Introduction
Stress likely plays a role in the onset of various mental disorders, including psychosis, notably in vulnerable individuals (Corcoran et al., Reference Corcoran, Walker, Huot, Mittal, Tessner, Kestler and Malaspina2003; Kessler et al., Reference Kessler, McLaughlin, Green, Gruber, Sampson, Zaslavsky and Williams2010). Besides major life events, minor daily-life stressors (daily hassles) are associated with the development of psychotic symptoms and more broadly with psychopathology (Kanner, Coyne, Schaefer, & Lazarus, Reference Kanner, Coyne, Schaefer and Lazarus1981; Tessner, Mittal, & Walker, Reference Tessner, Mittal and Walker2011). Sensitization has been proposed as a mechanism linking earlier stress exposure to later mental health issues; the stress sensitization model posits that past exposure to environmental stress can alter stress regulation, resulting in more intense responses to minor stressors, and heightens the risk for developing psychiatric disorders (Collip, Myin-Germeys, & Van Os, Reference Collip, Myin-Germeys and Van Os2008). Earlier studies have shown that daily stressors activate the hypothalamic–pituitary–adrenocortical (HPA)-axis by increasing cortisol levels (Collip et al., Reference Collip, Nicolson, Lardinois, Lataster, van Os and Myin-Germeys2011), and that the stress–cortisol relationship is mediated by negative affects (NA) (Jacobs et al., Reference Jacobs, Myin-Germeys, Derom, Delespaul, van Os and Nicolson2007). Therefore, measuring negative affective responses to minor stressors could provide indirect evidence of how sensitive individuals are to stress. Moreover, the strategies that are used to cope with these minor stressors might contribute to the intensity of stress responses (Sladek, Doane, Luecken, & Eisenberg, Reference Sladek, Doane, Luecken and Eisenberg2016) and be associated with psychopathological symptoms (Compas et al., Reference Compas, Jaser, Bettis, Watson, Gruhn, Dunbar and Thigpen2017).
Ecological momentary assessment (EMA), a structured diary method that enables repeated assessments in the flow of daily life is a particularly well-suited technique to investigate affective responses to stress (Myin-Germeys et al., Reference Myin-Germeys, Kasanova, Vaessen, Vachon, Kirtley, Viechtbauer and Reininghaus2018). EMA studies have shown that perceived stress is associated with increased NA (e.g. Myin-Germeys, van Os, Schwartz, Stone, & Delespaul, Reference Myin-Germeys, van Os, Schwartz, Stone and Delespaul2001), thus affective reactivity to stress has been defined as an increase in NA in relation to minor stressors. Similarly, an increase in momentary psychotic experiences related to stress is defined as psychotic reactivity to stress (Myin-Germeys, Delespaul, & van Os, Reference Myin-Germeys, Delespaul and van Os2005). Altered reactivity to stress is seen as a vulnerability marker for psychopathology, particularly for psychosis (Myin-Germeys et al., Reference Myin-Germeys, Peeters, Havermans, Nicolson, DeVries, Delespaul and Van Os2003; Myin-Germeys & van Os, Reference Myin-Germeys and van Os2007; Vaessen et al., Reference Vaessen, van Nierop, Decoster, Delespaul, Derom, De Hert and Thiery2017). It is thought that heightened sensitivity to stress at the ‘micro-level’ (as measured in the moment in daily life) may lead to the persistence of psychotic symptoms at the ‘macro-level’, and subsequently to the development of psychosis (Collip et al., Reference Collip, Wigman, Myin-Germeys, Jacobs, Derom, Thiery and van Os2013). Indeed, elevated affective and psychotic reactivity to stress have often been reported in patients with psychosis, their siblings and individuals at clinical high-risk (CHR) for psychosis (e.g. Lataster, Collip, Lardinois, van Os, & Myin-Germeys, Reference Lataster, Collip, Lardinois, van Os and Myin-Germeys2010; Myin-Germeys et al., Reference Myin-Germeys, van Os, Schwartz, Stone and Delespaul2001; Palmier-Claus, Dunn, & Lewis, Reference Palmier-Claus, Dunn and Lewis2012). Notably, it has been suggested that exposure to social stress (e.g. social-evaluative threat) could play a role in the development of psychosis in vulnerable individuals (Jones & Fernyhough, Reference Jones and Fernyhough2007). A recent review of EMA studies showed that individuals with schizophrenia experience increased social stress in their daily lives (Mote & Fulford, Reference Mote and Fulford2020). Similarly, heightened social stress and increased reactivity to social stressors have been reported in CHR individuals (Palmier-Claus et al., Reference Palmier-Claus, Dunn and Lewis2012). Moreover, Millman et al. (Reference Millman, Pitts, Thompson, Kline, Demro, Weintraub and Schiffman2018) recently showed an association between perceived social stress and more severe positive psychotic symptoms in CHR adolescents, supporting the role of social stress in psychosis. To further examine whether alterations in reactivity to (social) stress are related to the severity of subthreshold psychotic symptoms in vulnerable individuals, the study of a population at high risk for psychosis, such as individuals with chromosome 22q11.2 deletion syndrome (22q11DS), appears highly valuable.
