, Kazwala, Sijali, Bett, Heymann, Kock, Zumla and Dar2023) stated a need to increase domestically available financial resources for national and subnational One Health Networks.
Human health is currently at its highest quotas, with increased life expectancy and decreased global mortality rates in children under five. Over the past quarter-millennium, humans have been highly successful, performing a “great escape” from extreme dearth. Despite the upsurge in the total population of less developed countries, the overall number of people living in extreme poverty has dropped over the last 30 years, followed by unparalleled advancements in public health, healthcare, education, the human rights legislation framework and industrial evolution that have brought humanity innumerable benefits – despite their unfairness – and untold benefits (Whitmee et al., Reference Whitmee, Haines, Beyrer, Boltz, Capon, de Souza Dias, Ezeh, Frumkin, Gong, Head, Horton, Mace, Marten, Myers, Nishtar, Osofsky, Pattanayak, Pongsiri, Romanelli, Soucat, Vega and Yach2015). On the other hand, the state of the rest of the biosphere is the worst it has ever been in human history. Climate change may threaten human health in a variety of ways, primarily direct and indirect ones, that is extreme weather events; communicable diseases that are mediated by environmental, social and demographic changes and military conflicts, which are intervened by more dispersed and complex social disruptions (Arber et al., Reference Arber, Raven, Frumkin and Viana2020). Further, several environmental factors can potentially affect agricultural production, such as freshwater provision and sanitation, burning of biomass fuels and atmospheric air emissions, the occurrence and spread of diseases that are sensitive to climate change, and nutrient and waste absorption and detoxification (Haines et al., Reference Haines, Whitmee and Horton2014).
The Industrial Revolution’s intensification of human activities in the late 19th century caused soil, rivers and the air we breathe to become contaminated, harming our health and the natural systems supporting us. Afterwards, the gases created by pollution, burning fossil fuels and deforestation significantly changed the entire planet’s atmosphere, being the cause of global climate change that became apparent about 75 years ago (Arber et al., Reference Arber, Raven, Frumkin and Viana2020). Climate change would then respond by impacting and threatening human and planetary health. This chain reaction accelerated biodiversity loss worldwide, raising population morbidity and mortality rates.
Every region worldwide will likely experience further increases in climate hazards shortly, increasing multiple risks to ecosystems and people. A rise in heat-related human mortality and morbidity, food-, water-, and vector-borne illnesses, difficulties with mental health, flooding in coastal and other low-lying cities and regions, biodiversity loss in the land, freshwater, and ocean ecosystems, and a decline in air quality are among the dangers and risks anticipated in the near terms (Lee and Romero, Reference Lee and Romero2023).
A bibliometric analysis of climate change and zoonosis (Leal Filho et al., Reference Leal Filho, Ternova, Parasnis, Kovaleva and Nagy2022) found that the top four author keywords were “climate change,” “zoonosis,” “epidemiology” and “One Health,” and the authors' keywords' largest node of the bibliometric map contained the following: infectious diseases, emerging diseases, disease ecology, One Health, surveillance, transmission and wildlife. The research also revealed that zoonotic diseases, documented in the literature in the past, have evolved, especially during 2010–15, as evidenced by a sharp augmentation and peaking in 2020 with the COVID-19 outbreak, an emerging disease with a probable zoonotic origin.
Besides, the global crises COVID-19 pandemic and the human-induced impact on Earth’s life-support systems and planetary boundaries have reinvigorated the One Health and planetary health concepts, which build on equivalent systemic principles (Ruiz de Castañeda et al., Reference Ruiz de Castañeda, Villers, Faerron Guzmán, Eslanloo, de Paula, Machalaba, Zinsstag, Utzinger, Flahault and Bolon2023). The increased attention to One Health after the COVID-19 pandemic is an opportunity to focus efforts and resources on areas that need them most (Mwatondo et al., Reference Mwatondo, Shepherd, Hollmann, Chiossi, Maina, Kurup, Hassan, Coates, Khan, Spencer, Mutono, Thumbi, Muturi, Mutunga, Arruda, Akhbari, Ettehad, Ntoumi, Scott, Nel, Ellis-Iversen, Wolff Sönksen, Onyango, Ismail, Simachew, Wolking, Kazwala, Sijali, Bett, Heymann, Kock, Zumla and Dar2023).
This review combines:
-
1. An exploration of the recent literature on environmental changes affecting human, animal and planetary health.
-
2. A bibliometric analysis to understand better the quantitative evaluation of planetary health, health and climate change from 2012 to 22.
-
3. A reflection on the Research Directions One Health question: How can we improve and facilitate multi-sectoral collaboration in warning and response systems for infectious diseases and natural hazards to account for their drivers, interdependencies and cascading impacts? Our search addressed one and planetary health interactions, warning and surveillance, and capacity building in higher education institutions.
In 1 and 3, we complemented our search with the help of artificial intelligence (AI).
The structure of this review is as follows: In section “Methods”, we describe the methodological approaches. Section “Reviewing the environmental changes affecting human, animal and planetary health” summarises the state of the art of the environmental challenges on human and planetary health. Section “Results of the bibliometric analysis” presents the results of the bibliometric analysis from 2012 to 22 with a discussion. In section “Addressing the Research Directions question”, we address the Research Directions question. Finally, we summarise and conclude in section “Overall Summary and Conclusion”.
Methods
We combined qualitative and quantitative approaches. First, we explored the recent literature and comprehensive search on Planetary Health and One Health (section 3). We identified several articles and reports supporting climate change’s influence on the environment in which we live, human health and planetary health. In this context, comprehensive information was made available by exploring PubMed, Google Scholar and ScienceDirect databases for published journal articles and reports in English over the last decade. Also, we searched the websites of international organisations, that is the WHO, Intergovernmental Panel on Climate Change, Convention on Biological Diversity, World Wildlife Fund, Global Nutrition Report and United Nations Environmental Programme (UNEP).
Besides, we conducted complementary research with the help of the Microsoft AI tool, Copilot, to answer questions and identify sources related to our research topic. Copilot is an AI companion that provides information, answers questions and generates content using natural language processing and web search technologies (Harvard Online, 2023).
Second (Section 4) involved a bibliometric analysis to quantitatively assess the literature about the relationship between planetary health, health and climate change. In this research, we used the Scopus database by applying the following query: ( TITLE-ABS-KEY ( “planetary health” ) AND TITLE-ABS-KEY ( health ) OR TITLE-ABS-KEY (well-being) OR TITLE-ABS-KEY (well-being) AND TITLE-ABS-KEY ( “climate chang*” ) OR TITLE-ABS-KEY ( “climate variab*” ) ) AND PUBYEAR>2011 AND PUBYEAR <2023 AND ( LIMIT-TO ( LANGUAGE, “English” ) ) AND ( LIMIT-TO ( PUBSTAGE, “final” ) ). We identified 448 publications from 2012 to 2022, after removing doubled documents. For additional data analysis, we utilised the VOSViewer software. Table 1 provides summarised information about the search approach.
