Self-harm is a common problem among young people aged 15-20 in the UK, affecting 7-14% at some point in their lives (Reference Hawton, Rodham and EvansHawton et al, 2002; Reference Young, Van Beinum and SweetingYoung et al, 2007), and the problem is increasing (Reference Gunnell, Middleton and WhitleyGunnell et al, 2003; Reference Klonsky, Oltmanns and TurkheimerKlonsky et al, 2003). It remains the strongest predictor of future self-harm and completed suicide (Reference Hawton and JamesHawton & James, 2005). Death by suicide also remains tragically frequent in psychotic illness (Reference SirisSiris, 2001; Reference Palmer, Pankratz and BostwickPalmer et al, 2005; Reference TandonTandon, 2005; Reference Healy, Harris and TranterHealy et al, 2006), with an estimated 4.9-10% of patients with schizophrenia who complete suicide, usually near illness onset (Reference Hawton, Sutton and HawHawton et al, 2005). Recognising self-harm as a risk factor for future suicide attempts is of great importance. Studies investigating self-harm in psychotic illness have mainly looked at people with established illness, often chronic (e.g. Reference Harkavy-Friedman, Restifo and MalaspinaHarkavy-Friedman et al, 1999). The OPUS study (Reference Nordentoft, Jeppesen and AbelNordentoft et al, 2002), which focused on suicidal behaviour in first-episode psychosis in The Netherlands, found female gender, feelings of hopelessness, hallucinations and suicide attempts at baseline to be predictive of future suicide attempts.
Accurate knowledge of the frequency of self-harm at first presentation is essential in reducing the rate of suicide in psychotic disorders, and further information on demographic details of those who self-harm will be useful in targeting further research and effective interventions.
We aimed to establish the frequency of self-harm in patients with psychotic illness prior to and at presentation to psychiatric services. We also sought to study methods of self-harm for those individuals with a history of self-harm, and their demographic characteristics.
Method
Patient sample
The inclusion criteria for the study were patients aged 16-35 years, residents in Birmingham, experiencing first-episode psychosis, and referred to and accepted by Birmingham early intervention services between January and December 2006.
Setting and design
We undertook a case-note review within the early intervention services in Birmingham. Previous audits identify that the majority (over 90%) of patients with first-episode psychosis will be referred to and managed by early intervention services. Details of self-harm at baseline were extracted from patients’ initial risk assessment and care plan assessment records (details of patients’ history of self-harm are routinely recorded in their care plan assessment as part of risk screening). Acts of self-harm were divided into those prior to contact with services (>2 months) and at contact with services. Where acts of self-harm had been recorded without sufficient detail, further information was sought from the patient history and from case managers. Patient notes were also read thoroughly to investigate the possibility that acts of self-harm had come to light which were not detailed in the initial risk assessment.
Only actual acts of self-harm were included in the analyses. ‘Near misses’ and threats, although significant, were not categorised as acts of self-harm; self-neglect was not considered an act of self-harm.
Demographic details and substance misuse history were taken from patient notes. Postcodes were assigned the Townsend Material Deprivation Score (Reference Townsend, Phillimore and BeattieTownsend et al, 1989) using data from the 2001 census (www.statistics.gov.uk/census2001). Diagnoses were made by an experienced consultant psychiatrist (R.U.) and colleagues in accordance with ICD-10 research diagnostic criteria (World Health Organization, 1993).
Analysis
Analyses were carried out using SPSS version 15 for Windows. Tests of association (chi-squared) were used to ascertain which, if any, demographic variables were predictive of self-harming behaviour. For the two continuous variables (age and deprivation index scores) tests of normality were used to determine whether data were normally distributed. Given the exploratory nature of the study, and conflicting evidence in previous research regarding which demographic factors were significant, a stepwise binary logistic regression was also used to ascertain which model combination of variables was best predictive of self-harming behaviour.
Results
Frequency of self-harm
A total of 114 patients were accepted by early intervention services and met the inclusion criteria for the study; 32% (n=37) had a reported history of self-harm.
