Introduction
Posttraumatic stress disorder (PTSD) is a highly prevalent and chronic mental disorder (Kessler et al., Reference Kessler, Aguilar-Gaxiola, Alonso, Benjet, Bromet, Cardoso and Koenen2017), associated with personal (Schnurr, Lunney, Bovin, & Marx, Reference Schnurr, Lunney, Bovin and Marx2009) and societal costs (McGowan, Reference McGowan2019). Half (52%) of individuals with PTSD suffer from co-occurring depression (Rytwinski, Scur, Feeny, & Youngstrom, Reference Rytwinski, Scur, Feeny and Youngstrom2013); a comorbidity associated with severe symptoms, reduced functioning, and poorer treatment response in PTSD (Bedard-Gilligan et al., Reference Bedard-Gilligan, Duax Jakob, Doane, Jaeger, Eftekhari, Feeny and Zoellner2015; Haagen, Heide, Mooren, Knipscheer, & Kleber, Reference Haagen, Heide, Mooren, Knipscheer and Kleber2017). Given its chronic course and high personal and economic burden, it is crucial to identify effective psychological treatments for PTSD both in the immediate and long-term phase.
Numerous psychological PTSD treatments have been developed which can be differentiated by content (e.g. Ehlers et al., Reference Ehlers, Bisson, Clark, Creamer, Pilling, Richards and Yule2010). Trauma-focused treatment (TFT) mainly focusses on processing the individual's memory of the trauma and/or its meaning. Trauma-focused cognitive behavioral therapy (TF-CBT) typically incorporate psychoeducation, homework, relaxation, and cognitive and/or behavioral-based components (e.g. cognitive therapy, Ehlers & Clark, Reference Ehlers and Clark2000; cognitive processing therapy, Resick & Schnicke, Reference Resick and Schnicke1992; prolonged exposure, Foa & Rothbaum, Reference Foa and Rothbaum1998; Foa, Hembree, & Rothbaum, Reference Foa, Hembree and Rothbaum2007; narrative exposure therapy, Schauer, Neuner, & Elbert, Reference Schauer, Neuner and Elbert2011). Eye Movement Desensitization and Reprocessing (Shapiro, Reference Shapiro1995) recalls the traumatic memory using bilateral movements and some core elements of TF-CBT. Non-TFTs typically address coping with symptoms, emotion regulation, or current problems in life without a primary focus on the trauma. Techniques of non-TF-CBT comprise, inter alia, anxiety management, relaxation, stress management, social skills training, positive thinking, assertiveness training, or thought stopping (International Society for Traumatic Stress Studies, 2015; e.g. stress inoculation training, Veronen & Kilpatrick, Reference Veronen, Kilpatrick, Meichenbaum and Jaremko1983; seeking safety, Najavits, Reference Najavits2002). Series of other PTSD treatments exist (e.g. psychodynamic therapies or hypnotherapy), but are less frequently studied (Cusack et al., Reference Cusack, Jonas, Forneris, Wines, Sonis, Middleton and Gaynes2016).
Several systematic reviews and meta-analyses demonstrate the efficacy of psychological treatment for PTSD (e.g. Benish, Imel, & Wampold, Reference Benish, Imel and Wampold2008; Chen, Zhang, Hu, & Liang, Reference Chen, Zhang, Hu and Liang2015; Cusack et al., Reference Cusack, Jonas, Forneris, Wines, Sonis, Middleton and Gaynes2016; Gerger et al. Reference Gerger, Munder, Gemperli, Nüesch, Trelle, Jüni and Barth2014; Haagen, Smid, Knipscheer, & Kleber, Reference Haagen, Smid, Knipscheer and Kleber2015; Lambert & Alhassoon, Reference Lambert and Alhassoon2015; Lenz, Haktanir, & Callender, Reference Lenz, Haktanir and Callender2017; Sloan, Gallagher, Feinstein, Gayle Beck, & Keane, Reference Sloan, Gallagher, Feinstein, Gayle Beck and Keane2013; Thompson, Vidgen, & Roberts, Reference Thompson, Vidgen and Roberts2018; Watts et al., Reference Watts, Schnurr, Mayo, Young-Xu, Weeks and Friedman2013). TF-CBT has the strongest empirical support and current practice guidelines recommend this type of psychological treatment as first-line therapy for PTSD (e.g. American Psychological Association, [APA], 2017; Schäfer et al., Reference Schäfer, Gast, Hofmann, Knaevelsrud, Lampe, Liebermann and Wöller2019). Current evidence for TF-CBT and psychological treatment for PTSD in general, however, mainly relies on short-term outcomes; meta-analyses investigating its long-term benefits (e.g. 12 months after treatment) are largely missing. Understanding the long-term outcomes of psychological treatment for PTSD and identifying moderators of sustainable gains is critical for both clinical practitioners and researchers, particularly to inform clinical decision-making and to stimulate research into effective psychological treatment (e.g. in specific patient groups).