22q11DS is a neurogenetic condition, resulting from a 1.5–3 megabase deletion on the long arm of chromosome 22, which has an estimated prevalence of 1:2148 live births (Blagojevic et al., Reference Blagojevic, Heung, Theriault, Tomita-Mitchell, Chakraborty, Kernohan and Bassett2021). The syndrome is associated with a high prevalence of psychiatric comorbidities, notably schizophrenia-spectrum disorders (Schneider et al., Reference Schneider, Debbané, Bassett, Chow, Fung, van den Bree and Eliez2014). Individuals with 22q11DS are thought to experience high levels of chronic stress from childhood (Beaton & Simon, Reference Beaton and Simon2011) and use less adaptive coping strategies compared to individuals from the general population (Armando et al., Reference Armando, Sandini, Chambaz, Schaer, Schneider and Eliez2018; Ilen et al., Reference Ilen, Feller, Eliez, Micol, Delavari, Sandi and Schneider2022). Furthermore, indirect evidence of HPA-axis dysregulation, demonstrated as alterations in cortisol levels or in pituitary volume (Armando et al., Reference Armando, Sandini, Chambaz, Schaer, Schneider and Eliez2018; Jacobson, Bursch, & Lajiness-O'Neill, Reference Jacobson, Bursch and Lajiness-O'Neill2016; Sanders, Hobbs, Stephenson, Laird, & Beaton, Reference Sanders, Hobbs, Stephenson, Laird and Beaton2017; Sandini et al., Reference Sandini, Chambaz, Schneider, Armando, Zöller, Schaer and Eliez2020; van Duin et al., Reference van Duin, Vaessen, Kasanova, Viechtbauer, Reininghaus, Saalbrink and Myin-Germeys2019), could point toward altered stress reactivity in 22q11DS as well as the role of stress in the development of psychopathology (Ilen et al., Reference Ilen, Feller, Eliez, Micol, Delavari, Sandi and Schneider2022). However, affective and psychotic reactivity to daily-life stress has only been investigated once in a sample of adults with 22q11DS (Schneider et al., Reference Schneider, Vaessen, van Duin, Kasanova, Viechtbauer, Reininghaus and Myin-Germeys2020). This study did not show alterations in stress reactivity in adults with 22q11DS compared to healthy controls (HC), but suggested that they could experience minor events as more stressful. However, the sample of this study, consisting of relatively high-functioning adults, was not fully representative of the 22q11DS population. Given that adolescence and emerging adulthood is a period characterized by increased stress reactivity (especially toward social stressors) (van den Bos, De Rooij, Miers, Bokhorst, & Westenberg, Reference van den Bos, De Rooij, Miers, Bokhorst and Westenberg2014) as well as heightened risk for the onset of mental disorders (Kessler et al., Reference Kessler, Angermeyer, Anthony, R, Demyttenaere, Gasquet and Ustün2007), investigating stress reactivity and its link with psychopathology is particularly relevant at this age. In light with high social anxiety (Schneider et al., Reference Schneider, Debbané, Bassett, Chow, Fung, van den Bree and Eliez2014), impairments in social skills (Shashi et al., Reference Shashi, Veerapandiyan, Schoch, Kwapil, Keshavan, Ip and Hooper2012), and deficits in social cognition (for a review, see Milic, Feller, Schneider, Debbané, & Loeffler-Stastka, Reference Milic, Feller, Schneider, Debbané and Loeffler-Stastka2021) associated with the syndrome, social stress may be specifically important to investigate in youths with 22q11DS.
In the present study, the aim was to use EMA to investigate affective and psychotic reactivity to daily-life stressors (social, activity-related, and event-related stress) in adolescents and young adults with 22q11DS compared to HC. Moreover, we aimed to examine whether the effect of stress on NA/psychotic experiences is moderated by non-adaptive coping strategies, and whether stress reactivity is related to psychotic symptoms or more general psychopathology in 22q11DS. We hypothesized that the 22q11DS group would show higher levels of perceived stress and increased reactivity to stress compared to HC, and that heightened stress reactivity would be associated with more severe psychopathology in 22q11DS.
Methods
Sample
Forty participants (22 males, 18 females) with a confirmed diagnosis of 22q11DS aged 12–28 years participated in the present study. Data were collected since August 2018 through the Swiss 22q11DS longitudinal cohort. The 22q11.2 deletion was confirmed using microarray analysis. In total, 55 HC (27 males, 28 females) aged 12–25 years were recruited through the siblings of the participants with 22q11DS and within the Geneva local community. Sample characteristics are shown in Table 1. Of note, part of our sample (i.e. n = 21 22q11DS and n = 32 HC) overlapped with that of our earlier study (Ilen et al., Reference Ilen, Feller, Eliez, Micol, Delavari, Sandi and Schneider2022). There was no overlap with the earlier study investigating stress reactivity in adults with 22q11DS (Schneider et al., Reference Schneider, Vaessen, van Duin, Kasanova, Viechtbauer, Reininghaus and Myin-Germeys2020).
Table 1. Group comparisons of demographic characteristics and variables of interest

SCQ, The Social Communication Questionnaire (Rutter, Bailey, & Lord, Reference Rutter, Bailey and Lord2003); SSRI, selective serotonin reuptake inhibitors.
a For EMA variables, age, sex, and EMA period were controlled.
b Other diagnoses include gambling disorder and excoriation disorder.
Note: The same participant can have >1 diagnoses and medication. For one participant with 22q11DS, information about diagnosis, psychotic symptoms, and medication was not available.
