Introduction
Dissociative seizures (DS) are considered a paroxysmal presentation of functional neurological symptom disorder (as conceptualized in DSM-5) (Lesser, Reference Lesser1996; Reuber, Reference Reuber2008; American Psychiatric Association 2022). We previously described a cognitive behavioral model of DS which assumes that, while different stressors may trigger symptoms of dissociation which resemble seizures, a range of emotional, behavioral and cognitive responses perpetuate them (Chalder, Reference Chalder1996; Goldstein, LaFrance Jr, Mellers, & Chalder, Reference Goldstein, LaFrance, Mellers, Chalder, LaFrance Jnr and Schachter2018). Cognitive and behavioral factors such as fear of having a seizure lead to marked avoidance behavior and precaution taking. Indeed, adults with DS have been shown to have raised levels of agoraphobic avoidance compared to people with epilepsy, a common differential diagnosis (Goldstein & Mellers, Reference Goldstein and Mellers2006). As well as behavioral avoidance, there is some evidence for emotional or experiential avoidance in people with DS (Dimaro et al., Reference Dimaro, Dawson, Roberts, Brown, Moghaddam and Reuber2014; Myers, Gray, Roberts, Levita, & Reuber, Reference Myers, Gray, Roberts, Levita and Reuber2022; Pick, Mellers, & Goldstein, Reference Pick, Mellers and Goldstein2016). People with DS report more emotional regulation deficits than controls and specifically conceal or suppress their emotions more than healthy volunteers (Krámská, Hrešková, Vojtěch, Krámský, & Myers, Reference Krámská, Hrešková, Vojtěch, Krámský and Myers2020; Novakova, Howlett, Barker, & Reuber, Reference Novakova, Howlett, Barker and Reuber2015; Urbanek, Harvey, McGowan, & Agrawal, Reference Urbanek, Harvey, McGowan and Agrawal2014).
In cognitive behavioral models of functional somatic symptoms, beliefs about the unacceptability of negative emotions may result in people trying to hide or control their feelings leading to the development of clinical problems (Rimes & Chalder, Reference Rimes and Chalder2010). Paradoxically, this causes or increases distress and somatic symptoms of arousal, which may not be recognized as such (Wenzlaff & Wegner, Reference Wenzlaff and Wegner2000). In addition, this can lead to safety behaviors such as social avoidance. In a previous randomized controlled trial comparing cognitive behavior therapy (CBT) with counseling for persistent fatigue, we found the main predictor of a better outcome, irrespective of treatment, was the ability of patients to express, acknowledge and accept emotional distress (Godfrey, Chaider, Ridsdale, Seed, & Ogden, Reference Godfrey, Chaider, Ridsdale, Seed and Ogden2007). Arguably, in DS, changing patients' beliefs about the acceptability of expressing emotion could be one of the key processes in determining a good outcome.
The CODES trial
We compared the effectiveness of DS-specific CBT plus standardized medical care (SMC) with SMC alone in the CODES (COgnitive behavior therapy v. standardized medical care for adults with Dissociative non-Epileptic Seizures) trial (Goldstein et al., Reference Goldstein, Mellers, Landau, Stone, Carson, Medford and Chalder2015). We found significant improvements following DS-CBT plus SMC compared to SMC alone in 9/16 secondary measures but not in the primary outcome, which was monthly DS frequency, at 12 months.
The DS-CBT group rated their DS as less bothersome, they had a longer period of DS freedom in the previous six months, reported better health-related quality of life, less impairment in psychosocial functioning on the Work and Social Adjustment Scale, less overall psychological distress and fewer somatic symptoms than the SMC group. Clinical improvement at 12 months was also greater in the DS-CBT group as reported by patients and clinicians. In a secondary analysis, we found that at six months, which broadly coincided with the completion of DS-CBT, the DS-CBT plus SMC group was superior on all outcomes (including DS frequency) except the physical component summary (PCS) score of the SF-12v2, with moderate to large effect sizes (Goldstein et al., Reference Goldstein, Robinson, Chalder, Reuber, Medford, Stone and Landau2022a). In this paper we turn our attention to how treatment worked by examining potential mediators.
Mechanisms of change
Previous studies for DS treatments have not explored mechanisms of change. An understanding of the mechanisms that led to the treatment effects in the CODES trial could elucidate whether DS-specific CBT improved outcomes by changing key processes that were targeted in therapy. It might also guide further intervention development. We assessed putative mediators at baseline, six and 12 months (Goldstein et al., Reference Goldstein, Mellers, Landau, Stone, Carson, Medford and Chalder2015). Mediators are factors in clinical trials that help to explain how and why treatment works. They need to be distinguished from moderators which describe ‘who’ and under what circumstances some people improve. Based on our specific model of DS (Chalder, Reference Chalder1996; Goldstein et al., Reference Goldstein, Mellers, Landau, Stone, Carson, Medford and Chalder2015, Reference Goldstein, LaFrance, Mellers, Chalder, LaFrance Jnr and Schachter2018, Reference Goldstein, Robinson, Pilecka, Perdue, Mosweu, Read and Chalder2021b) and the evidence for the role of emotional avoidance in functional symptoms and DS specifically, we hypothesized that beliefs about emotions (believing it is unacceptable to express negative emotions) would mediate the treatment effect. Given that avoidance is at the heart of most cognitive behavioral models and commonly central to the clinical picture of DS, we also hypothesized that avoidance of people, places, and situations would mediate the treatment effect. As the prevalence of anxiety and depression in people with DS is high (Brown & Reuber, Reference Brown and Reuber2016) and because the targeted treatment processes are key to reducing anxiety and depression, we also hypothesized that change in anxiety and depression would mediate the treatment effect.