Table 1. Scopus search approach

Thirdly (section 5), we addressed the Research Directions question, focusing on animal, human and planetary health interactions, warning and surveillance, and capacity building in higher education institutions.
Reviewing the environmental changes affecting human, animal and planetary health
This section summarises the main environmental changes affecting human, animal and planetary health based on a targeted literature review of recent publications, including the state of the art of heat, extreme weather events and air pollution (Table 2).
Table 2. Summary of the most significant environmental challenges to human, animal and planetary health posed by heat, extreme weather events and air pollution

Table 3 summarises other relevant environmental changes.
Table 3. Summary of the environmental challenges to human and planetary health posed by food security and undernutrition, water scarcity and sanitation, vector-borne and zoonotic diseases, biodiversity loss and agriculture and deforestation

Finally, we comment on the surveillance system from the One and Planetary Health perspectives.
Heat, extreme weather events and air pollution
Rising atmospheric temperatures harm the health of all plants, animals and people who live on Earth (Sampath et al., Reference Sampath, Shalakhti, Veidis, Efobi, Shamji, Agache, Skevaki, Renz and Nadeau2023). Data analysis from 65 million deaths and temperature estimates in nine countries indicates that 17 causes of death are linked to extreme heat or cold, with the majority being cardiorespiratory or metabolic diseases. Extreme heat and cold were responsible for 17% of all deaths worldwide in 2019, of which 356,000 were related to heat (Lancet, Reference Lancet2021). Evidence suggests climate change has accelerated the spread of infections in the northern hemisphere because the global climate crisis can also alter the nature of zoonotic infections through its effect on temperature and precipitation (Sipari et al., Reference Sipari, Khalil, Magnusson, Evander, Hörnfeldt and Ecke2021).
Available data indicate that the rise in temperature and extreme weather events significantly impact vectors, rodents and foodborne pathogens. Numerous vector-borne diseases, such as dengue, chikungunya, visceral leishmaniasis and Lyme disease, are experiencing an increase in both incidence and geographic distribution (Stone et al., Reference Stone, Tourand and Brissette2017; Wahid et al., Reference Wahid, Ali, Rafique and Idrees2017; Pasquali et al., Reference Pasquali, Baggio, Boeger, Gonzalez-Britez, Guedes, Chaves and Thomaz-Soccol2019; Brady and Hay, Reference Brady and Hay2020; Vandekerckhove et al., Reference Vandekerckhove, De Buck and Van Wijngaerden2021; Yang et al., Reference Yang, Quam, Zhang and Sang2021). Although other factors related to global change, including urbanisation, land-use change and international travel, may be related (Tatem et al., Reference Tatem, Huang, Das, Qi, Roth and Qiu2012; Wilke et al., Reference Wilke, Beier and Benelli2019; Swei et al., Reference Swei, Couper, Coffey, Kapan and Bennett2020), the rise in mean temperatures play a crucial role in the increased prevalence of vector-borne diseases. This is attributable to an accelerated life cycle of the vector, heightened blood-feeding activity, a shorter extrinsic incubation period of the pathogens and increased fecundity facilitated by warmer temperatures (Hlavacova et al., Reference Hlavacova, Votypka and Volf2023; Rivas et al., Reference Rivas, de Souza, Peixoto and Bruno2014; Mordecai et al., Reference Mordecai, Caldwell, Grossman, Lippi, Johnson, Neira and Villena2019; Winokur et al., Reference Winokur, Main, Nicholson and Barker2020; Wiskel et al., Reference Wiskel, Al-Lawati and Humphrey2023). Moreover, extreme events like floods can elevate the incidence of mosquito-borne diseases due to the proliferation of potential breeding sites and increased humidity, contributing to higher vector survival (Coalson et al., Reference Coalson, Anderson, Santos, Madera Garcia, Romine, Luzingu, Dominguez, Richard, Little, Hayden and Ernst2021; Nosrat et al., Reference Nosrat, Altamirano, Anyamba, Caldwell, Damoah, Mutuku, Ndenga, LaBeaud and Viennet2021). Conversely, these events can reduce the risk of tick-borne diseases by creating a hostile environment for tick survival (Weiler et al., Reference Weiler, Duscher, Wetscher and Walochnik2017; Bidder et al., Reference Bidder, Asmussen, Campbell, Goffigan and Gaff2019). On the other hand, drought could increase the risk of certain mosquito-borne diseases by augmenting the number of breeding sites through the proliferation of water storage tanks and other containers near households (Chretien et al., Reference Chretien, Anyamba, Bedno, Breiman, Sang, Sergon and Linthicum2007; Trewin et al., Reference Trewin, Kay, Darbro and Hurst2013).
Furthermore, rodents are crucial reservoir hosts for zoonotic pathogens such as Leptospira and Hantaviruses. Also, they serve as potential reservoirs for emerging infectious diseases (Han et al., Reference Han, Schmidt, Bowden and Drake2015).
Heavy rainfall and high temperatures in the winter can significantly impact the epidemiology of rodent-borne pathogens by altering the food resources available and, thus, the population size of reservoir species (Engelthaler et al., Reference Engelthaler, Mosley, Cheek, Levy, Komatsu, Ettestad and Bryan1999; Muschetto et al., Reference Muschetto, Cueto, Cavia, Padula and Suárez2018). Floods and droughts can intensify the rodent–human interaction because food and habitat shortages can draw the rodents near households and buildings (Gubler et al., Reference Gubler, Reiter, Ebi, Yap, Nasci and Patz2001; Fichet-Calvet et al., Reference Fichet-Calvet, Lecompte, Koivogui, Soropogui, Doré, Kourouma and Meulen2007) and increase the susceptibility of the reservoirs to infections (Eads et al., Reference Eads, Biggins, Long, Gage and Antolin2016). In this context, Leptospirosis is a rodent-borne disease closely linked to heavy rainfall and flooding. Flooding can lead to increased human contact with contaminated water, the displacement and concentration of rodents and humans in dry areas, the dispersion of leptospires in the soil and the creation of poor hygienic conditions. A previous systematic review on this subject suggests that approximately 23% of leptospirosis outbreaks worldwide between 1970 and 2012 could be attributed to exposure to water during floods and extreme weather events (Munoz-Zanzi et al., Reference Munoz-Zanzi, Groene, Morawski, Bonner, Costa, Bertherat and Schneider2020).
