Introduction
Schizophrenia is known to have a strong genetic background, with a heritability of ca. 80% (Sullivan, Kendler, & Neale, Reference Sullivan, Kendler and Neale2003) and a strong familial risk (Mäki et al., Reference Mäki, Veijola, Jones, Murray, Koponen, Tienari and Isohanni2005). A current prevailing approach to estimate genetic risk for schizophrenia is to calculate polygenic risk scores on the basis of genome-wide association studies (GWAS), including a weighted set of the single nucleotide polymorphisms (SNP, a difference in a single DNA nucleotide) associated with schizophrenia. Recently identified polygenic risk scores for schizophrenia have typically ca. 7–8% of the variation in liability to schizophrenia (Legge et al., Reference Legge, Santoro, Periyasamy, Okewole, Arsalan and Kowalec2021).
A great body of evidence has shown that patients with psychotic disorders have impairments in their social life in terms of, for example, lower social support (Gayer-Anderson & Morgan, Reference Gayer-Anderson and Morgan2013), challenges in creating romantic relationships and an increased risk for divorce (Walid & Zaytseva, Reference Walid and Zaytseva2011), and narrow networks including on average three friends (Palumbo, Volpe, Matanov, Priebe, & Giacco, Reference Palumbo, Volpe, Matanov, Priebe and Giacco2015). Also, evidence in clinical high-risk samples has shown that social impairments are evident already before psychosis (Addington, Penn, Woods, Addington, & Perkins, Reference Addington, Penn, Woods, Addington and Perkins2008; Ballon, Kaur, Marks, & Cadenhead, Reference Ballon, Kaur, Marks and Cadenhead2007; Gayer-Anderson & Morgan, Reference Gayer-Anderson and Morgan2013) and increase risk for conversion to psychosis (Addington et al., Reference Addington, Liu, Perkins, Carrion, Keefe and Woods2017; Cannon et al., Reference Cannon, Cadenhead, Cornblatt, Woods, Addington, Walker and Heinssen2008).
Despite the obvious association between social impairments and psychosis, it has remained unclear to which extent some social impairments might reflect genetical liabilities, not necessarily preceding or resulting from a psychosis. That is, whether certain ‘deviances’ in social development might rather reflect ‘normative development’ in individuals with a genetic liability to psychosis, and might be evident also individuals who have not converted and will not convert to psychosis. To date, polygenic risk for schizophrenia is found to predict lower prosocial tendencies in childhood and adolescence (Schlag et al., Reference Schlag, Allegrini, Buitelaar, Verhoef, van Donkelaar, Plomin and St Pourcain2022) and impaired facial emotion recognition in adulthood (Germine et al., Reference Germine, Robinson, Smoller, Calkins, Moore, Hakonarson and Gur2016; Tripoli et al., Reference Tripoli, Quattrone, Ferraro, Gayer-Anderson, La Cascia, La Barbera and Murray2022). Those studies have not, however, differentiated between those converted v. not converted into psychosis.
The current study focused on individuals who have not developed a psychosis until middle age. We first investigated whether a polygenic risk for schizophrenia (PRSSCZ) predicts (a) different trajectories of perceived support and sociability from adolescence to adulthood and (b) differences in family structure (age in first-time parenthood, number of children, or partnership status) in adulthood. Second, we investigated whether possible associations between PRSSCZ and social trajectories are specific to PRSSCZ or whether similar associations can be obtained for polygenic risk for major depression. Polygenic risk for major depression could be a relevant comparison since major depression and schizophrenia have partly overlapping genetic liabilities (Schulze et al., Reference Schulze, Akula, Breuer, Steele, Nalls, Singleton and McMahon2014) and both represent common mental disorders in the population. We used the population-based Young Finns data with a 24-year prospective follow-up of social trajectories (participants being 12–49-year-olds during the follow-up). The data provided possibilities for taking into consideration a variety of potential confounders such as early family environment and adulthood socioeconomic factors.