In this paper we utilize data collected in the CODES trial (Goldstein et al., Reference Goldstein, Mellers, Landau, Stone, Carson, Medford and Chalder2015) to undertake mediation analyses to investigate whether the mechanisms hypothesized to bring about improvements in DS outcomes after DS-CBT can be shown to operate. We follow guidelines for reporting mediation analyses of randomized trials (Lee et al., Reference Lee, Cashin, Lamb, Hopewell, Vansteelandt and VanderWeele2021). In essence a mediation analysis assesses three aspects of the theory underlying the intervention development: (i) An action theory suggests that the intervention can improve the target variables. This can be empirically assessed by estimating the effect of the intervention on the putative mediator variable, known as the action effect. If there is evidence to support that the intervention has successfully induced change in the mediators, then the treatment can be considered to effectively target what was intended in the development of that treatment. (ii) A conceptual theory suggests that there is a causal link between variables targeted by the intervention and the clinical outcome. This can be empirically confirmed by estimating the causal effect of the putative mediator on the outcome, known as the conceptual effect. If there is evidence to support that change in the mediator causes a change in the outcome, then the conceptual mechanism of change holds. (iii) Finally, the presence of mediation, that is the intervention improving patient outcomes by changing the targeted intermediate variable, can be formally assessed by estimating the mediated or indirect effect of the intervention. We apply these principles to address the following three research questions:
(i) Does DS-CBT affect the proposed mediators at six months follow-up (broadly corresponding to end of treatment) when compared to SMC (i.e. is there evidence for the action path)?
(ii) Which of the putative mediators at six months had a mechanistic effect on outcomes at 12 months (i.e. is there evidence for the conceptual path)?
(iii) How much of the total effect of DS-CBT on outcomes at 12 months is transmitted by the hypothesized mediators (i.e. how large is the indirect effect?)
Methods
This is a planned secondary mediation analysis using the primary and secondary outcome measures and putative mediators of CODES comparing DS-CBT plus SMC to SMC alone for patients with DS. We previously compared the effectiveness of DS-specific CBT plus SMC with SMC alone (Goldstein et al., Reference Goldstein, Mellers, Landau, Stone, Carson, Medford and Chalder2015).
Study design and participants
The trial protocol (Goldstein et al., Reference Goldstein, Mellers, Landau, Stone, Carson, Medford and Chalder2015), 12-month follow-up outcomes (Goldstein et al., Reference Goldstein, Robinson, Mellers, Stone, Carson and Reuber2020, Reference Goldstein, Robinson, Pilecka, Perdue, Mosweu, Read and Chalder2021b), secondary analyses of post-treatment (six-month) outcomes (Goldstein et al., Reference Goldstein, Robinson, Chalder, Reuber, Medford, Stone and Landau2022a) in addition to their moderators and predictors (Goldstein et al., Reference Goldstein, Robinson, Chalder, Stone, Reuber, Medford and Landau2022b) have been published. Between October 2014 and February 2017, 698 people were initially recruited to the study (Goldstein et al., Reference Goldstein, Robinson, Pilecka, Perdue, Mosweu, Read and Chalder2021b). Between January 2015 and May 2017, we randomly assigned 368 patients to SMC alone (n = 182) or DS-CBT plus SMC (n = 186). Participants were recruited from the UK National Health Service. Inclusion and exclusion criteria for the CODES study have been described elsewhere (Goldstein et al., Reference Goldstein, Mellers, Landau, Stone, Carson, Medford and Chalder2015, Reference Goldstein, Robinson, Pilecka, Perdue, Mosweu, Read and Chalder2021b).
Interventions
SMC
SMC was initially delivered by neurologists or epilepsy specialists. They offered patients a diagnosis and explanation for their seizures, supervised the withdrawal of anti-seizure medications where appropriate, treated co-morbid physical problems and assessed for major psychiatric risk. Approximately three months later liaison or neuropsychiatrists assessed the patients and treated patients with pharmacotherapy if indicated. They were asked to refrain from offering CBT themselves due to the study design whereby participants were randomized to either SMC alone or DS-CBT plus SMC.