Additionally, elevated temperatures and increased precipitation have been linked to higher incidences of certain foodborne diseases, such as Salmonellosis and Campylobacteriosis (Djennad et al., Reference Djennad, Lo Iacono, Sarran, Lane, Elson, Höser, Lake, Colón-González, Kovats, Semenza, Bailey, Kessel, Fleming and Nichols2019; Lee et al., Reference Lee, Chang, Sarnat and Levy2019; Kuhn et al., Reference Kuhn, Nygård, Guzman-Herrador, Sunde, Rimhanen-Finne, Trönnberg and Ethelberg2020; Morgado et al., Reference Morgado, Jiang, Zambrana, Upperman, Mitchell, Boyle, Sapkota and Sapkota2021). This association is partially attributed to high temperatures facilitating the rapid replication of most foodborne pathogens, thereby heightening the risk of contamination along the food production chain. Conversely, heavy rainfall enhances the likelihood of water supplies and agricultural products becoming contaminated by facilitating the transport and dispersion of animal and human faeces containing the pathogens (Semenza et al., Reference Semenza, Herbst, Rechenburg, Suk, Höser, Schreiber and Kistemann2012).
The direct effects of heat on human health include heatstroke, cardiovascular, cerebrovascular, and respiratory conditions, and early mortality. Evidence suggests that temperatures above long-term averages during the summer and specific heat extremes (such as heat waves) cause an increase in mortality. One of the leading weather-related causes of death in high-income nations is heat. In addition, hot weather and heat extremes increase emergency room visits and hospital admissions, cardiorespiratory and other disease deaths, mental health problems, health care costs and several other outcomes besides mortality. Regardless of income, studies consistently demonstrate that adults over 65, those with cardiopulmonary and other chronic diseases, and very young children are especially susceptible to the effects of heat (Ebi et al., Reference Ebi, Capon, Berry, Broderick, de Dear, Havenith, Honda, Kovats, Ma, Malik, Morris, Nybo, Seneviratne, Vanos and Jay2021).
Air pollution, a globally distributed environmental change, is the most significant environmental health risk factor, although not always related to a cause/effect of climate change (Arber et al., Reference Arber, Raven, Frumkin and Viana2020). Air pollution causes millions of premature annual deaths and healthy years of life and is connected to many harmful health outcomes, including cancer, neurological issues, cardiovascular and respiratory disease, and birth outcomes (The Lancet Planetary Health, 2022; Southerland et al., Reference Southerland, Brauer, Mohegh, Hammer, van Donkelaar, Martin, Apte and Anenberg2022). Globally, there is a higher mortality rate today related to air pollution than HIV, malaria and tuberculosis altogether (COP22, ).
In 2019, 99% of people on Earth lived in areas where the WHO’s recommended air quality levels needed to be met (WHO, 2022), and circa one in six premature deaths per year were attributable to global pollution due to air and toxic pollution.
Regarding animal health, birds can develop respiratory distress, impaired reproduction and increased susceptibility to infections when exposed to air pollutants like aerosolised heavy metals, particulate matter and nitrogen oxides (Barton et al., Reference Barton, Henderson, Border and Siriwardena2023). Similarly, exposure to urban air pollution has been associated with the presence of carbon in the airway macrophages (anthracosis) in urban wildlife, companion and zoo animals (Ahasan et al., Reference Ahasan, Chowdhury, Azam, Parvin, Rahaman and Bhuyan2010; Leya et al., Reference Leya, Oh, Ha, Tien, Cha, Park and Kim2023; Torres-Blas et al., Reference Torres-Blas, Horsler, Paredes, Perkins, Priestnall and Brekke2023). Anthracosis has been associated with an increased risk of lung cancer in dogs (Bettini et al., Reference Bettini, Morini, Marconato, Marcato and Zini2010).
Impacts of Global Change on animal health
Global change can profoundly affect the health of both wild and domestic animals. Climate change and land-use alterations can modify the geographical range, interactions and abundance of various species and their pathogens (Hoberg and Brooks, Reference Hoberg and Brooks2015; Williams et al., Reference Williams, Freeman, Spooner and Newbold2022). These new interactions between pathogens and potential hosts create opportunities for spillover and infection across different species. Models developed for viral and parasitic pathogens project an increase in spillover events in the future under climate change conditions (Morales-Castilla et al., Reference Morales-Castilla, Pappalardo, Farrell, Aguirre, Huang, Gehman, Dallas, Gravel and Davies2021; Carlson et al., Reference Carlson, Albery, Merow, Trisos, Zipfel, Eskew and Bansal2022). Changes in host–pathogen interactions within climate change can threaten wildlife conservation; the global decline in some amphibian species adapted to cool weather could be explained by the interaction of rapidly rising temperatures and the infection of the pathogenic fungus Batrachochytrium dendrobatidis (Cohen et al., Reference Cohen, Civitello, Venesky, McMahon and Rohr2019).
Similarly, anthropogenic modifications such as water pollution and rising water temperatures might have played a pivotal role in disseminating fibropapillomatosis in marine turtles. This neoplastic disease is potentially induced by the infection with a herpesvirus and the complex interaction of poorly understood external factors (Manes et al., Reference Manes, Pinton, Canestrelli and Capua2022).
Furthermore, the anthropogenic drivers of emerging infectious diseases in wildlife can be categorised into those that induce immune suppression, such as pollution; those that facilitate spillover events, like habitat loss and urbanisation; and those that enable pathogen dispersion, such as international travel and trade (Manes et al., Reference Manes, Carthy and Hull2023).
The rise in temperatures driven by climate change can also affect the health and welfare of food-producing animals by increasing heat stress, elevating the risk of metabolic diseases, inducing oxidative stress and impairing immune function (Lacetera, Reference Lacetera2019).
Surveillance and warning system
The duplication of the human population in the last 50 years has exposed more people living closely to wildlife, livestock and pets, increasing the chances for zoonotic diseases to pass between animals and people. About three quarts of all emerging virus-associated infectious diseases have a zoonotic origin. One Health-inspired environmental surveillance campaign is the preferred tool for monitoring human-adjacent environments for known yet-to-be-discovered infectious diseases. One Health-driven approaches facilitate surveillance and harbour the potential of preparing humanity for future pandemics caused by aetiological agents with environmental reservoirs (Leifels et al., Reference Leifels, Khalilur Rahman, Sam, Cheng, Chua, Nainani, Kim, Ng, Kwok, Sirikanchana, Wuertz, Thompson and Chan2022).