Methods
Participants
The Young Finns Study (YFS) is an on-going prospective follow-up study that has begun in 1980 (baseline assessment), and follow-ups have been conducted in 1983, 1986, 1989, 1992, 1997, 2001, 2007, 2012, and 2017. Altogether 4320 subjects were invited (born in 1962, 1965, 1968, 1971, 1974, or 1977), and 3596 of them participated in the baseline study. The sampling was designed to include a population-based sample of non-institutionalized Finnish children, representative with regard to most crucial sociodemographic factors. In practice, the sampling was conducted in collaboration of five Finnish universities with medical schools (i.e. Universities of Helsinki, Turku, Tampere, Oulu, and Kuopio). A more detailed description of the YFS can be found elsewhere (20).
The study design has been approved by the ethical committees of all the Finnish universities conducting the study. All the participants or their parents (participants aged < 18 years) provided informed consent before participation. The Declaration of Helsinki has been followed throughout the study.
The design of the present study is illustrated in Fig. 1. Of the 3596 participants, we first excluded participants who had not been genotyped (n = 1153), who had been diagnosed with non-affective psychotic disorders (n = 37), or who had not reported family structure (number of children, age in first-time parenthood, and partnership status) or perceived social support and sociability in any measurement year (n = 29). Accordingly, altogether 2377 participants were included in the analyses of the present study. The number of observations per participant per longitudinal outcome is shown in online Supplementary Table S1.

Figure 1. An illustration of the measurement years and participants' age at each follow-up wave.
Measures
Polygenic risk score for schizophrenia (PRSSCZ)
Polygenic risk score for schizophrenia was calculated on the basis of the summary statistics of the most recent genome-wide association study (GWAS) on schizophrenia that was conducted by Schizophrenia Working Group of the Psychiatric Genomics Consortium et al., and published in Nature (Consortium, 2014). Specifically, a weighted polygenic risk score (Igo, Kinzy, & Cooke Bailey, Reference Igo, Kinzy and Cooke Bailey2019) for every study subject was created by summing up each participant's schizophrenia-associated risk alleles weighted by risk allele beta estimates (Consortium, 2014). Altogether 128 independent SNPs (single nucleotide polymorphisms) reaching genome-wide significance in the schizophrenia GWAS were included in the PRS. More specifically, genotyping was done for 2556 samples using custom build Illumina Human 670k BeadChip at Welcome Trust Sanger Institute. Sample call rate < 0.95, excess heterozygosity, sex mismatch, cryptic relatedness (pi-hat > 0.2), SNP call rate < 0.95, minor allele frequency (MAF) < 0.01, and Hardy–Weinberg Equilibrium (HWE) p value < 1 × 10−6 were used as quality control filters. After the quality control, there were 2443 samples and 546 677 genotyped SNPs available for further analysis. Genotype Imputation to 1000 Genomes reference was performed using the following pre-phasing tools: SHAPEIT v1 for haplotype phasing and IMPUTE2 and 1000 Genomes March 2012 haplotypes for genotype imputation. SNPs with imputation information metric > 0.3 were considered as well-imputed. This polygenic risk score for schizophrenia is shown to predict an increased likelihood of psychoses (Saarinen et al., Reference Saarinen, Lyytikäinen, Hietala, Dobewall, Lavonius, Raitakari and Keltikangas-Järvinen2022). The calculation of the polygenic risk score for major depression is described in the Supplementary Material.
Outcomes of social development
Perceived social support was assessed in 1989, 1992, 1997, 2001, and 2007 (participants being 12–45 years) with the Multidimensional Scale of Perceived Social Support (MSPSS) (Zimet, Dahlem, Zimet, & Farley, Reference Zimet, Dahlem, Zimet and Farley1988). The scale measures perceived social support from friends (4 items), family (4 items), and a significant other (4 items). The items (e.g. ‘My friends always help me, when I need help’) are rated on a 5-point Likert-scale (1 = totally disagree, 5 = totally agree). For each measurement year, we calculated a total score of perceived social support from friends, family, and a significant other. The internal consistency for the scale was high (Cronbach's α = 0.92‒0.95 in 1989‒2007). The MSPSS is found to be a valid and reliable measure of perceived social support (Hardan-Khalil & Mayo, Reference Hardan-Khalil and Mayo2015; Rajabi & Hashemi-Shabani, Reference Rajabi and Hashemi-Shabani2011).
