Background
Socio-economic disadvantage has been linked to increased risk of self-harm and suicide (Cairns, Graham, & Bambra, Reference Cairns, Graham and Bambra2017). Rates of self-harm and suicide are generally higher in areas characterized by greater socio-economic deprivation (SED) relative to areas of lower SED (Cairns et al., Reference Cairns, Graham and Bambra2017; Hawton, Harriss, Hodder, Simkin, & Gunnell, Reference Hawton, Harriss, Hodder, Simkin and Gunnell2001). Individuals who experience economic disadvantage, such as unemployment, low income and unmanageable debt, are also more likely to self-harm or die by suicide relative to their unaffected peers (Coope et al., Reference Coope, Donovan, Wilson, Barnes, Metcalfe, Hollingworth and Gunnell2015).
Little is known about socio-economic disparities in individuals who self-harm and present to hospital. Two recent studies have shown differential risk of suicide after presentation to hospital with self-harm according to level of SED. Data from the Multicenter Study of Self-harm in England showed an elevated risk of suicide following self-harm in individuals from less deprived relative to those from more deprived localities (Geulayov et al., Reference Geulayov, Casey, Bale, Brand, Clements, Farooq and Hawton2019). However, in a study of patients presenting to hospital for self-harm in Northern Ireland, subsequent suicide risk was greater in patients from areas of greater deprivation (O'Neill, Graham, & Ennis, Reference O'Neill, Graham and Ennis2019).
There is also evidence, albeit limited, of socio-economic disparities in the clinical care received by patients who self-harm and present to clinical services. Using data from 684 general practices across the UK (2001–2013), Carr et al. (Reference Carr, Ashcroft, Kontopantelis, While, Awenat, Cooper and Webb2016) found that patients registered at practices in the most deprived areas were 27% less likely to be referred for secondary mental health care than those in the least deprived areas (Carr et al., Reference Carr, Ashcroft, Kontopantelis, While, Awenat, Cooper and Webb2016), a finding which was also seen in adolescents despite the higher incidence of self-harm detected in the more socio-economically deprived practices (Morgan et al., Reference Morgan, Webb, Carr, Kontopantelis, Green, Chew-Graham and Ashcroft2017). A study (Carroll, Knipe, Moran, & Gunnell, Reference Carroll, Knipe, Moran and Gunnell2017) based on a single hospital in Bristol, UK, indicated that among patients who present to hospital for self-harm, psychosocial assessment was more likely to be conducted in patients residing in the least deprived localities relative to those from the most deprived localities, although the receipt of other forms of care was not associated with level of deprivation (Carroll et al., Reference Carroll, Knipe, Moran and Gunnell2017).
Presentation to clinical services following self-harm presents an important opportunity to offer patients help which may improve their prognosis. Understanding how SED influences clinical care in this patient group may contribute to the improvement of in-hospital and follow-up care for this population and inform future policies to reduce the harmful impacts of deprivation. Clinical care may also be an important mediating factor in the associations between socioeconomic disadvantage and health outcomes. However, the extent to which variations in clinical care are related to area-level SED is unclear.
In this study, we used data from the Multicenter Study of self-harm in England (Hawton et al., Reference Hawton, Bergen, Casey, Simkin, Palmer, Cooper and Owens2007) to investigate the associations of area-level SED with hospital management of self-harm, including both in-hospital care and referral for follow-up care.
Methods
Study design and population
We included consecutive presentations following non-fatal self-harm to the emergency department (ED) of five general hospitals, in Oxford (one hospital), Manchester (three hospitals) and Derby (one hospital). These hospitals form the Multicenter Study of Self-harm in England (Hawton et al., Reference Hawton, Bergen, Casey, Simkin, Palmer, Cooper and Owens2007). Information on demographic and clinical characteristics is collected through completion of psychosocial assessments (of the patient's mental state, risks, and needs) by specialist mental health practitioners in the hospitals. For patients who do not receive a psychosocial assessment, less complete data are extracted from emergency department electronic records by trained staff.
The study involved presentations by individuals aged 15 years and over who had attended the study hospitals between 1st January 2000 and 31st December 2016. Persons who had died as a direct result of the self-harm act were excluded.
Of the 115 119 hospital presentations by 61 247 individuals during the study period, we excluded observations of patients who had missing information on gender or age or if they had no valid postcode from which we could derive their area-level deprivation score. The resulting study sample comprised 108 092 hospital presentations by 57 306 patients i.e. 94% of all recorded presentations. In 9659 (8.9%) presentations, patients self-discharged. In 59 959 of 98 433 (60.9%) presentations, patients received a psychosocial assessment. The characteristics of the cohort according to area-level SED are described in detail elsewhere (Geulayov et al., Reference Geulayov, Casey, Bale, Brand, Clements, Farooq and Hawton2022).