From a Planetary Health perspective, a surveillance system should collect, analyse and share health and environmental data at different scales and be able to assess complex relations and trends (Haines et al., Reference Haines, Hanson and Ranganathan2018). From a One Health perspective, a joint surveillance and warning system should be developed using a transdisciplinary approach, fostering policy, institutional and operational collaboration to enhance cooperation among the institutions involved in environmental, animal and human Health (Bordier et al., Reference Bordier, Uea-Anuwong, Binot, Hendrikx and Goutard2020). Surveillance should focus on the drivers of disease rather than the disease itself, which should give signals that account for human and animal health and environmental degradation (Drewe et al., Reference Drewe, George and Häsler2023).
Results of the bibliometric analysis
Using the search query referred to in the methods section, between the years 2012 and 2022, we pointed out 448 published documents in English. Furthermore, we verified any publications that may have been listed twice, but the total number of publications remained the same.
Documents by the year of publication
The scientific literature published from 2012 to 2022 demonstrates that planetary health has gained more interest, mainly since 2017, as supported by the Scopus database. As a result, there were 149 publications in 2022, as opposed to 1 in 2013 (Figure 1).

Figure 1 Documents by the year of publication.
Documents by source
Figure 2 shows the most frequently published articles. Lancet Planetary Health had the majority (n = 74), followed by the Lancet (n = 23), International Journal of Environmental Research and Public Health (n = 21) and Frontiers in Public Health (n = 15). The other four following journals' publications ranged between 5 and 10 documents. Interestingly, Lancet Planetary Health and Frontiers in Public Health indicate a later publishing history on this subject than other journals. Most papers from the top four sources were released between 2020 and 2022.

Figure 2. Documents by source, over 2012–2022.
Documents by affiliation
The London School of Hygiene and Tropical Medicine (n = 27) topped the list of institutions actively participating in publishing documents on the subject, followed by the University of Washington (n = 19), the Australian National University (n = 16), the Harvard T.H. Chan School of Public Health (n = 15) and University of Melbourne (n = 14) (Table 4).
Table 4. Documents by affiliation

Documents by country
The United States was in the top spot with the most publications (n = 162), followed by the United Kingdom (n = 112), Australia (n = 72), Canada (n = 51) and Germany (n = 46) (Table 5).
Table 5. Documents by country

Documents by type
The “Articles” category, with 178 publications (40%), accounted for the most significant percentage of the literature on our topic of interest, followed by “Notes” with 91 publications (20%), “Reviews” with 81 publications (18%), “Editorial” with 34 publications (8%) and “Book Chapter” with 28 publications (6%), round out the top five categories under document type analysis.
Co-authorship analysis
We used “Countries” as the unit of analysis for the co-authorship analysis. While choosing the threshold, we set the requirements for a minimum number of documents and citations for a country to be 5, correspondingly. As a result, only 28 of the 89 countries met the requirement. The United States topped the list with the most documents (n = 160) and 5583 citations. The United Kingdom came second (n = 112) with 4183 citations. Australia, Canada and Germany ranked third, fourth and fifth, respectively. Australia counted 72 publications and 1564 citations, followed by Canada with 51 publications and 2722 citations, versus Germany, which counted 46 and 1240 citations.