Perceived sociability was measured in 1992, 1997, 2001, 2007, and 2012 (participants being 15–50 years) with the Sociability scale of the Emotionality, Activity, and Sociability Temperament Survey (EAS) (Buss & Plomin, Reference Buss and Plomin1975, Reference Buss, Plomin and Plomin1986). The scale includes five items (e.g. ‘I like to be with people’; ‘I engage in social interactions whenever possible’; ‘I would feel melancholic if I could not form many acquaintances’ [reversed]) that are responded with a 5-point scale (1 = totally disagree, 5 = totally agree). The scale assesses a tendency to prefer and enjoy the presence of others over being alone, and a tendency to feel comfortable in a group. The scale had adequate internal reliability (Cronbach's alpha = 0.78‒0.80 in 1992‒2012). The factor structure of the scale is shown in online Supplementary Fig. S1 (results of an non-rotated exploratory factor analysis), indicating a one-factor structure and providing support for the structural validity of the scale.
Partnership status was assessed in 2001, 2007, and 2011 (participants being 24‒49 years old) with a questionnaire asking whether a participant was unmarried (single), married, engaged, living in cohabitation, divorced, or a widow. We formed a dichotomous variable displaying whether a participant had been in a partnership at least once during the follow-up (value 1) or not (value 0). Number of children was assessed with an open response format. Age of first-time parenthood was calculated on the basis of participant's birth year and first child's birth year. In case a participant had not reported his/her number of children or his/her first child's birth year in 2011, we used the reports in 2007/2001.
Psychiatric diagnoses
In the present study, we excluded participants diagnosed with non-affective psychoses. Participants' psychiatric diagnoses over their lifespan were collected up to 2017 (when participants were 40–55 years old) from the Care Register for Health Care (https://thl.fi/en/web/thlfi-en/statistics-and-data/data-and-services/register-descriptions/care-register-for-health-care). The register covers all psychiatric disorders that have required hospital care in Finland. Regarding psychotic disorders, the register is estimated to cover ca. 97% of psychotic cases (Sund, Reference Sund2012). Diagnoses were given in accordance with the diagnostic classification at that time (ICD-8, ICD-9, or ICD-10). The conversion of ICD-diagnoses to DSM-IV diagnoses has been described elsewhere (Sormunen et al., Reference Sormunen, Saarinen, Salokangas, Telama, Hutri-Kähönen, Tammelin and Hietala2017). Non-affective psychoses included the diagnoses of DSM-IV 295 and 297–298. The register has been used also in previous research (Suvisaari, Haukka, Tanskanen, & Lönnqvist, Reference Suvisaari, Haukka, Tanskanen and Lönnqvist1999).
Covariates
Covariates included age, sex, participants' (2011) and their parents' (1980) socioeconomic factors (educational level, annual income), qualities of early family environment (stressful life events and emotional family atmosphere in 1980/1983), and a polygenic risk score for major depressive disorder (PRSDEP). A more detailed description of the covariates is available in Supplementary Material.
Statistical analyses
In all the analyses, participants diagnosed with non-affective psychotic disorders were excluded.
