Introduction
Primary care has been identified by the World Health Organisation (2008) as a place to serve better health for people. In developed countries, primary care is driven by key practitioners, mainly general practitioners and community pharmacists (Phillips and Bazemore, Reference Phillips and Bazemore2010; Roland et al., Reference Roland, Guthrie and Thomé2012). General practitioners have a role to diagnose and issue prescriptions of which medicines can be dispensed by community pharmacists nearby.
Primacy healthcare in Thailand is mainly managed by a contracting unit for primary care (CUP), similar to a local health authority, which government hospitals are mostly contracted and funded by the National Health Security Office (NHSO). CUPs have a role to deliver primary care services, basically through primary care units (PCU), and arrange the referral of patients to higher levels of care if necessary. A PCU generally covers a population of 10 000–15 000 (Health Insurance System Research Office, 2012) and is routinely operated by several key health providers: a physician, a registered nurse and a public health practitioner. A dentist and a pharmacist are assigned to work at PCU occasionally (Sriwanichakorn et al., Reference Sriwanichakorn, Yana, Chalordech and Bookboon2015). Notably, despite this distinctive establishment of primary healthcare, quality of primary care services does not seem satisfactory (Tangcharoensathien et al., Reference Tangcharoensathien, Swasdiworn, Jongudomsuk, Srithamrongswat, Patcharanarumol, Prakongsai and Thammathataree2010).
While community pharmacy is one of primary care partnership in other countries, it has not yet been successfully incorporated in Thai national healthcare system. This could be achieved if the local CUP agreed to commission pharmacy services and remunerate them appropriately. As financial issues are one of the key mechanisms to drive the healthcare system an optimal rate of remuneration is doubtful. Several models were previously evaluated with most studies being relevant to screening for diabetes and hypertension via community pharmacies (Kessomboon et al., Reference Kessomboon, Lochid-Amnuay, Poungkantha and Putthasri2010; Sookaneknun et al., Reference Sookaneknun, Saramunee, Rattarom, Kongsri, Senanok, Pinitkit, Sawangsri and Deesin2010; Ploylearmsang and Soondon, Reference Ploylearmsang and Soondon2012). Another study examined administrative cost of managing common illness and some chronic diseases at community pharmacies, reporting the cost as low as 22.31 baht (£0.51) per visit (Chaiyasong et al., Reference Chaiyasong, Osiri, Hirunyapanich, Aphasrithongsakul and Satayawongtip2005).
Previous evidence reported that Thai people normally seek health advice and treatment for common illnesses from community pharmacies, such as fever/headache, pain, skin problems and ear-eye-nose-throat disorders. These services are paid for directly by the patient (Thomudtha et al., Reference Thomudtha, Waleekhachonloet, Sakolchai, Limwattananon and Limwattananon2012). Another study indicated that community pharmacies in Thailand deal with common illnesses daily (Tongrod et al., Reference Tongrod, Bunditanukul, Yotsombut, Sermsinsiri, Subthawee, Kaeochinda and Sumpradit2013) and Thai community pharmacists are allowed by law to manage these ailments at a community pharmacy including prescribing antibiotics if necessary (Saramunee et al., Reference Saramunee, Chaiyasong and Krska2011). This activity can be done because all licensed pharmacists received education to perform patient assessment and to prescribe medications in a community pharmacy as part of their pharmacy school curriculum. Medicine(s) selected for each patient must be complied with the framework of Drug Act 1967 (Food and Drug Administration of Thailand, 2009). However, admittedly, this practice could be varied among pharmacists.
Incorporating community pharmacy into the national health services with the regard of common illness management is assumed to be feasible. As aforementioned, an evaluation of service cost will be helpful for CUP to determine remuneration rate for such service. This study was to perform and compare unit cost of treating common illnesses between PCU and the community pharmacy.
Methods
We conducted a research using the primary care service of one educational institution where a PCU and a community pharmacy established within the campus. This PCU provides health services to academic residents (students and staff), free of charge, supported by CUP of the university hospital. The community pharmacy selected is managed like any other pharmacy business, concurrently serves the same populations, particularly students, but requires payment for services from the patient. This demonstrates that the selected primary care system is similar to the ones being available nationwide.
A unit cost analysis of common illness management was performed, from health provider perspective, using activity-based costing approach. The study was conducted in two primary care settings (a community pharmacy and a PCU) located in an educational institution. Target population was service users who experienced a common illness and visited these settings. Data were collected at two places for three months during August to October 2013 – prospectively at the community pharmacy and retrospectively at the PCU.