Of patients with a history of self-harm, 27% (n=10) had a single episode of self-harm coinciding with their presentation to psychiatric services; 65% (n=24) had a history of episodes of self-harm more than 2 months before referral to psychiatric services. A small number of patients (n=3, 8%) had previous episodes of self-harm both at presentation and in the past. Of the 37 patients with a history of self-harm, 22% (n=8) had experienced more than one episode of self-harm.
Types of self-harm
The frequency of each subtype of self-harm is shown in Fig. 1. Self-laceration was the most frequently used method, occurring on 17 separate occasions, followed by self-poisoning occurring on a total of 14 occasions. The most common substance to use in self-poisoning was antipsychotic medication.
Demographic characteristics
Tables 1, 2, 3 shows the demographic characteristics of those with a history of self-harm compared with those who did not self-harm.
Table 1. Demographic characteristics of those in the cohort who self-harmed v. those who did not
| Demographic variable | Patients with a history of self-harm,a n (%) | Patients without a history of self-harm,b n (%) | Χ2 | d.f. | P |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 25 (68) | 65 (84) | |||
| Female | 12 (32) | 12 (16) | 4.27 | 1 | 0.04c |
| Ethnicity | |||||
| White | 15 (41) | 31 (40) | 0.00 | 1 | 0.57 |
| Asian | 15 (41) | 24 (35) | 0.78 | 1 | 0.22 |
| Black | 4 (11) | 10 (13) | 0.11 | 1 | 0.50 |
| Other | 3 (8) | 12 (16) | 1.22 | 1 | 0.21 |
| Marital status | |||||
| Single | 33 (89) | 64 (83) | 0.73 | 1 | 0.29 |
| Married | 3 (8) | 7 (9) | 0.30 | 1 | 0.58 |
| Other | 1 (3) | 6 (8) | 1.12 | 1 | 0.27 |
| Occupational status | |||||
| Unemployed | 24 (65) | 60 (78) | |||
| Employed/student | 13 (35) | 17 (22) | 2.20 | 1 | 0.11 |
| Substance misuse | |||||
| History of cannabis used | 18 (49) | 47 (61) | 1.57 | 1 | 0.15 |
Table 2. Mean age of those who self-harmed v. those who did not
| Patients with a history of self-harm, n=37 | Patients without a history of self-harm, n=77 | Mann–Whitney Z | P | |
|---|---|---|---|---|
| Age, mean (s.d.) | 19.4 (3.6) | 22.0 (4.4) | –3.19 | <0.01a |
Table 3. Mean deprivation scores for those who self-harmed v. those who did not
| Patients with a history of self-harm, n=37 | Patients without a history of self-harm, n=77 | t | P | |
|---|---|---|---|---|
| Deprivation Index score, mean (s.d.) | 3.5 (3.5) | 3.1 (3.3) | –0.58 | 0.56 |
Females and younger patients were more likely to have self-harmed (χ2=4.27, P=0.04 for females and Z=–3.19, P<0.01 for younger patients). Ethnicity, a history of substance misuse, marital status and occupational status at the time of presentation were not predictive of acts of self-harm.