Measures
Self-harm is defined as any act of intentional self-poisoning or self-injury, irrespective of motivation (Hawton et al., Reference Hawton, Harriss, Hall, Simkin, Bale and Bond2003; National Institute for Health and Care Excellence, 2022). Self-poisoning includes the intentional ingestion of any drug in an amount that exceeds the prescribed or recommended amount, the ingestion of non-ingestible substances, and overdoses of recreational drugs and severe alcohol intoxication where clinical staff considered these to be acts of intentional self-harm. Self-injury is defined as any intentionally self-inflicted injury.
Socio-economic deprivation
This was based on the English Index of Multiple Deprivation (IMD) (Department for Levelling Up Housing and Communities and Ministry of Housing Communities & Local Government, 2020). IMD is an official measure of deprivation of small geographical areas in England. This combined score is derived from several deprivation domains: income and employment, health and disability, education, skills and training, barriers to housing and services, living environment and crime. There are 32 844 small geographical areas across England which are ranked from 1 (most deprived) to 32 844 (least deprived). Oxford, Manchester and Derby populations are different in terms of deprivation. According to the IMD 2015 (Department for Communities and Local Government, 2015) Manchester was ranked 5th (worst), Derby 55th, and Oxford 166th of 326 local authorities in England. IMD score, which was based on the patient's postal address at a given presentation to hospital, was obtained through data linkage with GeoConvert (http://geoconvert.mimas.ac.uk/help/faq.html). We classified the cohort into five categories based on national IMD quintiles cut-off scores: 1st (least deprived) ⩽ 8.49, 2nd 8.5–13.79, 3rd 13.8–21.35, 4th 21.36–34.17, 5th (most deprived) IMD score ⩾ 34.18 (https://tools.npeu.ox.ac.uk/imd/).
Method of self-harm
The method of self-harm was recorded for all patients. For each hospital presentation, an individual was classified into one of three broad categories: self-poisoning alone, self-injury alone and both self-injury and self-poisoning.
History of self-harm
This was ascertained using three sources of information. In each presentation to hospital, an individual was considered to have had a history of self-harm for that presentation and subsequent presentations if 1. they had a record of a prior hospital presentation in the study (applies to 2nd and subsequent episodes in the study), 2. reported previous self-harm during their psychosocial assessment; or 3. had previously presented to hospital with self-harm based on hospital electronic records (data collectors had access to hospital electronic records).
Psychiatric care
Patients with recorded past or current psychiatric treatment during psychosocial assessment or through the hospital electronic system were assigned a positive status in this and all subsequent presentations to hospital. A negative status was assigned to patients who were identified as having no psychiatric treatment through both their psychosocial assessment and the hospital records. Otherwise this item was recorded as not known.
Outcomes
Indicators of clinical care
Psychosocial assessment status at a given presentation to hospital was defined as an assessment by a mental health professional while patients were in the general hospital. For other forms of assessments (e.g. assessment by emergency department staff) the patient was deemed not assessed. Admission status was defined as an admission to a general hospital bed, including short stay units.
Information about referral to follow-up care was contingent on psychosocial assessment status because patient's aftercare was arranged and recorded by the clinician conducting the psychosocial assessment. For each presentation to hospital, patients were classified into one of three groups (formal referral, advice to self-refer and no referral). These included: transfer to in-patient psychiatric care, referral to outpatient mental health care [including outpatient or day patient psychiatric services or Community Mental Health Team (CMHT)], referral to drug and alcohol dedicated services, referral to the care of a person's general practitioner (GP), referral to all other services (including social services, voluntary agencies, homeless outreach, probation and custody). In all the above, formal referral could be either a new referral or referral back to a currently provided service.
Importantly, most presentations to hospital involved a referral to one form of care e.g. drug and alcohol services or community mental health care or referral back to the GP only. However, some presentations involved a dual referral i.e. a referral back to the GP as well as a referral to some form of specific aftercare (e.g. secondary mental health care, alcohol and drugs services). Referral to one's GP only does not usually constitute referral for specific aftercare. We addressed this in a further analysis (see Analysis section for further information).
Ethical approval
All three study sites have approvals to collect data on self-harm for their local monitoring systems and the Multicenter Study of Self-harm. The three monitoring systems are compliant with the Data Protection Act (1998) and have approval under Section 251 of the National Health Service (NHS) Act (2006) to collect patient-identifiable information without explicit patient consent.
Online Supplementary Table S1 provides a glossary of terms relevant to the UK health service context.
Analysis
We estimated the associations between area-level SED and seven indicators of care: two indicators of in-hospital care, namely psychosocial assessment and admission to a medical bed, and five indicators of follow-up care: transfer to in-patient psychiatric care, referral to outpatient mental health care, alcohol and drug services, and other services (e.g. social work, homelessness outreach care) and referral to the care of the GP. Using the IMD score, presentations were grouped into five groups of SED according to cut-off scores which corresponded to national quintiles (see Measures for details).
We ran seven mixed effect logistic regression models in which episodes of self-harm were nested within individuals to account for dependency between multiple episodes by the same person.
