Introduction
Breast cancer is the second leading cause of death from cancer among women in Western countries (Ferlay et al., Reference Ferlay, Shin, Bray, Forman, Mathers and Parkin2010). Breast cancer survival, to a large extent, depends on its early detection. Despite recent questioning about regular mammography screening – due to high over-diagnosis and false-positive rates in Western countries (Gøtzsche and Jørgensen, Reference Croskerry2013), systematic screening programs, especially for average-risk women aged 50 years and over, have been shown to significantly increase early detection and reduce mortality (Oeffinger et al., Reference Oeffinger, Fontham, Etzioni, Herzig, Michaelson, Shih, Walter, Church, Flowers, LaMonte, Wolf, DeSantis, Lortet-Tieulent, Andrews, Manassaram-Baptiste, Saslow, Smith, Brawley and Wender2015). Average-risk women, aged 50–74 years and above, are currently being advised to engage in early detection practices by undergoing regular mammography testing once every two years (Israel Cancer Association, 2015).
The Arab population in Israel is an ethnic minority, constituting about 20% of the Israeli population. This population includes several religious groups: 83% Muslims, 8% Christians, 8% Druze, and 1% other (Central Bureau of Statistics, 2015). In spite of the diversity of religions, the Arab people share common history, culture, and tradition and express similarity in their way of life (Zoabi and Savaya, Reference Zoabi and Savaya2017). Although the Arab population is currently experiencing modernization processes, it is still, to a large extent, a traditional and religious society (Cohen, Reference Cohen2014). Breast cancer incidence has been found to be significantly lower among Arab women (Christians and Muslims) compared to Jewish women in Israel and women in Western countries, but Arab women are more frequently diagnosed at a more advanced stage of the disease (Cohen, Reference Cohen2014). It has been suggested that this tendency toward a later diagnosis could be attributed to the significantly lower rate of regular screening for the early detection of breast cancer among Arab women (Keinan-Boker et al., Reference Keinan-Boker, Baron-Epel, Fishler, Liphshitz, Barchana, Dichtiar and Goodman2013) and is predominantly related to social and cultural screening barriers (Azaiza and Cohen, Reference Azaiza and Cohen2008; Cohen and Azaiza, Reference Cohen and Azaiza2008; Azaiza et al., Reference Azaiza, Cohen, Awad and Daoud2010; Reference Azaiza, Cohen, Daoud and Awad2011). Largely due to the provision and promotion of the free-of-charge screenings and intensive efforts of the Israeli health services and the Israel Cancer Society, the majority of Arab women aged 50 years and over have undergone a mammography screening at least once. This has had an impact on narrowing the screening rate gap between Arab and Jewish women (Keinan-Boker et al., Reference Keinan-Boker, Baron-Epel, Fishler, Liphshitz, Barchana, Dichtiar and Goodman2013). However, the general rate of adherence to the recommended mammography schedule (undergoing mammography every two years) is still low among Arab women (Azaiza et al., Reference Azaiza, Cohen, Daoud and Awad2011).
Adherence to screening for the early detection of breast cancer was found to be predicted by health beliefs, especially perceived benefits of screening and perceived barriers to screening (Champion, Reference Champion1999), such as fear of pain or of the damage caused by radiation (Cohen and Azaiza, Reference Cohen and Azaiza2008). Several studies among Arab Muslim and Christian individuals elicited culture bounded perceptions of cancer and barriers to screening, including traditional beliefs concerning cancer, barriers related to exposure of the body, access barriers, and cancer fatalism (Cohen and Azaiza, Reference Cohen and Azaiza2008; Cohen, Reference Cohen, Carr and Steel2013). These cultural perceptions predicted adherence to mammography, even after controlling for various demographic variables (Azaiza et al., Reference Azaiza, Cohen, Daoud and Awad2011). However, in a comparison between women from the Palestinian Authority (a traditional society) and Arab women in Israel (a traditional society that has adopted a more Western lifestyle), both groups consisting of Muslims and Christians, the cultural beliefs were substantially higher among the Palestinian Authority participants (Azaiza et al., Reference Azaiza, Cohen, Awad and Daoud2010; Reference Azaiza, Cohen, Daoud and Awad2011).
