People with mental illnesses, especially schizophrenia, have a higher mortality rate than the general population, the causes of which are yet poorly understood but could be related to side-effects of antipsychotic medication (Reference Waddington, Youssef and KinsellaWaddington et al, 1998). Psychotropic medication has been shown to increase the risk of serious ventricular arrhythmias and thus, sudden cardiac death. Ray et al (Reference Ray, Meredith and Thapa2001) and Liperoti et al (Reference Liperoti, Gambassi and Lapane2005) showed that moderate doses of antipsychotics were associated with large absolute and relative increases in the risk of sudden cardiac death. Prolonged QT intervals reflect electrical dysfunction of the myocardium and may indicate predisposition to malignant tachycardias and sudden death. The QT interval is prolonged by a slow pulse and being female, and shortened by anxiety. Importantly, drugs and ischaemia can also prolong it. The corrected QT (QTc) gives a better indication of the risks by allowing for the pulse rate. There are various methods of calculating this, but the most commonly used is the Bazett's formula (Box 1) because of its relative simplicity, despite inaccuracies associated with heart rate. Failure to identify a prolonged QT leaves patients at risk of sudden death.
Recent work by Minerotti et al (2006) has shown increased QTc intervals in healthy men with neurotic personality traits, in alcohol dependence syndrome (Reference Borini, Terrazas and Ferreira JuniorBorini et al, 2003), and in incident diabetics (Reference Carnethon, Prineas and TemprosaCarnethon et al, 2006). The new consensus statement on high-dose antipsychotic medication from the Royal College of Psychiatrists (2006) recommends assessing cardiovascular risk with electrocardiogram (ECG) monitoring prior to use of antipsychotic medication to reduce risk of arrhythmias – we presume this has increased awareness and ordering of ECGs. Proper monitoring of QTc interval may detect prolongation and reduce occurrence of potentially lethal cardiac arrhythmias.
In this context, doctors have come to be more dependent upon computer ECG interpretation. The reliability of such programs has not been proven (Reference Willems, Abreu-Lima and ArnaudWillems et al, 1991). Standards regarding the accuracy of these readings were developed in the 1980s, but they have been largely ignored. Recent work in this area (Krishnan et al, 2006) has highlighted their deficiencies. The British Heart Foundation (2005) advises that computer-assisted ECG interpretation can identify important anomalies, but errors are common and interpretation should not be accepted without visual inspection. Electrocardiogram departments and cardiologists lack the capacity to provide a QTc validation service. We thus feel that psychiatrists should be competent in this skill – the Royal College of Psychiatrists recommended this in a consensus statement on high-dose antipsychotic medication (Royal College of Psychiatrists, 2006).
Box 1. QTc calculating formula
Bazett's formula:
QTc, QT interval corrected for rate; RR, interval from the onset of one QRS complex to the onset of the next QRS complex, measured in seconds.
Bazett's formula over-corrects at high heart rates and under-corrects at low heart rates, but it is widely used in clinical practise because of its simplicity.
In a small study, Warner et al (Reference Warner, Gledhill and Connell1996) reported that less than 20% of psychiatric trainees were able to identify a prolonged QT interval on an ECG. Moreover, studies in medical and surgical specialties have shown lack of elementary knowledge of ECGs among non-psychiatric doctors (Reference Montgomery, Hunter and MorrisMontgomery et al, 1994). Ten years on from the publication of Warner et al's study we aimed to find out how much psychiatric clinicians knew about interpretation of aspects of an ECG of immediate clinical relevance.
Method
The study was carried out in London (Oxleas National Health Service (NHS) Foundation Trust) and Manchester (Bolton, Salford and Trafford Mental Health NHS Trust) hospitals, over a 6-month period. Both consultants and trainees in psychiatry were approached with a short questionnaire.
A pilot study produced deceptively good results, as participants took the questionnaires away and filled in researched, perfect answers. Therefore, in the proper study, we asked participants to fill out a semi-structured questionnaire (nine questions in total; see online data supplement 1) in approximately 10 minutes, with the researcher present. Each participant was presented with this questionnaire and a copy of an ECG of a healthy person (online data supplement 2) with instructions to calculate the rate, mark out the QT interval and calculate the QTc. The questionnaire (one side of an A4 sheet) comprised basic questions about grade, post-graduate training in other specialties, medication on which they monitored ECGs and calculation of rate, QT and QTc – all questions considered most relevant in the literature and clinical practice. We did not insist on exact calculation of the QTc, which would have required a calculator, but accepted the answer as right if the formula was written down. The normal ECG used showed a heart rate of 66 beats per minute with a QT interval of 0.38 seconds. We used the Bazett's formula to calculate the QTc, which was 0.39 seconds.