Seven recent systematic reviews and meta-analyses examined the lasting benefits of psychological treatment in adult PTSD. Their findings mainly represent treatment effects at short-term to medium-term, indicating medium to large improvements in PTSD symptoms up to 6 months of follow-up (Bisson, Roberts, Andrew, Cooper, & Lewis, Reference Bisson, Roberts, Andrew, Cooper and Lewis2013; Carpenter et al., Reference Carpenter, Andrews, Witcraft, Powers, Smits and Hofmann2018; Ehring et al., Reference Ehring, Welboren, Morina, Wicherts, Freitag and Emmelkamp2014; Kline, Cooper, Rytwinksi, & Feeny, Reference Kline, Cooper, Rytwinksi and Feeny2018; Lee et al., Reference Lee, Schnitzlein, Wolf, Vythilingam, Rasmusson and Hoge2016; Mavranezouli et al., Reference Mavranezouli, Megnin-Viggars, Daly, Dias, Welton, Stockton and Pilling2020; van Dis et al., Reference van Dis, van Veen, Hagenaars, Batelaan, Bockting, van de Heuvel and Engelhard2020). Two of these studies give insights into the long-term treatment effects of PTSD, i.e. at 12-month follow-up and above. One meta-analysis investigated evidence-based treatments for PTSD at medium-term, with at least 6 months of follow-up (Kline et al., Reference Kline, Cooper, Rytwinksi and Feeny2018). The findings were based on uncontrolled comparison only, and showed larger treatment effects for active treatments from baseline to medium-term follow-up (d = 2.14) compared to active control conditions for the same period (d = 1.04). Uncontrolled comparisons between psychological treatments for PTSD demonstrated no significant differences from pretest to follow-up. For the posttest to follow-up phase, exposure-based treatments were superior, while CBTs without exposure were inferior to all other treatments combined. Of the 32 included trials, eight studies (25%) had a 12-month follow-up. Only one study comprised more than 12 months of follow-up, making it difficult to disentangle any long-term benefit from medium-term outcomes. Another meta-analysis focused on CBT for anxiety disorders compared with usual care or wait-list group with at least 1 month of follow-up (van Dis et al., Reference van Dis, van Veen, Hagenaars, Batelaan, Bockting, van de Heuvel and Engelhard2020). Longer-term outcomes for PTSD alone showed medium effects at 6–12 month of follow-up and large treatment effects compared with the control group at more than 12 months of follow-up. The analyses were limited to direct comparisons, and 16 studies with a follow-up of at least 6 months were available for PTSD.
This systematic review and meta-analysis aimed to investigate the long-term outcomes across psychological treatments for adults with PTSD. We aimed to assess PTSD severity and comorbid depressive symptoms at least 12 months after treatment completion. Using comparisons both within and between studies, we aimed to increase the number of available studies with a long-term follow-up but simultaneously control for time and placebo effects. We examined whether (1) psychological treatment differed from control groups and whether (2) TFT differed from non-TFT in PTSD severity and comorbid depressive symptoms at long-term follow-up. In addition, we investigated specific moderators and their potential impact on long-term benefits of psychological treatment for PTSD.
Method
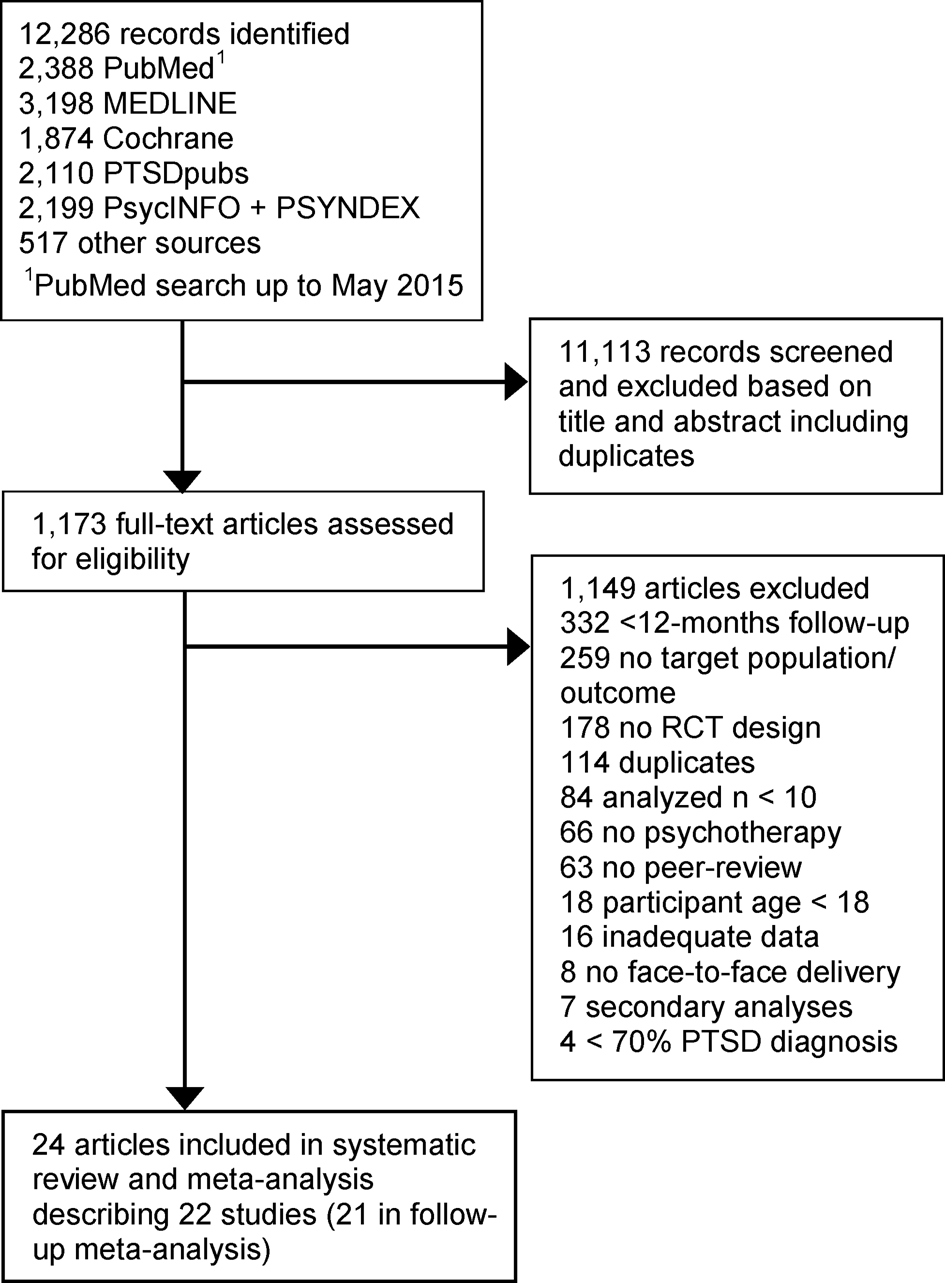
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for conducting and reporting this meta-analysis (Liberati et al., Reference Liberati, Altman, Tetzlaff, Mulrow, Gøtzsche, Ioannidis and Moher2009, see Appendix A). The study protocol was not registered a priori.