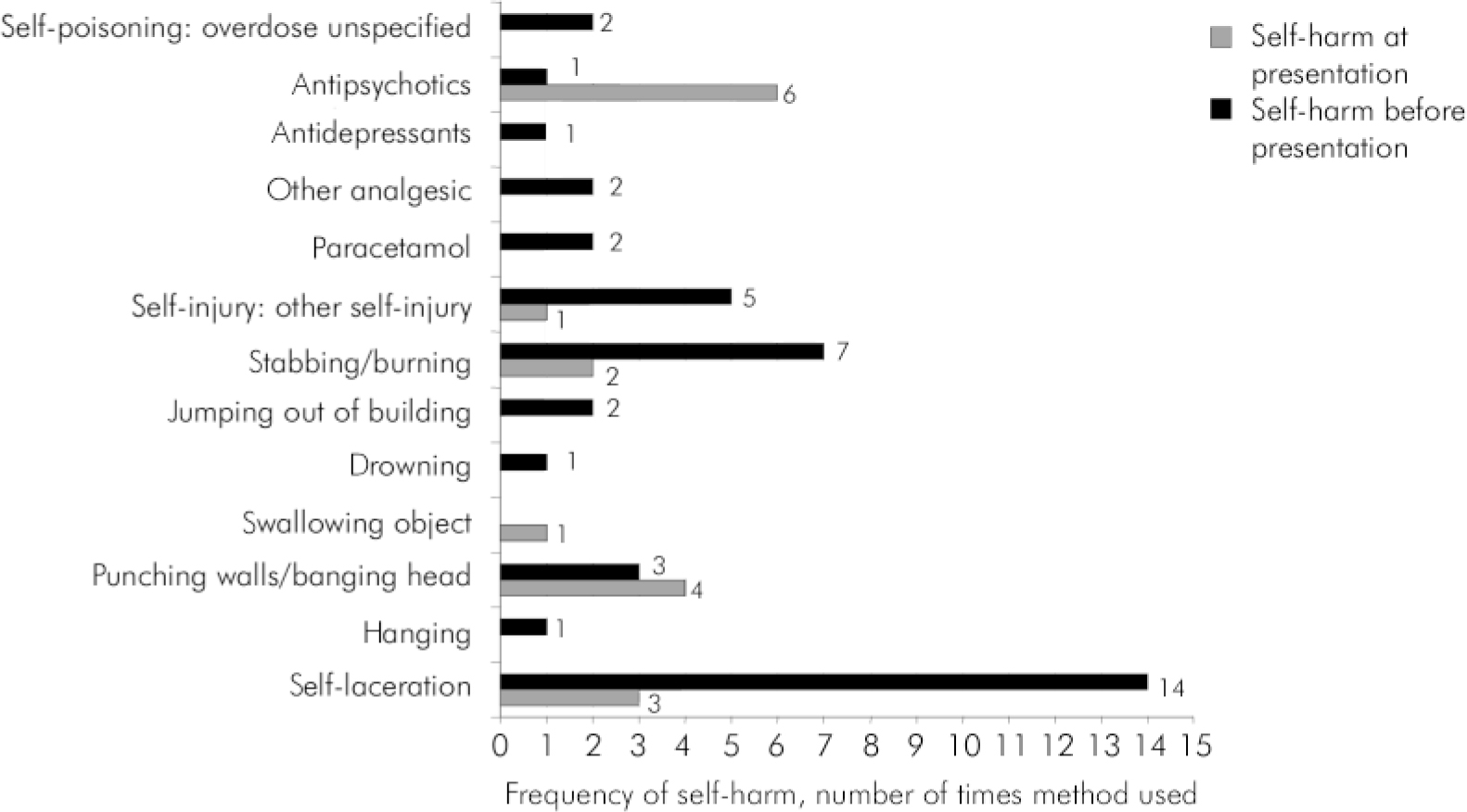
Fig. 1. Self-harm before and at presentation. Total greater than 37 as eight patients experienced more than one episode of self-harm.
Diagnoses
Diagnoses were obtained for 97% (n=111) of patients in the cohort. It was not possible to obtain diagnoses for the remaining three patients as they had only recently been accepted into the service. Schizophrenia was the most common diagnosis, occurring in 61% (n=68). Other diagnoses included mania with psychotic symptoms in 6.3% (n=7), bipolar affective disorder in 4.5% (n=5), delusional disorder in 3.6% (n=4) and acute and transient psychotic disorder in 14% (n=16). No other diagnosis was significantly associated with self-harm behaviour.
Regression analysis
A forward stepwise binary logistic regression was used to determine which combination of variables was best predictive of self-harm. As a stepwise regression model was used, both significant and non-significant factors from the univariate analysis were included. A model of younger age in combination with employment/being a student was significant in the prediction of self-harming behaviour. However, the influence of these variables in predicting self-harming behaviour using the regression model was small (r 2=0.120; Table 4).
