Anorexia nervosa is a not uncommon disorder in adolescents and young adults (Reference HoekHoek, 1991). It varies widely in severity, but is usually associated with considerable disruption, suffering and morbidity, both psychiatric and physical. Furthermore, it has one of the highest mortalities of any functional psychiatric disorder (Reference Neilsen, Moller-Madsen and IsagerNeilsen et al, 1998). It is often difficult to manage within general services and new specialist services are being created throughout the country (Reference Palmer and TreasurePalmer & Treasure, 1999).
People suffering from anorexia nervosa are sometimes portrayed as ‘difficult’ patients. Certainly they are characteristically wary and have mixed feelings about treatment and change. The typical sufferer may hate the state in which she finds herself, but nevertheless she may be very fearful of what might happen were she to loosen the tenuous control which eating restraint seems to give her. The clinician who tries to help cannot simply apply treatments in an instrumental fashion. Treatment requires an adequate working alliance with the patient. The construction and maintenance of such an alliance may well be the most demanding part of the treatment process (Reference PalmerPalmer, 1996).
Such difficulties have probably contributed to the relative dearth of good evidence about what treatments are and are not effective in this disorder. There are few randomised controlled trials and the results are difficult to generalise (Reference Russell, Szmuckler and DareRussell et al, 1987; Reference Crisp, Norton and GowersCrisp et al, 1991). Systematic observational studies could provide another kind of evidence but these too are largely lacking as yet (Reference Treasure and KordyTreasure & Kordy, 1998). The worried clinician has to rely for advice mainly upon the accumulated experience and views of those who claim to know about these things. They do not always speak with one voice. Those who would plan rational services do not have much to go on.
The Leicester Eating Disorders Service is a specialist secondary service which takes adult patients (aged 16 years and above) from a defined catchment area of just under 1000 000. It accepts some referrals from afar, but the present study reports data only on patients who came from the catchment area. Most such patients are treated as out-patients. However, there is the facility to admit patients to an in-patient regime based in a general psychiatric ward. At any one time there would usually be several patients with anorexia nervosa on the ward. In the main, admission is offered as an additional form of management to people who have failed to respond to out-patient therapy. Moreover, it would be usual for the same out-patient therapist on the team to continue to see the patient through her stay in hospital and indeed throughout their career as a patient within the service. The relationship with the therapist may be thought of as the ‘carrier wave’ onto which other interventions are added as required. In terms of weight gain, the aim of admission — and indeed of treatment in general — is to attain and maintain a ‘plateau weight’ corresponding to a body mass index (BMI) of around 20 kg/m2.
The Leicester service is well established and has been running in broadly its present form for over a decade. It is different from both the many newer local services which have been established more recently around the country and from other older, but predominantly tertiary, services. It is hoped that these data from Leicester may serve as some guide to the level of service consumption that might be anticipated in the treatment of cases of anorexia nervosa arising within a catchment area based service for adults.
Method
The subjects of the study were local patients presenting consecutively to the service with a diagnosis of anorexia nervosa. Such diagnoses had been made according to the DSM criteria current at the time. However, cases were rediagnosed from the case notes according to DSM-IV criteria (Amercian Psychiatric Association, 1994) and none were excluded by this process. Only those with full syndrome disorders were included. People who were referred from outside of the catchment area were excluded.
For the examination of the rate of admission, the cohort consisted of all local patients for whom at least one year had passed by the time of study. It would be unusual for a patient to be admitted for the first time more than a year after their first contact with the Service.
For the examination of the total service consumption, a subgroup of subjects presenting before 31 March 1994 was studied. This allowed for a study period of at least four years. Case notes were examined to count up the following indices of service consumption — total time in contact, number of individual sessions, number of admissions and number of days spent in hospital. Individual sessions were defined as any contact or interview recorded in the case notes. Recorded sessions included initial assessment appointments, therapy sessions and other meetings for a variety of purposes. However, most appointments for most patients would be appropriately described as therapy sessions. The service is multidisciplinary and all clinicians of whatever discipline, except for ward-based nurses, record their sessions in the same notes. Body weight as BMI was used as a crude index of initial severity and outcome.
Results
The larger cohort presenting consisted of 106 patients. Of these, 31 (29%) were admitted at some stage in their career. The mean BMI at first admission was 13.5 (s.d.=1.9) kg/m2 compared with 14.6 (s.d.=1.5) kg/m2 at presentation since most of those admitted had first failed to progress with a trial of out-patient therapy. The mean BMI at discharge from first in-patient care was 18.5 (s.d.=2.3) kg/m2. All patients gained weight in hospital and only eight patients failed to achieve a BMI of at least 17.5 kg/m2 by the time of discharge.
There were 78 patients in the smaller cohort presenting up to 1994. All but five were female, and their ages ranged from 16-51 (mean 23.2). Of this group 23 (30%) were ever admitted. Of these 78 patients, 14 (18%) attended five or fewer appointments and were considered to have not engaged in treatment. Table 1 shows the mean BMI at presentation and at last contact and indices of service consumption for the 64 patients who did engage, classified into those who were ever admitted (n=23) and those who were never admitted (n=41). Of those who were ever admitted, 12 were admitted more than once. Figure 1 shows a scatter plot of BMI at presentation and BMI at last contact with the service for this cohort. None of the subjects died while in touch with the service.