Four clusters were visible using the VOSviewer (Figure 3): the red cluster – nine items (United States, United Kingdom, Brazil, Canada, Chile, Colombia, Kenya, Malaysia and South Africa); the green cluster – 9 items (Austria, China, Finland, Germany, India, Japan, Philippines, Sweden and Switzerland); the blue cluster – 9 items (Belgium, Denmark, France, Indonesia, Ireland, Italy, the Netherlands, Norway and Spain); and the yellow cluster including only one item – Australia. Countries that belonged to the same cluster had significant interests in the same scientific field. As shown in subsection 4.4, the United States and the United Kingdom had the highest percentage of published documents relevant to our topic. The same can be affirmed if referring to the large node visualised on the map produced by VOSviewer. Furthermore, a strong collaboration between these two countries is indicated by the close distance between the two nodes that represent them.

Figure 3. Co-authorship analysis.
Co-occurrence analysis
We applied the “Author keywords” as our analysis units in the co-occurrence analysis and set 5 as the minimum number of keyword occurrences. As a result, out of 890 keywords, 43 met the threshold when the criteria above were used. The top five keywords used by researchers in publications about planetary health’s relation to human health and climate change were: “climate change”, “planetary health”, “sustainability”, “public health” and “environmental health” (Figure 4).
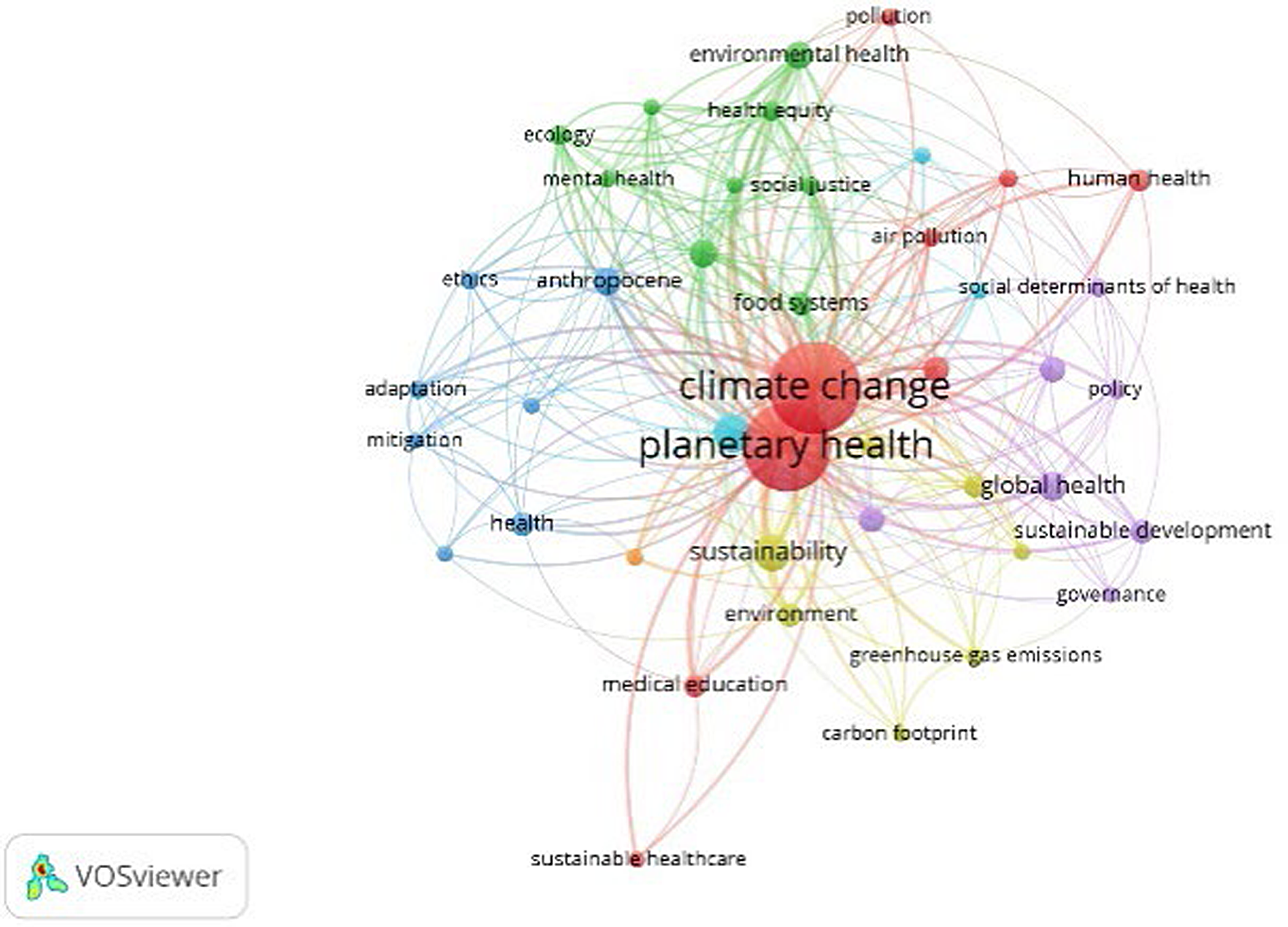
Figure 4. Visualisation of co-occurrence analysis by authors’ keywords, using VOSviewer.
Seven clusters were detected in the VOSviewer visualisation (Figure 4): the red cluster representing nine items (e.g., air pollution, climate change, COVID-19, human health, medical education, planetary health, pollution, sustainable healthcare and urbanisation); the green cluster representing nine items (e.g., biodiversity, ecology, environmental health, food systems, health equity, health promotion, mental health, microbiome and social justice); the blue cluster representing seven items (e.g., adaptation, Anthropocene, ethics, global warming, health, mitigation and well-being); the yellow cluster representing seven items (e.g., carbon footprint, environment, food security, greenhouse gas emission, nutrition, planetary boundaries and sustainability); the purple cluster representing seven items (e.g., global health, governance, One Health, policy, social determinants of health, sustainable development and sustainable development goals); the cyan cluster representing three items (e.g., public health, infectious diseases and system thinking); and the orange cluster representing only one item – higher education.
Citation analysis
We applied the “Sources” counting method to citation analysis, establishing five as the bare minimum for the number of a source’s documents and its citations. It resulted that out of 214 sources, 11 met the threshold. Table 6 shows that the top ten cited sources are led by The Lancet (n = 1759), followed by The Lancet Planetary Health (n = 1231), the International Journal of Environmental Research and Public Health (n = 505), Journal of Climate Change and Health (n = 264) and Nature Food (n = 260).
Table 6. Citation analysis by the source of publication

Bibliographic coupling
We applied “Documents” as the unit of analysis for the bibliographic coupling and set 5 as the minimum number of citations for a document. Out of 448 documents, 226 met the threshold. As a result, we obtained eleven clusters from the map (Figure 5). With a total of 1440 citations, the article with the most citations was “Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation-Lancet Commission on planetary health” (Whitmee et al., Reference Whitmee, Haines, Beyrer, Boltz, Capon, de Souza Dias, Ezeh, Frumkin, Gong, Head, Horton, Mace, Marten, Myers, Nishtar, Osofsky, Pattanayak, Pongsiri, Romanelli, Soucat, Vega and Yach2015). This article is included in the orange cluster, mainly focused on planetary health publications, that is “Limits to growth, planetary boundaries, and planetary health” (Butler, Reference Butler2017), “Planetary Epidemiology: Towards First Principles” (Butler, Reference Butler2018),” “Planetary health: a new science for exceptional actions” (Horton and Lo, Reference Horton and Lo2015), “Human and planetary health: towards a common language” (Demaio and Rockström, Reference Demaio and Rockström2015), “Governance for planetary health and sustainable development” (Clark, Reference Clark2015) and “Connecting planetary health, climate change, and migration” (Schütte et al., Reference Schütte, Gemenne, Zaman, Flahault and Depoux2018).