We aimed to approach 100 doctors and to get roughly equal numbers of senior house officers v. specialty registrars and consultants. As senior house officers congregated at the Member of the Royal College of Psychiatrists (MRCPsych) course teaching it was easy to get them to fill out the forms and return them between lectures. Things were more difficult with consultants and a number of questionnaires were left uncompleted as we were asked to return later to collect them. Our responses from consultants for non-participation varied: some did not have the time, some felt it was not relevant to them, and some gave no explanation at all. A total of 49 senior house officers in psychiatry, out of 64 approached (77%, pre-membership), 8 out of 10 specialist registrars (80%) and 5 out of 26 general adult, old age, forensic and learning disability consultants (19%) agreed to complete the semi-structured questionnaire (total response rate 62%). As copies of the same ECG of a healthy person verified by a cardiologist was used, there were no uncertainties about the rate, QT interval and QTc.
Results
No statistically significant differences were noted in responses between hospitals in the two cities and the data was pooled.
Using Fisher's exact test, subgroup analysis showed that clinicians with previous experience in other medical specialties were significantly more likely to calculate the heart rate correctly (P=0.0193, Fisher's exact test). However, they were no more likely to read ECGs themselves or able to perform QT interval indication/calculation (P=1) than those with no medical experience.
Specialty registrars and consultants were significantly less likely to read ECGs and calculate the heart rate correctly themselves (P=0.0245, Fisher's exact test) than senior house officers (the small number of participating consultants severely limits the validity of these conclusions). QT interval indication/calculation was equally poor for both groups.
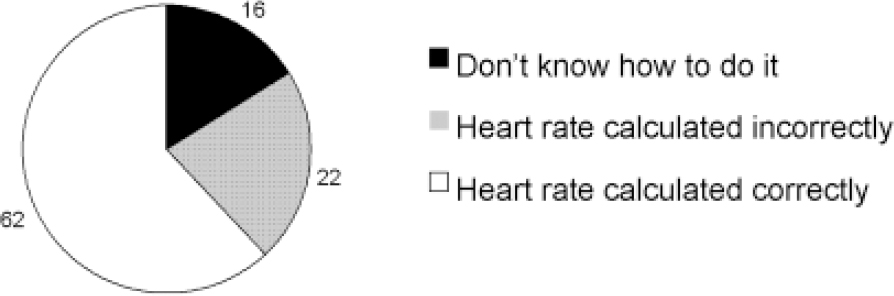
Fig. 1. Heart rate calculation (%).
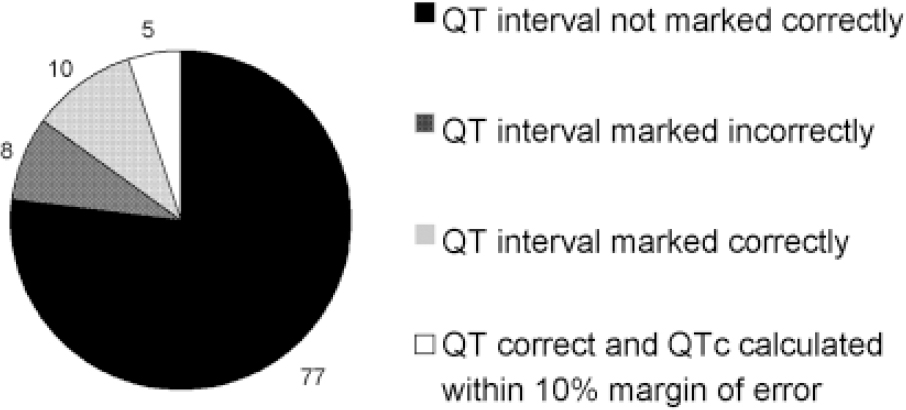
Fig. 2. QT interval calculation.
General questions
About three-quarters of respondents felt the questionnaire had highlighted deficiencies in their knowledge (Table 1).
Table 1. Overview of ECG interpretation by psychiatric clinicians
| Parameter | Percentage of respondents (n=62) |
|---|---|
| Pre-membership trainees (senior house officers) | 79% |
| Post-membership psychiatrists (specialty registrars & consultants) | 21% |
| Previous experience in medicine/on accident and emergency wards | 38% |
| Regularly monitored ECGs on patients | 83% |
| When monitoring ECGs, | |
| Read ECGs themselves | 69% |
| Rely exclusively on computerised readings | 31% |
| On what psychotropic classes was ECGs monitored | |
| Antipsychotics | 78% |
| Antidepressants | 70% |
| Lithium and mood stabilisers | 23% |
| Clozapine therapy | 22% |
| Features checked | |
| Heart rate and rhythm | 56% |
| Ischaemic changes | 61% |
| QT interval | 70% |
| Not confident about ECG interpretation | 72% |
Calculations
The respondents’ ability to calculate heart rate and QT interval on the ECG is shown in Table 2 and Figs. 1 and 2. Only 62% of respondents calculated the heart rate correctly and 5% correctly indicated/calculated QTc using Bazett's formula.