Common illness
A meeting of health professionals who worked for the PCU (a doctor and nurses) and the community pharmacy was set up to identify key common illnesses of interest. A companion book of common illness treatment for community pharmacists was used as a guide to the group meeting whether or not they would agree with those ailments to be included in the study. Group members discussed and made an agreement to choose the ailments which were frequently found in daily practice. Eventually, common illnesses of eight systems were incorporated as a focus of this study. These illnesses included upper respiratory system, gastrointestinal system, urinary system, reproductive health, musculoskeletal system, eyes and ears system, skin problems, and helminths and parasites. A community pharmacist has authority to provide assessment and therapy to common illnesses as listed in Table 1. The ICD-10 (the 10th revision of the International Statistical Classification of Diseases and Related Health Problems), which are relevant to those selected common illnesses was subsequently tracked and selected by researchers. A medical doctor revised all selected ICD-10 codes to ensure appropriateness of common illness classification for the use of recruiting patients at the PCU.
Table 1 Common illnesses identified at community pharmacies

Common illness management at community pharmacies
Pharmacy patients of the selected community pharmacy, normally present at the community pharmacy and provide details of their health problems. As a common practice, a community pharmacist investigates symptoms of the patient by asking some questions and assessing symptoms before making decision of which common illness they have. Community pharmacists, consequently, choose and dispense medicines as appropriate together with providing necessary advice. This practice is legal based on Thai pharmacy regulations. In summary, community pharmacists perform four functions for managing common illness; (1) interviewing and assessing patient, (2) choosing appropriate treatment, (3) dispensing and (4) providing advice (Figure 1).

Figure 1 Functions of common illness management
Recruitment of participants
During August to October 2013, research assistants stayed at the community pharmacy for several hours per day to invite participants to take part in the study. Pharmacy patients who experienced any of the eight common illnesses were invited, using a convenience sampling approach, to participate after the service was completed. Participants were informed about the purpose and details of the study. Written consent form was provided and signed, if they agreed to do so. All participants were followed-up at 3–14 days, depending on their problems, by telephone to ensure the efficacy of treatment provided by the community pharmacist. At the follow-up, participants were asked to self-report their symptoms – three choices were given; completely recovered, partially recovered and not recovered.
Common illness management at PCU
A PCU is administered by a university hospital, acting as a CUP, where this research was originally conducted. This unit is officially under the universal coverage scheme by the NHSO, a national insurer of Thailand. Patients living in this health authority area have to co-pay as little as 30 baht (£0.65), or perhaps free of charge, when they visit to receive care from the PCU. Care for common illness is generally composed of four functions: (1) patient registration by a nurse assistant, (2) pre-assessment by a nurse, (3) physical examination and diagnosis by a doctor and (4) drug dispensing and advice by a pharmacist (Figure 1).
Recruitment of participants
Data on patients who had one of the common illnesses at the PCU was collected retrospectively via an electronic database. Permission to access an electronic patient medical record was approved by the PCU director before the study. Patient visits recorded between August and October 2013 were drawn. Researchers screened and selected patients who were primarily diagnosed with the assigned ICD-10. Medicines and laboratory tests which were not related to managing the eight common illnesses were excluded from the analysis.
Economic analysis
Cost components
Direct medical cost of each illness was observed and captured at both settings; including material cost (MC) and labour cost (LC) related to the focal activity.
MC
MC covered expenses related to community pharmacy service or medical care, including medicines, laboratory tests and utilities. Items of medicines and laboratory tests used were listed and counted for each patient. Unit price of these medical materials was based on the inventory databases of community pharmacy and the PCU. Multiply the quantity of each medical material with its unit price to yield a medical cost for one patient. A summation of this cost obtained from all patients denoted the total medical cost. Divide this total medical cost by the number of patients diagnosed or assessed to project the medical cost per patient.
A sum of utility cost (electricity, water and telephone) was reported in a financial statement of both settings. Utility cost per minute was calculated. Duration of managing each illness was timed. Multiply the cost per minute with duration of service and the proportion of area utilised these utilities to demonstrate utility cost per patient.
LC
A monthly income of the community pharmacist was based on the salary of a full-time pharmacist of the selected community pharmacy. Standard monthly income for health professionals and staff working in educational institution was used as a reference to calculate LC of workers at the PCU because specific information for the personnel at the PCU was confidential. Standard working hours for the community pharmacists and PCU workers was ~160 h/month excluding overtime shift (four weeks×five days×8 h). Average time for managing common illness at both settings was measured using minute as a unit. Labour wage per minute was computed – multiplying this rate with an average service time to denote LC per each common illness (Table 2).