Eligibility criteria
Studies were selected if they comprised (1) face-to-face psychological treatment for PTSD, (2) adult participants, (3) at least 70% of participants diagnosed with PTSD (e.g. according to DSM-IV/V, ICD-10); (4) either active or passive, nonpharmacological control conditions (e.g. supportive counseling, wait-list) or psychological treatment as comparators; (5) PTSD severity as primary outcome measured at least 12 months after the end of treatment; (6) a randomized controlled trial design, and (7) at least ten participants per treatment arm. Trials were included based on any type of trauma, type of setting (e.g. inpatients, outpatients), presence of comorbidity, or adjuvant drug treatment (e.g. by prescription or as part of the study protocol).
Selection of studies
A systematic literature search in MEDLINE, PsycINFO, PSYNDEX, PTSDpubs, and Cochrane Library was conducted for articles in English or German language until November 7, 2019. The search strategy derived from the preparation of the German S3 treatment guideline for PTSD (Schäfer et al., Reference Schäfer, Gast, Hofmann, Knaevelsrud, Lampe, Liebermann and Wöller2019), and included the following keywords: (PTSD OR OR Posttraumatische Belastungsstörungen or PTBS) AND ((treatment trial OR randomized controlled trial) or (indexed by a thesaurus term as a clinical trial)). In addition, we performed a systematic snowball search by screening reference lists from included primary studies and relevant review articles. Two researchers independently screened articles and decided on eligible studies. In cases of disagreement between the researchers, a third researcher decided on eligibility.
Data extraction
Several study characteristics were extracted (see Appendix A). Means and standard deviations or reported effect sizes for PTSD severity (primary outcome) and comorbid depressive symptoms (secondary outcome) were extracted at baseline, posttest, and at ⩾12 months after treatment completion. In cases of multiple follow-up intervals, data from the latest was used (e.g. Karyotaki et al., Reference Karyotaki, Smit, De Beurs, Henningsen, Robays, Huibers and Cuijpers2016; Kline et al., Reference Kline, Cooper, Rytwinksi and Feeny2018). Data for clinician-rated PTSD and intent-to-treat samples (ITT) were extracted if available. If further statistical data or data subsets were needed (e.g. for adult subsample), we contacted the study authors and sent a follow-up e-mail in case of non-response (57% response rate). One researcher (MW) extracted data, which were cross-checked by a second (SSch) to ensure accuracy.
Treatment coding
We coded treatment conditions as psychological treatment or control. Psychological treatment was classified as TFT or non-TFT (Ehring et al., Reference Ehring, Welboren, Morina, Wicherts, Freitag and Emmelkamp2014; see Ehlers et al., Reference Ehlers, Bisson, Clark, Creamer, Pilling, Richards and Yule2010 for discussion). Control conditions were rated as active, if interventions were not directive or trauma-focused such as supportive counseling or treatment as usual (TAU), and served to control for non-specific mechanisms (e.g. Kline et al., Reference Kline, Cooper, Rytwinksi and Feeny2018; Lambert & Alhassoon, Reference Lambert and Alhassoon2015; Powers, Halpern, Ferenschak, Gillihan, & Foa, Reference Powers, Halpern, Ferenschak, Gillihan and Foa2010). We classified control groups as passive if there was no clinician involvement, i.e. during wait-list. Treatment coding was performed by two independent researchers (MW, WH), and a third (BK) was consulted if raters disagreed.
