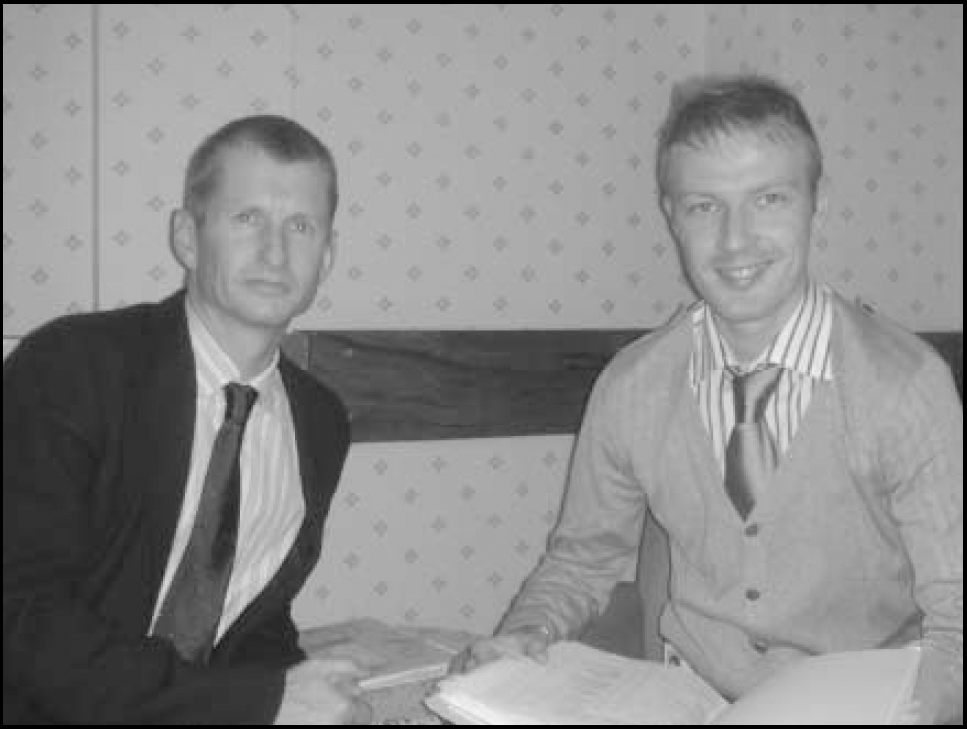
The Foundation Programme is a 2-year programme in the UK which forms the bridge between medical school and specialist/general practice training. It provides trainees with a broad range of experiences enabling them to apply for specialty training at an earlier stage. J.K., consultant psychiatrist in old age psychiatry, tells us about the experiences of hosting a Foundation Year 1 (FY1) doctor for the first time and the first incumbent G.T. (FY1) adds his views.
Development of the post from a consultant's perspective
Training of medical staff has always been a core activity of Lancashire Care National Health Service (NHS) Foundation Trust. There have never been pre-registration house officers in psychiatry and we were delighted to be approached with the concept of developing an innovative FY1 post in elderly psychiatry. Although we knew of Foundation Year 2 (FY2) posts developed from more traditional senior house officer roles, the FY1 post was unique in that we had no mental health reference points to guide us in its establishment. Review of traditional roles of the pre-registration house officer helped us draw parallels between the training objectives of trainees in medicine or surgery and those in psychiatry. The Foundation Year curriculum inspired confidence that this training opportunity could meet those objectives.
The FY1 post was developed within a multidisciplinary team. Clinical responsibilities were confined to the in-patient unit but experience of how complex health and social service provision is delivered was encouraged throughout. Skills of history taking, physical examination, documenting, preparation for team meetings, arranging investigations, developing management plans and referring to others are not unique. Older adult mental health does, however, provide specialist expertise in the assessment of confusion, the management of challenging behaviour, informant history taking and other communication skills, risk assessment, assessment of capacity and best interest decisions. A valuable induction is provided for all trainees including mental state examination, risk assessment, the Mental Health Act, personal safety and breakaway techniques.
Developing such a post has posed various challenges, such as ensuring the availability of senior supervision at all times, policies not permitting independent prescribing and mental health nurses lacking familiarity with FY1 competence. The time spent on supervision has been repaid by the contribution to continuity of care as senior trainees are drawn away from it with shift systems and training. The incorporation of a new trainee has facilitated the involvement of more senior trainees in training and the FY1's educational objectives inspired us to raise standards and perform in areas such as audit.
Our ambitions have been to provide an opportunity for nascent psychiatrists to experience the specialty before the Core Trainee choice and, more importantly, to instil recognition that a large proportion of all clinical care is for older adults with mental health disorder. Understanding this and grasping how to identify that disorder, conduct initial assessment and access services will serve our trainees and their patients well.
A trainee's perspective
As an undergraduate I was interested in psychiatry and was delighted to be accepted for this new psychiatry FY1 placement.
Foundation Year 1 and 2 trainees are assessed with direct observation of procedural skills, clinical evaluation exercise (mini-CEX), case-based discussion and multisource feedback (mini-PAT). I had no problems completing mini-CEX and case-based discussion because of the weekly educational supervision sessions. I was encouraged to experience other services within a multidisciplinary team, hence the multisource feedback was truly multidisciplinary. I was able to appreciate what each discipline brings to care and when, why and how they are accessed. Regarding direct observation of procedural skills, only simple procedures could be undertaken, although the same standards were achieved in general regardless of complexity.
Achieving the overall ‘generic’ competency standards did not pose any problems, although ‘acute care’ competencies were challenging. For mental health problems, the senior house officer would take responsibility. For physical problems, I found there was the limitation in treating physical problems in the psychiatric setting. I felt that not having on-call commitments and the Trust guidelines not allowing independent prescribing was restricting; however, subsequent feedback from senior colleagues has shown that overall development has not suffered.
On reflection, I have enhanced my patient-centred approach by appreciating the circumstances of those with mental health problems. I have been able to discuss psychiatric referrals of variable quality and have been able to educate others where a mental health multidisciplinary team opinion might be of value, who in the multidisciplinary team can best provide this and what information adds to the quality of their response. I also appreciate why physical problems receive limited treatment in psychiatric settings. A growing number of doctors working in diverse specialties will increase understanding of how others work, leading to better working relationships and ultimately improving care.
The new training structure in the UK has received criticism, but my experiences have converted me to be its cautious welcomer. I await my application to psychiatry specialty training with interest.
Declaration of interest
None.



eLetters
No eLetters have been published for this article.