- ACSM
American College of Sports Medicine
- CDC
Centers for Disease Control and Prevention
- HRmax
maximum heart rate
For over half a century CVD has been the number one cause of death in Europe, accounting for approximately half all deaths(1). Its causes lie in a combination of genetic, environmental and lifestyle factors. Given that the human genetic makeup has not altered substantially since Stone Age times(Reference Booth, Chakravarthy and Gordon2), the increased prevalence of CVD deaths in relatively recent years must be a result in considerable part of the influence of environmental and lifestyle changes, including increased urbanisation, growth in industry and technology and the abundance of high-fat energy-dense foods.
Daily energy expenditure has decreased as society has progressed from agrarian to industrial, to service and most recently to information-based economies(Reference Grilo, Brownell, Stunkard, Stunkard and Wadden3). This change has resulted in decreased energy expenditure through physical exertion from approximately 84 kJ (20 kcal)/kg body weight per d for hunter–gatherers to <21 kJ (5 kcal)/kg body weight per d for modern sedentary Western populations, a fourfold differential(Reference Eaton, Strassman and Nesse4). However, modern man is not evolutionarily prepared for a sedentary existence(Reference Blair and Dishman5), ‘resembling Stone Age hunter–gatherers displaced through time to a world that differs from that for which the genetic constitution was selected’(Reference Eaton, Konner and Shostak6). This mismatch between biology and lifestyle fosters the development of degenerative diseases(Reference Eaton, Strassman and Nesse4), with CVD being a prime example.
The national decline in physical activity levels, often attributed to increasing sedentary work patterns, increased use of automotive transport, the development of labour-saving devices in the home and an increase in sedentary leisure pursuits, has been mirrored by an unprecedented rise in the incidence of obesity and non-communicable diseases such as hypertension, CHD, non-insulin-dependent diabetes mellitus and certain cancers(Reference Carmichael7). At a societal level this situation has placed an augmented burden on the National Health Service; recent statistics suggest an estimated cost of £1.06×109/year with 35 000 deaths directly associated with a lack of physical activity(Reference Allender, Foster and Scarborough8). Physical activity prescription designed to prevent premature morbidity and mortality has become an imperative issue for both government and society. Many expert bodies have attempted to translate the evidence from the scientific literature into physical activity guidelines that can be disseminated to the general population in an effort to increase physical activity levels for the health of the nation. The purpose of the present paper is to provide an overview of the development and evolution of current physical activity guidelines for nutritionists and healthcare professionals (a time line for the key exercise and physical activity guidelines is shown in Table 1).
Table 1. Time line showing key exercise and physical activity guidelines
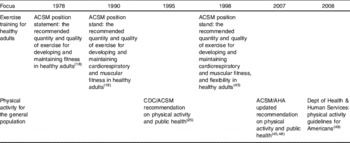
ACSM, American College of Sports Medicine; CDC, Centers for Disease Control and Prevention; AHA, American Heart Association.
History of physical activity prescription for health
The scientific associations between physical activity and health began with the emergence of results from epidemiological studies conducted during the 1940s, which directly compared sedentary and active subjects working in a similar environment. In this landmark study London bus conductors (working on double-decker vehicles) were found to have less CHD than bus drivers and civil service postmen less CHD than telephonists, executive officers and clerks(Reference Morris, Heady and Raffle9, Reference Morris, Heady and Raffle10). These findings led to the hypothesis that men in physically-active jobs suffer less CHD and IHD than comparable men in sedentary jobs; such disease that active individuals do develop is less severe and strikes at later ages(Reference Paffenbarger, Blair and Lee11). The benefits of vigorous activity were extolled in a study conducted in the late 1960s that involved 16 822 male civil servants. It was found that for men who perform vigorous exercise the relative risk of developing coronary disease is about one-third of that in comparable men who do not perform vigorous exercise(Reference Morris, Chave and Adam12). Similarly, in a follow-up study of 17 944 middle-aged male office workers in the civil service the incidence of CHD in the subsequent 8·5 years for men who had engaged in vigorous sport and keep-fit during the initial survey was found to be less than half that of their colleagues who had recorded no vigorous exercise(Reference Morris, Everitt and Pollard13).
