Neuropsychiatric sequelae of brain injury are numerous and can include disturbances in cognition, mood and behaviour. They commonly impede individuals’ ability to function in their work and family life and are responsible for at least as much disability as the associated physical symptoms (Reference LishmanLishman, 1998).
Treatment includes pharmacological medication and rehabilitation. Rehabilitation is multifaceted (Reference Rao and LyketsosRao & Lyketsos, 2000) and it is often difficult to determine which specific interventions are responsible for improvements in an individual. It is therefore necessary to have good outcome measures. Fleminger & Powell (Reference Fleminger and Powell1999) highlighted that most importantly, outcome measures need to be relevant to the patient and carer; they must also be trustworthy, and ideally used consistently across studies to facilitate comparison of treatment methods.
The Health of the Nation Outcome Scales (HoNOS; Reference Wing, Beevor and CurtisWing et al, 1998) were produced to provide an easily administered and reliable measure to be used in general adult mental health. Subsequent versions have been developed for more specialist settings. The Health of the Nation Outcome Scale for Acquired Brain Injury (HoNOS—ABI) for the assessment of individuals who have sustained a brain injury was developed by the UK Brain Injury Psychiatrists Group in conjunction with the Royal College of Psychiatrists’ Research Group, and has been available since 1999 (further details available from the author upon request).
Little work has been done to investigate the clinical relevance of HoNOS—ABI. Coetzer & Du Toit (Reference Coetzer and Du Toit2001) found promising correlations between the scale and three other outcome measures, including post-injury employment status. These findings indicate that the HoNOS—ABI is valid and pertinent to patients, as it relates outcome to reintegration into the community. However, there is no published assessment of interrater reliability for HoNOS—ABI, an index Portney & Watkins have argued is ‘especially important when measuring devices are new’ (Reference Portney and WatkinsPortney & Watkins, 1993, p. 60). Our study therefore investigated the interrater reliability of this measure.
Method
Raters
The 24 raters consisted of staff from five neuropsychiatric brain injury rehabilitation sites in the UK. They were all healthcare professionals and included psychiatrists, psychologists and charge nurses. None had received formal training in using the HoNOS—ABI but all were familiar with the completion of outcome measures.
Participants
The 50 in-patients ranged in age from 18 years to 65 years. All had disabling neuropsychiatric sequelae following severe traumatic brain injury requiring in-patient rehabilitation.
Design and materials
Every patient was assessed independently by two raters. Each pair of raters saw only a sample of the study participants. The assessments were made separately by the two raters in the course of routine clinical practice and were not conducted through an interview process. The raters were well acquainted with the patients they assessed, who were all residents of the in-patient units.
The HoNOS—ABI consists of 12 items, each reflecting a different domain of symptoms rated on a five-point scale (with 0 indicating no problem). Items 11 and 12 are designed for patients in community settings and were therefore excluded from the analysis. Item 3 relates to problems associated with alcohol and drug use, which can be difficult to assess among in-patients (n=36 for this item). All analyses were performed on a personal computer using Microsoft Excel, the Statistical Package for the Social Sciences version 11.0 and Stata version 8.
Statistical analysis
The intraclass correlation provides an assessment of interrater reliability by comparing the amount of variation between raters with the amount of variation between individuals. A one-way random analysis of variance was used to calculate the intraclass correlation coefficient (ICC) because each pair of raters had not assessed all the participants. In order to take the closeness of agreement between raters into account, weighted kappa values (κw) were also calculated for each item (Fig. 1). Significance tests can identify whether raters show an agreement above chance or not. Values of κ w are always lower than their corresponding ICC. To interpret the degree of agreement, the guidelines provided by Landis & Koch (Reference Landis and Koch1977) were used: 0.21-0.40 is seen as a fair level of agreement, 0.41-0.60 as moderate, 0.61-0.80 as substantial and >0.81 as almost perfect. Although these ‘ divisions are arbitrary, they do provide useful benchmarks’ (Reference Landis and KochLandis & Koch, 1977, p.165).