Table 4. Binary logistical regression model
| 95% CI | |||
|---|---|---|---|
| Model | OR | Lower | Upper |
| Occupational statusa | 0.379 | 0.145 | 0.990 |
| Agea | 0.826 | 0.734 | 0.930 |
Discussion
Clinical implications
There was a high rate of self-harm in the cohort - just under a third of patients had episodes of self-harm in their history. This was in keeping with findings from other studies, in which self-harm rates in early psychosis ranged from 15.1 to 42.9% (Reference Verdoux, Liraud and GonzalesVerdoux et al, 2001; Reference Addington, Williams and AddingtonAddington et al, 2004), and demonstrates rates much higher than those in the general population; Young et al (Reference Young, Van Beinum and Sweeting2007) showed a 7.1% lifetime prevalence of self-harm, with only 1.6% current incidence of self-harm. The high rate in our cohort may represent suicidal thinking as part of untreated psychosis or as part of emotional distress in the prodromal phase; both phases have been documented to have high rates of suicidal thinking (Reference Larsen, Friis and HaahrLarsen et al, 2004). We were not able to distinguish between these in this study.
The high incidence of self-laceration prior to presentation is a reflection on how such self-harming behaviour can escape attention by services. Our finding was different to that of the AESOP study (Reference Harvey, Dean and MorganHarvey et al, 2008), who identified self-poisoning as the most common method, closely followed by self-laceration, in their older sample of patients with first-episode psychosis. Their focus was on self-harm during the untreated psychotic phases of a first episode, whereas in our study all previous attempts were included. The medical profession should be alerted to the significance of self-harm and how this may constitute part of an individual's first presentation with psychotic illness or indeed prodromal symptoms. The most frequent medication used for self-poisoning in our sample was an antipsychotic, a reminder that extreme care and attention to risk needs to be taken when first starting treatment for psychosis. This is more important with the increasing focus on home treatment models, where patients or family may be left to supervise medication.
Univariate analysis showed that female gender was a significant predictor of self-harming behaviour (P=0.04). The age of those with a history of self-harm was also significantly lower than the age of those without such a history. This demographic profile is different to the profile of those who die by suicide. For example, although females are more likely to self-harm (Reference Hawton, Rodham and EvansHawton et al, 2002; Reference Douglas, Cooper and AmosDouglas et al, 2004;Reference Young, Van Beinum and SweetingYoung et al, 2007), suicide rates in males with schizophrenia remain higher than in females (Reference Hunt, Kapur and WindfuhrHunt et al, 2006).
Within the regression model, younger age and employment point to an increased risk. This reflects findings in the general population, such as those of Young et al's (Reference Young, Van Beinum and Sweeting2007), which also demonstrated a transient nature of self-harm in young people in employment or education, suggesting a better clinical outcome for this group. How far this is reflected within our sample of patients with first-episode psychosis warrants further investigation.
No significant difference in terms of substance misuse was found. There was no correlation between acts of self-harm and Townsend score, although previous studies have identified such an association in completed suicide (Reference Gunnell, Lopatatzidis and DorlingGunnell et al, 1999).
Limitations
The reliability of case-note review results depends on the quality of information recorded in the notes, the care plan assessment and risk assessment documentation, and therefore it is probable that the true incidence of self-harm was higher than that recorded. A small sample size is also a clear limitation.
Conclusions
This simple case-note review highlights the frequency of self-harm in early psychosis and should serve to remind clinicians of the importance of adequate risk assessment and mental state examination, with a focus on enquiring about early psychotic symptoms in all young patients presenting with acts of self-harm. There is increasing evidence to suggest that the early detection of psychosis can prevent suicidal behaviour (Reference Harkavy and JillHarkavy & Jill 2006; Reference Melle, Johannesen and FriisMelle et al, 2006) and this study supports existing evidence of the prevalence of risk at onset of psychotic illness.
Declaration of interest
None.








eLetters
No eLetters have been published for this article.