DS-CBT
Twelve sessions plus one additional session of DS-specific, manualized CBT were offered in person or occasionally by telephone to patients with DS. Therapists delivering DS-CBT were qualified CBT therapists. They had additional specialist training in DS-CBT over three days. Supervision was provided by therapists experienced in treating DS. DS-CBT was based on a theoretical model; although individualized and formulation based, it focused on seizure control techniques, exposure to avoidances, dealing with unhelpful cognitions and facilitating emotional processing (Goldstein et al., Reference Goldstein, Robinson, Pilecka, Perdue, Mosweu, Read and Chalder2021b). Therapy fidelity was acceptable (Goldstein et al., Reference Goldstein, Robinson, Mellers, Stone, Carson and Reuber2020, Reference Goldstein, Robinson, Pilecka, Perdue, Mosweu, Read and Chalder2021b). The intervention techniques used to address cognitive, behavioral, and emotional aspects of DS targeted in our DS-CBT are illustrated in Fig. 1.
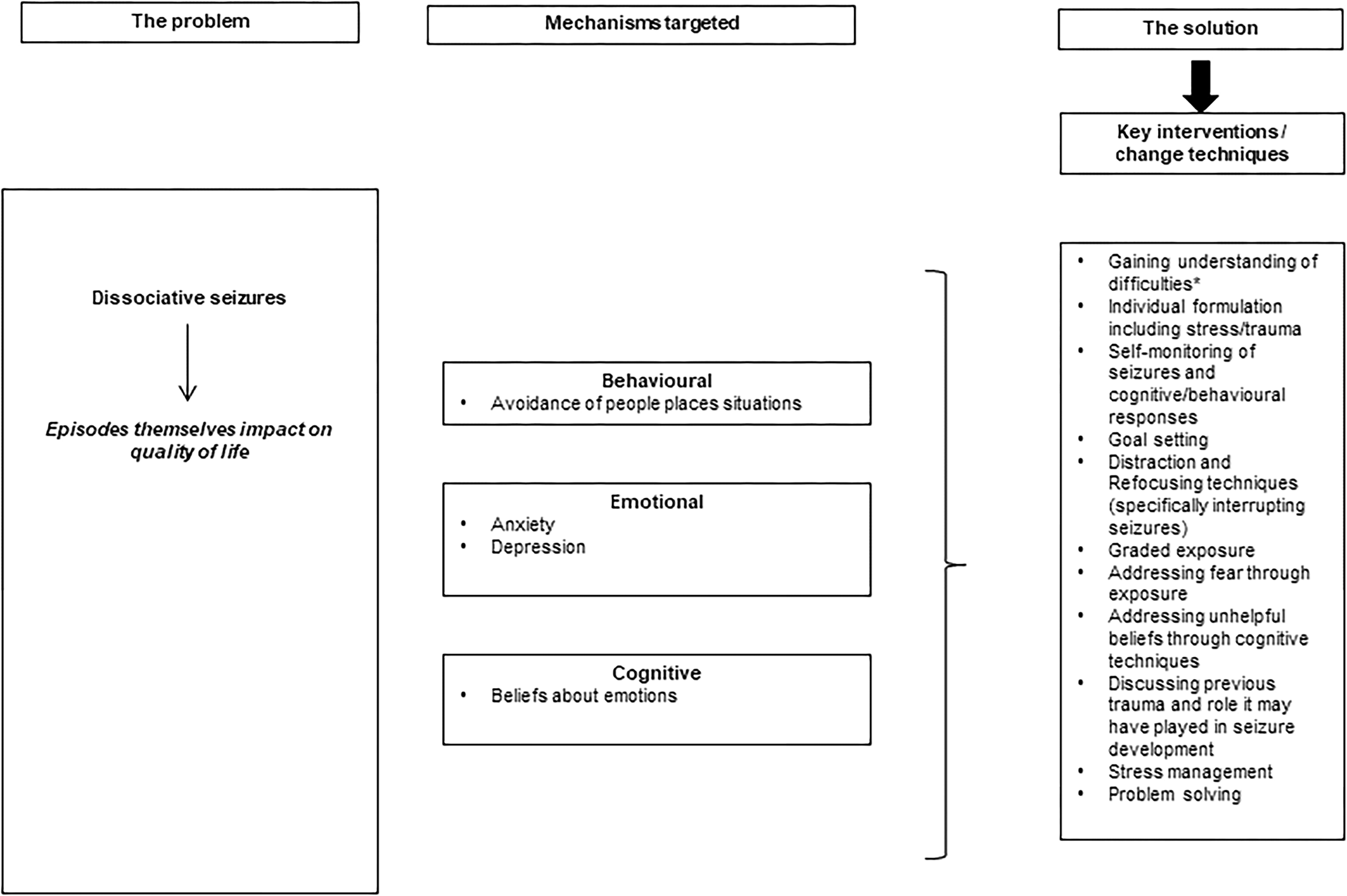
Figure 1. LOGIC model: mechanisms and interventions.
*Gaining understanding of difficulties including patterns of seizure occurrence.
This figure is adapted with permission from Goldstein et al. (Reference Goldstein, Robinson, Pilecka, Perdue, Mosweu, Read and Chalder2021b). This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The current figure includes formatting changes from the original figure and focuses on a subset of targeted mechanisms.
Description of the mediation model
Figure 2 shows our mediation model in relation to CODES. We show the pathways between our intervention, DS-CBT plus SMC, the putative mediators and our outcomes of interest.

Figure 2. Mediation models showing putative mediators, outcomes, and pathways.