Further evidence of reduced morbidity and mortality as a result of an active lifestyle has been demonstrated among US postal workers(Reference Kahn14), railroad men(Reference Taylor, Klepetar and Keys15) and longshoremen(Reference Paffenbarger, Laughlin and Gima16). Thus, the notion that occupational physical activity is inversely associated with cardiac events was established. However, given the nature of these cross-sectional studies a causal relationship between physical activity and CHD could not be established.
Following this pioneering work, epidemiologists used cohort studies to further define the associations between physical activity and health. Studies on a population of Harvard University male alumni who entered college during the years 1916–1950 have examined the role of physical activity in protecting against heart disease. The first 16-year follow-up study, which examined 16 936 graduates aged 35–74 years, concludes that the risk of first heart attack is inversely related to energy expenditure(Reference Paffenbarger, Wing and Hyde17). Stair-climbing, walking, strenuous sports and composite physical activity were all found to show reduced risk. Alumni who reported fewer than five flights of stair-climbing daily were found to be at 25% increased risk of heart attack over those who climbed more daily during the follow-up interval; alumni who walked fewer than five city blocks (or equivalent) daily were found to increase their risk of heart attack by 26% over the risk of those that walked more and the men who reported no strenuous sports play were found to be at 38% greater risk of heart attack than those men who engaged in strenuous sports.
The important associations from these epidemiological studies, which were recognised by the first International Olympic Committee medal to the principal researchers in 1996, allowed the firm conclusion that regular lifelong physical activity provides health benefit. However, despite this conclusion many questions remained unanswered. Further research was required to determine the ‘dose’ for the prescription of physical activity to elicit maximum protection against the development of CVD, in terms of the frequency, intensity, duration and best type of physical activity.
1978 American College of Sports Medicine position statement
The first guidelines on exercise were issued by the American College of Sports Medicine (ACSM) in 1978. These guidelines, the recommended quantity and quality of exercise for developing and maintaining fitness in healthy adults, outline the exercise that healthy adults would be required to perform in order to develop and maintain cardiorespiratory fitness(18). This requirement was defined as undertaking 15–60 min aerobic physical activity using large muscle groups on 3–5 d/week at an exercise intensity between 60% and 90% maximum heart rate (HRmax) or 50–85% maximal O2 consumption. These guidelines were largely based on short intervention studies (8–16 weeks) involving white male subjects.
Since these guidelines were issued several countries have sought to produce public health guidelines on physical activity. For the most part these guidelines have developed in line with and have drawn upon successive reviews of the scientific evidence by expert panels under the auspices of the ACSM.
1990 American College of Sports Medicine position stand
After 12 years the ACSM updated these guidelines. The 1990 guidelines recommend that on 3–5 d/week individuals should undertake between 20 min and 60 min moderate- to vigorous-intensity exercise (defined as 60–90% HRmax or 50–85% maximal O2 consumption). In addition, individuals are advised to perform resistance training consisting of one set of eight to twelve repetitions for each major muscle group ≥2 d/week(19). The key changes from the 1978 guidelines are: recommendations for resistance training are included; a distinction is made between the quantity and quality of exercise required for fitness and health benefits. It is noted that there is potential for health benefits from regular exercise performed more frequently and for longer duration, but at lower intensities than prescribed in the position stand. This document may be seen as the beginning of a shift away from an exclusively ‘performance-related fitness’ paradigm to one that includes activity recommendations for both performance- and health-related outcomes(Reference Blair, LaMonte and Nichaman20).