Study quality assessment
The included studies were assessed using the six domains from the Cochrane risk of bias tool (Higgins et al., Reference Higgins, Altman, Gotzsche, Juni, Moher, Oxman and Sterne2011): (1) random sequence generation, (2) allocation concealment, (3) blinding of participants, personnel, and (4) outcome assessment, (5) incomplete outcome data (e.g. if no ITT data were available for follow-up analysis), and (6) selective outcome reporting (e.g. if studies deviated from trial registration). All domains were rated as either low, unclear (unknown), or high risk of bias closely following the recommendations for risk of bias ratings in psychotherapy research (see Munder, & Barth, Reference Munder and Barth2018). Two researchers independently (MW, WH) coded risk of biases and consulted a third (SSch) in case of disagreement.
Statistical analyses
Effect size calculation
Two types of effect sizes were estimated using Hedges’ g (Hedges, Reference Hedges1981). Within-group effect sizes were obtained by subtracting the follow-up (or posttest) mean from the baseline (or posttest) mean. For between-group effect sizes, the control group mean was subtracted from the treatment group at follow-up or posttest divided by the pooled standard deviation. For within-group effect sizes, the standard deviation within groups was used including the correlation between the two measurements (Borenstein, Hedges, Higgins, & Rothstein, Reference Borenstein, Hedges, Higgins and Rothstein2009). Both types of effect sizes used were corrected for small sample biases (Hedges & Olkin, Reference Hedges and Olkin1985). A magnitude of 0.2, 0.5, and 0.8 represents a small, medium, and large effect size, respectively (Cohen, Reference Cohen1977). Positive effect sizes indicate improved symptoms, while the width of the respective 95% confidence interval (CI) quantifies its precision (Borenstein et al., Reference Borenstein, Hedges, Higgins and Rothstein2009).
Comprehensive meta-analysis software, version 3 (Biostat) was applied to pool effect sizes using a random-effects model. If no correlation was available to calculate within-group effect sizes, sensitivity analyses were performed by replacing the coefficient with r = 0.2, r = 0.5 and r = 0.8; the default value was set to r = 0.5 (k = 10; Borenstein et al., Reference Borenstein, Hedges, Higgins and Rothstein2009). Heterogeneity of effect sizes was tested with the Q-statistic, the I 2 value, and by visual inspections of forest plots. A p-value of the Q-statistic below 0.05 indicates heterogeneity (Cochran, Reference Cochran1954). I 2 values range from 0 to 100% and suggest presence of low (25%), medium (50%), and large (75%) heterogeneity (Higgins & Thompson, Reference Higgins and Thompson2002).
Subgroup analysis
Subgroup analyses of treatment conditions (active treatment v. control condition), treatment types (TFT v. non-TFT) were performed for the primary and secondary outcome. Dropout rates (i.e. ratio of participants initiating but not completing treatment; Ehring et al., Reference Ehring, Welboren, Morina, Wicherts, Freitag and Emmelkamp2014) were calculated for both conditions and treatment subgroups. For PTSD severity, six additional variables were analyzed: proportion of female participants [high (⩾50%) v. low (<50%); Sloan et al., Reference Sloan, Gallagher, Feinstein, Gayle Beck and Keane2013; Watts et al., Reference Watts, Schnurr, Mayo, Young-Xu, Weeks and Friedman2013], type of population (military personnel v. civilian; Kline et al., Reference Kline, Cooper, Rytwinksi and Feeny2018), treatment format (individual v. group-based; Ehring et al., Reference Ehring, Welboren, Morina, Wicherts, Freitag and Emmelkamp2014; Haagen et al., Reference Haagen, Smid, Knipscheer and Kleber2015), average number of treatment sessions [high (⩾10 sessions) v. low (<10 sessions); Lambert & Alhassoon, Reference Lambert and Alhassoon2015], outcome measure (self-rated v. clinician-assessed, Lambert & Alhassoon, Reference Lambert and Alhassoon2015), and type of analysis at follow-up (Kline et al., Reference Kline, Cooper, Rytwinksi and Feeny2018). Analyses on within-group effect sizes were conducted using the mixed-effect model and the Q-statistics (Borenstein et al., Reference Borenstein, Hedges, Higgins and Rothstein2009) if at least three comparisons per subgroup were available.
Publication bias
We applied Egger's regression test (Egger, Davey Smith, Schneider, & Minder, Reference Egger, Davey Smith, Schneider and Minder1997) and Duval and Tweedie's trim-and-fill procedure (Duval & Tweedie, Reference Duval and Tweedie2000) to test publication bias if data sets contained at least six studies presenting no substantial heterogeneity (Ioannidis & Trikalinos, Reference Ioannidis and Trikalinos2007; Rothstein, Sutton, & Borenstein, Reference Rothstein, Sutton and Borenstein2005; Sterne, Becker, & Egger, Reference Sterne, Becker, Egger, Rothstein, Sutton and Borenstein2006; Terrin, Schmid, Lau, & Olkin, Reference Terrin, Schmid, Lau and Olkin2003).
Results
Included studies
The search yielded 12 286 hits. Twenty-two eligible studies were included in this meta-analysis (Fig. 1). Studies were published between 1999 and 2018 and comprised 28–353 participants per study sample (N = 2638; Median = 101; Table 1). Participants (53% female) were on average 40 years old and met DSM-III/IV diagnostic criteria for PTSD (96%). Studies assessed civilian (64%) and military populations (32%) in individual-based treatment (86%). Nine studies (41%) quantified that 31–100% of participants received additional psychotropic medication during treatment. Five studies (23%) reported a stable medication dose for > 30 days at study entry for inclusion, and two studies (9%) excluded participants receiving any additional medication.