We used growth curve models (with maximum likelihood estimation) to examine whether polygenic risk for schizophrenia (PRSSCZ) predicts trajectories of (a) perceived support from family, (b) perceived support from friends, (c) perceived support from a significant other, and (d) perceived sociability. We estimated separate curves for each outcome over the follow-up. The follow-ups ranged from 1989 to 2007 for perceived social support (participants being 12–45 years) and from 1992 to 2012 for perceived sociability (participants being 15–50 years). The scores of perceived social support and sociability were standardized with the mean and s.d. of the first measurement year (1992 for perceived sociability, 1989 for perceived social support) to stabilize the scales of the growth curves. PRSSCZ was set as a predictor variable (i.e. included in the fixed effects). The growth curve models were run with different blocks of covariates (included in the fixed effects). Model 1 was adjusted for age and sex; Model 2 also for qualities of early family environment (parents' socioeconomic factors, early emotional family atmosphere and stressful life events); and Model 3 also for participants' socioeconomic factors in adulthood (educational level, annual income). Also, as the effects of age2 and age3 were significant when predicting perceived social support (p < 0.001 for age2 and age3) or perceived sociability (p < 0.001 for age2 and p = 0.036 for age3), those effects were included in the growth curve models. Random effects included variance of intercept and residual variance. As the PRS*sex interaction was non-significant when predicting the growth curves, we ran the analyses simultaneously for both sexes.
Next, we used linear regression models to predict age in first-time parenthood (approximately normally distributed variable), Poisson regression models to predict number of children (continuous and slightly skewed responses), and logistic regression models to predict the likelihood of being in a partnership (0 = not in a partnership, 1 = in a partnership) over the follow-up. PRSSCZ was set as the predictor. Covariates were similar to those in the growth curve models.
Then, we examined whether possible associations with social outcomes are specific to PRSSCZ or whether the associations between PRSSCZ and social domains can be obtained independently of PRS for major depression (PRSDEP). For this purpose, we reran the analyses so that PRSSCZ AND PRSDEP were included as predictors simultaneously.
Finally, we investigated possible bias in participant drop-out over the follow-up. That is, we compared included and dropped-out participants with regard to study variables using independent samples t tests and chi-square tests.
Results
Descriptive statistics of the sample are shown in Table 1. First, we examined attrition over the follow-up: whether included and dropped-out participants differed with regard to the study variables (for details, see online Supplementary Table S2). In summary, we did not find any attrition bias in PRSSCZ, PRSDEP, number of children, perceived sociability, or socioeconomic factors in adulthood. Included participants had, however, slightly higher age in first-child parenthood (28.1 v. 27.5 years, p < 0.05), higher likelihood of being in partnership (86.0% v. 72.5%, p < 0.001), and slightly higher perceived social support (p < 0.001). Also, females were more likely to participate in the follow-ups than male (54.6% v. 43.9%).
Table 1. Descriptive statistics of the sample

This table includes participants who were included in at least one analysis.
Table 2 shows the results of growth curve models. As can be seen in Table 2a, high PRSSCZ predicted lower trajectories of perceived support from friends (B = −0.035–0.040, p = 0.009–0.035 in Models 1–3), perceived support from family (B = −0.035–0.040, p = 0.009–0.035) but not perceived support from a close friend. Additionally, high PRSSCZ predicted lower perceived sociability (B = −0.045–0.048, p = 0.010–0.026) in all the models. These associations sustained after adjusting for different sets of potential confounders: age, sex, early family environment (parents' socioeconomic factors, and early emotional family atmosphere and stressful life events), and socioeconomic factors in adulthood (Models 1–3).
Table 2. Results of growth curve models

Estimates (B) with standard errors (s.e.) of PRS for schizophrenia and PRS for major depression, when predicting standardized scores of perceived social support and sociability from adolescence to middle age. Statistically significant associations are bolded.
Model 1 (n = 2281) was adjusted for age and sex.
Model 2 (n = 2148) was adjusted for age, sex, parents' socioeconomic factors, and stressful life events and emotional atmosphere.
Model 3 (n = 1515) was adjusted for age, sex, parents' socioeconomic factors, and stressful life events and emotional atmosphere, and participants' annual income and educational level in adulthood.