The important role of physical activity in health promotion was reinforced in the early 1990s when the burden of disease and injury attributable to physical inactivity was listed among the top ten risk factors endangering global health(Reference Murray and Lopez21). Notably, in 1992 the American Heart Association published a statement recognising inactivity as a risk factor for the development of coronary artery disease(Reference Fletcher, Blair and Blumenthal22). Despite these developments and the messages contained in both the 1978 and 1990 guidelines, physical inactivity continued to soar. It was demonstrated in epidemiological studies that a large majority (60%) of the US population were inadequately active and 25% were completely inactive(23). This rising tide of physical inactivity despite the existence of clear public guidance on the quantity and quality of physical activity required to maintain health led to a re-examination of the existing scientific evidence and an evaluation of new data that had emerged between 1990 and 1995(Reference Dunn, Andersen and Jakicic24).
1995 Centers for Disease Control and Prevention/American College of Sports Medicine physical activity recommendations and 1996 report of the US Surgeon General
In 1995 the Centers for Disease Control and Prevention (CDC) in collaboration with the ACSM issued a public health recommendation for physical activity(Reference Pate, Pratt and Blair25). The purpose of the recommendation was to provide a clear concise public health message that would encourage increased participation in physical activity among Americans of all ages by providing guidance on the types and amounts of physical activity required for health promotion and disease prevention(Reference Pate, Pratt and Blair25). This document was ‘intended to complement, not supersede, previous exercise recommendations’ and advised that ‘every adult should accumulate 30 minutes or more of moderate intensity physical activity on most days of the week’. Resistance training recommendations remain and guidelines for flexibility training have been added. Unique aspects are that the health benefits of moderate-intensity physical activity are emphasised, potential effectiveness of activities of daily living or ‘lifestyle activity’ for achieving health benefits are noted(Reference Phillips, Pruitt and King26) and accumulation of physical activity in intermittent short bouts are supported. As the target audience for the recommendation (the 40–50 million US adults who are sedentary and who account for much of the public health burden of chronic disease) are unlikely to have the physical capacity to engage in greater quantities of high-intensity physical activity, and because compelling evidence shows health benefits can be accrued with even more-moderate amounts and intensities of regular exercise, the CDC/ACSM report recommends a dose of physical activity that would likely be achievable by the primary target population(Reference Blair, LaMonte and Nichaman20). These recommendations have subsequently been adopted by numerous agencies(1, 27–32).
In 1996 the first report of the US Surgeon General on physical activity and health was published(23). This report reiterates 1995 CDC/ACSM guidelines relating to moderate-intensity exercise, but also emphasises the flexibility available in achieving these guidelines. It is suggested that the guidelines could be met by a 30 min brisk walk, 30 min lawn-mowing or raking leaves, 15 min run or 45 min playing volleyball. In other words, a combination and moderate- and vigorous-intensity exercise is seen as sufficient and thought to help individuals adapt exercise recommendations to personal preference and life circumstances. It is also stated that the additional health benefits could be attained through greater amounts of physical activity.
Inherent problems with 1995 guidelines
At the time of issuing the 1995 guidelines no randomised controlled trials on intermittent moderate-intensity physical activity had been published. The guidelines were largely based on indirect epidemiological evidence showing a link between physical activity and reduced risk of CHD and surmising that the activity is most probably performed in short bouts, e.g. stair-climbing, gardening and walking and cycling for personal transport. Furthermore, some direct empirical evidence was available that vigorous-intensity exercise performed in several bouts throughout the day can increase fitness(Reference Ebisu33, Reference DeBusk, Stenestrand and Sheehan34). This evidence raises some key questions relating to the 1995 CDC/ACSM guidelines: is moderate-intensity exercise enough; can exercise be accumulated.