Table 2 Resource used and reference value
PCU=primary care unit.
a Cost of medicine and laboratory test was based on the amount of use. Conversion rate £1=45.92 baht (ref. date 27 July 2016).
b Administrative cost of community pharmacy was as of 47.5% of medicine price.
The unit cost of each common illness was calculated by summation of relevant MC and LC obtained previously. Sensitivity analysis was performed in two scenarios; (1) increasing the cost of medicines 10–30%, (2) replacing monthly income of a pharmacist and a doctor by the lowest [22 000 baht (£435.54) and 30 000 baht (£653.31), respectively] and the highest [30 000 baht (£653.31) and 100 000 baht (£2177.70), respectively] values generally reported publicly.
Cost per successful case at community pharmacy
Cost per a successful case was performed only at the community pharmacy setting. This was analysed by using the total cost and the number of completely recovered patients (successful outcome) as numerator and denominator, respectively.
Results
Participants
A total of 9141 visits were recorded at the community pharmacy. Of those, 775 visits (759 patients) were eligible and included in the study – representing 8.5% (775/9141) of all pharmacy visits. All participants were students and the majority were female (77.6%, 601/775). At the PCU, 6701 visits were captured with 60.4% (4048/6701) were students. Of those, 1545 visits were primarily diagnosed with at least one of the eight common illnesses – female was also predominant (70.4%, 1093/1545). This yields the prevalence rate of common illness was as high as 23.1% (1545/6701).
Distribution of common illness
Distribution of common illness was examined comparing between the community pharmacy and the PCU. Upper respiratory disorders were the most frequent, whereas helminths and parasites were the fewest. Patients with upper respiratory (51.9%) and eyes/ears (7.7%) were found significantly higher in the PCU (P-value<0.05). In contrast, patients experienced with musculoskeletal problems (23.6%) was more likely to be higher (P-value<0.05) in the community pharmacy. Gastrointestinal disorder, reproductive health and skin problem were found similarly between the two settings (Table 3).
Table 3 Distribution of common illness
PCU=primary care unit.
a Tested by χ 2.
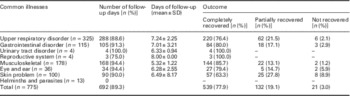
Treatment outcome for community pharmacy
Participants were followed-up at approximately one week by telephone after the pharmacy visit. Over two-thirds of participants (77.9%) self-reported that the symptoms were completely gone, whereas about one-fifth (19.1%) felt partially recovered. Musculoskeletal problem was the ailment frequently eradicated (85.7%) (Table 4).
Table 4 Treatment outcome from community pharmacy
Unit cost analysis
Figure 2 illustrates the unit cost analysis of common illness treatment. The unit cost at the community pharmacy, overall, was 69.39 baht (£1.51), ranging from 54.15 baht (£1.18) for musculoskeletal to 82.71 baht (£1.80) for skin problems. The unit cost at PCU was 128.35 baht (£2.79), ranging from 94.79 baht (£2.06) for eyes and ears to 229.00 baht (£4.99) for reproductive health. Cost of medicine, had impacted predominantly on the overall unit cost at both settings – 29.72 baht (£0.65) for community pharmacy setting (42.8% of the unit cost) and 44.71 baht (£0.97) for PCU (34.8% of the unit cost). The cost of other materials (such as laboratory tests and utilities) contributed greatly for the PCU [68.38 baht (£1.48), 53.3% of unit cost]. LC was the smallest cost component, 10.56 baht (£0.23) for community pharmacy, 15.2% of unit cost, and 15.26 baht (£0.33) for PCU, 11.9% of unit cost.

Figure 2 Unit cost of common illness management. PCU=primary care unit, CP=community pharmacy, conversion rate £1=45.92 baht (ref. date 27 July 2016)
Sensitivity analysis shows that the increase in medicine cost for 10–30% would elevate the unit cost for 4.3–12.8% at the community pharmacy and 3.5–10.5% at the PCU. The other two scenarios used the minimum and maximum monthly income generally reported for doctors and pharmacists to replace the LC variable. When the minimum value was used, the overall unit cost for managing common illnesses at the community pharmacy would decrease 1.8%, but increase 3.3% for the PCU. The maximum values would increase the overall unit cost 3.1 and 19.7% for the community pharmacy and the PCU, respectively.