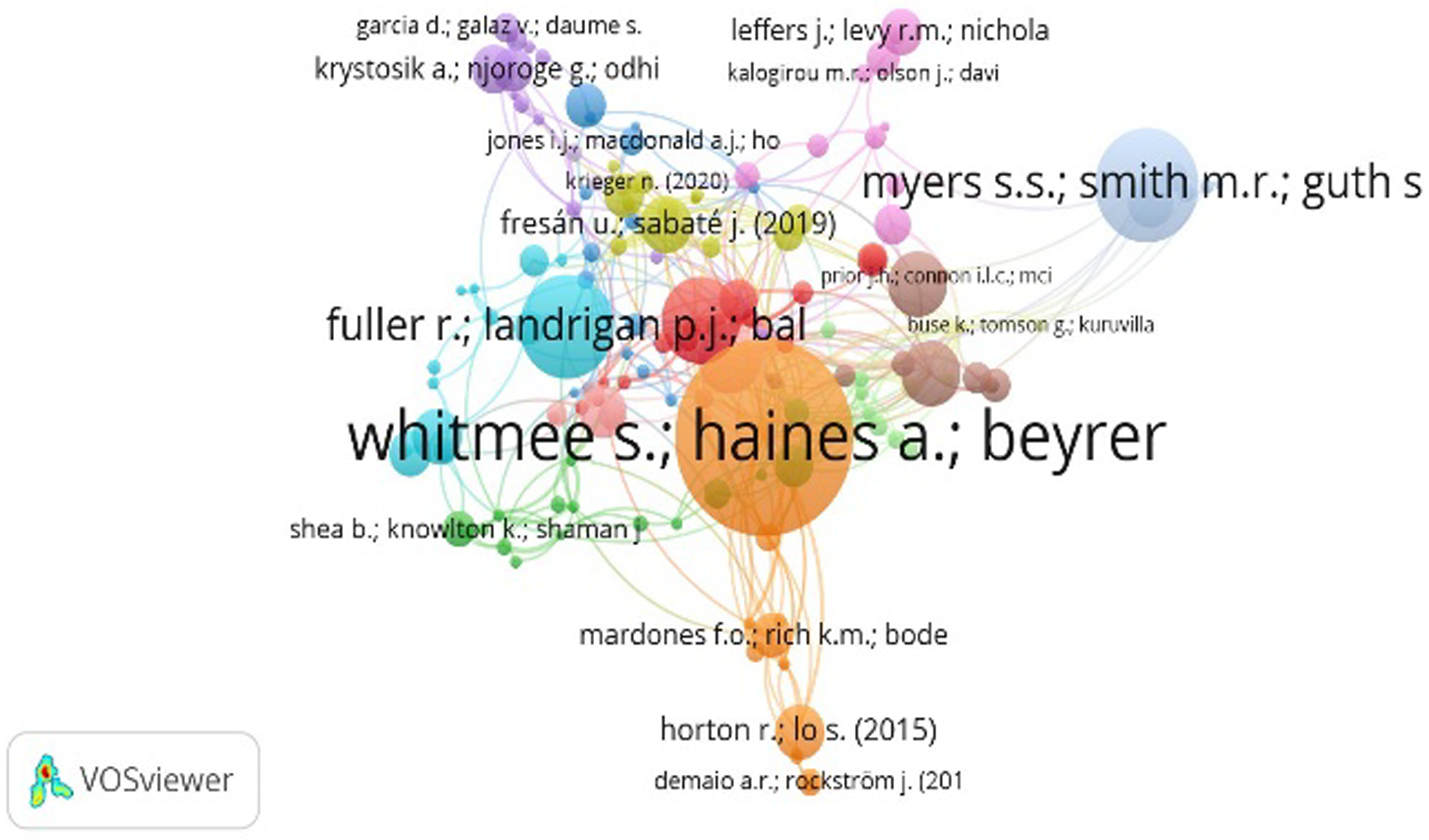
Figure 5. Visualisation of Bibliographic coupling by documents, using VOSviewer.
The second most cited article was “Climate Change and Global Food Systems: Potential Impacts on Food Security and Undernutrition” (Myers et al., Reference Myers, Smith, Guth, Golden, Vaitla, Mueller, Dangour and Huybers2017a), with 491 citations. This publication, along with five others, was a part of the tan cluster, principally directed to environmental issues on a global level, that is “Global environmental and non-communicable diseases risks” (Frumkin and Haines, Reference Frumkin and Haines2019) and “Implementation of policies to protect planetary health” (Pattanayak and Haines, Reference Pattanayak and Haines2017).
The article “Pollution and health: a progress update” (Fuller et al., Reference Fuller, Landrigan, Balakrishnan, Bathan, Bose-O'Reilly, Brauer, Caravanos, Chiles, Cohen, Corra, Cropper, Ferraro, Hanna, Hanrahan, Hu, Hunter, Janata, Kupka, Lanphear, Lichtveld, Martin, Mustapha, Sanchez-Triana, Sandilya, Schaefli, Shaw, Seddon, Suk, Téllez-Rojo and Yan2022), with 408 citations, was included under the cyan cluster. Such a cluster consists of other publications whose key focus was planetary health integrated with sustainable health care/education, that is “Education for the Anthropocene: Planetary health, sustainable health care, and the health workforce” (Barna et al., Reference Barna, Maric, Simons, Kumar and Blankestijn2020), “Opportunities and challenges within urban health and sustainable development” (Fisher et al., Reference Fisher, Andersen, Loft and Pedersen2017), “Envisioning planetary health in every medical curriculum: An international medical student organisation’s perspective” (Omrani et al., Reference Omrani, Dafallah, Paniello Castillo, Amaro, Taneja, Amzil, Sajib and Ezzine2020), “Planetary health and primary care: what’s the emergency?” (Kemple, Reference Kemple2019).
Discussion of the bibliometric analysis
The scientific literature on Planetary Health in the Scopus database increased from 1 in 2013 to 149 in 2022. Indeed, since the early 2000s, health-related concepts like “Planetary Health” or even “One Health” have become popular in the fields of science, politics and medicine (Zschachlitz et al., Reference Zschachlitz, Kümpfel, Niemann and Straff2023).
The four top journals by the number of publications are Lancet Planetary Health (n = 74), followed by the Lancet (n = 23), International Journal of Environmental Research and Public Health (n = 21) and Frontiers in Public Health (n = 15). Many of them are from the 2020 to 22 period. The greater number of publications in the Lancet Planetary Health journal can be possibly explained by its focus on all critical aspects of society and its relationship with the environment, including drivers of change, impacts on people and communities, and practical strategies and interventions for a better planet (About The Lancet Planetary Health, n.d.)
The leading research institutions publishing documents are The London School of Hygiene and Tropical Medicine (n = 27), followed by the University of Washington (n = 19), the Australian National University (n = 16), the Harvard T.H. Chan School of Public Health (n = 15) and University of Melbourne (n = 14).
Regarding the top publishing countries, the United States leads the list (n = 162), followed by the United Kingdom (n = 112), Australia (n = 72), Canada (n = 51) and Germany (n = 46). The above results are in line with those reported by Miao et al. (Reference Miao, Li and Ding2022), cited by Mwatondo et al. (Reference Mwatondo, Shepherd, Hollmann, Chiossi, Maina, Kurup, Hassan, Coates, Khan, Spencer, Mutono, Thumbi, Muturi, Mutunga, Arruda, Akhbari, Ettehad, Ntoumi, Scott, Nel, Ellis-Iversen, Wolff Sönksen, Onyango, Ismail, Simachew, Wolking, Kazwala, Sijali, Bett, Heymann, Kock, Zumla and Dar2023) – a bibliometric analysis of One Health highlights the prominent role of the USA-based authors' publications followed by the UK and Europe. Similarly, a systematic review conducted from 2005 to 2019 found that the United States, United Kingdom, Australia and Canada were among the countries associated with publications on planetary health (Rossa-Roccor et al., Reference Rossa-Roccor, Acheson, Andrade-Rivas, Coombe, Ogura, Super and Hong2020).
By the type of publications, “Articles” lead the list (40%), followed by “Notes” (20%), “Reviews” (18%), “Editorial” (8%) and “Book Chapter” (6%). We thought the low percentage of chapters could be attributable to a low representativity in the Scopus database; however, they are well-represented and accessible (Scopus a, n.d).