Fig. 1. Long-term outcomes of psychological treatment for PTSD.
Table 1. Study characteristics of included randomized controlled trials with at least 12 months follow-up (LFU)

A, alprazolam; AC, academic catch-up; B–CBT, brief cognitive behavioral therapy; BA + E, behavioral activation and exposure; BA + E TH, behavioral activation and exposure telehealth-based; BDI–II, beck depression inventory–II; BDI, Beck depression inventory; C, d-cycloserine; CAPS, clinician-administered PTSD scale; CBT, cognitive behavioral therapy; CPT–M, cognitive processing therapy modified; CPT, cognitive processing therapy; CR, cognitive restructuring; EG, educational group therapy; EMDR, eye movement desensitization and reprocessing; HADS, hospital anxiety and depression scale – depression subscale; HAM–D, Hamilton depression scale; HDRS, Hamilton depression rating scale; ICBTcom, integrated cognitive behavioral treatment for comorbidities; IOE, impact of events scale; IR, imagery rescripting therapy; MINI, mini international neuropsychiatric interview; n, sample size; n session, average number of sessions; NET, narrative exposure therapy; NTF, non-trauma-focused treatment; PCL-C, PTSD checklist – civilian version; PCL-M, PTSD checklist – military version; PCLS, post-traumatic checklist scale; PCT, present-centered therapy; PDSi, posttraumatic diagnostic scale – Interview-based; PE, prolonged exposure; Pla, placebo; PSS-I, PTSD symptom scale – Interview; PTSD, posttraumatic stress disorder; SC, supportive counseling; Se, sertraline; SIT, stress inoculation training; SMT, self-management therapy; SS, seeking safety; TAU, treatment as usual; TF, trauma-focused treatment; VR, virtual reality exposure therapy; WET, written exposure therapy; WL, wait-list.
a We thank primary study authors for providing additional data and/or data subsets.
b Treatment condition was excluded from all meta-analyses.
c Treatment condition was excluded from follow-up meta-analysis.
Of 46 included treatment conditions at posttest, 35 were active treatments including 28 TFT (k = 27 TF-CBT, k = 1 EMDR), and 7 non-TFT (all CBT). The 11 active, non-directive control conditions consisted of TAU (k = 5), social counseling (k = 3), present-centered therapy (k = 2), and educational groups (k = 1). One of six wait-list conditions was available at follow-up, and thus all passive control conditions were removed from analyses. Three active treatment conditions had inadequate follow-up data (k = 2 TF-CBT, k = 1 EMDR), and remained for qualitative and pre-post analyses, resulting in 43 CBT-based conditions for primary analyses. The average follow-up lasted 18 months and ranged from 12 to 74 months. Five studies (23%) had more than 12 months of follow-up. The dropout rate in active treatments (24%, k = 30) did not significantly differ from active control groups (18%, k = 7, p = 0.32). Dropouts in TFT (25%, k = 24) did also not differ significantly from non-TFT (21%, k = 6, p = 0.42).
Long-term treatment effects on PTSD severity
Within-group effect sizes
Across all active treatments, the pooled within-group effect size was large for PTSD severity from pretest to follow-up, g = 1.36, 95% CI (1.14–1.57), p < 0.001 (Table 2; see Appendix A for all forest plots). Non-directive control conditions showed a medium effect size for the same period, g = 0.59, 95% CI (0.14–1.04), p < 0.05. Active treatments were more effective in reducing PTSD severity compared to non-directive control conditions from pretest to follow-up, respectively (p < 0.01). In addition, TFT and non-TFT types both yielded large within-group effect sizes from pretest to follow-up g = 1.44, 95% CI (1.20–1.67), p < 0.001; g = 1.08, 95% CI (0.52–1.63), p < 0.001, and effect sizes did not significantly differ from each other (p = 0.24). From posttest to follow-up, PTSD symptoms slightly improved in the active treatment and control conditions, g = 0.33 95% CI (0.23–0.44), p < 0.001; g = 0.16, 95% CI (0.04–0.28), p < 0.05 (see Appendix A). From pretest to posttest, within-effect sizes were large for active treatments and medium for control groups, g = 1.01, 95% CI (0.87–1.14), p < 0.001; g = 0.52, 95% CI (0.16–0.87), p < 0.01.
Table 2. Within-effect sizes (pretest – follow-up) and subgroup analyses for PTSD severity

Note. Analyses based on 21 studies (20 for proportion female).
p-values less than 0.05 represent statistical significance. 95% CI = 95% confidence intervals, g = Hedges’ g, k = number of comparisons, PTSD = posttraumatic stress disorder.
1 Additional subgroup analyses for PTSD indicated significantly larger treatment effects for intention-to-treat samples with higher compared to lower dropout rates (⩾20%; <20%, p < 0.01), while treatment effects remained unaffected by losses to follow-up (<40%; ⩾40%, p = 0.61). In completer samples, attrition rates had no impact on treatment outcomes (p = 0.56; p = 0.34).
a p-value of Hedges’ g.
b p-value of Q-statistics.
c p-value between groups.
d Analyses include active treatments only.
