The National Institute for Health and Clinical Excellence (NICE) guidelines on the treatment of obsessive-compulsive and body dysmorphic disorders (National Institute for Health and Clinical Excellence, 2005) describe a 6-stage model of stepped care, based on severity of the condition (online Table DS1). They recommend that each mental healthcare and children's trust should have a specialist obsessive-compulsive and body dysmorphic disorders multidisciplinary team offering age-appropriate care. They also recommend that people with severe, chronic, treatment-refractory disorders be referred to specialist treatment services staffed by multidisciplinary teams of healthcare professionals with expertise in the management of the disorders.
At present there is a lack of such highly specialised treatment services. This is not surprising considering the relatively small numbers of individuals with severely refractory disorders. It has been estimated that approximately 1% of the European population have clinically relevant obsessive-compulsive disorder (OCD) (Reference Wittchen and JacobiWittchen & Jacobi, 2005). In the UK where the population is estimated at about 48 million adults (Office for National Statistics, 2001) it gives a number of 480 000 individuals potentially requiring treatment for this disorder. However, modern psychological and pharmacological treatments have revolutionised outcomes for the majority of such individuals (Mohammed et al, 2000) - for example, approximately 75% will improve following graded exposure (Reference Drummond and FinebergDrummond & Fineberg, 2007) and 60% will respond to selective serotonin reuptake inhibitor (SSRI) drugs (Reference Fineberg and GaleFineberg & Gale, 2005). Thus, if we were to assume that all individuals in England and Wales with OCD received an SSRI in primary care we might expect around 288 000 to improve and 192 000 still to require treatment. A second trial of a different SSRI would result in over 76 000 requiring treatment. If they were then referred for treatment using graded exposure, then about 19 200 throughout the UK may be expected not to respond to treatment locally and require more specialised treatment.
These 19 200 individuals may need to be treated in a variety of ways. Augmentation of SSRIs with dopamine antagonists or other pharmacological treatments has been recommended (Reference Fineberg, Amit Nigam and SivakumaranFineberg et al, 2006) and may be effective in up to 50% cases (Reference Bloch, Landeros-Weisenberger and KelmendiBloch et al, 2006). This would leave 9600 individuals still needing further treatment. In the NICE guidelines, these individuals lie at level 5 in the continuum of severity and treatment requirement. Many will require intensive home-based psychological treatment, which can be delivered by regional specialist services such as the already described behavioural cognitive psychotherapy unit (Reference Drummond, Pillay and KolbDrummond et al, 2008, this issue). On the basis of the results from our unit, we may expect 62% of individuals at level 5 to improve with treatment by at least 30% reduction in symptoms. This leaves 3500 potentially to be treated at level 6. However, currently only a small percentage of individuals present for treatment and many prefer to manage for many years on their own before accepting treatment (Reference Hollander and WongHollander & Wong, 1998).
Few centres in England have expertise and experience in the intensive treatment of refractory obsessive-compulsive and body dysmorphic disorders. Specialist care is offered at Queen Elizabeth II Hospital in Welwyn Garden City which specialises in a psychopharmacological treatment combined with psychological approach. Community and out-patient treatment based more on psychological therapies but also with medication review is available at South London and Maudsley National Health Service (NHS) Foundation Trust and at the South West London and St George's Mental Health NHS Trust. A residential unit at the Bethlem Royal Hospital in south London treats individuals who do not need 24-h nursing care but who are unsuitable for community treatment and the behavioural cognitive psychotherapy unit at South West London and St George's Trust has 10 in-patient beds for those who require 24-h supervised and nursed treatment. Services for the small group of children and adolescents with severe, treatment-resistant OCD are provided by the young people's out-patient service at the Maudsley Hospital. There are also specialist in-patient beds for adolescents with the most severe illness available within the adolescent service at the Priory Hospital in north London.
Historically, access to these services has been patchy due to the funding constraints of primary care trusts and different priorities in various geographical areas. In response, the services delivering level 6 intervention for obsessive-compulsive and body dysmorphic disorders (Fig. 1) decided collaboratively to invite the Department of Health to coordinate and fund a comprehensive and highly specialised service dedicated to treating such individuals. From 1 April 2007 the Department of Health, via the National Commissioning Group, agreed to commission and fund a national service for those with the most severe level 6 obsessive-compulsive/body dysmorphic disorders who have failed all previous treatments (including home-based treatments) provided by regional specialists. This agreement covers all individuals in England, with reciprocal arrangements existing for Scotland, Northern Ireland and Europe. Separate arrangements exist for Wales whereby each referral is examined on an individual basis.