*p < 0.05; **p < 0.01; ***p < 0.001.
All participants had to have sufficient verbal and intellectual skills, and at least one parent/caretaker available to participate in the study. For participants with an IQ score within the intellectual disability range (n = 16), reading comprehension as well as comprehension about the principles of a Likert scale was clinically assessed during the EMA briefing session and it was ensured that the participants understood and were able to answer all the questions. Exclusion criteria for HC were (1) premature birth, (2) first-degree relative with developmental disorder (with the exception of a de novo 22q11.2 deletion), (3) neurological disorder, (4) history of psychiatric disorder, or (5) history of learning/language disorder requiring treatment. All participants and caretakers gave their written consent. Participants received a financial compensation of 100 Swiss francs (CHF) for participating in a larger study including also additional measures. The study was approved by the Cantonal Research Ethics Committee of Geneva (CCER).
Materials
Ecological momentary assessment
Smartphone-based EMA was used to evaluate participants' affects, momentary psychotic experiences, and perceived stress in daily-life context. EMA data collection and measures are detailed in the online Supplementary material.
Questionnaires
The use of coping strategies was evaluated with two self-reported questionnaires. In the Cognitive Emotion Regulation Questionnaire (CERQ) (Garnefski, Kraaij, & Spinhoven, Reference Garnefski, Kraaij and Spinhoven2001), the use of adaptive (acceptance, positive refocusing, refocus on planning, positive reappraisal, putting into perspective) and non-adaptive (self-blame, rumination, catastrophizing, and blaming others) strategies in response to negative events is examined on a 5-point Likert scale (1 = almost never, 5 = almost always). The Adolescent Coping Orientation for Problem Behaviors (A-COPE) (Patterson & McCubbin, Reference Patterson and McCubbin1987) evaluates how often on a 5-point Likert scale (1 = never, 5 = most of the time) participants use different behaviors when confronted with difficulties or feeling tense. Studies using the A-COPE operationalized the underlying dimensions of coping behaviors in different ways. In this study, we used a factor structure derived from an European (Spanish) sample, which grouped different behaviors in eight coping styles: engaging in demanding activities, seeking diversion, seeking family support, positive re-appraisal, seeking spiritual support, escaping, ventilating feelings, and searching for friendship (Forns et al., Reference Forns, Kirchner, Peró, Pont, Abad, Soler and Paretilla2013). According to a second-order factor analysis, the authors considered the first five strategies as approach focus of coping (respective factor loadings = 0.73, 0.71, 0.67, 0.64, and 0.32) and the three last strategies as avoidance coping (0.78, 0.66, 0.61) (Forns et al., Reference Forns, Kirchner, Peró, Pont, Abad, Soler and Paretilla2013). However, it should be noted that there is no consensus on the second-order grouping of items; notably, seeking friends' support has previously been considered as an adaptive coping strategy (Patterson & McCubbin, Reference Patterson and McCubbin1987). Therefore, the eight dimensions were also investigated separately to get a clearer picture about the use of different strategies.
General psychopathology was measured through a parent-reported questionnaire: the Child Behavior Checklist (CBCL) or the Adult Behavior Checklist (ABCL) (Achenbach & Rescorla, Reference Achenbach and Rescorla2001, Reference Achenbach and Rescorla2003). The age-normalized T-scores of total psychopathology and externalizing and internalizing subscales were used in the analyses. In a supplementary analysis, the anxious-depressed dimension was also used.
Clinical assessment
A comprehensive clinical assessment was conducted with participants with 22q11DS to examine the presence of DSM diagnoses (see the online Supplementary material). Psychiatric comorbidity was measured as the sum of current psychiatric diagnoses (Sandini et al., Reference Sandini, Chambaz, Schneider, Armando, Zöller, Schaer and Eliez2020). Moreover, the Structured Interview for Psychosis-Risk Syndromes (SIPS) (Miller et al., Reference Miller, McGlashan, Rosen, Somjee, Markovich, Stein and Woods2002) was used to assess (attenuated) positive and negative psychotic symptoms.
The Global Assessment of Functioning (GAF) and the Childhood Global Assessment Scale (CGAS) (Shaffer et al., Reference Shaffer, Gould, Brasic, Ambrosini, Fisher, Bird and Aluwahlia1983) were used as global measures of functioning.
Cognitive assessment
Intellectual functioning was assessed with Wechsler Intelligence Scale for Children (Wechsler, Reference Wechsler2014) or Adults (Wechsler, Reference Wechsler2008).
Statistical analyses
Most of the analyses were conducted using Stata 16 (StataCorp, 2019). The likelihood ratio tests (LRTs) and Spearman rank correlations were conducted in R version 3.6.3 (R Core Team, 2020) using nlme (Pinheiro, Bates, & R Core Team, Reference Pinheiro and Bates2022) and ppcor (Kim, Reference Kim2015) packages. Moreover, potentially influential bivariate outliers based on the Cook's distance (Di > 1.0 or other comparatively large values detected from a graph) were detected using R. The analyses were repeated by removing these outliers, and the results remained unchanged. In the correlation analyses, stress reactivity values >3 s.d. from mean were defined as univariate outliers. Removing outliers, most correlations remained unchanged. Therefore, in the main document, the results from the full sample are reported. Results of the correlations without outliers are reported in an online Supplementary material.