For each outcome, we ran a standard logistic regression model and a mixed effect logistic regression model with presentations nested within individuals. The two models were compared with the Bayesian information criterion (BIC) and Akaike information criterion (AIC) statistics that indicated that the latter fitted the data better. Subsequently, we included ‘Individuals’ as a random effect factor. We further considered adding ‘hospital’ as a random effect factor. We compared two types of multilevel models, one where hospital was included as a fixed effect factor with ‘individuals’ as a random effect factor and another where both ‘hospital’ and ‘individuals’ were included as random effect factors. We chose the former model as the BIC and AIC statistics indicated a better fit.
Some presentations involved a dual referral i.e. a referral back to the GP as well as a referral to some form of aftercare (see Indicators of clinical care above for details). We therefore split this group of presentations into those where the individual was formally referred back to their GP only and presentations where the individual received a referral to back to their GP as well as a referral to some form of aftercare. We combined presentations where the patient was formally referred to their GP only with presentations where the patient received no-referral to any form of aftercare (a ‘no-aftercare’ group of presentations) and compared these to the group of presentations where the patient received formal referral to some form of aftercare (inpatient, outpatient, drug and alcohol services or ‘other’ services). In a final model we compared the chance of receiving some form of aftercare relative to receiving ‘no-aftercare’ (reference category).
Analysis using unadjusted models were followed by models adjusted for gender, age (in years), year of hospital presentation (grouped into three time periods, 2000–2004, 2005–2011, 2012–2016, which coincide with the release of two national guidelines on self-harm management by NICE (National Institute for Health and Care Excellence, 2004; National Institute for Health and Clinical Excellence, 2011), method of self-harm (self-poisoning alone, self-injury alone, combined methods), previous self-harm, receipt of psychiatric care (past or current), time of presenting to hospital (grouped into day time [9am–5pm] and out of hours [5pm–9am]), and time since last presentation to hospital for self-harm. These covariates are assumed to influence the type of care offered to patients and are also likely to be associated with SED.
In a subsequent analysis, models were adjusted for the above covariates and also for hospital to control for hospital variations in care.
We tested for a linear trend in the association between SED and care indicators.
We also examined the associations between SED and self-discharge. The data on presentations to hospital where individuals took their own discharged (8.9% of the presentations) were excluded from further analyses because care outcomes could not be reliably assessed in this group.
We ran a series of sensitivity analyses whereby we excluded observations with missing data (online Supplementary Table S2). We also tested the associations between SED and indicators of care using study derived quintiles to create more balanced groups of SED. We classified the presentations into the following five categories: 1st (least deprived) – IMD score ⩽10.24, 2nd – IMD score >10.24–21.73, 3rd – IMD score >21.73–35.9, 4th – IMD score >35.9–51.94881, 5th (most deprived) – IMD score >51.94881 (online Supplementary Table S3).
In all models, the reference category for care provision following self-harm was ‘no care’ following self-harm. In each model we estimated the odds of receiving care relative to being offered ‘no care’. The reference category for level of deprivation was comprised of presentations to hospital by patients from the least deprived areas (1st SED group of presentations).
The statistical analysis was carried out in Stata 14.2.
Results
Sample characteristics
There were 108 092 presentations (by 57 306 individuals) to hospital following self-harm, with 64 500 (59.7%) presentations being by females. 36 565 (33.8%) presentations were by individuals aged 15–24 years, 26 675 (24.7%) by 25–34 year-olds, 37 648 (34.8%) by 35–54 year-olds, and 7204 (6.7%) were by individual aged 55 years and over at the time of hospital presentation. 8153 (7.5%) of presentations involved individuals from non-White ethnic groups. Information on ethnicity was not available for 14.3% (n = 15 450) of hospital presentations (either because the patient did not disclose it or because the information was not collected). Thirty percent of the presentations (n = 32 484) were by individuals who were unemployed at the time of hospital attendance, 20.5% (n = 22 118) were by employed persons and 11.0% (n = 11 948) by students. In two-thirds of presentations (n = 70 888) the patients had self-harmed previously.
79 301 (73.3%) of presentations were due to self-poisoning alone, while 23 423 (21.7%) were for self-injury alone. In 5368 (5.0%) of presentations the patient had self-poisoned and self-injured in the same episode.
The mean number of presentations to hospital in the study was 1.86 per person (95% CI 1.83–1.90). The number of self-harm presentations per person varied across SED levels from 1.75 (95% CI 1.66–1.84) in the least deprived areas to 1.92 (95% CI 1.87–1.97) in the most deprived areas. In an earlier paper (Geulayov et al., Reference Geulayov, Casey, Bale, Brand, Clements, Farooq and Hawton2022), we have described the characteristics of this cohort in terms of levels of deprivation. We have shown that presentations to hospital from the most socio-economic deprived areas included a higher proportion of males and that self-injury alone was more common in presentations from more deprived areas, while presentations to hospital after self-poisoning with self-injury were more common in less deprived areas. Similarly, presentations to hospital where the patient had self-harmed previously were more common in the two most deprived areas. We have attempted to address these differences within the statistical analyses.