Table 1. Mean service consumption and body mass index (BMI) for cohort of patients admitted up to 1994(n=64)(those seen less than six times excluded)

| BMI at presentation | Total months in hospital | Total sessions | Months in contact | BMI at end of contact | |
|---|---|---|---|---|---|
| Ever admitted (n = 23) | 14.6 (± 1.5) (13.6 at first admission) | 9.8 | 106.6 | 49.8 | 18.0 (± 3.5) |
| Never admitted (n = 41) | 15.6 (± 1.4) | 0 | 31.6 | 26.1 | 18.0 (± 3.2) |
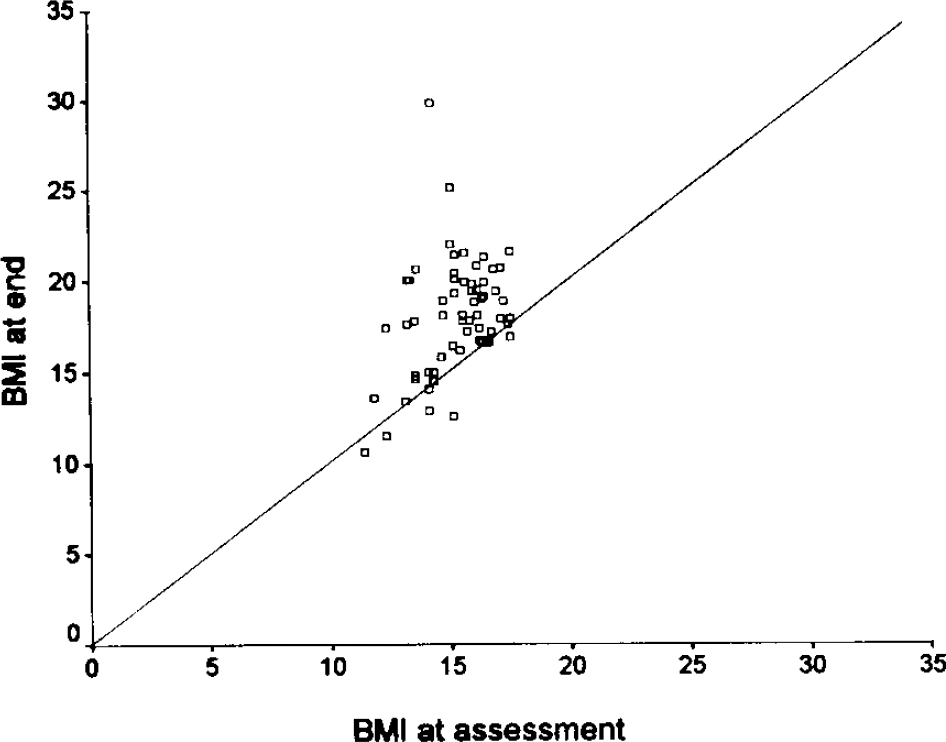
Fig. 1. Body mass index (BMI) at the beginning and end of contact with the service (n=64)
Discussion
The indices of service consumption used in this study are crude. The patients were wholly under the care of the Eating Disorders Service and typically there would have been little contact with other secondary psychiatric services. However, some contacts may well have gone unrecorded and this would certainly be the case for nursing interviews with in-patients. Furthermore, the contact counts take no account of the length, nature or probable cost of the sessions. The figures given are therefore likely to be underestimates and are certainly rough and ready. Nevertheless, there are few similar data available in the literature.
The index of outcome used in this study is even cruder. There is much more to recovery from anorexia nervosa than change in weight. However, weight change is necessary although not sufficient for recovery and it has the advantage of being easy to measure reliably. Most patients made progress while in touch with the service. The mean BMIs at last contact for both the ever admitted and never admitted groups were 18 kg/m2 and thus just about within the normal range. However, as the scatter plot demonstrates, the means hide considerable variation and some patients remained at low weight.
The news about service consumption is mixed. In this study, just under three-quarters were managed with out-patient treatment alone. However, nearly a fifth did not engage in significant treatment. On average, those out-patients within the pre-1994 cohort (who stayed in contact for at least five appointments) received 32 sessions. By contrast the minority from the same cohort who required admission received on average 107 sessions — over three times as many — and were in contact nearly twice as long. However, they had a similar final outcome of their contact in terms of weight.
Admissions were long but usually led to successful weight restoration. However, half of the admitted cohort came into hospital more than once. The average total cost of treatment for the ever admitted group was probably 20 times or more the cost of that of the never admitted group. To a degree, this marked bimodality reflects the policy of the service which tends to reserve admission for those who fail to progress with out-patient care but to go for full weight restoration for those who are admitted. Such full restoration takes time. If someone weighs 30 kg and gains to say, 53 kg, weight restoration alone may well take six months. We have recently developed a special day programme for severe anorexia nervosa with the aim of cutting our overall use of in-patient care by avoiding some admissions and cutting the length of others. This seems to be working well but it is too soon for any formal evaluation.
Services for people with anorexia nervosa need to provide for both the substantial needs of the majority of patients who can be managed as out-patients and to consider how best to provide for those whose needs seem even greater. Innovation and variety of provision is to be welcomed in the present limited state of knowledge but it should be accompanied by documentation and evaluation.





eLetters
No eLetters have been published for this article.