Method
The operation of this service requires close collaboration between clinicians and managers at several sites. Clinicians discuss and make decisions about each individual in monthly referral meetings, run via video conference to save travelling time. The service aims to disseminate good practice and offer education and support to mental health professionals in local community mental health teams, and child and adolescent mental health services and regional centres managing individuals who have not yet received treatments at level 2-5 (National Institute for Health and Clinical Excellence, 2006). Joint working with care coordinators as co-therapists is encouraged. Following treatment continuity of care is ensured by actively involving local care coordinators in the later stages of treatment and discharge process.
The National Commissioning Group has commissioned services for the following number of individuals with obsessive-compulsive/body dysmorphic disorders, for the first year of operation:
-
• South West London and St George's Trust: 25-30 adult in-patients and 60 adult out-patients per annum plus post-admission treatment and follow-up at the behavioural and cognitive psychotherapy unit for in-patients;
-
• South London and Maudsley Trust:16 adult in-patients on Bethlem Hospital residential unit, 60 adult out-patients and 12-15 child and adolescent out-patients treated at Maudsley Hospital;
-
• Hertfordshire Partnership NHS Trust: 20 adult out-patients and 2 in-patients at the Queen Elizabeth II Hospital, Welwyn Garden City;
-
• Priory Hospital: 6 adult out-patients with body dysmorphic disorder and 6 adolescent in-patients.
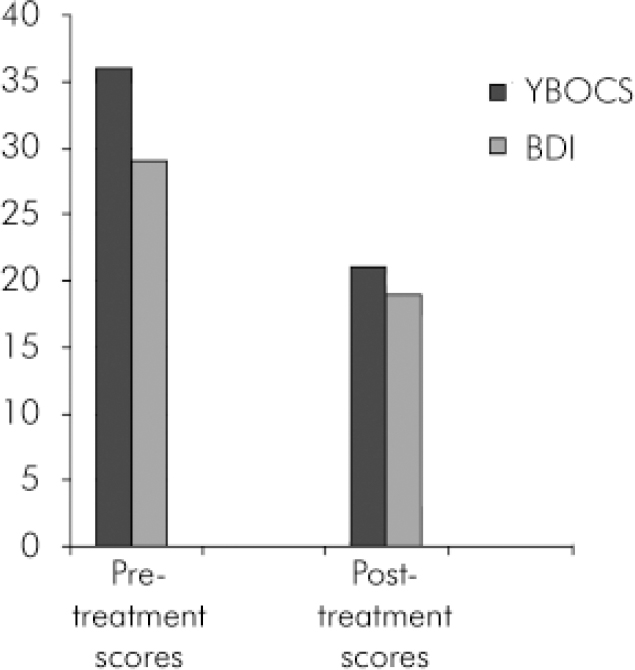
Fig. 1. Patient severity scores at the beginning and end of treatment for in-patients treated at South West London and St George's NHS Trust. YBOCS, Yale-Brown Obsessive Compulsive Score (maximum 40); BDI, Beck Depression Inventory (over 20= severe depression).
Entry to a national out-patient, community or residential unit service
To ensure these services are not overburdened or inequitably accessed by individuals across the country, strict protocols are applied. Individuals with obsessive-compulsive/body dysmorphic disorders must fulfil the following criteria:
-
• Yale-Brown Obsessive Compulsive Scale (ten-item scale, maximum score 40) score more than 30 (severe-extreme disorder; Reference Goodman, Price and RasmussenGoodman et al, 1989);
-
• failed to respond or refused two trials of cognitive-behavioural therapy, one of which should be home-based or in the situation where symptoms are maximal;
-
• failed to respond to two trials of an SSRI or clomipramine at British National Formulary recommended doses for a minimum of 3 months each;
-
• failed to respond to pharmacological augmentation of SSRI with a recognised agent or high-dose SSRI (Reference Pallanti, Hollander and BienstockPallanti et al, 2002).
For children and adolescents under 18 years of age:
-
• Yale-Brown Obsessive Compulsive Scale score more than 30;
-
• failed to respond to two trials of SSRI at British National Formulary recommended doses for a minimum of 3 months each;
-
• failed to respond to a previous trial of cognitive-behavioural therapy which included elements of graded exposure and response-prevention.