The EMA data have a two-level structure, with repeated measurements (level 1) nested within individuals (level 2). The models were corrected for autocorrelation between residuals using an AR(1) autocorrelation structure.
Group comparisons for non-EMA variables were done using Mann–Whitney U tests or χ2 tests. For time-invariant EMA variables (e.g. % time spent alone) group comparisons were performed using multiple linear regression models. For time-varying EMA variables (e.g. NA), group comparisons were performed using multilevel regression models with random intercepts. For the analyses conducted on the EMA variables, age, gender and EMA period [i.e. period during which each participant took part in the EMA assessment; (1) school/work; (2) holidays; or (3) lockdown due to COVID-19] were included as covariates. Of note, since lower IQ is part of 22q11DS phenotype, we did not use IQ as a covariate in between-group analyses since this would have removed some of the variance inherent to the diagnosis (Dennis et al., Reference Dennis, Francis, Cirino, Schachar, Barnes and Fletcher2009). However, IQ was added as a covariate in the within-group analyses (see below).
To examine associations between stress and NA/momentary psychotic experiences, separate multilevel regression models with random intercepts and random slopes were estimated, with each stress variable as the independent variable and NA/momentary psychotic experiences as the dependent variable using the MIXED command. The stress × group interaction was added to the model to investigate possible group differences in stress reactivity, again controlling for age, gender, and EMA period. To examine whether coping moderated the effect of stress on NA, the score of non-adaptive coping was included into the model. For the CERQ, the non-adaptive coping subscale was used, whereas for the A-COPE, the subscale of avoidance coping as well as all the avoidant strategies were investigated separately. To be able to compare models with different predictors, LRTs using maximum-likelihood (ML) estimation were used to assess model fit for two- (stress × coping) and three-way (stress × coping × group) interactions.
Finally, to examine correlations between stress reactivity and psychopathology in 22q11DS, stress reactivity variables were created calculating momentary-level within-person beta coefficients of the association between stress and NA for each participant (three beta coefficients per participant) (see Kramer et al., Reference Kramer, Simons, Wigman, Collip, Jacobs, Derom and Wichers2014). Social stress reactivity was not calculated for participants if they reported being in a company of others on less than four beeps (n = 4). Moreover, the stress reactivity variables could not be calculated due to collinearity issues for a few participants (social stress, n = 3; activity stress, n = 2; event stress, n = 2). Spearman rank correlations between stress reactivity and psychopathology variables were conducted, controlling for the effects or age, sex, IQ, and EMA period. Multiple comparisons were corrected with Benjamini–Hochberg (B–H) correction (Thissen, Steinberg, & Kuang, Reference Thissen, Steinberg and Kuang2002).
The current study was co-registered during the data collection (https://doi.org/10.17605/OSF.IO/3W4C6; https://doi.org/10.17605/OSF.IO/4V2ZA). Deviations from the co-registration are detailed in the online Supplementary material. The data set is publicly available through the YARETA data preservation system.
Results
Sample characteristics and group differences in demographic variables
From the total sample (n = 95), four participants (two from each group) provided less than 16 valid responses (<33.3% of total number of beeps) and were therefore excluded from the study. The final sample consisted of 91 individuals (n = 38 participants with 22q11DS with 1132 valid responses, n = 53 HC with 1727 valid responses). Due to difficulties in understanding the meaning of questions related to past events, responses for these questions were excluded for one participant with 22q11DS. Detailed information about compliance of valid participants is shown in Table 1. The groups did not differ in terms of compliance, but the 22q11DS group had a significantly longer mean response time than HC. Note that IQ was not significantly associated with compliance rate in participants with 22q11DS (r s(37) = −0.116, p = 0.493).
Characteristics of participants are shown in Table 1. Most demographic variables did not differ between the groups. Compared to HC, participants with 22q11DS had a significantly lower mean IQ, in line with previous literature (De Smedt et al., Reference De Smedt, Devriendt, Fryns, Vogels, Gewillig and Swillen2007). Of note, age or sex was not associated with stress in any context or any of the stress reactivity measures (see the online Supplementary material).
Group differences in EMA measures
Group differences in EMA measures are shown in Table 2. The groups did not significantly differ in the proportion of time spent alone during the period of evaluation. However, participants with 22q11DS reported being less often engaged in work/school-related activities and activities related to social contact compared to HC. On the contrary, participants with 22q11DS reported doing leisure activities more frequently than HC.
Table 2. Group comparisons of EMA measures, controlling for age, sex, and EMA period

*p < 0.05; **p < 0.01.
Levels of positive affects (PA) and NA did not significantly differ between the groups. However, participants with 22q11DS reported higher levels of momentary psychotic experiences than HC.
Participants with 22q11DS reported higher levels of social stress but lower levels of activity stress compared to HC. A supplementary analysis was conducted to investigate whether the global level of functioning was associated with activity-related stress in individuals with 22q11DS, but no significant association was observed [b = 0.004 (95% confidence interval (CI) −0.01 to 0.018), p = 0.533]. Finally, the level of event stress did not significantly differ between the groups.