Heterogeneity was large for within-group effect sizes from pretest to follow-up across condition and treatment types (Q > 62, p < 0.001, I 2 > 81, Table 2). None of the moderators examined for PTSD severity – except for self-rated PTSD measure (Q = 5.16, p = 0.16, I 2 = 41.91) – increased homogeneity in active treatments. However, subgroup analyses showed higher effect sizes for civilian compared to military populations (p < 0.01), for studies with larger proportions of female participants (p < 0.001), and for interview-based compared to self-rated outcome measures (p < 0.001). Subgroups did not significantly differ regarding treatment format, number of sessions, type of analysis used, or follow-up duration.
Between-group effect sizes
The pooled between-group effect size comparing active treatments to non-directive control groups was small for improved PTSD severity at follow-up, g = 0.42, 95% CI (0.15–0.68), p < 0.001 (Table 3). TFT showed a medium controlled effect size compared with control groups at follow-up, g = 0.51, 95% CI (0.15-0.86), p < 0.05. The effect size comparing TFT with non-TFT at follow-up was small and did not reach statistical significance, g = 0.35, 95% CI (−0.03 to 0.74), p = 0.07. At posttest, between-group effect sizes were small favoring active treatments and TFT over control groups, g = 0.24, 95% CI (0.04–0.44), p < 0.05; g = 0.25, 95% CI (0.03–0.47), p < 0.05 (see Appendix A).
Table 3. Between-effect sizes at follow-up

Note. 95% CI = 95% confidence intervals, g = Hedges’ g, k = number of comparisons, PTSD = posttraumatic stress disorder, TFT = trauma-focused treatment.
a p-value of Hedges’ g.
b p-value of Q-statistics.
Heterogeneity was moderate for between-condition effect sizes at follow-up (Q > 26, p < 0.001, I 2 > 71), and low in the treatment type comparison (Q = 0.47, p = 0.79; I 2 = 0, k = 3).
Long-term treatment effects on comorbid depressive symptoms
Within-group effect sizes
Active treatments demonstrated a medium within-group effect size for reduced depressive symptoms from pretest to follow-up, g = 0.73, 95% CI (0.55–0.71), p < 0.001 (Table 4). Non-directive control conditions showed a small effect size from pretest to follow-up, g = 0.34, 95% CI (0.11–0.58), p < 0.01, which was significantly lower compared to the effect size of active treatments for the same period (p < 0.05). Within-group effect sizes were medium for TFTs, g = 0.78, 95% CI (0.58–0.99), p < 0.01, and small for non-TFTs from pretest to follow-up, g = 0.45, 95% CI (0.17–0.74), p < 0.01. However, this contrast was statistically not significant (p = 0.06). From posttest to follow-up, depressive symptoms remained stable in active treatments and control conditions, g = 0.10, 95% CI (−0.01 to 0.21), p = 0.08; g = 0.24, 95% CI (0.09–0.38), p < 0.001 (see Appendix A). Effect sizes from pretest to posttest were medium for active treatments and small for control groups, g = 0.68, 95% CI (0.55–0.80), p < 0.001; g = 0.24, 95% CI (0.09–0.39), p < 0.01.
Table 4. Within-effect sizes (pretest, follow-up) and subgroup analyses for comorbid depressive symptoms

Note. 95% CI = 95% confidence intervals, g = Hedges’ g, k = number of comparisons, PTSD = posttraumatic stress disorder.
a p-value of Hedges’ g.
b p-value of Q-statistics.
c p-value between groups.
d Analyses include active treatments only.
All within-group effect sizes were largely heterogeneous at follow-up (Q > 33, p < 0.001; I 2 > 76, see Table 3), except for non-TFTs (Q = 4.54, p = 0.21; I 2 = 33.91, k = 4).
Between-group effect sizes
Table 3 reports small and non-significant between-group effect sizes of active treatments compared with active control conditions for comorbid depressive symptoms at follow-up, g = 0.15, 95% CI (−0.02 to 0.31), p = 0.08. Effect sizes of TFT were small compared with active control groups, g = 0.14, 95% CI (−0.03 to 0.32), p < 0.05, and did not differ statistically significant from non-TFT at follow-up, g = 0.10, 95% CI (−0.38 to 0.58), p = 0.68. At posttest, again between-group effect sizes for active treatments and TFTs were small compared with control groups, g = 0.30, 95% CI (0.06–0.53), p < 0.05; g = 0.32, 95% CI (0.04–0.59), p = 0.12 (see Appendix A).
Heterogeneity of between-condition effect sizes was low (Q < 4, p > 0.05; I 2 < 27) to large (Q > 30, p < 0.001; I 2 > 80, see Table 3).
Study quality
The overall risk of bias from studies included in this systematic review and meta-analysis ranged from low (50%) and unclear (24%) to high (26%) across all bias domains (see Appendix A for details per study). Most studies generated a low risk of bias concerning sequence generation (68%, k = 15), allocation concealment (50%, k = 11), and blinding of outcome assessors (90%, k = 20). Nine studies (41%) provided complete outcome data at follow-up indicating a low risk of bias. Nine studies (41%) also registered or published their study protocol a priori and adhered to it, while in half of the studies (50%) selective outcome reporting remained unclear. Few studies applied blinding of participants and personnel (9%, k = 2), and only one study had a low risk of bias in all domains.