Entry to other services
In addition to be eligible for in-patient admission to the behavioural and cognitive psychotherapy unit at South West London and St George's Mental Health Trust, to Queen Elizabeth II Hospital or Priory Hospital, individuals must have specific reasons why less intensive treatment is unsuitable such as:
-
• danger to self either because of chronic suicidality (acute suicidal episodes should be managed by local services) or extreme self-neglect (e.g. failure to have a sufficient intake of liquids with incipient renal failure without nursing input);
-
• danger to others because of the disorder (e.g. impulsive acts);
-
• compulsions so severe that a person cannot manage without 24-h care (e.g. regular incontinence because of OCD compulsions taking one 3 h to get up in morning);
-
• severe delayed sleep phase shift resulting in individual not being awake during the day;
-
• complicating additional diagnosis making close observation throughout treatment essential (e.g. anorexianervosa, schizophrenia - both diagnoses may be exacerbated by the stress of exposure therapy);
-
• diagnostic doubt meaning that 24-h observation is useful initially.
Results
The service has only been commissioned on 1 April 2007 and thus a full year's data are not yet available. However, the behavioural cognitive psychotherapy unit at South West London and St George's Trust in-patient service has been operating for many years in its current format and has been recording individuals who meet the National Commissioning Group criteria over the past 2 years.
Results from the behavioural cognitive psychotherapy unit service
Since 1 July 2005 there have been 23 individuals who met National Commissioning Group criteria admitted as in-patients to the behavioural cognitive psychotherapy unit. Their mean age was 37 years old (s.d.=13, range 18-63), with a mean duration of illness being 17 years (s.d.=13, range 4-50); average hospital stay was 20 weeks (s.d.=51 days; range 25-208 days). The outcome results are given in Table 1 and Fig. 1.
Table 1. Patient severity scores at the beginning and end of treatment for in-patients treated at South West London and St George's NHS Trust
| Measures | Admission mean (s.d.) | Discharge mean (s.d.) | Clinical significance of reduction | P |
|---|---|---|---|---|
| YBOCS (n=23) | 36 (3) | 21 (9) | Profound to moderate obsessive–compulsive disorder | <0.0005 |
| Padua inventory1 (n=13) | 90 (47) | 58 (39) | A normal American population scored about 41 on this scale (Reference SanavioSanavio, 1988) | <0.05 |
| BDI (n=16) | 29 (11) | 19 (14) | A score under 10 is ‘non-depressed’ | <0.005 |
Overall, this represents a 42% reduction in OCD symptomatology measured by the Yale-Brown Obsessive Compulsive Scale (n=23) and a 35% reduction in depressive symptomatology measured by the Beck Depression Inventory (Reference BeckBeck, 1978) (n=16).
Discussion
The coordinated, collaborative pharmacological/psychological specialist service for refractory obsessive-compulsive/body dysmorphic disorders in adolescents and adults was established in five units in the south-east England. Instead of individual trusts competing for patients, clinicians have taken the lead and with Department of Health support they have joined together to ensure that those with the most severe illness receive optimal care tailored to individual need.
There are still a number of challenges to be overcome. Despite NICE guidelines, local and regional services for such individuals remain patchy throughout the UK. It is therefore essential that the national service is not simply used to ‘paper over cracks’ in existing services. By offering education and support to mental health professionals across the country, we aim to ensure that every individual with obsessive-compulsive/body dysmorphic disorder has access to the highest standard of psychopharmacological and psychological treatment in their local area, including the option of home-based exposure treatment for those with the most severe illness. Only once this has failed should they be referred to the national units. Geographical referral patterns need to be carefully monitored to ensure equitable access to the service nationwide. Following national treatment, continuity of care and ongoing rehabilitation is dependent upon active involvement of local mental health team workers.
This model, whereby the extremely treatment-resistant individual is treated at a national centre, seems suited for the treatment of profound obsessive-compulsive/body dysmorphic disorders. However, it may also be applicable to other diagnoses. Recent emphasis on local treatment is to be applauded but it may lead to a ‘hard core’ of the most disabled and intractable individuals being overlooked if their needs are unmet.
Declaration of interest
All authors work in the services described but have no other interest in this paper.





eLetters
No eLetters have been published for this article.