Anthropologist and psychiatrist Arthur Kleinman (Reference Kleinman1980) coined lay or patients’ understanding or perceptions of illness ‘Explanatory Models’ (EMs). According to Kleinman (Reference Kleinman1980), EMs are frameworks through which individuals and groups understand diseases. A patient’s EM of an illness, according to Kleinman et al. (Reference Kleinman, Eisenberg and Good2006), consists of his/her beliefs and perceptions of the illness, the individual and social meaning that the illness holds for him/her, his/her expectations concerning what will happen to him/her as well as the physician’s actions, and his/her own therapeutic goals. They further argued that physicians’ EMs may differ from those of their patients, while such discrepancies – if not addressed by accounting for the patient’s model and communicating the physician’s EM in a way that allows the patient to understand and accept the EM – might interfere with clinical care.
Kleinman et al. (Reference Kleinman, Eisenberg and Good2006) argued that:
[c]ontemporary medical practice has become increasingly discordant with lay expectations. Modern physicians diagnose and treat diseases (abnormalities in the structure and function of body organs and systems), whereas patients suffer illnesses (experiences of disvalued changes in states of being and in social function; the human experience of sickness). (Kleinman et al., Reference Kleinman, Eisenberg and Good2006:140–141)
Based on Kleinman’s seminal work, Ashton and colleagues’ (2003) ‘integrative model’ of patient–physician communication in the case of cultural discord between physician and patient suggests that the EM of an illness formulates the behaviors of both the patient (i.e., illness behavior) and the physician. They further argue that discordance between the physician’s and patient’s EMs impacts the patient’s behavior and, consequently, his/her health outcomes. It is worth noting that this assumption was supported by Rich and colleagues’ (Reference Rich, Patashnick and Chalfen2002) qualitative study of EM, which focused on asthma and health-related behaviors among children and youth with asthma.
Comparative studies of EM of illnesses between physicians and patients have yielded mixed results. Ample research supports the fact that physicians have different EMs or perceptions of illness than their patients (e.g., Haidet et al., Reference Haidet, O’Malley, Sharf, Gladney, Greisinger and Street2008; Weller et al., Reference Weller, Baer, Garcia and Rocha2012; Nowicka-Sauer et al., Reference Nowicka-Sauer, Pietrzykowska, Banaszkiewicz, Hajduk, Czuszyńska and Smoleńska2016), even if they share the same language and culture (see, e.g., Aido and Harpham, Reference Aidoo and Harpham2001; Weller et al., Reference Weller, Baer, Garcia and Rocha2012). These studies’ findings imply that medicine is a type of ‘culture’ as it is characterized by the biomedical understanding of the body and pathology (Kleinman, Reference Kleinman1980; Schouten and Meeuwesen, Reference Schouten and Meeuwesen2006; Tirodkar et al., Reference Tirodkar, Baker, Makoul, Khurana, Paracha and Kandula2011; Lupton, Reference Lupton2012), whereas patients’ EMs are influenced by, among other things, culture (Kleinman et al., Reference Kleinman, Eisenberg and Good2006).
Nevertheless, there are studies that did not find differences between laypersons or community samples and physicians’ EMs. A study, for example, which explored EMs of AIDS among US and Mexican communities, as well as among physicians from both of these countries, found a core and similar biomedical EM of AIDS in all four subsamples (Baer et al., Reference Baer, Weller, García and Rocha2004). Similarly, a study which examined the EM of the common cold between physicians and laypersons in Texas and Mexico found that they all shared a common EM for this disease (Baer et al., Reference Baer, Weller, García and Rocha2008).
In this study, we examined the role of EMs of illness (cancer-related perceptions) in physicians’ and laywomen’s behaviors.
Specifically, our aims were
-
1. To compare cancer-related perceptions and perceptions of women’s barriers to screening between Arab physicians and Arab laywomen.
-
2. To examine the role of cancer-related perceptions in Arab physicians’ decisions to recommend undergoing regular mammography screening and in Arab women’s reports of adhering to mammography screening.
Methods
Participants
This study is a secondary analysis of two surveys. Both surveys received the approval of the Ethics board of the Faculty of Health and Social Welfare Sciences at the University of Haifa (approval #232/13, for the physician’s survey; approval #128/13, for the women survey). In this study, the two independent samples from the aforementioned surveys were combined and compared as follows.