Additional analyses
The replaced correlations using r = 0.2 and r = 0.8 revealed marginally altered within-group effect sizes for active treatments and control conditions in all comparisons (see Appendix A for sensitivity analyses).
Publication bias remained untested due to moderate or large heterogeneity between effect sizes and small number of studies in our datasets (Ioannidis & Trikalinos, Reference Ioannidis and Trikalinos2007; Rothstein et al., Reference Rothstein, Sutton and Borenstein2005; Sterne et al., Reference Sterne, Becker, Egger, Rothstein, Sutton and Borenstein2006; Terrin et al., Reference Terrin, Schmid, Lau and Olkin2003).
Discussion
Summary of evidence
This systematic review and meta-analysis of 22 randomized controlled trials indicate that psychological treatment for adults with PTSD is efficacious in the long term. Active treatments yielded large symptom reductions of PTSD from pretest up to at least 12 months after initial treatment. Small treatment effects favored psychological treatment over non-directive control groups at follow-up, and symptom improvements remained stable from posttest to follow-up. TFT and non-TFT yielded large sustained improvements in PTSD from pretest to follow-up. Treatment effects of TFT were medium relative to non-directive control groups, and not significantly different from non-TFT at follow-up. Effect size estimates were of considerable heterogeneity and the number of available comparisons was low.
The large and stable within-group effect sizes of psychological treatment for PTSD in this meta-analysis are comparable with previous results at both short-term and medium-term follow-up (Ehring et al., Reference Ehring, Welboren, Morina, Wicherts, Freitag and Emmelkamp2014; Kline et al., Reference Kline, Cooper, Rytwinksi and Feeny2018), yet uncontrolled comparisons must be interpreted cautiously. The between-group effect size of psychological treatment compared with active control groups is smaller than reported in a previous study with pooled wait-list and active control groups as comparator at follow-up (van Dis et al., Reference van Dis, van Veen, Hagenaars, Batelaan, Bockting, van de Heuvel and Engelhard2020). However, the between-group effect size of TFT relative to active control groups is consistent with the previous finding. All active treatments included cognitive behavioral therapy (CBT) with TFT most frequently (78%) studied long-term, which is in line with previous evidence at medium-term follow-up (e.g. Kline et al., Reference Kline, Cooper, Rytwinksi and Feeny2018). The enduring treatment effects of trauma-focused CBT after an average of 18 months confirm its recommendation as first-line therapy for PTSD (e.g. APA, 2017). One follow-up study was available on EMDR, yet the long-term data were insufficient to be included for meta-analysis. This finding highlights its current weaker empirical support as PTSD treatment (APA, 2017), and lasting benefits beyond CBT outcomes require future research. A few studies examined non-TFT showing large and enduring benefits for PTSD, which mirrors prior short-term findings regarding its empirical support and efficacy (e.g. Ehring et al., Reference Ehring, Welboren, Morina, Wicherts, Freitag and Emmelkamp2014; Lenz et al., Reference Lenz, Haktanir and Callender2017; Powers et al., Reference Powers, Halpern, Ferenschak, Gillihan and Foa2010). Effect sizes of non-TFT were smaller compared with TFT at follow-up as previously reported (Ehring et al., Reference Ehring, Welboren, Morina, Wicherts, Freitag and Emmelkamp2014), but the difference was statistically non-significant. Given the small number of comparisons for non-TFT in particular, non-significant results should be interpreted as the absence of statistical evidence rather than as evidence of non-inferiority (Rief & Hofmann, Reference Rief and Hofmann2018).
The within-group effect sizes of psychological treatments for improved comorbid depressive symptoms were medium from pretest to follow-up (or posttest), and smaller than previous findings at short-term follow-up on treatments aiming to reduce depression or PTSD (Morina, Malek, Nickerson, & Bryant, Reference Morina, Malek, Nickerson and Bryant2017). Between-group effect sizes at follow-up were also smaller than in the previous study mainly comparing active treatments to waitlist groups. Studies less frequently (73%) reported secondary depression outcomes at follow-up, and comparisons for depressive symptoms were likely underpowered.
The included studies differed widely across sample-related and treatment-related characteristics, and meta-analyses including the present one are inherently associated with heterogeneous effect sizes. In addition, dropout in active treatments was slightly higher compared to previous rates from mixed populations (Kline et al., Reference Kline, Cooper, Rytwinksi and Feeny2018; Lewis, Roberts, Gibson, & Bisson, Reference Lewis, Roberts, Gibson and Bisson2020), but lower than in military samples alone (Goetter et al., Reference Goetter, Bui, Ojserkis, Zakarian, Brendel and Simon2015). TFT and non-TFT types did not differ in dropout rates, which reflects some findings (e.g. Imel, Laska, Jakupcak, & Simpson, Reference Imel, Laska, Jakupcak and Simpson2013; Thompson et al., Reference Thompson, Vidgen and Roberts2018), and opposes others (Lewis et al., Reference Lewis, Roberts, Gibson and Bisson2020).