Cost per successful case at community pharmacy
In overall, the total cost of common illness treatment at the community pharmacy was 53 758.53 baht (£1170.70). Since the number of participants who self-reported as completely recovered after the pharmacy visit was 539. Therefore, this denotes the cost as of 99.74 (£2.17) baht per a successful outcome.
Discussion
This present study has emphasised for a broad range of common illnesses but this list of ailments may be different from the pharmacy-based minor ailment scheme in the United Kingdom (Paudyal et al., Reference Paudyal, Watson, Sach, Porteous, Bond, Wright, Cleland, Barton and Holland2013), due to the difference in pharmacy practice. Common illnesses are fairly prevalent at the PCU, 23.1% over three months. High prevalence was also noted by other Thai studies (Thomudtha et al., Reference Thomudtha, Waleekhachonloet, Sakolchai, Limwattananon and Limwattananon2012; Tongrod et al., Reference Tongrod, Bunditanukul, Yotsombut, Sermsinsiri, Subthawee, Kaeochinda and Sumpradit2013) and in other countries (Neuberger et al., Reference Neuberger, Tenenboim, Golos, Pex, Krakowsky, Urman, Vernet and Schwartz2012; Wändella et al., Reference Wändella, Carlssona, Wettermark, Lordc, Carsc and Ljunggrenc2013). Although, the prevalence rate could not be ensured at the community pharmacy because of limited data, nonetheless, it is assumed to be quite high since 8.5% of pharmacy patients (775 out of 9141 visits) sought help regarding common illnesses.
Overall, the unit cost of common illnesses managed at the community pharmacy (69.39 baht or £1.51) was approximately half as much as the cost at the PCU (128.35 baht or £2.79). This trend is similar to the findings of one UK study, reporting the cost of consultation and follow-up of minor ailments at general practice (£82.34) was almost three times higher than that of community pharmacy (£21.60) (Watson et al., Reference Watson, Ferguson, Barton, Maskrey, Blyth, Paudyal, Bond, Holland, Porteous, Sach, Wright and Fielding2015). Other two studies employed a unit cost analysis of primary care services. One Canadian study evaluated direct cost of delivering services for minor acute illness in three types of primary care clinics, except in community pharmacies. Unit cost reported was varied ($24–$177 or £19.24–£142), depended on clinic type and illness (Campbell et al., Reference Campbell, Silver, Hoch, Ostbye, Stewart, Barnsley, Hutchison, Mathews and Tyrrell2005). The one from Portugal used a time-driven activity-based costing (TDABC) to evaluate cost of community pharmacy services. Authors reported costs of dispensing, counselling and health screening ranging from €1.24 to €4.55 (£1.07–£3.92), dispensing was the highest (Gregorio et al., Reference Gregorio, Russo and Lapao2016).
A bottom-up approach and activity-based costing was used in this study, which gives more accurate data. In summary, to calculate the cost, direct medical materials were quantified and multiplied by its quantity. Time of each activity was multiplied by rate cost of utilities and staff involved. This approach is similar to the method used by Gregorio et al. (Reference Gregorio, Russo and Lapao2016), a TDABC. However, they emphasised on service cost calculation such as interaction of pharmacist in medicine dispensing but medicine cost was unlikely to be included.
Capital cost was not included in this present study since it has no significant effect on cost calculation (Sookaneknun et al., Reference Sookaneknun, Saramunee, Rattarom, Kongsri, Senanok, Pinitkit, Sawangsri and Deesin2010; Ploylearmsang and Soondon, Reference Ploylearmsang and Soondon2012). As shown in Figure 1, service protocol at both settings were apparently different; patient care at the PCU involved four health professionals, while the pharmacist performed multiple tasks at the community pharmacy. Nonetheless, LC was likely to have the least impact on the unit cost. Other materials, laboratory cost and utility, tend to exhibit the effect. Notably, the LC proportion at the PCU was slightly lower than that of the community pharmacy since it was diluted by the greater value of unit cost.