Affective and psychotic reactivity to stress
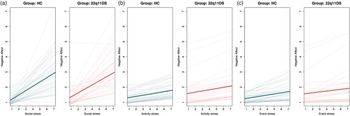
In the entire sample, NA was significantly associated with all stress variables (Table 3). However, the stress × group interaction was not significant for any stress variable, indicating no significant differences in affective reactivity to stress between the two groups (Fig. 1). In the clinical group, a post-hoc analysis investigating the potential impact of selective serotonin reuptake inhibitor (SSRI) medication on stress reactivity was conducted and no impact of medication status was detected (see the online Supplementary material).

Fig. 1. Estimated intercepts and slopes for the two groups of the effect of (a) social stress on NA (n = 53 HC, n = 38 22q11DS), (b) activity stress on NA (n = 53 HC, n = 38 22q11DS, and (c) event stress on NA (n = 53 HC, n = 37 22q11DS).
Table 3. Association of stress with negative affects and psychotic experiences, and the effect of non-adaptive coping in participants with 22q11DS and HC, controlling for age, sex, and EMA period

a LRT with ML estimation for stress × coping × group interaction.
b CERQ: score of CERQ non-adaptive subscale.
c A-COPE: score of A-COPE avoidance subscale.
*p < 0.05; **p< 0.01; ***p < 0.001.
For all participants, the level of momentary psychotic experiences was not associated with stress in any context. Moreover, the stress × group interaction on psychotic experiences was not significant for any stress variable (Table 3).
As the results indicate a link between stress and NA, but not between stress and momentary psychotic experiences, the following analyses were only conducted for the affective reactivity to stress.
Effect of coping strategies
The 22q11DS group reported using less adaptive coping strategies to regulate their emotions but did not differ from HC regarding the use of non-adaptive coping (CERQ) (Table 1). Moreover, when investigating more concrete coping behaviors (A-COPE), several strategies were reported to be used less often by participants with 22q11DS: engaging in demanding activities, positive re-appraisal, ventilating feelings, and searching for friendship. On the other hand, they reported more often seeking family support. The use of other strategies did not significantly differ between the groups.
Examining possible moderating effect of coping on the stress–NA association, LRT showed no evidence that three-way interaction (by adding the group to the interaction) improved the model fit, so the moderating effect of coping was examined for the whole group using a two-way interaction (see Table 3). A-COPE avoidance coping positively moderated the effect of social stress and event stress on NA, but not the effect of activity stress on NA. When examining different strategies separately, a more frequent use of escaping and ventilating feelings moderated the effect of event stress on NA, and ventilating feelings moderated the effect of social stress on NA. Searching for friendship did not have an effect on stress reactivity. Finally, CERQ non-adaptive coping did not moderate the effect of any of the stress variables on NA.
Correlations between affective reactivity to stress and psychopathology
Correlations between stress reactivity and psychopathology variables are illustrated in Fig. 2. Affective reactivity to social stress was significantly associated with the severity of SIPS positive symptoms (r s(30) = 0.505, p = 0.008; B–H threshold = 0.0083). Affective reactivity to social stress was also associated with negative symptoms, but the association did not survive the multiple comparison correction (r s(30) = 0.516, p = 0.007; B–H threshold = 0.0042). Moreover, we observed associations between activity stress reactivity and SIPS positive symptoms (r s(35) = 0.372, p = 0.039; B–H threshold = 0.0042) as well as between event stress reactivity and SIPS negative symptoms (r s(34) = 0.410, p = 0.025; B–H threshold = 0.0042), but they did not survive the B–H correction.

Fig. 2. Spearman rank correlations between stress reactivity and psychopathology variables in the 22q11DS group, after controlling for age, sex, IQ, and EMA period. soc, social stress reactivity; act, activity stress reactivity; eve, event stress reactivity; pos, score of SIPS positive psychotic symptoms; neg, score of SIPS negative symptoms; psytot, score of total psychopathology (ABCL/CBCL); psyint, score of internalizing psychopathology (ABCL/CBCL); psyext, score of externalizing psychopathology (ABCL/CBCL); comorb, number of psychiatric comorbidities.
When investigating associations between affective reactivity to stress and more general psychopathology, we observed that either the number of psychiatric comorbidities or other measures of general psychopathology did not significantly correlate with stress reactivity. Finally, a supplementary analysis showed that anxio-depressive symptoms were not associated with affective reactivity to social (r s(30) = 0.05, p = 0.816), activity-related (r s(35) = −0.14, p = 0.448), or event-related stress (r s(34) = 0.26, p = 0.173).
Discussion
Our results indicate that adolescents and young adults with 22q11DS report higher levels of perceived social stress but lower levels of activity-related stress in their daily lives compared to HC. Contrary to our hypotheses, the 22q11DS group did not show increased affective or psychotic reactivity to daily stressors. However, increased affective reactivity to social stress was associated with more severe psychotic symptoms in the 22q11DS group. Finally, participants with 22q11DS differed from HC on the use of several coping strategies, with a tendency to use less adaptive strategies. The use of avoidance coping moderated the stress–NA association in daily life.