SED and indicators of clinical care
Self-discharge
Individuals self-discharged in 9659 (8.9%) of hospital presentations. Self-discharge following hospital attendance was more likely after presentations to hospital from more deprived localities (3rd SED group: adjusted odds ratio [aOR] 1.13, 95% CI 1.02–1.25, p = 0.02; 4th SED group [2nd most deprived]: aOR 1.25, 95% CI 1.14–1.38, p < 0.0001; 5th SED group [most deprived]: aOR 1.57, 95% CI 1.43–1.73, p < 0.0001) relative to presentations by patients from the least deprived localities (reference group). There was no difference between presentations by patients from the lowest two deprivation groups in terms of self-discharge (2nd least deprived group v. 1st least deprived group [reference category]: aOR 1.03, 95% CI 0.93–1.15, p = 0.6).
After excluding presentations by patients who took their own discharge, the cohort was comprised of 98 433 hospital presentations following self-harm by 53 067 individuals.
In-hospital care
Psychosocial assessment was provided in 60.9% of presentations (Table 1). Psychosocial assessment at a given episode was associated with SED in that the chance of assessment decreased with increased level of deprivation, even after adjustment for the covariates (gender, age, year of hospital attendance, method of self-harm, hour of hospital attendance, previous self-harm, receipt of psychiatric care, and time since last episode) (Table 3). There was evidence of a linear trend (p < 0.0001). After further adjustment for hospital, psychosocial assessment was more likely after presentations by patients living in the least deprived localities relative to presentations by patients living in all other SED areas. There was no evidence of a linear trend (p = 0.49) (Table 3, Fig. 1a).
Table 1. In-hospital clinical management of self-harm in patients who present to hospital with self-harm by level of socio-economic deprivation

Socio-economic deprivation is based on the English Index of Multiple Deprivation (IMD). Number and percent are displayed by episodes, N = 108 092 hospital presentations.

Figure 1. a–b: In-hospital care (a) and follow-up care (b) following hospital attendance for self-harm according to level of socio-economic deprivation (based on IMD score).
*Models are adjusted for gender, age at a given episode, year of hospital presentation, method of self-harm, previous self-harm, psychiatric care, hospital, and time since last hospital attendance for self-harm.
**Other services including social services, voluntary agencies, homeless outreach, probation and custody.
IMD – the English Index of Multiple Deprivation.
Assessment and admission to medical bed (n = 98 433 episodes); inpatient psychiatric care, outpatient psychiatric care, alcohol and drug services, other services, general practitioner (GP) care (n = 59 959 episodes).
Aftercare: referral to any follow-up care v. no referral to follow-up care or referral back to one's GP care only (n = 59 959 episodes).
Less than half of presentations to hospital (48.5%) resulted in admission to a medical bed. Adjusting for all covariates but hospital showed that the chance of being admitted to a bed in the general hospital decreased with increased deprivation. Linear trend (p < 0.0001). Further adjustment for hospital showed that presentations by patients from the least deprived localities were more likely to result in admission to hospital relative to presentations by patients from all other SED localities (Table 3, Fig. 1a). There was no evidence of a linear trend (p = 0.15). However, information about hospital admission was missing in 14.6% of presentations; missing data increased with level of deprivation (this information was missing in 3.4% of presentations from the least deprived localities and increased to 22.6% in presentations from the most deprived localities).
Follow-up care
Referral for follow-up care was contingent on completion of a psychosocial assessment. Therefore, the following analyses include presentations where the patient received an assessment (n = 59 959 presentations by 33 821 patients). Only formal referrals were treated as ‘referrals’. Observations in which patients were advised to self-refer to a service were treated as ‘no-referral’ to a respective service. Presentations where patients were referred to their GP as the only form of care were deemed ‘no referral’ for aftercare (see Methods).
In 8.2% of presentations to hospital, patients were transferred to in-patient psychiatric care (Table 2). Controlling for all confounders, including hospital, presentations by patients from more deprived areas (the three most deprived groups: 3rd to 5th SED groups) were less likely to result in in-patient psychiatric care after attending hospital for self-harm relative to presentations by patients from the least deprived areas (1st SED group – reference group). There was no difference between the two lowest SED groups (2nd and 1st SED groups) in terms of in-patient care (Table 3, Fig. 1b). There was evidence of a linear trend (p < 0.0001).