All of the putative mediators are presented in this figure. Each mediator pathway was tested in a separate model.
Outcome measures
We chose the same outcomes employed in our previously published moderator and predictor analyses (Goldstein et al., Reference Goldstein, Robinson, Chalder, Stone, Reuber, Medford and Landau2022b). We included the primary outcome, DS frequency over the previous four-week period at 12 months post randomization derived from self-report diaries or questionnaire (Goldstein et al., Reference Goldstein, Robinson, Mellers, Stone, Carson and Reuber2020, Reference Goldstein, Robinson, Pilecka, Perdue, Mosweu, Read and Chalder2021b). We also chose the Work and Social Adjustment Scale (WSAS), a five-item scale assessing participation in work, home management, social and private leisure activities and relationships (Mundt, Marks, Shear, & Greist, Reference Mundt, Marks, Shear and Greist2002). Finally, we used the mental component summary (MCS) and the PCS score from the SF-12v2 (Ware, Kosinski, Turner-Bowker, & Gandek, Reference Ware, Kosinski, Turner-Bowker and Gandek2002). The MCS includes items related to the vitality, social functioning, role emotion, and mental health domains. The PCS includes items related to the pain, general health role-physical health domains. All standardized outcome measures are reliable and valid (Cheak-Zamora, Wyrwich, & McBride, Reference Cheak-Zamora, Wyrwich and McBride2009; Mundt et al., Reference Mundt, Marks, Shear and Greist2002). The rationale for choosing measures related to impact on life was because although symptoms are important, it is the effect that symptoms have that is key, not the symptoms themselves. This philosophy is at the heart of third wave psychotherapies (Hayes, Luoma, Bond, Masuda, & Lillis, Reference Hayes, Luoma, Bond, Masuda and Lillis2006).
Putative mediators
Avoidance behavior: The Avoidance of People, Places, Situations (APPS) three-item scale was devised specifically for the CODES study (Goldstein et al., Reference Goldstein, Robinson, Mellers, Stone, Carson and Chalder2021a). Items asked ‘How much have you avoided other people for fear of having a seizure?’ ‘How much have you avoided specific activities (e.g. physical exertion, bathing unsupervised) for fear of having a seizure?’ and ‘How much have you avoided specific situations (e.g. being out in public alone, social gatherings, using public transport) for fear of having a seizure?’ Response options were on a scale from 0 (‘never avoid’) to 10 (‘always avoid’). The total possible score was 30; Cronbach's α = 0.83 at baseline (Goldstein et al., Reference Goldstein, Robinson, Mellers, Stone, Carson and Chalder2021a).
Beliefs about Emotions: The Beliefs about Emotions (BES) scale (Rimes & Chalder, Reference Rimes and Chalder2010) assesses beliefs such as ‘it is a sign of weakness if I have miserable thoughts’ and ‘it would be a sign of weakness to show my emotions in public’. It has 12 items. Response options include 6 = ‘Totally agree’, 5 = ‘Agree very much’, 4 = ‘Agree slightly’, 3 = ‘Neutral’, 2 = ‘Disagree slightly’, 1 = ‘Disagree very much’ and 0 = ‘Totally disagree’. The scale is reliable and valid. In this study Cronbach's α was 0.92.
The Generalized Anxiety Disorder Assessment 7-item scale (GAD-7; Spitzer, Kroenke, Williams, and Lowe, Reference Spitzer, Kroenke, Williams and Lowe2006) was used to assess generalized anxiety disorder and the nine-item Patient Health Questionnaire (PHQ-9; Kroenke and Spitzer, Reference Kroenke and Spitzer2002) was used to assess depression. Higher scores indicate worse distress. Using data from the CODES trial, we found the PHQ-9 to be highly reliable with high diagnostic accuracy against the Mini-International Neuropsychiatric Interview (M.I.N.I.; Sheehan et al., Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs, Weiller and Dunbar1998) (Baldellou Lopez et al., Reference Baldellou Lopez, Goldstein, Robinson, Vitoratou, Chalder, Carson and Reuber2021). Internal consistency for the GAD-7 was high in people with DS and validity was good (Goldstein et al., Reference Goldstein, Vitoratou, Stone, Chalder, Baldellou Lopez, Carson and Reuber2023).
Confounders of the mediator-outcome relationship
While confounding does not affect the estimate of the total DS-CBT effect due to randomization in the CODES trial, when carrying out a mediation analysis, confounding of the mediator-outcome path can occur. We considered the following baseline variables as confounders of this relationship: We recorded age just prior to randomization to the CODES RCT and self-reported gender. We also used a categorization of whether people had ⩾1 current M.I.N.I.-confirmed co-morbid psychiatric diagnosis just prior to randomization.