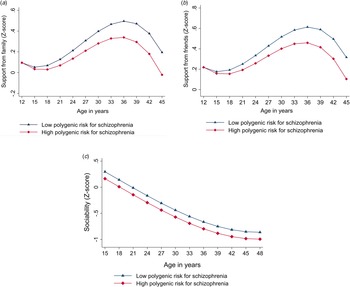
Also, we found a significant interaction effect of age*PRSSCZ when predicting perceived support from family (p = 0.042) and friends (p = 0.042) but not when predicting perceived support from a close friend (p = 0.472) or perceived sociability (p = 0.904). This indicated that age modified the association of PRSSCZ with perceived support from family and friends but did not modify the association between PRSSCZ and perceived support from a close friend or sociability. The findings are illustrated in Fig. 2. In the figure, we included the significant age*PRSSCZ effects. Taken together, participants with high (v. low) PRSSCZ seemed to perceive lower support from family and friends especially in middle age, ca. 30–50 years of age, but not in teenage years or early adulthood. In sociability, the difference between high v. low PRSSCZ appeared to be similarly evident from adolescence to middle age.

Figure 2. Model-predicted values of (a) perceived support from family, (b) perceived support from friends, and (c) perceived sociability separately for subjects with low (−1 s.d.) or high (+1 s.d.) polygenic risk for schizophrenia. Adjusted for age and sex.
Next, we reran the analyses so that both PRSSCZ and PRSDEP were included as predictors. Table 2b shows the results. In summary, the associations between PRSSCZ and social development remained. Further, when including both PRSSCZ and PRSDEP as predictors simultaneously, PRSDEP did not have any main effect on the trajectory of any outcome variable: perceived support from friends (p = 0.680–0.791 in Models 1–3), perceived support from family (p = 0.680–0.791), perceived support from a close friend (p = 0.239–0.798), or perceived sociability (p = 0.192–0.939). Also, PRSDEP did not have any main effect on social support or sociability when PRSSCZ was not included as predictors (online Supplementary Table S3).
Table 3 presents the results of regression analyses. As can be seen in Table 3a, PRSSCZ did not predict age in first-time parenthood (p = 0.617–0.964 in Models 1–3), number of children (p = 0.834–0.963), or likelihood of being in partnership (p = 0.284–0.867). Further, when including both PRSSCZ and PRSDEP as predictors, all the associations remained non-significant (see Table 3b). Also, PRSDEP did not have any main effect on any outcome when PRSSCZ was not included as predictors (online Supplementary Table S4).
Table 3. Results of regression analyses

Estimates (B) with standard errors (s.e.) of PRS for schizophrenia, when predicting age at becoming a parent, number of children, and marital status in adulthood.
Model 1 (n = 1795) was adjusted for age and sex.
Model 2 (n = 1684) was adjusted for age, sex, parents' socioeconomic factors, and stressful life events and emotional atmosphere.
Model 3 (n = 1228) was adjusted for age, sex, parents' socioeconomic factors, and stressful life events and emotional atmosphere, and participants' annual income and educational level in adulthood.
Discussion
The present study investigated whether polygenic risk for schizophrenia (PRSSCZ) predicts social trajectories in individuals without manifest psychosis until middle age. We found that high PRSSCZ predicted lower perceived support from friends and family and lower perceived sociability. PRSSCZ did not predict participants' adulthood family structure as measured by age in first-time parenthood, number of children, or partnership status. Thus, individuals with high PRSSCZ appeared to have an intact adulthood family structure but they experienced lower support (than those with low PRSSCZ). The associations of PRSSCZ with social trajectories were evident independently of PRSDEP (i.e. evident after controlling for PRSDEP). This suggests that the observed social trajectories may be preferentially related to schizophrenia-related genetic liabilities although many vulnerability gene loci are shared by non-affective psychoses and affective disorders.