The relationship between the intensity of physical activity and the incidence of major CHD events was studied in 4311 older British men 4 years after reporting no history of CHD, stroke or ‘other heart trouble’(Reference Wannamethee, Shaper and Walker35). The death rates per 1000 person-years for the ‘inactive or occasionally active’, ‘light activity’, ‘moderate and moderately-vigorous activity’ and ‘vigorous activity’ groups were found to be 18·5, 11·4, 7·3 and 9·1 respectively. It was concluded that vigorous activity is not essential for reduction in CVD risk and that even light activities such as regular walking and weekend recreation can bring a marked decrease in mortality for men >60 years. Similarly, a longitudinal study of older men has found an inverse association between relative intensity of physical activity and risk of CHD, even among men not satisfying current activity recommendations(Reference Lee, Sesso and Gurna36). The relative risk of CHD among men who perceived their exercise exertions as ‘moderate’, ‘somewhat strong’ and ‘strong’ or more intense was found to be 0·86, 0·69 and 0·72 respectively compared with ‘weak’ or less intense. Stronger evidence for the benefits of moderate-intensity exercise comes from a recent meta-analysis of twenty-four randomised controlled trials that have examined the effect of walking on fitness, fatness and resting blood pressure(Reference Murphy, Nevill and Murtagh37). Results show that walking interventions (mean intensity 70·1% predicted HRmax or 56·3% maximal O2 consumption) increase maximal O2 consumption and decrease body weight, BMI, percentage body fat and resting diastolic blood pressure in previously-sedentary adults.
The issue of whether several short bouts of exercise are as effective in influencing health outcomes as one longer session of the same total duration has often been debated by exercise physiologists. In the ‘classic’ epidemiological exercise studies already discussed many of the activities reported, such as stair-climbing, walking and cycling for personal transport, household tasks and gardening, were likely to have been performed intermittently in short bouts accumulated during the day. Evidence from the Harvard Alumni study lends further support to this notion. The subjects (n 7307) were prospectively followed from 1988 to 1993 and mode, frequency and average duration of exercise was reported. During follow-up 482 men were reported to have developed CHD. Longer sessions of exercise were not found have a different effect on risk compared with shorter sessions at similar total energy expenditures(Reference Lee, Sesso and Paffenbarger38).
A recent systematic review has examined sixteen published studies that have compared the training effects of continuous and accumulated exercise of the same total duration(Reference Murphy, Blair and Murtagh39). The available evidence suggests that, at least for fitness, accumulated and continuous patterns of exercise training of the same total duration confer similar benefits. For the effect of continuous and accumulated training on body composition, blood pressure, blood lipids and psychological well-being it is difficult to draw firm conclusions. However, it is likely that the strict inclusion criteria for the review precluded the inclusion of a number of studies that may add to this evidence base. Interestingly, there is emerging evidence that accumulating 13·5, 11 and 6 min bouts of vigorous stair-climbing activity in short bouts over the course of the day may also be effective(Reference Boreham, Kennedy and Murphy40–Reference Kennedy, Boreham and Murphy42). A further research question that remains unanswered is how short the accumulated bouts of exercise can be without diminishing the health benefits.
It would appear that since the publication of the 1995 activity guidelines evidence has accrued supporting the promotion of moderate-intensity activity that may be accumulated in short bouts over the course of 1 d.
1998 American College of Sports Medicine position stand
In 1998 the ACSM replaced the 1990 position paper with the publication of the recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults(Reference Pollock, Gaesser and Butcher43). Unlike the 1995 CDC/ACSM guidelines relating to physical activity and public heath, this 1998 ACSM position stand was aiming to provide exercise prescription guidelines for the many individuals involved in cardiorespiratory fitness and resistance training programmes and were designed for the middle-to-higher end of the exercise–physical activity continuum. It recommends that the healthy adult should engage in 20–60 min of continuous or intermittent (minimum of 10 min bouts accumulated throughout the day) aerobic activity at 55–65 (minimum) – 90% HRmax or 40–50 (minimum) – 85% maximum O2 uptake reserve or HRmax reserve on 3–5 d/week. It is suggested that duration is dependent on the intensity of the activity; thus, lower intensity activity should be conducted over a longer period of time (≥30 min) and, conversely, individuals training at higher levels of intensity should train for ≥20 min. In addition, resistance training involving one set of eight to ten exercises that conditions the major muscle groups and flexibility exercises that stretch the major muscle groups performed on a minimum of 2–3 d/week was recommended. The position stand stresses that the ACSM view exercise or physical activity for health and fitness in the context of an exercise dose continuum in that many important health benefits are achieved by going from a sedentary state to a minimal level of physical activity and programmes involving higher intensities and greater frequency or durations provide additional benefits(Reference Pollock, Gaesser and Butcher44).