Table 2. Referral for follow-up care after presentation to hospital for self-harm by level of socio-economic deprivation. Socio-economic deprivation is based on the English Index of Multiple Deprivation (IMD). Number and percent are displayed by episodes
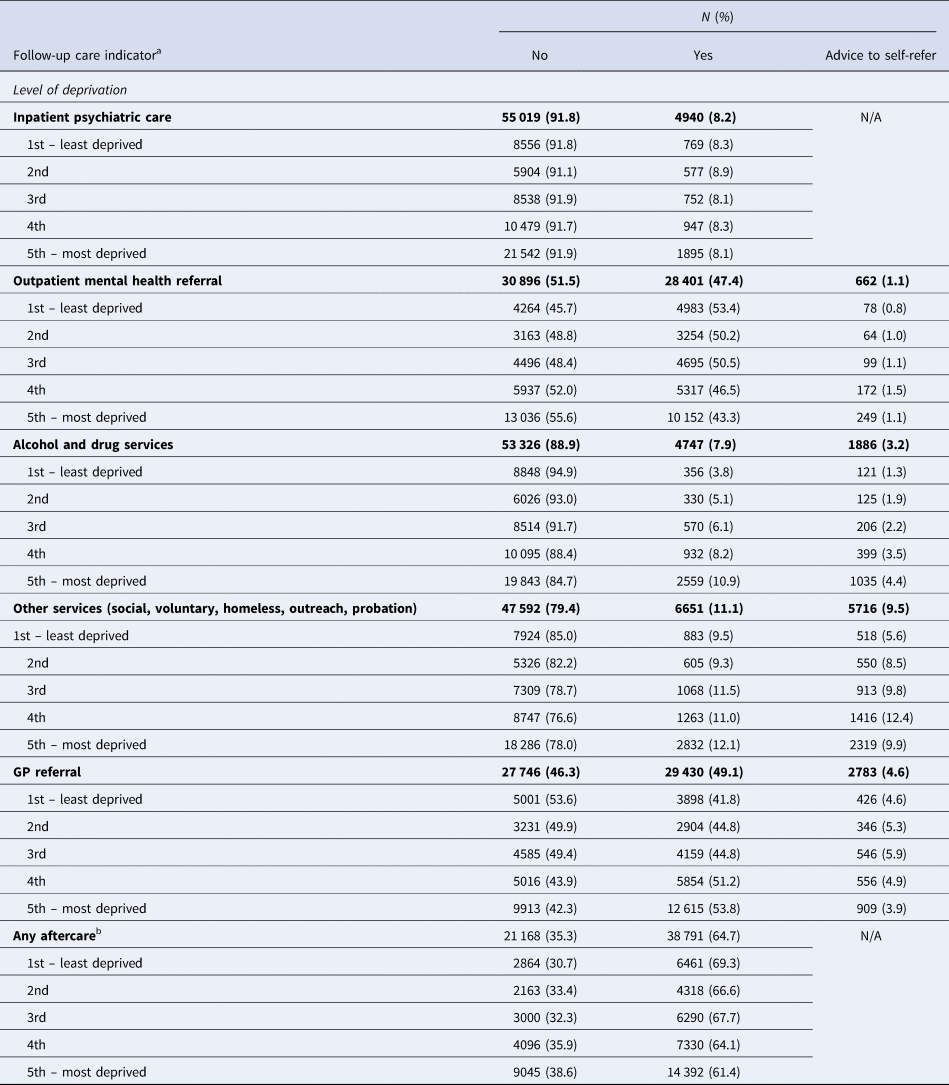
a Includes presentations to hospital where the patients did not self-discharge and where they received psychosocial assessment (N = 59 959 presentations).
b Includes in-patient care, outpatient psychiatric services, alcohol and drug services, and ‘other’ services (i.e. social services, voluntary agencies, homeless outreach, probation and custody) v. no-aftercare or GP care only.
Table 3. The association of socio-economic deprivation with indicators of clinical care for self-harm. Odds ratio and 95% CI

a Adjusted for gender, age at a given episode, year of hospital presentation, previous self-harm, psychiatric care, method of self-harm, time of presentation to hospital, and time since last hospital attendance.
b Adjusted as in (a) and also for hospital.
c Includes presentations where patients did not self-discharge and where they received psychosocial assessment.
d Those advised to self-refer are treated as ‘not referred’.
e Referred for any form of aftercare (inpatient, outpatient, alcohol and drug services, other services) v. no-care or referral back to GP only.
*random effect factor: ID.
**p for linear trend refers to the linear association between IMD quintiles and clinical care receipt.
In 47.4% of presentations, patients were referred for outpatient psychiatric care (Table 2). There was evidence that presentations by patients from the most deprived areas (4th and 5th SED groups) were less likely than presentations by patients from the least deprived areas (1st SED group) to result in referral to outpatient mental health follow-up care (Table 3). There was evidence of a linear trend (p < 0.0001) (Table 3).
In 7.9% of presentations patients were referred for substance dependency (alcohol and drugs) services and in 11.1% of presentations patients were referred to a variety of ‘other’ services including social, voluntary, homeless, outreach, probation (Table 2). Referral to alcohol and drug services and to all ‘other’ services was more common after presentations by patients from more deprived localities. There was evidence of a linear trend (p < 0.0001) (Table 3).
In almost half (48.5%) of presentations, patients were referred to the care of their GP. Presentations by patients from more deprived neighborhoods were more likely than presentations by patients from the least deprived neighborhoods to result in referral to the GP (Table 3).