The co-authorship by countries shows similarities with the top publishing countries. The USA tops the list (n = 160), followed by the UK (n = 112), Australia (n = 72), Canada (n = 51) and Germany (n = 46). The number of citations follows the same order, except Canada received more than Australia. Regarding One Health research, Mwatondo et al. (Reference Mwatondo, Shepherd, Hollmann, Chiossi, Maina, Kurup, Hassan, Coates, Khan, Spencer, Mutono, Thumbi, Muturi, Mutunga, Arruda, Akhbari, Ettehad, Ntoumi, Scott, Nel, Ellis-Iversen, Wolff Sönksen, Onyango, Ismail, Simachew, Wolking, Kazwala, Sijali, Bett, Heymann, Kock, Zumla and Dar2023) identified the bibliometric analysis from Miao et al. (Reference Miao, Li and Ding2022), who ranked the United States highest regarding the strength of their international, cross-institutional collaboration.
Apropos the co-occurrence analysis based on the author’s keywords, the top five are “climate change”, “planetary health”, “sustainability”, “public health” and “environmental health”. The VOSviewer visualisation finds seven clusters, in decreasing order by the number of items: red (e.g., air pollution, climate change, COVID-19, human health, medical education, planetary health, pollution, sustainable healthcare and urbanisation); green (e.g., biodiversity, ecology, environmental health, food systems, health equity, health promotion, mental health, microbiome and social justice); blue (e.g., adaptation, Anthropocene, ethics, global warming, health, mitigation and well-being); yellow (e.g., carbon footprint, environment, food security, greenhouse gas emission, nutrition, planetary boundaries and sustainability); purple (e.g., global health, governance, One Health, policy, social determinants of health, sustainable development and sustainable development goals); cyan (e.g., public health, infectious diseases and system thinking) and orange (e.g., higher education).
Addressing the Research Directions question
From a health perspective, surveillance should focus on the drivers of disease rather than the disease itself. The drivers should give signals that account for human and animal health and environmental degradation. Some examples are land-use change, international travel and commerce, climate and weather and urbanisation (Drewe et al., Reference Drewe, George and Häsler2023). In this regard, the global climate crisis influences the transmission rates of several vector-borne diseases, mainly in tropical low- and middle-income countries. Besides, in recent years, changes in the timing and magnitude of temperature and rainfall have also accelerated the spread of infectious diseases in northern countries (Leal Filho et al., Reference Leal Filho, Ternova, Parasnis, Kovaleva and Nagy2022).
Notably, two-thirds of all new and emerging infectious diseases are zoonoses (Fong, Reference Fong2017). In contrast, sixty per cent of infectious diseases arise from animal-to-human transmission with global prevalence (Cross et al., Reference Cross, Baldwin, Roy, Essex-Lopresti, Prior and Harmer2019). Zoonotic diseases have become a global crisis beginning around 2010–15, evidenced by the sharp augmentation of publications peaking in 2020, likely due to the COVID-19 outbreak and the increased interest in animal-to-human disease transmission (Leal Filho et al., Reference Leal Filho, Ternova, Parasnis, Kovaleva and Nagy2022).
Effectively preventing and controlling zoonotic diseases requires a One Health approach involving collaboration across sectors responsible for human health, animal health (domestic and wildlife), the environment and other partners (Ghai et al., Reference Ghai, Wallace, Kile, Shoemaker, Vieira, Negron, Shadomy, Sinclair, Goryoka, Salyer and Barton Behravesh2022).
Therefore, warning and response systems for infectious diseases and natural hazards, to account for their drivers (Fernandez de Cordoba, Reference Fernandez de Cordoba Farini2023), should focus on climate- and weather-based observational early warning systems and compound index integrating weather, ecological, human mobility, and animal-to-human, and mainly human-to human transmission rates.
The complementary One Health and Planetary Health scientific approaches have solid leverage for translation into policy and practice (Ruiz de Castañeda et al., Reference Ruiz de Castañeda, Villers, Faerron Guzmán, Eslanloo, de Paula, Machalaba, Zinsstag, Utzinger, Flahault and Bolon2023). Incorporating integrative concepts of both approaches into educating human, animal and environmental health professionals is necessary. Multi-sectoral collaboration should be improved in the future by offering specialised academic degrees (Togami et al., Reference Togami, Gardy, Hansen, Poste, Rizzo, Wilson and Mazet2018), interdisciplinary courses (Chakraborty et al., Reference Chakraborty, Andrade and Smith2022), student clubs (Nguyen et al., Reference Nguyen, Tb, Pham, Tk and Pham2022) and other means. Including these contents early at an undergraduate level and aiming at a diverse cohort of students can be a valuable strategy for building collaboration skills and fostering transdisciplinary thinking (Villanueva-Cabezas et al., Reference Villanueva-Cabezas, Winkel, Campbell, Wiethoelter and Pfeiffer2022).
Many One Health educational efforts were initially designed in response to emerging zoonotic diseases (Stephen, Reference Stephen2022), and the same applies to planetary health in response to global environmental changes (Whitmee et al., Reference Whitmee, Haines, Beyrer, Boltz, Capon, de Souza Dias, Ezeh, Frumkin, Gong, Head, Horton, Mace, Marten, Myers, Nishtar, Osofsky, Pattanayak, Pongsiri, Romanelli, Soucat, Vega and Yach2015). Against this background, Higher Education Institutions should partner with local organisations to foster dialogue and raise awareness about the health impacts of climate change, for example the spread of vector-borne diseases, the effects of air pollution and urban heat on health, and the mental health consequences of extreme weather events (Leal Filho et al., Reference Leal Filho, Aina, Pimenta Dinis, Purcell and Nagy2023), which will allow transcending from knowledge into transdisciplinary action.
Achieving such translation demands a better understanding and integration of climate, environmental, health and social sciences interrelationships. Despite the solid advance in the required knowledge, there is also a need for enhanced communication, comprehension and partnership among public health and environmental health professionals, whether physicians, veterinarians or biologists, with public policy decision-makers to be influential.
Overall summary and conclusion
This review combined qualitative and quantitative analysis sources from an exploration of recent literature on environmental changes affecting human, animal and planetary health up to 2023, a comprehensive search with the help of AI revisiting the concepts of zoonosis and zoonotic diseases, and bibliometric analysis of planetary health from 2012 to 22 focused on the quantitative evaluation of planetary health, human and animal health and climate change.
Then, we analysed the Research Question: How can we improve and facilitate multi-sectoral collaboration in warning and response systems for infectious diseases and natural hazards to account for their drivers, interdependencies and cascading impacts? Our analysis addressed One Health and Planetary Health interactions, warning and surveillance, and capacity building in higher education institutions.