Statistical analysis
We undertook formal causal mediation analyses to investigate whether each of the four hypothesized mediators (at six months post randomization) was on the causal pathway from DS-CBT to one of the four important outcomes (at 12 months). We considered each mediator-outcome combination in a set of 16 single mediator models. We assumed parametric linear mixed models for continuous mediator and outcome variables and constant mediator effects across trial arms. The linear mixed models contained baseline values of the mediator and the outcome as covariates to adjust for potential confounding (Landau, Emsley, & Dunn, Reference Landau, Emsley and Dunn2018) as well as age, gender and presence of a psychiatric diagnosis at baseline. Consistent with the modeling approach used previously (Goldstein et al., Reference Goldstein, Robinson, Mellers, Stone, Carson and Reuber2020, Reference Goldstein, Robinson, Chalder, Reuber, Medford, Stone and Landau2022a) the models for the mediator and the outcome further contained trial arm as a fixed effect and randomization stratifier (the 17 psychiatry sites from which participants were recruited) as random intercepts. The model for the outcome further included the mediator under investigation. Under this parameterization the regression coefficient of trial arm in the mediator model represents the action effect of DS-CBT on the respective mediator and the coefficient of the mediator in the outcome model the conceptual effect of the respective mediator-outcome relationship. In addition, the natural indirect effect – which we will estimate to assess the amount of mediation – is the product of the action and conceptual effects. We handle missing values in the mediator or outcome variable under a missing at random (MAR) assumption, that is observed variables were allowed to drive missingness.
Models were fitted by combining parametric mediation modeling via quasi-Bayesian Monte Carlo simulation with multiple imputation (MI; Imai, Keele, and Tingley, Reference Imai, Keele and Tingley2010). Missing values in the six-month mediator and the 12 month-outcome were multiply imputed using Multivariate Imputation by Chained Equations in Stata (MICE; van Buuren, Reference van Buuren2007). To ensure that the respective imputation models were more general than the analysis models and adjusted for missing data biases they included the following variables: All the variables of the respective mediator and outcome models, dummy variables for psychiatry sites, variables previously found to predict missingness (non-compliance with DS-CBT and five baseline variables, see Goldstein et al., Reference Goldstein, Robinson, Mellers, Stone, Carson and Reuber2020, Reference Goldstein, Robinson, Pilecka, Perdue, Mosweu, Read and Chalder2021b) and additional measurements of the mediator variable at 12 months and the outcome variable at six months. Specifically, we created 100 imputed data sets for each mediator-outcome combination in Stata 15, read these into R version 4.1.1 and used the mediations and amelidiate functions of the mediation package (1000 Monte Carlo simulations per imputed data set: Tingley, Yamamoto, Hirose, Keele, and Imai, Reference Tingley, Yamamoto, Hirose, Keele and Imai2014) to construct 95% percentile intervals for the natural direct and indirect effects.
In the results section we present estimates of action effects, conceptual effects and indirect effects. Total DS-CBT effects quoted are MI estimates derived in Stata from outcome models that exclude mediator variables and potential confounding variables for consistency with our original analyses (Goldstein et al., Reference Goldstein, Robinson, Mellers, Stone, Carson and Reuber2020). Similarly, the action effect estimates quoted are MI estimates derived from mediator models that exclude outcome variables and potential confounding variables (Goldstein et al., Reference Goldstein, Robinson, Chalder, Reuber, Medford, Stone and Landau2022a). Finally, the conceptual effects quoted are MI estimates of the regression coefficient of the mediator in the outcome model derived in Stata 15.
Results
Of the 368 adults studied here, 266 (72%) were self-reported women. Median age of the overall sample was 35 years and the median age when DS had first occurred was 29 years (IQR 19, 42). The median duration of participants' DS disorder prior to receiving their diagnosis in the CODES trial was 3 years (IQR 1, 8). Nearly two-thirds of the sample (241; 65%) indicated having previously sought help for a mental health problem. The most commonly M.I.N.I-identified co-morbid diagnoses were agoraphobia (45%), major depressive disorder (31%), generalized anxiety disorder (29%), posttraumatic stress disorder (23%) and social anxiety disorder (20%) (Goldstein et al., Reference Goldstein, Robinson, Mellers, Stone, Carson and Chalder2021a, Reference Goldstein, Robinson, Pilecka, Perdue, Mosweu, Read and Chalder2021b); the median number of current M.I.N.I diagnoses was 2 (range 0–8). Further information about the sample is reported elsewhere (Goldstein et al., Reference Goldstein, Robinson, Mellers, Stone, Carson and Reuber2020, Reference Goldstein, Robinson, Mellers, Stone, Carson and Chalder2021a, Reference Goldstein, Robinson, Pilecka, Perdue, Mosweu, Read and Chalder2021b).
The 12-month outcome variables considered here were previously summarized (Goldstein et al., Reference Goldstein, Robinson, Mellers, Stone, Carson and Reuber2020), as were two of the four putative mediator variables considered here (GAD-7 and PHQ-9; Goldstein et al., Reference Goldstein, Robinson, Chalder, Reuber, Medford, Stone and Landau2022a). At 12 months 85%, 80%, 80% and 80% of participants provided outcome data for seizure frequency, WSAS, SF-12v2 PCS and SF-12v2 MCS respectively. Attrition was slightly higher at six months with mediator variables avoidance, Beliefs about Emotions, GAD-7 and PHQ-9 being available for 75% of the trial sample. Thus, there was the potential for missing data biases to operate, which we attempted to minimize using MI.
Does DS-CBT affect the proposed mediators when compared to SMC?