Perceived stress
As expected, due to the high prevalence of social anxiety previously described in the syndrome (Schneider et al., Reference Schneider, Debbané, Bassett, Chow, Fung, van den Bree and Eliez2014), participants with 22q11DS reported higher levels of daily social stress (i.e. their current social context is subjectively experienced as more negative) than HC. The conflicting results with previous findings (Schneider et al., Reference Schneider, Vaessen, van Duin, Kasanova, Viechtbauer, Reininghaus and Myin-Germeys2020) could be explained by age differences between the samples: it is likely that adolescents and young adults report more intense social stress than older adults, knowing that the period of adolescence is particularly susceptible to social evaluation (van den Bos et al., Reference van den Bos, De Rooij, Miers, Bokhorst and Westenberg2014). In the general population, better social skills have been associated with lower stress (Segrin, Hanzal, Donnerstein, Taylor, & Domschke, Reference Segrin, Hanzal, Donnerstein, Taylor and Domschke2007), so social skills deficit in youths with 22q11DS, together with high social anxiety and impaired social cognition (Milic et al., Reference Milic, Feller, Schneider, Debbané and Loeffler-Stastka2021; Schneider et al., Reference Schneider, Debbané, Bassett, Chow, Fung, van den Bree and Eliez2014; Shashi et al., Reference Shashi, Veerapandiyan, Schoch, Kwapil, Keshavan, Ip and Hooper2012), could contribute to a more negative experience of their social interactions. In 22q11DS, high rates of autism spectrum disorders (ASD) and subthreshold autistic symptoms are reported (Vorstman et al., Reference Vorstman, Morcus, Duijff, Klaassen, Heineman-de Boer, Beemer and van Engeland2006), which may contribute to elevated interpersonal stress in daily life. Indeed, a recent study reported high levels of subjective daily-life stress, including social stress, in individuals with ASD (van der Linden et al., Reference van der Linden, Simons, Viechtbauer, Ottenheijm, van Amelsvoort and Marcelis2021). However, it should be noted that in 22q11DS, the findings regarding perceived social stress are not necessarily consistent across samples, potentially pointing toward significant inter-individual variability (Feller, Ilen, Eliez, & Schneider, Reference Feller, Ilen, Eliez and Schneider2022). Indeed, one factor contributing to the intensity of social stress may be the impact of previous, negative social interactions, such as bullying victimization, which is more frequent in youths with special needs, including those with ASD (Blake, Lund, Zhou, Kwok, & Benz, Reference Blake, Lund, Zhou, Kwok and Benz2012; Maiano, Normand, Salvas, Moullec, & Aimé, Reference Maiano, Normand, Salvas, Moullec and Aimé2016). More qualitative investigation of the types of social situations perceived as stressful by youths with 22q11DS is important to provide valuable leads for targeted interventions.
On the contrary, participants with 22q11DS reported lower levels of activity-related stress than HC, which can likely be explained by the different types of activities reported by the groups. Indeed, we observed, in line with earlier results (Schneider et al., Reference Schneider, Vaessen, van Duin, Kasanova, Viechtbauer, Reininghaus and Myin-Germeys2020), that individuals with 22q11DS were less often engaged in activities requiring a certain level of effort (i.e. school/work) or in social contact. The reduced time spent on difficult/unpleasant activities and increased time spent on leisure activities potentially decreases the number of opportunities to experience stressful events in daily life. This could offer an explanation for the current findings of similar levels of event-related stress between groups, challenging previous findings (Schneider et al., Reference Schneider, Vaessen, van Duin, Kasanova, Viechtbauer, Reininghaus and Myin-Germeys2020). It is also possible that the various confinement measures due to the COVID-19 pandemic, during which a proportion of the participants was assessed, explain why some of the youths were less exposed to stressful daily-life events, especially social ones.
Stress reactivity and link with psychopathology
In line with previous literature (Myin-Germeys et al., Reference Myin-Germeys, van Os, Schwartz, Stone and Delespaul2001), we observed a significant increase in NA in relation to stress in all contexts. However, contrary to our hypothesis, the increase was similar for both groups, indicating that adolescents and young adults with 22q11DS did not show increased reactivity to daily-life stress. Our results replicate the previous findings of Schneider et al. (Reference Schneider, Vaessen, van Duin, Kasanova, Viechtbauer, Reininghaus and Myin-Germeys2020), conducted on a sample of adults with 22q11DS. On the other hand, they do not correspond to previous findings of heightened affective or psychotic reactivity to stress in other CHR individuals (van der Steen et al., Reference van der Steen, Gimpel-Drees, Lataster, Viechtbauer, Simons, Lardinois and Myin-Germeys2017), and are not consistent with previous indirect findings of HPA-axis dysregulation in 22q11DS in children or adult samples, possibly suggesting altered stress reactivity (Armando et al., Reference Armando, Sandini, Chambaz, Schaer, Schneider and Eliez2018; Jacobson et al., Reference Jacobson, Bursch and Lajiness-O'Neill2016; Sanders et al., Reference Sanders, Hobbs, Stephenson, Laird and Beaton2017; Sandini et al., Reference Sandini, Chambaz, Schneider, Armando, Zöller, Schaer and Eliez2020; van Duin et al., Reference van Duin, Vaessen, Kasanova, Viechtbauer, Reininghaus, Saalbrink and Myin-Germeys2019). In adolescents and young adults, we recently showed no evidence of altered daily cortisol in 22q11DS (Ilen et al., Reference Ilen, Feller, Eliez, Micol, Delavari, Sandi and Schneider2022). The mixed findings could possibly be explained by high inter-individual variability within individuals with 22q11DS. In the current study, we effectively observed a relatively high variation in affective reactivity to stress within the 22q11DS group, which could indicate increased stress reactivity in a subgroup of participants. Therefore, inter-individual variability in stress reactivity should be further investigated in youths with 22q11DS, also through physiological measures, to draw stronger conclusions.