Table 2. Calculation of heart rate and QTc
| Parameter | Percentage of respondents (n=62) |
|---|---|
| Heart rate calculation correct (margin of error — 10%) | 62% |
| Heart rate incorrect | 22% (16% did not calculate) |
| QT interval marked on ECG | 23% |
| QT interval marked on ECG correctly | 15% |
| QTc indicated correctly (margin of error — 10%) | 5% |
Presentation of the findings and discussion with colleagues at an Oxleas NHS Trust audit meeting brought forward suggestions that psychiatrists could not be expected to read ECGs and that they should depend on automated readings and on general practitioners to provide physical healthcare (including interpreting ECGs).
Krishnan et al (2006) suggest overreading of 12 lead ECGs is required to circumvent errors of computerised ECG interpretation. In light of this, we undertook a further audit of ECG tracings of machines used by the Oxleas NHS Foundation Trust, looking at the accuracy of the measurement of QT intervals. Fifty-three consecutive ECGs performed on three of the Trust's five Mortara Eli 250 electrograph machines (which use Mortara's Veritas analysis algorithm for interpretation) were reviewed. We found that on a sample of 53 consecutive ECGs, seven QT intervals were incorrectly measured. Thus, 13% of the sample of Trust ECG machine QT reports were inaccurate and 6% had underestimated QT interval.
Discussion
This study suggests that knowledge of role of ECGs and the interpretation of heart rate, QT interval measurement and QTc calculation is unsatisfactory among psychiatrists. The study was carried out across teaching and non-teaching settings in a sample we expect is representative of UK psychiatrists generally, though several consultants did not participate for various reasons, which may limit the generalisation of findings. Our sample size of 64 respondents was more than twice the size of the earlier study of psychiatric trainees by Warner et al (Reference Warner, Gledhill and Connell1996). Our response rate was 62% compared with 97% in the earlier study. We endeavoured to cover all trainees and consultants in the participating hospitals, but were limited by the nature of our criteria, namely that the specified questionnaires be completed and returned immediately to the researchers. There were statistically significant differences between the trainee and consultant groups, but the small number of consultants could affect validity.
Most respondents were aware of the need to monitor ECGs, but a significant proportion was unable to calculate heart rate and measure QT intervals. These findings replicate those of previous studies (Reference Montgomery, Hunter and MorrisMontgomery et al, 1994) of doctors working in acute medicine, in which 24% of doctors correctly identified the QT interval, as well as a study of psychiatrists in training (Reference Warner, Gledhill and ConnellWarner et al, 1996) in which 20% of the sample identified prolonged QT intervals correctly. We expected that the increased awareness of the cardiotoxicity of psychotropics and interaction between medications would have made psychiatrists more adept at QT interval and ECG abnormality interpretation, but this study indicates that the problem remains.
As reviewed in the introduction, evidence suggests that it is important to monitor QT intervals and ECGs in high-risk patient groups. The British Heart Foundation has presented good evidence, in line with the Oxleas Trust audit, that computerised readings of ECGs are not completely reliable. Data suggest that the type of error made by computerised ECG recording includes dangerous underestimation of the QT interval. Requesting other clinicians to check all ECGs will have huge resource and time implications. We therefore think it essential that psychiatrists improve their skills in this important area. The view that psychiatrists monitor mental health and do not have time to provide holistic care is potentially dangerous. O’Brien & Oyebode (Reference O'Brien and Oyebode2003), acknowledging that widespread monitoring of the psychiatric population is difficult, suggested that some interested psychiatrists may do more of this work than others. We argue that ECG interpretation is a basic medical skill and calculation of rate, rhythm and QTc measurement are relatively straightforward and deserve to be carried out within existing services (for a short instruction on how to interpret ECGs see online data supplement 3).
The statement on high-dose antipsychotic medication published by the Royal College of Psychiatrists (2006) calls for training in ECG interpretation for clinicians, and also for ready access to a cardiologist for interpretation. This need is being addressed in some ways by the introduction of an ECG interpretation Observed Standardised Clinical Examination (OSCE) station in the MRCPsych exam and could be one reason for improved knowledge of ECGs among senior house officers compared with consultants. Introduction of mandatory ECG teaching for psychiatrists in training and refresher courses for consultants is one way forward and will help improve the care of our patients.
Declaration of interest
None.







eLetters
No eLetters have been published for this article.