Current physical activity recommendations
In the decade following the publication of the 1996 report of the Surgeon General physical inactivity remained a pressing public health issue, with less than half the US population achieving the CDC/ACSM physical activity recommendations(Reference Haskell, Lee and Pate45). Unfortunately, some of the general population at whom the recommendations were targeted did not understand or appeared to misinterpret the guidelines. Some individuals continued to believe that only vigorous-intensity physical activity would improve health while others believed that the light activities of their daily life were sufficient to promote health(Reference Porter46). A UK study has reported that 56% of men and 71% of women aged 25–65 years believe that moderate activity offers greater health benefits than vigorous activity and that moderate activity is recommended(Reference O'Donovan and Shave47). As a result of these findings, in 2003 an expert working group was established with the aim of updating the 1995 CDC/ACSM recommendations to provide a more comprehensive and explicit public health recommendation. These guidelines were simultaneously co-published in two leading journals(Reference Haskell, Lee and Pate45, Reference Haskell and Lee48) and, although they remain essentially unchanged from the 1995 recommendations, they are improved in several ways. In brief, the role of vigorous-intensity exercise is explicitly stated and adults are encouraged to combine moderate- and vigorous-intensity exercise to meet the minimum recommendation of moderate-intensity physical activity for a 30 min on 5 d/week or vigorous-intensity aerobic activity for 20 min on 3 d/week. Finally, the dose–response relationship between physical activity and health is reinforced, with individuals informed that they will probably benefit by exceeding the minimum recommended amount of physical activity. A summary of the guidelines is provided in Table 2.
Table 2. Summary of 2007 physical activity recommendations for adults aged 18–65 years (adapted from Haskell et al.(Reference Haskell, Lee and Pate45))

Meanwhile, following a review of the scientific data relating physical activity to health published since the release of the 1996 report of the Surgeon General on physical activity and health, revised US guidelines aimed at policymakers and health professionals were published in October 2008(49). These physical activity guidelines are designed to provide information and guidance on the types and amounts of physical activity that provide substantial health benefits. These guidelines reinforce the message of a dose–response relationship between physical activity and health found in the 1996 report of the Surgeon General and provide tailored guidelines for children and adolescents, adults, older adults, women during pregnancy and the postpartum period and adults with disabilities(49). Advice is also provided for ‘safe physical activity’ and ‘people with chronic medical conditions’. In relation to adults it is recommended that all adults should avoid inactivity and for substantial health benefits should do ≥150 min moderate-intensity or 75 min vigorous-intensity aerobic physical activity per week, or a combination of moderate- and vigorous-intensity aerobic activity. It is noted that for more extensive health benefits adults should increase their aerobic activity to 300 min moderate intensity per week or 150 min vigorous intensity per week. Muscle-strengthening activities on two more days per week are additionally recommended.
Conclusions
Physical activity prescription guidelines for public health have evolved markedly since the first guidelines were published in 1978. There is now firm evidence relating to the intensity, dose and duration of physical activity for improved fitness and cardiovascular health. The challenge that remains is imparting the knowledge contained in the current guidelines to the wider population whilst providing sufficient advice and support to sustain increased physical activity throughout the life cycle.
The future of physical activity research may shift towards considering the balance between active and sedentary behaviours in the daily lives of individuals. It has been suggested that leisure-time activity will be insufficient to prevent increasing population levels of obesity and chronic diseases, and it may be necessary to focus on decreasing sitting and increasing activity in transport and at work to restore the energy balance that resulted in a much-more-stable body weight at the beginning the 20th century than is evident today(Reference Brown, Bauman and Owen50).
Acknowledgements
The authors declare no conflicts of interest. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. The paper is based on the lecture presented by M. M., E. M. and M. M. were responsible for researching and writing the paper and A. M. wrote drafts of some sections of the paper. Both M. M. and E. M. reviewed and edited the paper.