First, the literature review of the environmental changes emphasises the state of the art of heat, extreme weather events and air pollution, summarised in two comprehensive tables and comments on the surveillance system from the One Health and Planetary Health perspectives. The primary outcomes are the following.
Rising atmospheric temperatures harm the health of all plants, animals and people who live on Earth. The rise in temperature and extreme weather events impact vectors, rodents and foodborne pathogens, while numerous vector-borne diseases are experiencing an increase in incidence and geographic distribution.
Floods can elevate the incidence of mosquito-borne diseases due to the proliferation of potential breeding sites and increased humidity, contributing to higher vector survival. On the other hand, drought could increase the risk of certain mosquito-borne diseases by augmenting the number of breeding sites through the proliferation of water storage tanks and other containers near households.
Evidence is that climate change has accelerated the spread of zoonotic infections in the northern hemisphere through its effect on temperature and precipitation.
Rodents are crucial reservoir hosts for zoonotic pathogens such as Leptospira and Hantaviruses. Also, they serve as potential reservoirs for emerging infectious diseases.
Winter heavy rainfall and high temperatures can significantly impact the epidemiology of rodent-borne pathogens by altering the food resources available and, thus, the population size of reservoir species. Floods and droughts can intensify rodent–human interaction because food and habitat shortages can draw rodents near households and buildings and increase the susceptibility of the reservoirs to infections.
Air pollution is the fourth leading cause of human deaths worldwide and affects domestic and wild animals.
Table 2 summarises the environmental challenges to human, animal and planetary health posed by heat, extreme weather events and air pollution, showing the increase in people affected and exposed to extreme heat and other weather events.
The adverse effects of global changes (climate change and land-use change) on animals include modifying their geographical range, interactions and abundance of species and pathogens.
Emerging infectious diseases driven by global changes threaten many endangered species, and rising temperatures affect the health and welfare of food-producing animals.
Table 3 shows that rising temperatures, altered precipitation patterns and increased occurrence of extreme events adversely impact food security. The success of the global increase in food production over the last six decades for public health was only feasible given our planet’s natural resources; therefore, it is detrimental to planetary health.
In the last 50 years, the increased human population has exposed more people living close to wildlife, livestock and pets, increasing the chances for zoonotic diseases to pass between animals and people.
About three quarts of all emerging virus-associated infectious diseases have a zoonotic origin. One Health-inspired environmental surveillance campaign is the preferred tool for monitoring human-adjacent environments for known yet-to-be-discovered infectious diseases. It harbours the potential to prepare humanity for future pandemics caused by aetiological agents with environmental reservoirs.
Surveillance should concentrate on the drivers of disease, giving signals that account for human and animal health and environmental degradation.
Second, the planetary health bibliometric review findings show that it is a growing field attracting increased attention yearly, supported by the 448 documents published from 2012 to 2022, one-third of which were published in 2022.
The London School of Hygiene and Tropical Medicine leads the institutions actively publishing documents on the subject, followed by the University of Washington.
The United States is the leading country for the number of publications, followed by the United Kingdom.
Only 31% of the nations considered for the co-authorship analysis met the criteria of having at least five documents and citations. The United States and the United Kingdom had the highest percentages of published documents.
The co-occurrence analysis of “Author keywords” revealed that only less than 5% of the keywords met the criterion of five as the minimum number of keyword occurrences. The top five terms cited by researchers concerning the connections between planetary health, human health and climate change were “climate change”, “planetary health”, “sustainability”, “public health” and “environmental health”.
The Lancet was the most cited source, followed by The Lancet Planetary Health and the International Journal of Environmental Research and Public Health. When “Documents” were used as the unit of analysis in the bibliographic coupling analysis, with five defined as the minimum number of citations for a document, 50% of the documents met the threshold, creating a map of eleven clusters.
Third, regarding the Research Directions One Health question, we focused on a) improving and facilitating multi-sectoral collaboration in warning and response systems for infectious diseases and natural hazards to account for their drivers and b) integrating global environmental change, One Health and Planetary Health concepts and knowledge in the Higher Education Institutions.
The current global climate and pandemic crises highlight the need for a new paradigm integrating climate, extreme weather, ecosystems, plant, animal and human health approaches, surveillance, response and education.
The evolving and complementary concepts of One Health and Planetary Health address these interrelationships, and since 2020, global environmental changes and challenges have demanded greater unification of these concepts and approaches. However, we must acknowledge that planetary health could be a more complex way for the public health community, which hardly integrates ecology, human medicine and veterinary medicine. Therefore, as usual, education will be the key to such integration in the long term.
Multi-sectoral efforts should focus on surveillance, early warning and response systems watchful of the drivers of infectious diseases, mainly climatic and weather ones with known environmental changes or degradation leading, directly or indirectly, to adverse health effects on plants, animals and the very nature of these drivers is highly diverse. Their effects occur with different delays, only sometimes (if ever) determined. However, the sharp increase in the published literature on Planetary Health and climate change and zoonosis triggered by the COVID-19 pandemic since 2020 will help better understand the complexity of the involved causes, drivers, timing and effects.
As Ruiz de Castañeda et al. (Reference Ruiz de Castañeda, Villers, Faerron Guzmán, Eslanloo, de Paula, Machalaba, Zinsstag, Utzinger, Flahault and Bolon2023) argued: “The complementary One Health and Planetary Health scientific approaches have solid leverage for translation into policy and practice.” Also, as Stephen (Reference Stephen2022) stated, many One Health educational efforts were initially designed in response to emerging zoonotic diseases, while the leading The Rockefeller Foundation–Lancet Commission on Planetary Health report claimed the same in response to global environmental changes. Hence, it is necessary to integrate approaches in the curricula of medicine, veterinary, environmental health and even environmental sciences from the beginning of the studies or through interdisciplinary environmental health courses or degrees, including decision-making areas. By doing this, transdisciplinary systems thinking will permeate students, allowing them to transcend knowledge, research and observation into action.
Data availability statement
The data supporting this study’s findings are available from the corresponding author, [GJN], upon reasonable request.
Acknowledgements
The authors acknowledge the support of the Graduate programme in Environmental Sciences, Faculty of Sciences, University of the Republic, Montevideo, Uruguay.
Author contributions
LT, GN and LV wrote the original draft of the manuscript. GN coordinated the writing team. LT, LV and GN critically reviewed the manuscript. LT conducted the bibliometric analysis. All authors contributed to the revisions.
Financial support
None.
Competing interests
None.
Ethics statement
Ethical approval and consent are not relevant to this article type.















Comments
No accompanying comment.