Finally, we estimated the likelihood that a presentation to hospital would result in referral to some form of aftercare (inpatient, outpatient, drug and alcohol services or ‘other’ services) relative to ‘no-aftercare’. The reference group was comprised of presentations where a patient received no formal referral for aftercare or presentations where the patient was referred back the GP only (this group was collectively termed as ‘no aftercare’). Adjusted analysis showed that referral for any form of follow-up care was less likely after presentations to hospital by patients living in the two most deprived geographical areas (Table 3, Fig. 1b). There was evidence of a linear trend (p < 0.0001).
Having self-harmed before was associated with a higher chance of receiving care. In all adjusted models, presentations to hospital where the patient had previously self-harmed were more likely than presentations where the patient had not self-harmed before to result in provision of care. For example, referral for aftercare (any form of aftercare) was more likely after presentations by patients with a history of self-harm than after presentations by patients without a history of self-harm, controlling for all other covariates (aOR 1.70, 95% CI 1.60–1.81).
To assess the impact of missing data, we re-ran the models excluding presentations to hospital where information on one of the covariates was missing (previous self-harm, psychiatric care, time of presentation to hospital). Finding from models using complete-case analysis were broadly in line with findings from the main analysis except for models assessing the impact of SED on admission to a medical bed where there was no evidence of differences in admission between presentations from the five SED areas after adjusting for all measured confounders (online Supplementary Table S1).
Discussion
We studied socio-economic disparities in clinical care following presentation to general hospitals with self-harm in England over a 17-year period. Area-level SED was associated with indicators of care, both while in hospital for self-harm and in terms of referral for aftercare. Presentations to hospital by patients from more deprived areas were less likely than presentations by patients from less deprived areas to result in both admission to a medical bed and provision of a psychosocial assessment following self-harm. Adjustment for covariates, especially for hospital, was associated with a marked attenuation of these associations. That is, compared to presentations by patients living in the least deprived areas, presentations to hospital from all other areas were less likely to be followed by both admission to the general hospital and assessment after self-harm.
Presentations by patients from the two most deprived areas were less likely than presentations by patients from the least deprived areas to result in referral for follow-up mental health care after psychosocial assessment. However, referral for services such as substance dependency and ‘other’ services (social services, voluntary agencies, homeless outreach, probation and custody) was more likely for presentations by individuals from more deprived localities. Transfer to in-patient psychiatric care was also less common in those from more deprived localities. Overall, a referral for aftercare was less likely for presentations by patients from the two most deprived areas relative to presentations by patients from the least deprived areas.
The present findings are broadly in keeping with results of earlier studies (Carr et al., Reference Carr, Ashcroft, Kontopantelis, While, Awenat, Cooper and Webb2016; Carroll et al., Reference Carroll, Corcoran, Griffin, Perry, Arensman, Gunnell and Metcalfe2016; Morgan et al., Reference Morgan, Webb, Carr, Kontopantelis, Green, Chew-Graham and Ashcroft2017). In an earlier report (Carroll et al., Reference Carroll, Knipe, Moran and Gunnell2017), psychosocial assessment after hospital attendance for self-harm was more likely in patients from the least deprived areas relative to patients from the most deprived localities but this difference was largely explained by differences in level of self-discharge. In our study, however, the association between SED and indicators of care held after excluding presentations to hospitals following which patients took their own discharge. Our study also showed that follow-up care varied across SED groups, a finding which was not supported by Carroll et al.'s (Carroll et al., Reference Carroll, Knipe, Moran and Gunnell2017) data. The latter study, however, was relatively small and limited to a single hospital. Our findings are in line with those of Carr et al., who have shown that patients who were registered at primary care practices in the most deprived areas and had self-harmed were 27% less likely to be referred for secondary mental health care than those in the least deprived areas (Carr et al., Reference Carr, Ashcroft, Kontopantelis, While, Awenat, Cooper and Webb2016), a finding which was documented also in adolescents despite the higher incidence of self-harm detected in adolescents from more socio-economically deprived practices (Morgan et al., Reference Morgan, Webb, Carr, Kontopantelis, Green, Chew-Graham and Ashcroft2017). We further showed that presentations to hospital by patients who lived in the most deprived areas were less likely to result in referral to aftercare (any form of aftercare). That is, presentations by patients from the two most deprived localities were more likely to result in ‘no-referral’ for aftercare or referral to the GP only. Taken together, these data point to reduced healthcare provision for patients who self-harm from more disadvantaged areas. Of note, data from the Improving Access to Psychological Therapies (IAPT) program, a national health services initiative in England designed to increase the availability of psychological treatments in the community, similarly showed that referrals from patients in deprived areas were less likely to receive a course of treatment than referrals in wealthier areas (Hodgson, Reference Hodgson2019).