Our study focused on participants without manifest psychosis until middle age (until age of 40–55 years). As the onset of schizophrenia typically occurs in early adulthood (at the age of ca. 24–28 years) and late-onset psychoses are very rare with prevalence of 0.1% (Chen, Selvendra, Stewart, & Castle, Reference Chen, Selvendra, Stewart and Castle2018; Copeland et al., Reference Copeland, Dewey, Scott, Gilmore, Larkin, Cleave and McKibbin1998; Häfner, Hambrecht, Löffler, Munk-Jørgensen, & Riecher-Rössler, Reference Häfner, Hambrecht, Löffler, Munk-Jørgensen and Riecher-Rössler1998; Ochoa, Usall, Cobo, Labad, & Kulkarni, Reference Ochoa, Usall, Cobo, Labad and Kulkarni2012), our participants are unlikely to convert to psychosis in their later life but rather display a long-term and mostly stable vulnerability for psychosis. Taking this into consideration, our study showed that individuals with high PRSSCZ who have not converted to psychosis have different social trajectories, especially after early adulthood and in middle age. This age period differs from individuals with prodromal psychoses or ultra-high risk for psychosis: on average they are shown to have most evident cognitive and social impairments in early adolescence and early adulthood (Velthorst et al., Reference Velthorst, Fett, Reichenberg, Perlman, van Os, Bromet and Kotov2017). Taken together, among those not converted to psychosis in a typical age period, high PRSSCZ may predict a ‘later risk phase’ and reduced functional resilience when approaching middle age.
A possible interpretation of our results is that PRSSCZ may modify one's perceptions of social support (not necessarily objectively measured social support). In our study, high PRSSCZ was not related to a narrower family structure (lower number of children or lower likelihood of being in a partnership). Nevertheless, individuals with high PRSSCZ experienced lower social support from their family. Thus, our findings indicate that individuals with high PRSSCZ may have an impaired ability to experience available support around them or to form close emotional relationships with their family members. This is in accordance with previous studies in clinical high-risk samples, demonstrating that individuals at clinical risk for psychosis have a stronger bias to perceive hostility and blame for others (An et al., Reference An, Kang, Park, Kim, Lee and Lee2010), impaired theory of mind and less accurate recognition of negative facial expressions and (Piskulic et al., Reference Piskulic, Liu, Cadenhead, Cannon, Cornblatt, McGlashan and Addington2016; Thompson, Bartholomeusz, & Yung, Reference Thompson, Bartholomeusz and Yung2011), lower awareness of social inferences (Glenthøj et al., Reference Glenthøj, Fagerlund, Hjorthøj, Jepsen, Bak, Kristensen and Nordentoft2016), and increased prevalence (12%) of autism spectrum traits (Vaquerizo-Serrano, Salazar de Pablo, Singh, & Santosh, Reference Vaquerizo-Serrano, Salazar de Pablo, Singh and Santosh2022).
Patients with psychotic disorders are known to have narrower social networks consisting of family members for the most part (Palumbo et al., Reference Palumbo, Volpe, Matanov, Priebe and Giacco2015), which seems to be related to e.g. rejection, discrimination, and internalized stigma (Cullen et al., Reference Cullen, Mojtabai, Bordbar, Everett, Nugent and Eaton2017; Perry, Reference Perry2011). Our study showed that individuals with high PRSSCZ have lower trajectory in perceived sociability from adolescence to middle age. Sociability as such is a normal temperament trait, being partly genetically determined and partly affected by social environment, and indicates one's personal motivation (not social skills or deficits) to spend time with others. In our study, individuals with high PRSSCZ self-reported a lower motivation to prefer and enjoy the presence of others over being alone. This raises a question whether narrower social networks in individuals with high PRSSCZ may not reflect deficits in forming social relationships but lower personal motivation to spend time in social networks.
Genetic and environmental risk factors are known to commonly accumulate within families. For example, offspring of schizophrenia patients have increased risk for prenatal substance exposure (Simoila et al., Reference Simoila, Isometsä, Gissler, Suvisaari, Halmesmäki and Lindberg2020), premature birth (Simoila et al., Reference Simoila, Isometsä, Gissler, Suvisaari, Halmesmäki and Lindberg2018), and placement in out-of-home care (Simoila et al., Reference Simoila, Isometsä, Gissler, Suvisaari, Sailas, Halmesmäki and Lindberg2019). Also, polygenic risk for schizophrenia correlates with unfavorable child-rearing practices, traumatic experiences in childhood, and stronger socioeconomic neighborhood deprivation (Zhu et al., Reference Zhu, Ward, Cullen, Lyall, Strawbridge, Smith and Lyall2021). In our study, different social trajectories in participants with high PRSSCZ sustained after controlling for a set of normal-life adversities such as adverse emotional family atmosphere (e.g. harsh parenting attitudes, parental life dissatisfaction), stressful life events (e.g. parental divorce), or socioeconomic factors.