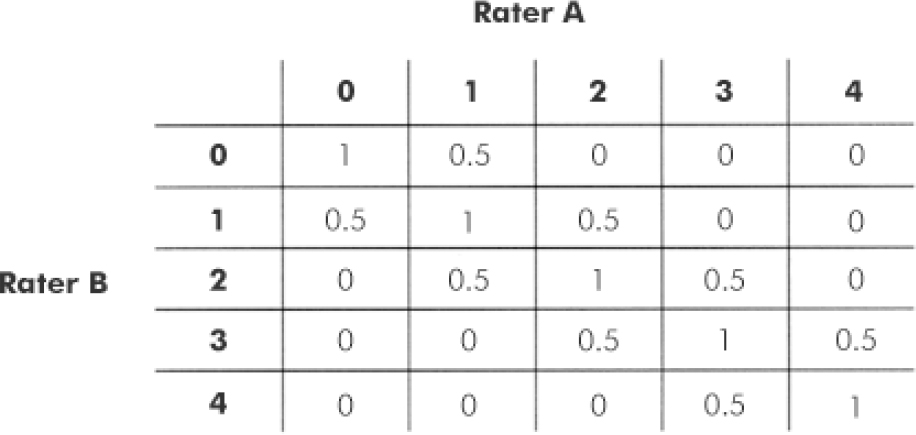
Fig. 1. Weight matrix used to calculate weighted kappa values.
Results
Table 1 shows the mean scores for each item, which range from 0.21 to 3.04. The low mean score (0.21) and associated standard deviation (0.01) on the item relating to alcohol or drug misuse may be because the participants were in-patients without ready access to alcohol or drugs. The domains with the highest mean scores were those assessing cognitive problems, problems with activities of daily living, and relationships. The standard deviation for all items is quite low, suggesting that most participants had similar levels of problems.
Table 1. Scores on each HoNOS—ABI item (0-4) and across all ten items (0-40)

| Item | Symptoms | Mean (s.d.) |
|---|---|---|
| 1 | Antisocial | 2.17 (0.41) |
| 2 | Self-injury | 0.47 (0.21) |
| 3 | Alcohol/drugs1 | 0.21 (0.01) |
| 4 | Cognitive | 3.04 (0.34) |
| 5 | Physical | 1.78 (0.34) |
| 6 | Psychotic | 1.17 (0.47) |
| 7 | Depression | 1.25 (0.47) |
| 8 | Other | 1.45 (0.55) |
| 9 | Relationships | 2.29 (0.41) |
| 10 | Activities of daily living | 2.80 (0.37) |
| Total scores | 19.09 (1.46) |
Table 2 shows the κ w and ICC values and their confidence intervals for each item. The interrater reliability ranges from 0.43 to 0.84 for κ w and 0.58 to 0.97 for ICC. Calculation of test statistics for κw(z=κw/standard error) indicated that, for all items, the level of agreement between the pairs of raters was significantly greater than chance (P<0.001), which was also supported by the finding that the confidence intervals for both κw and ICC values did not include zero. The level of agreement was highest for the item relating to drug or alcohol problems (κw=0.82, ICC=0.97). The lowest interrater reliability was for the item corresponding to depressive symptoms (κw=0.43), whereas the lowest reliability for the ICC values was for the item relating to other symptoms (0.58). All values showed at least moderate agreement (Reference Landis and KochLandis & Koch, 1977).