Physicians’ sample
The sample was composed of 146 Arab physicians who were employed in community health services (family physicians, gynecologists, or internal medicine physicians), recruited from 14 communities in the northern, central, and southern regions of Israel, including Arab cities and villages and mixed Jewish-Arab cities, sampled by the multi-stage sampling method. According to the size of each community, 5–20 participants were randomly recruited from each. The sampling frame was the list of physicians registered in the Israeli Medical Association. We telephoned the randomly sampled physicians, explained the study aims and procedure, and scheduled a close-ended interview. Prior to the interview, participants signed an informed consent form. Non-answered calls were attempted several times. Out of the 320 physicians who were approached and asked to participate in a survey on early detection of breast cancer among their patients, 146 agreed to participate (a 47% participation rate).
Women’s community sample
A representative sample of the main Arab groups residing in northern, central, and southern Israel (Muslims, Christians) was drawn. The sample composed of 290 Arab women between the age 50 and 70 years. First, a random sample of ten cities and villages in northern, central, and southern Israel was conducted. Second, a random sample of women was drawn from Arab phone directories within each sampled city or village. The number of women that were sampled was contingent on the size of the population within the sampled city or village. Eligibility criteria were as follows: age 50–70 years, not being ill with cancer in the past or present, and fluent in Arabic. We phoned the women and invited them to participate in a survey on early detection of breast cancer and scheduled a close-ended interview. Prior to the interview, the women signed an informed consent form. Non-answered calls were attempted several times. The response rate was 90.9%.
Questionnaires
Women’s questionnaire
The women’s questionnaire composed of questions pertaining to socio-demographic characteristics; adherence to screening guidelines; cultural beliefs regarding cancer, social and access barriers to screening, fear of pain; fear of radiation; and fatalistic beliefs.
Socio-Demographic characteristics included age, family status, education, perceived economic status, and perceived level of religiosity.
Adherence to screening guidelines included questions on mammography frequency, and the last time the participant underwent mammography. Adherence to guidelines was defined as being on time with mammography, namely, having undergone a mammography examination every two years, with the last mammogram having been conducted not later than two years ago for women aged 52+ years, and having undergone at least one mammogram if the woman was between 50 and 52 years of age.
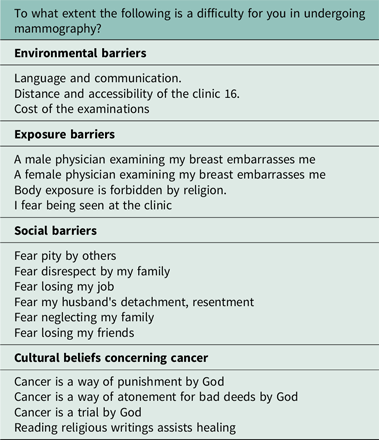
Cultural beliefs regarding cancer, social, and access barriers to screening
Cultural beliefs and the two types of barriers to screening (social and access) are three sub-scales of the Arab culture-specific barriers (ACSB) questionnaire (Appendix 1) (Cohen and Azaiza, Reference Cohen and Azaiza2008) that was previously validated and found with good validity and reliability indices (for details concerning development, reliability, and validity, see Cohen and Azaiza, Reference Cohen and Azaiza2008). The questionnaire was used in several studies (e.g., Azaiza et al., Reference Azaiza, Cohen, Awad and Daoud2010; Reference Azaiza, Cohen, Daoud and Awad2011).
Women’s cultural beliefs regarding cancer: This subscale of the ACSB comprises of items related to cultural beliefs regarding breast cancer (e.g., prayers help the healing process, traditional medicine helps, cancer is a punishment for one’s personal sins, cancer is one of God’s tests). Participants were asked to rate each question on a scale from 1 = not at all to 5 = very much. The internal consistency of this subscale was .91 (Cronbach’s alpha).
Women’s social barriers to screening: This subscale of the ACSB comprises of items probing perceptions of stigma and shame related to breast cancer (e.g., fear pity of others, fear of losing friends). Participants were asked to rate each question on a scale from 1=not at all to 5=very much. The internal consistency of this subscale was 0.93 (Cronbach’s alpha).