Figure 3 shows mean mediator values by trial arm and observation time point. It appears that for avoidance behavior, GAD-7 and PHQ-9 mean values in the DS-CBT plus SMC arm reduce more over the first six months of therapy than values in the SMC arm. In contrast, time trajectories for BES appear similar in both arms.

Figure 3. Change in putative mediators over time and by trial arm. Symbols represent group means (circles indicating SMC and triangles indicating DS-CBT plus SMC) and error bars are 95% CIs for means.
For the APPS, a higher score indicates greater avoidance behavior. For the BES, a higher score indicates a greater belief that it is unacceptable to express negative emotion. For the GAD-7 a higher score indicates higher anxiety and for the PHQ-9 a higher score indicates greater depression.
This figure is adapted with permission from Goldstein et al. (Reference Goldstein, Robinson, Mellers, Stone, Carson and Reuber2020). This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited.
See: http://creativecommons.org/licenses/by/4.0/. The current figure includes formatting changes from the original figure and the addition of data plots for the APPS and BES.
Table 1 provides formal estimates of the action effects of DS-CBT on each of the putative mediator variables. For avoidance behavior (−0.40 baseline standard deviations, p < 0.001), GAD-7 (−0.35, p < 0.001) and PHQ-9 (−0.26, p = 0.004) allocation to the DS-CBT plus SMC arm led to a significant reduction in scores at six months relative to SMC alone. The amount of relative change induced in these target variables was small to moderate (standardized differences 0.25-0.5). In contrast, there was no evidence that DS-CBT brought about change in BES scores at six months (−0.072, p = 0.52).
Table 1. Estimated standardized effect sizes and 95% CIs for action effects, conceptual effects, and natural indirect effects

Effect size estimates that are statistically significant at the 5% test level are shown in bold. Estimates of conceptual effects, and direct and indirect effects are adjusted for age, gender and co-morbid psychiatric diagnosis.
a Standardized effect sizes as per analyses presented in Goldstein et al. (Reference Goldstein, Robinson, Chalder, Reuber, Medford, Stone and Landau2022).
b Total effect estimates used in the decomposition can vary from the total effect estimates produced in Goldstein et al. (Reference Goldstein, Robinson, Mellers, Stone, Carson and Reuber2020) due to extra adjustments for mediator baseline variable and mediator-outcome path confounders, and due to mediator-specific imputations.
c Standardized effect sizes as per analyses presented in Goldstein et al. (Reference Goldstein, Robinson, Mellers, Stone, Carson and Reuber2020).
+ Confidence intervals for direct and indirect effects are constructed by simulation (percentile intervals). p values for these effects were not available and software only provides confidence interval output with 2 decimal places.
This mediator effect pattern was maintained at 12 months: At the 5% level DS-CBT could still be shown to reduce avoidance behavior [standardized difference −0.39, 95% CI (−0.59, −0.19), p < 0.001], while the DS-CBT effect on GAD-7 was attenuated and became non-significant [−0.18, (−0.37, 0.014), p = 0.069], as did the PHQ-9 effect [−0.17, (−0.37, 0.031), p = 0.099], (Goldstein et al., Reference Goldstein, Robinson, Mellers, Stone, Carson and Reuber2020), and BES continued not to be changed by the intervention [−0.12, (−0.35, 0.10), p = 0.29].
Which of the putative mediators had a mechanistic effect on outcomes?
Table 1 also summarizes the conceptual effects of our four putative mediators at six months on each of the four outcome measures at 12 months. We standardized mediator and outcome variables by their respective baseline standard deviations so that estimates of conceptual effects are presented on a correlation scale (absolute values around 0.25 = ‘modest link’, 0.5 = ‘strong link’, 0.8 = ‘very strong link’). Table 1 shows that all estimates of conceptual effects were in the hypothesized direction, that is, when statistically significant, reductions in mediator variables were linked to reductions in seizure frequency or WSAS, and to increases in SF-12v2 PCS and SF-12v2 MCS.
Statistically significant mechanistic links were detected between all putative mediators and 12-month outcomes seizures, WSAS and SF-12v2 MCS (all p values ⩽0.002). In contrast, the outcome variable SF-12v2 PCS could only be shown to be linked to avoidance behavior (p = 0.002), but not BES (p = 0.75), GAD-7 (p = 0.17) nor PHQ-9 (p = 0.098). Thus, except for the SF-12v2 PCS score our conceptual theories were supported with very strong links (standardized regression coefficient 0.66) observed between changes (relative to baseline) in avoidance behavior and changes in WSAS, and strong links between avoidance behavior and seizures, and between GAD-7 or PHQ-9 and WSAS or SF-12v2 MCS score (coefficients in 0.4–0.5 range).
How much of the total effect of DS-CBT on outcomes was transmitted by the hypothesized mediators?