Interpretation and implications
The reasons for the differences in clinical care provision between levels of deprivation are currently not clear. These differences may be due, at least in part, to pre-existing differences in patients' profile and therefore in treatment needs. It may be that more severe mental health problems were more common in patients who self-harmed and presented to hospital from less deprived areas, while problems related to substance misuse were more common in individuals who presented to hospital for self-harm from more deprived localities. In the general population, socio-economic advantage is inversely related to the risk of mental health problems. Individuals from more advantaged background who develop mental health problems and/or self-harm may be experiencing more severe mental health problems. This may result in them receiving more resource intensive care (as evident in our study showing higher rates of both inpatient and outpatient psychiatric care). There is some evidence, including from the Multicenter Study of Self-harm, that in individuals with pre-existing mental health problems the risk of suicidal behavior is higher for those from more advantaged background relative to those from less advantaged background (Dorner & Mittendorfer-Rutz, Reference Dorner and Mittendorfer-Rutz2017; Geulayov et al., Reference Geulayov, Casey, Bale, Brand, Clements, Farooq and Hawton2019; Martin et al., Reference Martin, McLean, Park, Martin, Connolly, Mercer and Smith2014). Similarly, there is evidence that substance dependency is more common in individuals from disadvantaged backgrounds. However, the association between area-level deprivation and substance use disorders is complex and varies by sociodemographic factors (Karriker-Jaffe, Reference Karriker-Jaffe2011). Our analysis was adjusted for prior and current psychiatric treatment but we did not have information on specific diagnoses or on substance-related disorders. Nevertheless, the finding that presentations by individuals from the most disadvantaged localities were more likely to result in referral to the GPs only or ‘no aftercare’, cannot be readily explained by differences in patients' profiles. It is possible, albeit speculative at present, that patients from more deprived areas are more often viewed as having problems likely to be related to their environmental conditions (e.g. financial, housing) and hence less amenable to available therapeutic interventions. It could also be that some patients may be less receptive to suggestions regarding mental health care (Polling, Woodhead, Harwood, Hotopf, & Hatch, Reference Polling, Woodhead, Harwood, Hotopf and Hatch2021), and/or that institution located in areas of high deprivation may have more limited resources relative to more affluent areas (Buck & Dixson, Reference Buck and Dixson2013). Further work is needed to understand the reasons for these differences.
Presentation to clinical services following self-harm offers an important opportunity for offering patients help which may improve their prognosis. National guidelines such as those of NICE (UK) recommend that all patients who present to hospital following self-harm receive a comprehensive psychosocial assessment (National Institute for Health and Care Excellence, 2004, 2022; National Institute for Health and Clinical Excellence, 2011), which should be followed by a psychological intervention (Hawton et al., Reference Hawton, Witt, Salisbury, Arensman, Gunnell, Hazell and van Heeringen2016; National Institute for Health and Care Excellence, 2004; National Institute for Health and Clinical Excellence, 2011). However, our data show that in 39% of instances such assessment did not take place and that less than 50% of presentations which resulted in an assessment were followed by referral for mental health follow-up care. This means that just over a quarter of presentations to hospital for self-harm resulted in referral for mental health follow-up care. Given that most patients who self-harm have significant mental health problems (Hawton, Saunders, Topiwala, & Haw, Reference Hawton, Saunders, Topiwala and Haw2013), it is imperative that as many patients as possible are assessed and offered mental health follow-up care, regardless of other problems such as substance misuse, which may require problem-specific adjunct service. Moreover, we found evidence for differential referral for aftercare, so this problem may be further exacerbated in the most deprived populations. However, the real number of patients who receive follow-up care may be even lower due to other barriers e.g. busy services and long waiting times, so in reality a small fraction of patients who could benefit from care may actually receive the recommended psychological interventions.
More equitable care for individuals who self-harm may require a multilevel approach including at the national and local levels to achieve a better balance in the distribution and availability of services. It is also important to ensure that healthcare services are compatible with the needs of diverse populations as well as to better understand patients' perspective and experience of services to minimize disengagement and mistrust. It is equally important to tackle the factors that contribute to the development of poor mental health and which are more prevalent in individuals from more disadvantaged areas.
Some notable national and global events, such as the publication of the NICE self-harm guidance (published in 2004, 2011) and the economic crisis (which commenced in 2008), have taken place during the study period. Such events may have influenced the associations between SED and provision of care. We attempted to address this by adjusting our analysis for the year of hospital presentation. However, further work could examine the temporal changes in the relationship between SED and provision of care to better understand the possible impact of such events.
Strengths and limitations
The Multicenter Study of Self-harm is a large study of more than 100 000 presentations to hospitals in England involving socio-economically diverse populations, including some of the most socioeconomically deprived populations in England (Geulayov et al., Reference Geulayov, Casey, Bale, Brand, Clements, Farooq and Hawton2022).
However, our indicator of SED is an area-level indicator which does not address individual-level socioeconomic position, nor the interaction between these. Some studies have highlighted the importance of considering area-level measures and their interaction with individual characteristics to better understand the epidemiology of self-harm (Hawton et al., Reference Hawton, Harriss, Hodder, Simkin and Gunnell2001; Martin et al., Reference Martin, McLean, Park, Martin, Connolly, Mercer and Smith2014; Neeleman & Wessely, Reference Neeleman and Wessely1999). Further work should explore the interaction between area-level SED and characteristics such as ethnicity, employment status, financial strain, mental health and substance use disorders in influencing receipt of clinical care in patients who self-harm.