Women’s access barriers to screening: This subscale of the ACSB comprises of questions pertaining to environmental barriers (distance, communication barriers, financial expenses), exposure barriers (being examined by a male/female physician, religious barriers related to not wanting to expose the body (modesty issues), the fear of being seen in a breast clinic). Participants were asked to rate each question on a scale from 1=not at all to 5=very much. The internal consistency (Cronbach’s alpha) was .84.
Fear of pain was assessed by an item probing the degree of fear of the pain experienced during mammography. Participants were asked to rate each question on a scale from 1 = not at all to 5 = very much.
Fear of radiation was assessed by an item probing the degree of fear from the radiation caused by mammography. Participants were asked to rate each question on a scale from 1 = not at all to 5 = very much.
The fatalistic beliefs scale (Azaiza et al., Reference Azaiza, Cohen, Awad and Daoud2010; Reference Azaiza, Cohen, Daoud and Awad2011) was composed of four items: two items that related to fatalistic beliefs about breast cancer (e.g., breast cancer is a death sentence, despite the treatment); two items related to avoidance of cancer (i.e., it is better not to do the screening; ‘what you don’t know can’t hurt you’). Participants were asked to rate each question on a scale from 1 = not at all to 5 = very much. Internal consistency was .78 (Cronbach’s alpha).
Physicians’ questionnaires
The physician’s questionnaire composed of questions pertaining to socio-demographic characteristics, patterns of recommending and discussing screening facilitators and barriers with patients, physicians’ cultural beliefs regarding cancer, perceived patients’ social and access barriers to screening, perceived patients’ fear of mammography-related pain and radiation, and fatalistic beliefs.
Socio-demographic characteristics included gender, age, family status, education, years of seniority as a physician, and specialty.
Patterns of recommending and discussing screening facilitators and barriers with patients consisted of five separate items examining the rate of recommending biannual mammography to women aged 50–70 years and discussing the barriers to screening and screening advantages with women who refused to attend the exams. Responses ranged from 1=never to 4=always.
Physician’s cultural beliefs regarding cancer; perceived patient’s social and access barriers to screening
Physicians’ cultural beliefs regarding cancer: Was measured by the cultural beliefs regarding cancer subscale of the ACSB which was described above. The internal consistency of this subscale was .85 (Cronbach’s alpha).
Perceived patients’ social barriers to screening: Was measured by the social barriers to screening subscale of the ACSB, adjusted version for physicians. Physicians were asked to rate the extent to which each barrier to screening is true for their women patients. The internal consistency of this subscale was .81 (Cronbach’s alpha).
Perceived patients’ access barriers to screening: Was measured by the access barriers to screening subscale of the ACSB, adjusted version for physicians. Physicians were asked to rate the extent to which each barrier to screening is true for their women patients. Internal consistency (Cronbach’s alpha) was .84.
The physician’s perception of patients’ barriers to mammography due to fear of pain was assessed by one item probing the degree fear of the pain consists a barrier to undergoing mammography.
The physician’s perceptions about patients’ barriers to mammography due to fear of radiation were assessed by one item probing the degree fear of the radiation consists a barrier to undergoing mammography.
The fatalistic beliefs scale (Azaiza et al., Reference Azaiza, Cohen, Awad and Daoud2010; Reference Azaiza, Cohen, Daoud and Awad2011) was composed of four items: two items that related to fatalistic beliefs about breast cancer (e.g., breast cancer is a death sentence, despite the treatment); two items related to avoidance of cancer (i.e., it is better not to do the screening; ‘what you don’t know can’t hurt you’). Participants were asked to rate each question on a scale from 1=not at all to 5=very much. Internal consistency (Cronbach’s alpha) was .76.
Data analysis
Descriptive statistics of the socio-demographic and study variables were conducted followed by t- and chi-square tests for the comparison in background and study variables between the two groups. Binary logistic regression analyses were conducted to identify the contribution of the cancer-related perceptions on physicians’ recommending and women adhering to mammography. Physicians’ recommendation variable was dichotomized into 1 = recommend to all or most women in the relevant age group 0 = none or some of the women. Adherence was defined as 1 = being on schedule and 2 = not being on schedule (see Measures section). Two models of logistic regression were tested, a model adjusted for age and religion and an unadjusted model that includes the study variables only. A P < 0.05 was considered significant.