Table 1 further summarizes the indirect effects for each mediator-outcome combination. The estimates of the total DS-CBT effects on each outcome are shown on the left-hand side of the table. These inferences have been previously presented in our main trial publication (Goldstein et al., Reference Goldstein, Robinson, Mellers, Stone, Carson and Reuber2020). However, note that, since we required continuous variables for the purposes of causal mediation analysis, we log-transformed the original seizure outcome and this led to a slightly smaller but still non-significant estimate of the total DS-CBT effect on this variable. As reported before, the largest total effect of DS-CBT was found for WSAS at 12 months with an estimated standardized difference of −0.39 (p < 0.001), while the total DS-CBT effects on the other three outcomes considered here were small (<0.2) and did not reach statistical significance.
We found that the DS-CBT effects on 12-month seizure frequency, WSAS and the SF-12 MCS score were mediated by six-month changes in avoidance behavior, GAD-7 and PHQ-9 respectively (zero not included in the 95% CI for the respective indirect effect). There was no evidence to suggest that DS-CBT-induced changes in beliefs about emotions brought about improvements in any outcome measure. In addition, for the 12 months SF-12v2 PCS score only improvements in six months APPS could be shown to bring about outcome improvements. Estimates of the indirect (mediated) effects tended to be of small size (standardized differences 0.1–0.2) with the largest indirect effect estimated for mediator avoidance behavior and outcome WSAS [−0.27 with 95% CI (−0.40, −0.15)].
Discussion
In this study we conducted a mediation analysis of the CODES trial in which participants with DS were randomized to either DS-CBT plus SMC or SMC alone. Twelve-month outcomes included monthly seizure frequency, Work and Social Adjustment Scale and the SF-12v2, a quality-of-life measure. Mediators assessed at six months were: seizure-specific avoidance behavior, beliefs about emotions, anxiety, and depression. These mediators were chosen as important in our causal model of how DS-CBT treatment can improve DS outcomes.
Our mediation analyses found that all of the hypothesized mediators, except beliefs about emotions, were improved by DS-CBT. We found that DS-CBT acted on the targeted mediator variables avoidance behavior, GAD-7 and PHQ-9, with largest effects achieved for avoidance behavior, but did not act on beliefs about emotions.
Assessing the conceptual effects helps us to determine whether a putative mediator had a mechanistic effect on the outcome as hypothesized by the treatment model of DS. All estimates of conceptual effects were in the hypothesized direction, i.e., when statistically significant, reductions in mediator variables were linked to reductions in seizure frequency or WSAS, and to increases in SF-12v2 PCS and SF-12v2 MCS. Only avoidance behavior was linked to the outcome variable SF-12v2 PCS. Thus, except for the SF-12v2 PCS score our conceptual theories were on the right path.
Although we found no difference between treatment arms in our primary outcome at 12 months, consistent with the action and conceptual effects detected, we found evidence that the DS-CBT effects on 12-month seizure frequency, WSAS and the SF-12 MCS score were mediated by six-month changes in avoidance behavior, GAD-7 and PHQ-9. There was no evidence to suggest that DS-CBT-induced changes in beliefs about emotions brought about improvements in any outcome measure. Avoidance behavior at six months mediated improvement in SF-12v2 PCS.
This is the first study to demonstrate that changes in physical functioning were mediated by changing seizure-specific avoidance behavior. Although an understandable coping mechanism, this finding indicates that encouraging patients to engage in social activities and with situations that were anxiety provoking was linked to changes in physical functioning. Avoidance behavior is a key maintaining factor in anxiety disorders such as social anxiety and agoraphobia (Hofmann & Hay, Reference Hofmann and Hay2018). Although one of the key targeted processes in CBT for anxiety disorders, few studies have examined its mechanistic role. A notable exception suggested that targeting avoidance behavior was more important than targeting cognitions in social anxiety disorder (Lervik, Hoffart, Knapstad, & Smith, Reference Lervik, Hoffart, Knapstad and Smith2022). Furthermore, two studies found change in avoidance behavior mediated change in fatigue and or physical functioning in studies of behavioral interventions for people with chronic fatigue syndrome (Chalder, Goldsmith, White, Sharpe, & Pickles, Reference Chalder, Goldsmith, White, Sharpe and Pickles2015; Wearden & Emsley, Reference Wearden and Emsley2013). In DS it is important to understand the function of avoidance behavior more fully. Whilst it is easy to comprehend how it may be useful in the short term as a means of alleviating anxiety or averting the potential threat of having a seizure in an uncontrollable environment, it can become maladaptive in the longer term. Additional gains may be made in CBT by ensuring patients understand the function of avoidance, whilst being empowered to deal with arousal, threat and hypervigilance simultaneously.
Both anxiety and depression mediated change in outcomes suggesting that the cognitive and behavioral interventions targeting seizures and quality of life worked to some extent by changing mood. Given that DS are associated with a wide range of comorbid psychiatric and psychological difficulties (Walsh, Levita, & Reuber, Reference Walsh, Levita and Reuber2018) this is reassuring. Which specific aspects of anxiety and depression are key mechanistically is impossible to say, as we used the total scores of the GAD-7 and PHQ-9 scales in this study. A post hoc analysis could examine sub-scales to explore the mechanisms further.