Implication to practice and policy
A huge effort has been engaged by policy makers and researchers to incorporate community pharmacies into the Thai national health system. Two models of establishing community pharmacy as a public private partnership had been proposed since the universal coverage scheme was implemented nationally in 2001. Chaiyasong et al. (Reference Chaiyasong, Osiri, Hirunyapanich, Aphasrithongsakul and Satayawongtip2005) piloted to incorporate a community pharmacy into the universal coverage scheme, reporting administrative cost of 22.31 baht (£0.49) per visit. Sookaneknun et al. encouraged community pharmacies to provide screening service for diabetes and hypertension – supported testing devices by CUP. Authors reported the unit cost of this service was 351.7 baht (£7.66) (Sookaneknun et al., Reference Sookaneknun, Saramunee, Rattarom, Kongsri, Senanok, Pinitkit, Sawangsri and Deesin2010). Other two reports had also performed the unit cost analysis of screening and managing chronic health conditions at community pharmacy – 64.0 baht (£1.39) (Ploylearmsang and Soondon, Reference Ploylearmsang and Soondon2012) and ~180–1100 baht (£3.92–£23.95) (Kessomboon et al., Reference Kessomboon, Lochid-Amnuay, Poungkantha and Putthasri2010). All this evidence demonstrates that the unit cost of common illness management at a community pharmacy has never been explored.
So far, engaging a community pharmacy as a part of Thai National Health Service has not yet been accomplished. However, promotion of this service should continue due to the vast advantages of community pharmacies in the community. These advantages include location and longer operating hours (both weekdays and weekend), which increase accessibility to health service (Saramunee et al., Reference Saramunee, Krska, Mackridge, Suttajit, Richards and Phillips-Howard2014; Anderson and Thornley, Reference Anderson and Thornley2016). Our results provide policy makers with cost data that should lead to a payment scheme for community pharmacies providing primary care services. If they were to be contracted as a service node for common illness, we would propose the remuneration rate for community pharmacy as of 80–100 baht (£1.74–£2.18) per visit. This proposed charge is ~15 times cheaper than the pharmacy-based management of minor illness in the United Kingdom, reported unit cost of £29.30 per pharmacy visit (Watson et al., Reference Watson, Holland, Ferguson, Porteous, Sach, Cleland, Bond and Wright2014). This is because of the lower living cost in Thailand. However, if screening and managing chronic health conditions would be inclusive, then the remuneration rate would need reconsideration since reported unit cost was varied (Kessomboon et al., Reference Kessomboon, Lochid-Amnuay, Poungkantha and Putthasri2010; Sookaneknun et al., Reference Sookaneknun, Saramunee, Rattarom, Kongsri, Senanok, Pinitkit, Sawangsri and Deesin2010; Ploylearmsang and Soondon, Reference Ploylearmsang and Soondon2012).
From the above epidemiologic information and Thai pharmacy regulation (Food and Drug Administration of Thailand, 2009; Saramunee et al., Reference Saramunee, Chaiyasong and Krska2011), community pharmacy has the potential to be contracted by a local CUP to commission a service for common illnesses with reasonable reimbursement. Moreover, a specific suggestion can be possibly proposed to the university board, where this study was conducted. Since it is clear that students are the key users of the university primary care. Therefore, a primary care system might be established with incorporation of community pharmacy provision to help increase accessibility and reduce healthcare burden of students.
Limitation
Some limitations exist in this study. Using both retrospective and prospective data collection concurrently may diminish the power of comparative analysis. However, the by comparison could be possible since data were collected within the same period of time. Selection bias may exist due to the use of convenience sampling, especially for participants included in the community pharmacy setting. In addition, people who perceived themselves of getting serious symptoms (or more anxious patients) might prefer to attend the PCU. Clinical effectiveness of treatment at the PCU was assumed to be acceptable, though not observed, because the care was conducted by a doctor. The results of this study may be applied for implementing in other educational health service. However, generalisability should be annotated if the service is to be implemented to the nationwide perspective. Furthermore, this could demonstrate as a model of primary care – since the component and process used are similar to service delivery in other provincial areas of Thailand.
Conclusion
Primary care in Thailand frequently deals with common illnesses, upper respiratory and gastrointestinal disorders are highly prevalent. Managing common illness at the community pharmacy shows satisfactory effectiveness with lower unit cost. These findings are valuable to policy makers for designing a reimbursement system for community pharmacy.
Acknowledgements
The authors would like to thank all research assistants for data collection; Kaenphukhieo T., Supattarachaikun T., Loakhom I. and Saman T. The authors are also grateful to all contributions of all participants, to Assistant Professor Sirithanawutichai T. and Dr Sujirakul P. for ICD-10 review and being a coordinator of the PCU, and to Professor Smith G.H. for language editorial assistance.
Financial Support
This work was supported by the Health Promotion Fund for the Faculty of Pharmacy, Mahasarakham University.
Conflicts of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant institutional guidelines on human experimentation (Mahasarakham University).