Table 2. Weighted kappa and interclass correlation values for all items of the HoNOS—ABI
| Item | Symptoms | k w (95% CI) | ICC (95% CI) |
|---|---|---|---|
| 1 | Antisocial | 0.54 (0.38-0.70) | 0.73 (0.57-0.84) |
| 2 | Self-injury | 0.56 (0.36-0.76) | 0.71 (0.55-0.83) |
| 3 | Alcohol/drugs1 | 0.84 (0.59-1.09) | 0.97 (0.94-0.98) |
| 4 | Cognitive | 0.53 (0.35-0.71) | 0.68 (0.50-0.80) |
| 5 | Physical | 0.66 (0.50-0.82) | 0.81 (0.68-0.88) |
| 6 | Psychotic | 0.51 (0.32-0.70) | 0.64 (0.44-0.78) |
| 7 | Depression | 0.43 (0.26-0.60) | 0.62 (0.41-0.76) |
| 8 | Other | 0.53 (0.35-0.71) | 0.58 (0.36-0.74) |
| 9 | Relationships | 0.52 (0.36-0.68) | 0.73 (0.57-0.84) |
| 10 | Activities of daily living | 0.54 (0.36-0.73) | 0.68 (0.50-0.80) |
Discussion
Reliability across items
The Z test of significance on the κw values and the finding that none of the confidence intervals for κw or ICCs contained zero indicated that the level of agreement between the pairs of raters was significantly greater than chance for all items of the HoNOS—ABI assessed. The interrater reliability of the item relating to problems with drugs or alcohol was 0.84, which may be spuriously high owing to the smaller sample size used, but is more likely to be due to the lack of access to drugs in rehabilitation settings and the concrete nature of the question. The lowest κw value was for the depressive symptoms item, indicating that it is more difficult to rate this item consistently. The ICC was lowest for the item assessing other mental and behavioural problems, with a wide confidence interval of 0.38. This item is disparate in nature and might be more clinically useful if viewed qualitatively. Interrater reliability values for the other items were all similar and showed at least moderate agreement.
Rater training
It is possible that differences in raters’ interpretation of the items, rather than their assessment of the patients, led to lower reliability. Brooks (Reference Brooks2000) examined the efficacy of staff training on the reliability of the generic HoNOS and concluded that although ‘reasonable improvements could be gained’ (p. 509), staff training could also be of ‘no value’ (p. 609). The findings are clearly inconclusive, although training could increase the reliability of the scales.
Neuropsychiatric sequelae
Overall, the participants were rated as having particular problems within the domains of cognitive functioning, relationships and activities in daily life, in line with the findings of Coetzer & Du Toit (Reference Coetzer and Du Toit2001). In contrast, Orrell et al (Reference Orrell, Yard and Handysides1999) investigated scores on the generic HoNOS among a population of psychiatric patients and found that the patients were rated as having more problems with depressed mood, other mental health problems and relationships. In this investigation, participants were rated as having more severe problems on most items (mean scores 0.21-3.04) compared with those assessed in the study by Orrell and colleagues (mean scores 0.24-1.64; Reference Orrell, Yard and HandysidesOrrell et al, 1999). The findings reported here and by Coetzer & Du Toit (Reference Coetzer and Du Toit2001) support the proposal that individuals who have sustained a brain injury tend to present with particular difficulties in cognition which then affect their general psychosocial functioning and ability to perform activities of daily living (Reference Ponsford, Sloan and SnowPonsford et al, 1995).
Potential criticisms
The generalisability of the study is limited; all the participants were in-patients on neuropsychiatric brain injury units with moderate to severe cognitive, behavioural and/or neuropsychiatric problems resulting from traumatic brain injury. Reliability will be higher because all raters had the opportunity to observe and discuss the patients in some detail. Raters did not have to rely on taking a history from the patient or an informant to rate the patient, as they would probably need to do in an out-patient or community setting. On the other hand, we used data from several sites and the ratings were made during the course of routine clinical care without specific training.
Implications of the study
The findings from our study indicate that interrater reliability was good for most items of the HoNOS—ABI and moderate for one item. Although there is still a need for further evaluation of the validity and reliability (including test—retest) of this scale, our study complements the work of Coetzer & Du Toit (Reference Coetzer and Du Toit2001) and highlights the potential usefulness of the scale both in a research setting and as part of routine clinical practice. The HoNOS—ABI proved to be a reliable outcome measure of the neuropsychiatric sequelae of brain injury across different raters when used for assessment within a rehabilitation setting, during the course of routine clinical practice.
Declaration of interest
None.






eLetters
No eLetters have been published for this article.