Mediated effects were relatively small which suggests that treatment may need to target these difficulties more directly and/or that CBT was working via mediators not measured here. It is possible that changes in other processes such as self-efficacy in relation to seizure control, or meta-cognitions related to danger or controllability would have brought about change in the outcomes. Given that beliefs about emotions (BES) did not mediate change it is plausible that targeting this aspect of emotional regulation in a more direct and focused way may bring about additional change, as therapists may have found dealing with behavioral avoidance easier than emotional avoidance (Goldstein et al., Reference Goldstein, Robinson, Pilecka, Perdue, Mosweu, Read and Chalder2021b).
Models of emotional processing in the context of DS have been developed (Jungilligens, Paredes-Echeverri, Popkirov, Barrett, & Perez, Reference Jungilligens, Paredes-Echeverri, Popkirov, Barrett and Perez2022; Pick, Goldstein, Perez, & Nicholson, Reference Pick, Goldstein, Perez and Nicholson2019) and suggestions have been made regarding specific emotion focused interventions. To summarize, depending on the theoretical model, therapies could focus on helping patients with developing skills in recognizing emotion, labeling emotion, recognizing how it is manifested in the body and strategies to regulate emotion. Although dissociation was targeted in a variety of ways cognitively and behaviorally we do not have a measure of dissociation so we cannot comment on whether it mediated outcome.
Strengths and limitations
This study is the first to carry out a planned mediation analyses in the context of a randomized controlled trial of DS-CBT for DS. Our theoretical model and interventions assumed that affective, behavioral and cognitive responses maintain DS and poor quality of life and were specifically targeted. Our mediators were, therefore, theoretically informed. Although the CODES trial was a fully powered effectiveness study it was not powered for mediation investigations. Our statistical models controlled for known confounders. We included age, gender, and psychiatric diagnosis at baseline but ultimately our analysis relies on the assumption that there were no unobserved common causes of the M-Y relationships in addition to the ones modeled. Temporal ordering of the variables ensured plausibility of the hypothesized mechanisms. Nevertheless, at six months when mediators were assessed, treatment was at or nearing completion. We did not demonstrate temporal precedence in that mediators and outcomes appeared to be changing simultaneously. Frequent measurement of mediators during CBT may have been more informative. We also did not have a control group that controlled for therapist time and attention. It is unclear therefore whether the effects of DS-CBT were specific.
In conclusion, a planned mediation analysis showed that our approach did indeed change mechanisms which led to changes in DS and quality of life, providing some empirical evidence for our theoretical model. Although somewhat speculative, it is possible that avoidance of people, places and situations would have been changed by the behavioral exposure parts of the treatment. It also seems likely that gaining understanding of difficulties through the individual formulation including stress and trauma as well as addressing unhelpful beliefs through cognitive techniques will have generated change in anxiety and depression. The latter techniques are transdiagnostic and likely to change a range of somatic and emotional responses. DS-specific avoidance, anxiety and depression should be targeted in DS-CBT due to their mediating role. To improve outcomes the intervention could be further developed to better target beliefs about emotions. Future treatment trials should assess a range of theoretically-driven mediators and ensure that they are sufficiently targeted to bring about meaningful change.
Funding statement and acknowledgements
This paper describes independent research funded by the National Institute for Health and Care Research (Health Technology Assessment program, 12/26/01, COgnitive behavioral therapy v. standardized medical care for adults with Dissociative non-Epileptic Seizures: A multicenter randomized controlled trial (CODES)). This paper also describes independent research part-funded (TC, SL, and LHG) by the National Institute for Health and Care Research (NIHR) Maudsley Biomedical Research Centre at the South London and Maudsley NHS Foundation Trust and King's College London. SL was also supported by the NIHR Applied Research Collaboration South London (NIHR ARC South London) at King's College Hospital NHS Foundation Trust. JS is supported by an NHS Scotland NHS Research Scotland (NRS) Career Fellowship and JS and AC also acknowledge the financial support of NRS through the Edinburgh Clinical Research Facility. MR benefitted from the support of the NIHR Sheffield Biomedical Research Centre (Translational Neuroscience). EJR received salary support from the NIHR Biomedical Research Centre based at Guy's and St Thomas' NHS Foundation Trust and King's College London. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
For the purposes of open access, the author has applied a Creative Commons Attribution (CC BY) license to any Accepted Author Manuscript version arising from this submission.
Competing interests
AC reports being a paid editor of the Journal of Neurology, Neurosurgery and Psychiatry, and is the director of a research program on functional neurological disorders; he gives independent testimony in Court on a range of neuropsychiatric topics (50% pursuer, 50% defender). SL is a paid editor of the Journal of Child Psychology and Psychiatry. MR is the paid Editor-in-Chief of Seizure – European Journal of Epilepsy and receives authorship fees from Oxford University Press in relation to a number of books about DS. JS reports independent expert testimony work for personal injury and medical negligence claims, royalties from UpToDate for articles on the functional neurological disorder and runs a free non-profit self-help website, www.neurosymptoms.org. The remaining authors have no conflicts of interest to declare.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The CODES trial was approved by the London – Camberwell St Giles Research Ethics Committee. The trial was registered with Current controlled Trials ISRCTN05681227 and ClinicalTrials.gov NCT02325544.