A potential explanation for the inter-individual differences in stress reactivity could be the use of medication. For instance, earlier literature has shown the efficacy of long-term SSRI treatment in reducing cortisol reactivity to stress in chronic post-traumatic stress disorder (PTSD) (Vermetten et al., Reference Vermetten, Vythilingam, Schmahl, De Kloet, Southwick, Charney and Bremner2006). Positive effects of SSRIs on cognition and brain development have also recently been shown in youths with 22q11DS (Mancini et al., Reference Mancini, Maeder, Bortolin, Schneider, Schaer and Eliez2021). In our study, participants with SSRI medication at the time of testing did not differ from those without SSRIs in terms of affective reactivity to stress, even when dose equivalent and duration of treatment were added as covariates. However, the subsample of participants treated with SSRIs was quite small, so it would be interesting to further study the impact of medication, including SSRIs, on stress reactivity and, eventually, on the risk for psychopathology in vulnerable populations with a larger sample size. Another possible factor explaining inter-individual differences in stress reactivity could be the exposure to (early-life) stress or trauma, as higher levels of childhood trauma have been associated with increased stress reactivity in other vulnerable populations (Paetzold et al., Reference Paetzold, Myin-Germeys, Schick, Nelson, Velthorst, Schirmbeck and Reininghaus2021; Rauschenberg et al., Reference Rauschenberg, Van Os, Cremers, Goedhart, Schieveld and Reininghaus2017). It is thought that individuals with 22q11DS are more frequently exposed to stress than their peers, due to the different challenges (e.g. medical, cognitive, and social) that they may face from childhood onward (Beaton & Simon, Reference Beaton and Simon2011). In particular, 22q11DS is associated with various medical issues, including congenital heart disease, palatal abnormalities, and immunodeficiency (Swillen & McDonald-McGinn, Reference Swillen and McDonald-McGinn2015), and medical procedures could be important sources of stress for certain children with 22q11DS. The role of stressful and traumatic life events in stress reactivity in 22q11DS is worth exploring in future studies.
Inter-individual differences in stress reactivity are potentially important to determine which individuals are more prone to develop mental health issues and psychosis in general. Increased reactivity to momentary stress is thought to be a mechanism that can lead to persistent ‘macro-level’ symptoms and heighten the risk of a transition to mental health issues (Collip et al., Reference Collip, Wigman, Myin-Germeys, Jacobs, Derom, Thiery and van Os2013; Vaessen et al., Reference Vaessen, van Nierop, Decoster, Delespaul, Derom, De Hert and Thiery2017). At the cross-sectional level, we indeed observed an association between increased affective reactivity to social stressors at the momentary level and more severe (‘macro-level’) psychotic symptoms. The association was notably significant for positive symptoms of psychosis, in line with earlier findings in individuals with psychosis (Lataster, Valmaggia, Lardinois, van Os, & Myin-Germeys, Reference Lataster, Valmaggia, Lardinois, van Os and Myin-Germeys2013). This is the first study to demonstrate an association between social stress reactivity and psychotic symptoms in 22q11DS, even though social stress has previously been linked with more severe psychotic symptoms in other CHR populations (Millman et al., Reference Millman, Pitts, Thompson, Kline, Demro, Weintraub and Schiffman2018; Veling, Pot-Kolder, Counotte, van Os, & van der Gaag, Reference Veling, Pot-Kolder, Counotte, van Os and van der Gaag2016) and elevated (social) stress reactivity has been associated with increased momentary psychotic experiences in early psychosis (Reininghaus et al., Reference Reininghaus, Kempton, Valmaggia, Craig, Garety, Onyejiaka and Morgan2016). Altogether, it suggests that increased stress sensitivity over long periods of time could create a snowball effect on the development of mental health symptoms: heightened moment-to-moment reactivity to stress might increase the vulnerability for developing psychotic symptoms and ultimately psychosis in vulnerable individuals, such as youths with 22q11DS. However, this remains hypothetical, as we used a cross-sectional design, and the causal relationship between stress reactivity and psychopathology was not investigated.
Although our results show more severe symptoms in youths with 22q11DS who are more reactive to stress, stress does not appear to increase momentary psychotic experiences in daily life (given the lack of association between stress and psychotic experiences measured through EMA). It is possible that a direct link between stress and momentary psychotic experiences could be observed in people who are more symptomatic, and that our results would therefore be explained by the fact that most of our participants neither had psychosis or CHR. Moreover, although only two participants with 22q11DS had a diagnosis of psychotic disorder, several participants used an antipsychotic medication to treat psychotic symptoms or anxiety. As the treatment likely attenuates the intensity of symptoms, it is possible that it partially explains the lack of relationship between stress and momentary psychotic experiences.