Half of all studies (50%) were at high risk of bias in at least two domains potentially increasing the risk of overestimated treatment effects (e.g. Cuijpers, van Straten, Bohlmeijer, Hollon, & Andersson, Reference Cuijpers, van Straten, Bohlmeijer, Hollon and Andersson2010b). Subgroup analysis indicated large and non-significantly different effect sizes from ITT and completer samples at follow-up. However, in ITT samples (but not in completer samples) higher dropout was associated with larger effect sizes. This suggests that dropout is a critical source of bias that ITT analyses may not fully resolve assuming data are missing at random (White, Horton, Carpenter, & Pocock, Reference White, Horton, Carpenter and Pocock2011). In addition, treatment effects were significantly higher for studies using interview-based outcome measures compared to self-rated measures, challenging prior results from subgroup analyses in PTSD (Kline et al., Reference Kline, Cooper, Rytwinksi and Feeny2018; Lambert & Alhassoon, Reference Lambert and Alhassoon2015). As suggested for depression outcomes earlier, self-rated measures either underrated the improved symptoms, clinician-rated interviews were more sensitive to change, or a combination of both (Cuijpers, Li, Hofmann, & Andersson, Reference Cuijpers, Li, Hofmann and Andersson2010a).
The improved PTSD symptoms at follow-up in female and civilian populations compared with male and military subgroups replicate previous findings at short-term (Sloan et al., Reference Sloan, Gallagher, Feinstein, Gayle Beck and Keane2013; Watts et al., Reference Watts, Schnurr, Mayo, Young-Xu, Weeks and Friedman2013) and medium-term follow-up (Kline et al., Reference Kline, Cooper, Rytwinksi and Feeny2018; Wade et al., Reference Wade, Varker, Kartal, Hetrick, O'Donnell and Forbes2016). However, we noted that proportions of male participants were small in civilian populations but close to 100% in military samples, and future studies with balanced samples need to disentangle the effect of gender and population type. Importantly, treatment effects for PTSD did not differ regarding the length of follow-up duration, indicating that symptom improvements persisted beyond 12 months after treatment. The current number of studies with longer follow-up intervals is limited, and future evidence is required to confirm treatment gains beyond 12 months following treatment. Subgroup analyses on pre-specified moderators are exploratory and should be interpreted with caution as additional study-level factors may confound the results (Higgins & Green, Reference Higgins and Green2011).
Strengths and limitations
This systematic review and meta-analysis on long-term benefits of psychological treatment exceeds the number and variety of treatment studies included in former meta-analyses for PTSD (Kline et al., Reference Kline, Cooper, Rytwinksi and Feeny2018; van Dis et al., Reference van Dis, van Veen, Hagenaars, Batelaan, Bockting, van de Heuvel and Engelhard2020), and provides first evidence for comorbid depressive symptoms in PTSD at long-term. In addition, we performed a comprehensive literature search, adhered closely to the PRISMA recommendations, and examined pre-specified moderators of lasting treatment gains. However, there are several limitations to be noted. First, publication bias could not be tested due to small databases and considerable heterogeneity (Ioannidis & Trikalinos, Reference Ioannidis and Trikalinos2007; Rothstein et al., Reference Rothstein, Sutton and Borenstein2005; Sterne et al., Reference Sterne, Becker, Egger, Rothstein, Sutton and Borenstein2006; Terrin et al., Reference Terrin, Schmid, Lau and Olkin2003). Second, several studies had small sample sizes and included an unclear or high risk of bias. We analyzed two bias domains with no impact on effect sizes, but confidence in the results may remain limited. Third, the number of comparisons at follow-up was low, and specific treatment types beyond broad categories (i.e. TFT, non-TFT) remained untested. Finally, the studies provided few and inconsistent data on additional treatment (e.g. medication) during psychological treatment, and on whether participants received any treatment during the follow-up phase. It remains unclear if benefits can be ascribed to the initial psychological treatment alone.
Conclusion
The results of this meta-analysis on psychological treatment for PTSD demonstrate large and sustained benefits after at least 12 months of follow-up. Active treatments were CBTs, and most studies examined TFT. Effect sizes of TFT were large for improved PTSD and medium for comorbid depressive symptoms from pretest to follow-up and superior to active control groups at follow-up. Non-TFT showed small to large benefits for PTSD and depressive symptoms from pretest to follow-up, respectively, but the number of available studies was scarce. Future well-designed studies are essential to determine the sustained gains from specific CBT types and other psychological treatments, and to confirm benefits beyond 12 months following initial treatment.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S003329172100163X.
Acknowledgements
With thanks to the German PTSD treatment guideline group for providing the results from earlier literature searches, and for supporting the implementation of this work. We thank Helen Niemeyer for statistical advices. We also like to thank all authors of the included primary studies for providing additional data for this systematic review and meta-analysis.
Author contributors
MW and BK initiated this project. MW, WH, AL, TE, and ISch were involved in the literature research. MW extracted the data, which were cross-checked by SSch. MW and WH independently performed the treatment coding, which was supervised by BK. MW and WH independently performed the quality assessment, and SSch acted as the third rater. MW performed the statistical analyses and wrote the first draft of the manuscript under close supervision of BK and SSch. JB contributed to the statistical analyses and interpretation. All authors approved the final manuscript.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
All authors declare no conflict of interest.