Regarding limitations, there was some drop-out over the long follow-up from 1980 onwards. When investigating whether this drop-out caused some bias in the composition of our sample, we did not find any bias PRSSCZ, PRSDEP, perceived sociability, number of children, or adulthood socioeconomic factors. Included (v. dropped-out) participants had, however, slightly higher age in first-child parenthood (28.1 v. 27.5 years), higher likelihood of being in partnership (86.0% v. 72.5%), and slightly higher perceived social support. Thus, included participants seemed to live in a slightly more favorable social environment than dropped-out participants.
Second, we had data available on participants' psychotic disorders but not their parents' psychotic disorders. Thus, we could not prove that different social trajectories were resulting directly from schizophrenia-related genetic liabilities rather than psychosocial effects of parents' psychotic disorders. Offspring of schizophrenia patients are at risk for stigmatization (Corrigan, Watson, & Miller, Reference Corrigan, Watson and Miller2006), weaker reciprocal relationships with parents (Strand, Boström, & Grip, Reference Strand, Boström and Grip2020), and perceived difficulties to connect with other people (Foster, Reference Foster2010). On the basis of prevalence estimates of schizophrenia, however, it is not likely that a major number of parents had been diagnosed with schizophrenia in our general population sample.
Third, our analyses cannot confirm possible causal relationships between PRSSCZ and social outcomes. Also, it is complicated to separate between individuals' proactive behavior v. individuals' responses to environmental adversities and between genetically guided v. psychosocially learned individual dispositions. Further studies are needed to explore possible mediator variables between PRSSCZ and social outcomes.
Regarding implications, there have been a number of social functioning interventions for youth at risk of psychosis (Devoe, Farris, Townes, & Addington, Reference Devoe, Farris, Townes and Addington2019). Cognitive behavioral therapy or cognitive remediation, however, are shown not to significantly improve social functioning at any follow-up point (2, 3, 6, or 12 months) in high-risk groups (Devoe et al., Reference Devoe, Farris, Townes and Addington2019). Our study indicates that, first, individuals at high risk for psychosis might need social interventions also in middle age, not only in adolescence or early adulthood. Second, our study indicates that individuals at risk for psychosis may in general have a lower temperament-based need for being in a group (over being alone). Thus, they may not benefit from broadening their social network but from increasing their emotional supportiveness of their close relationships. Finally, future studies are needed to investigate factors that could modify the associations from PRSSCZ to social trajectories; such studies could provide concrete implications for interventions.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S003329172300346X.
Funding statement
This study was financially supported by Emil Aaltonen Foundation (grant 220255). The Young Finns Study has been financially supported by the Academy of Finland: grants 356405, 322098, 286284, 134309 (Eye), 126925, 121584, 124282, 255381, 256474, 283115, 319060, 320297, 314389, 338395, 330809, and 104821, 129378 (Salve), 117797 (Gendi), and 141071 (Skidi); the Social Insurance Institution of Finland; Competitive State Research Financing of the Expert Responsibility area of Kuopio, Tampere and Turku University Hospitals (grant X51001); Juho Vainio Foundation; Paavo Nurmi Foundation; Finnish Foundation for Cardiovascular Research; Finnish Cultural Foundation; The Sigrid Juselius Foundation; Tampere Tuberculosis Foundation; Emil Aaltonen Foundation; Yrjö Jahnsson Foundation; Signe and Ane Gyllenberg Foundation; Diabetes Research Foundation of Finnish Diabetes Association; EU Horizon 2020 (grant 755320 for TAXINOMISIS and grant 848146 for To Aition); European Research Council (grant 742927 for MULTIEPIGEN project); Tampere University Hospital Supporting Foundation, Finnish Society of Clinical Chemistry and the Cancer Foundation Finland.
Competing interests
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.