Coping strategies
Interestingly, we replicated earlier findings (Armando et al., Reference Armando, Sandini, Chambaz, Schaer, Schneider and Eliez2018) regarding the reduced use of adaptive coping in 22q11DS using the CERQ, which measures more abstract emotion regulation strategies. Some differences also emerged on the A-COPE questionnaire, which measures more concrete coping behaviors, such as a lower use of positive re-appraisal or engagement in demanding activities. In terms of non-adaptive strategies, youths with 22q11DS reported ‘escaping’ from their problems less often than HC, which could be explained by the fact that most of the behaviors that were considered as ‘escaping’ were linked with alcohol/tobacco consumption or spending time with a boyfriend/girlfriend, which is less frequent in youths with 22q11DS compared to HC (Feller et al., Reference Feller, Ilen, Eliez and Schneider2022; Vingerhoets et al., Reference Vingerhoets, van Oudenaren, Bloemen, Boot, van Duin, Evers and van Amelsvoort2019).
We also observed that a more frequent use of strategies that are considered as avoidant (i.e. escaping, ventilating feelings) heightened the affective response to daily-life stressors. Similar findings were not observed for the third strategy ‘searching for friendships’, probably because this type of behavior can be less clearly considered as an avoidance coping strategy and can also be seen as an adaptive way to cope with stressors (Patterson & McCubbin, Reference Patterson and McCubbin1987). Even though avoidance can have a short-term impact on decreasing distress, it has been shown to have negative consequences in the long run, such as an increase in NA or social withdrawal (Werner & Gross, Reference Werner, Gross, Kring and Sloan2010). Avoidance is also associated with psychopathology, including depression and anxiety (Compas et al., Reference Compas, Jaser, Bettis, Watson, Gruhn, Dunbar and Thigpen2017). Therefore, considering the current results together with previous findings showing that maladaptive coping mediates the association between stress and psychotic symptoms in 22q11DS (Armando et al., Reference Armando, Sandini, Chambaz, Schaer, Schneider and Eliez2018), one could tentatively suggest that the use of maladaptive and avoidant coping strategies might increase the risk for psychosis in this vulnerable population through an increase in affective reactivity. In our study, the moderating effect of coping was not specific to the 22q11DS group, indicating that adolescents and young adults in general could likely benefit from using more adaptive coping skills to minimize the impact of daily stressors on negative affective states. However, specific interventions targeting vulnerable youths might be particularly important to implement in order to prevent negative clinical outcomes. These interventions could focus on reducing avoidance through cognitive-behavioral techniques such as exposure, developing more adaptive strategies (e.g. cognitive reappraisal), mindfulness, or practicing acceptance (Werner & Gross, Reference Werner, Gross, Kring and Sloan2010).
Limitations and future directions
Some methodological limitations should be considered. First of all, the EMA assessment is based on a subjective evaluation of participants and interpretation of items can somewhat differ between persons. Moreover, even though EMA has been used with individuals with mild to moderate intellectual deficit (Wilson et al., Reference Wilson, Chen, Mahoney, Buchanan, Marks and Cordier2020), we cannot neglect the fact that understanding certain EMA items could have been difficult to some participants with 22q11DS, especially if they had an intellectual disability. However, to avoid problems related to comprehension or different interpretation of items, all the questions were extensively reviewed with participants during the installation of application.
Furthermore, as the data were collected at a single time point, we were not able to do interpretations regarding the directionality of the stress–NA associations. Future studies could use time-lagged analyses to better understand the causal relationship of stress and affective states. Furthermore, the current study only examined the link between stress reactivity and psychotic symptoms in a cross-sectional way, and longitudinal follow-up of participants would be needed to investigate whether stress reactivity can predict the emergence of psychotic symptoms.
Finally, the use of coping strategies was not assessed at a momentary level (contrary to stress and NA), but at a more general level, which does not offer direct information about the use of specific coping strategies when confronted with stressors in daily-life context. Moreover, as the self-reported questionnaires required evaluating how often in general the youths used different strategies, possible memory or reasoning difficulties may have affected the results more than in the EMA assessment. A limitation of the A-COPE is that the factor-structure of coping styles has been operationalized differently across studies (Forns et al., Reference Forns, Kirchner, Peró, Pont, Abad, Soler and Paretilla2013). To investigate more direct links between momentary stress, coping, and NA in daily life, the use of coping strategies should also be assessed using EMA.
Conclusions
The results of the current study suggest an increased vulnerability for daily social stress in youths with 22q11DS, which could be linked with social anxiety and social impairments associated with the syndrome and should be qualitatively examined to target specific interventions. Furthermore, our results link heightened affective reactivity to social stress with elevated psychotic symptom severity. Given the high risk for psychosis in 22q11DS, interventions should focus on reducing social stress and developing adaptive coping strategies.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291722004019
Acknowledgments
We would like to warmly thank all the participants for their participation and commitment, as well as the family associations Connect22, Génération 22, Relais 22, and 22q11Europe for their ongoing support. We also thank Charlotte Dubois and Eva Micol for their help in data collection.
Author contributions
Formal analysis: Laura Ilen. Investigation: Laura Ilen, Clémence Feller, Stephan Eliez, and Maude Schneider. Methodology and supervision: Maude Schneider. Writing – original draft: Laura Ilen. Writing – review and editing: Laura Ilen, Maude Schneider, Clémence Feller, and Stephan Eliez.
Financial support
This work was supported by an Ambizione grant from the Swiss National Science Foundation to MS (PZ00P1_174206), a research grant from the Swiss National Science Foundation to SE (320030_179404), and a grant from the National Center of Competence in Research (NCCR) ‘Synapsy-The Synaptic Bases of Mental Diseases’ (51NF40-185897).
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The study was approved by the Cantonal Research Ethics Committee of Geneva (CCER).