Within the multicenter study, referral to follow-up care entails either a new referral or referral back to a currently provided service. We were unable to separate the two forms of referrals in our analysis. Furthermore, our study focused on broad categories of aftercare. It did not allow investigating specific types of interventions, such as those for patients with dual diagnoses or other complex problems.
In this study, we record referral for follow-up care, which may or may not be followed by actual receipt of care. Differential service uptake may be influenced by further factors such as long waiting times, variations in engagement with services. Such information is not available within this study. Furthermore, we are not able to record information on the aftercare received, if any, among non-assessed patients.
Additionally, our fully adjusted models included hospital as a covariate which led to a marked attenuation of the associations. There is likely to be a significant overlap between area-level measures of deprivation (the exposure) and the regional effect and the characteristics of hospitals in these regions. By controlling for hospital, we may be underestimating the impact of socio-economic differences on inequality in care provision. However, the relationship between hospital characteristics and practices and measures of deprivation is complex and may be difficult to separate. Furthermore, while adjustment for hospital gives an indication of the impact of hospital as a confounder, it cannot explain which hospital characteristics are driving the differences. Hospitals may have differed in uptake and adherence to NICE guidance on management of self-harm, and varied in staffing levels, and local availability of aftercare services. Unfortunately, we do not have detailed information about hospital characteristics and practices.
There were some differences in the distribution of patients' characteristics across levels of SED, including by gender, method of self-harm, the number of self-harm presentations to hospital and the proportion of presentations where the patient had self-harmed previously. A detailed account of the cohort can be found in an earlier publication (Geulayov et al., Reference Geulayov, Casey, Bale, Brand, Clements, Farooq and Hawton2022). We attempted address this by adjusting our analyses for these and other potential confounders but some residual confounding may have remained.
Finally, we derived SED groups which correspond to national levels of deprivation. Using this approach facilitated interpretation, generalizability and understanding of the implications for practice and policy. However, since our sample was skewed towards the more deprived, we conducted a further sensitivity analysis in which we used study derived quintiles to create more balanced SED groups. The findings from these two analytic approaches appeared to vary to some extent. However, the conclusions remained similar. That is, there was evidence of reduced provision of secondary mental health care following presentations to hospital for self-harm from more deprived localities. In contrast, provision of other forms of care (drug and alcohol dedicated services and all ‘other’ services) was more common for presentations to hospital from more deprived localities. Nevertheless, there was no evidence that presentations to hospital from the two most deprived areas (4th and 5th quintiles) relative to presentation from the least deprived areas (1st quintile) resulted in reduced provision of psychosocial assessment after self-harm.
Conclusion
Admission to a medical bed and psychosocial assessment were more likely after presentations to hospital by patients living in the least deprived localities. Hospital presentations by patients from all other localities were equally likely to result in admission to hospital and psychosocial assessment. Presentations to hospital by patients from the most socio-economically disadvantaged areas were less likely to result in referral for follow-up mental health care but more likely to be followed by a referral to other services such as alcohol and drug dependency services, social and outreach services. Overall, presentations by patients from areas deemed most deprived were less likely to be followed by a referral for aftercare relative to presentations by patients from less deprived areas. Clinical care may be an important factor in the association between socioeconomic disadvantage and health outcomes. Research is needed to better understand the reasons for these inequalities. Reducing disparities in care for patients who self-harm may require a holistic approach involving national and local policies and better understanding of the service user needs and barriers to care.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291723002799
Acknowledgements
We thank the clinicians and the research staff in all three research centers for their support with the data collection.
Funding statement
The Multicenter Study of Self-harm in England is funded by the UK Department of Health and Social Care. KH is supported by Oxford Health NHS Foundation Trust.
Role of the funding source
The Department of Health and Social care had no role in study design, data collection, analysis, and interpretation of data, or in the writing of the report, and in the decision to submit the paper for publication.
Authors’ contributions
GG and KH were responsible for study conception and design, and interpretation of the results. GG was responsible for data analysis. SW provided statistical support. DC, LB, FB, NK, CC, BF, JN, AP, and KW acquired the data. GG drafted the report, which all authors critically revised for intellectual content. All authors approved the final report and are accountable for all aspects of this work.
Competing interests
KH declare grants from the National Institute for Health Research and the Department of Health and Social Care. He is a member of the National Suicide Prevention Strategy for England Advisory Group and is a National Institute for Health Research (NIHR) Senior Investigator (Emeritus).
NK is a member of the Department of Health's National Suicide Prevention Advisory Group. NK chaired the NICE guideline development group for the longer-term management of self-harm and is currently Topic Advisor for the new NICE self-harm guideline. He also chairs the NICE guideline committee for depression in adults.
All other authors declare no competing interests.
The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care.