All analyses were run using SPSS 20.0. Missing data were less than 1%; therefore, data imputation was not performed. Sample size was calculated according to Cohen’s formula: The sample size required to receive a medium effect size at alpha < 0.01 for a multiple regression logistic regression with seven independent variables is N = 102.
Results
Table 1 shows the background details of the participants. The majority of the physicians were male (Arab women are underrepresented in the medical field in Israel (see Keshet et al., Reference Keshet, Popper-Giveon and Liberman2015), with a mean age of about 44 years. The physicians were predominantly Muslims; the rest were Christians (the ratio was proportional to the distribution of the Arab population in Israel (Central Bureau of Statistics, 2015), married, and mildly, or moderately religious. All of the physicians were employed in the community health services. About 70% specialized in family medicine; the remainder specialized in gynecology and internal medicine. The mean years of seniority were about 15, ranging from 1 to 42 years. The mean age of the women sample was 58, about 77% were married, similar to the physicians they were predominantly Muslims. Significant differences between the physician’s and women’s samples for all background variables. The women’s mean age was higher than that of the physicians. Similarly, women were more religious than the physicians. However, more physicians than women were married or had a partner, and more physicians than women were Muslims.
Table 1. Background variables: physicians’ sample and women’s sample

*P < .05; **P < .001
Comparison between physicians’ reports of recommending mammography and laywomen’s reports that they were advised to undergo mammography
The majority (77.62 %; N = 111) of the physicians reported that they recommend annual or bi-annual mammography screening to all their women patients; 12.59% (N = 18) recommended screening to most of their patients. In addition, 75.52% (N = 108) said that they always discuss the advantages of regular mammography with non-adherent patients, 16.78% (N = 24) do so most of the time, and 7.69 (N = 11) do so seldom or never. In contrast, only 72.41% (N = 210) of the women participants recalled their family physician, gynecologist, or other specialized physician ever discussing or recommending undergoing a mammography test. Nevertheless, the vast majority (92.00%, N = 266) of the women participants had, at some time in the past, undergone a mammography test, 60.34% (N = 175) had performed a mammography during the previous two years and reported undergoing mammography every 1–2 years, in accordance with the guidelines (this figure includes women aged 50–52 years who said they had performed the test once, in compliance with the guidelines). In addition, the vast majority (93.70%, n = 134) of the physicians perceived mammography as effective or very effective, while 6.29% (N = 9) ascribed medium or low importance to conducting regular mammography. Similarly, 92.75% (N = 269) of the women perceived mammography as an effective or a very effective test.
A comparison of beliefs and barriers to mammography screening between physicians and laywomen
An independent sample t test was performed to examine the differences in cultural and fatalistic beliefs, as well as in barriers to mammography screening (Table 2). Women held more cultural beliefs than physicians. Women also held more fatalistic beliefs than physicians. Physicians attributed more access barriers to screening as well as fear of radiation to women patients, compared with the women’s community sample. In contrast, women reported greater social barriers to breast cancer screening than were attributed to women patients by physicians. No significant differences were found in the perception of barriers to screening due to fear of pain between the two samples.
Table 2. Physicians and women cancer-related perceptions

*P < .001
The role of beliefs and barriers to mammography screening in physicians’ decision to recommend undergoing mammography and women adhering to mammography
A logistic regression was conducted in order to test the effect of physicians’ cancer-related perceptions on recommending mammography screening and the effect of cancer-related perceptions on women’s adherence to screening (see Table 3). First, an adjusted model was examined, including age and religion and the study variables: for the recommending mammography by physicians were entered the variables of their cultural beliefs and their perception of women’s social; barriers, access barriers, women’s fatalistic belief, and the barriers of fear of pain and radiation. For the women’s adherence with mammography guidelines, the independent variables were their own cultural perceptions, perceived social barriers, access barriers, fear of pain and radiation, and fatalistic beliefs. Physicians who had higher fatalistic beliefs and those who perceived that accessing barriers impede women’s adherence had a lower tendency to recommend mammography screening. Nevertheless, among physicians, higher perceived fear of pain as their patient’s barriers to attending mammography was related to a higher chance of recommending screening. In contrast, the only variable that had a significant effect on undergoing screening in the women’s group was fatalistic beliefs, while higher fatalistic beliefs were related to a lower chance of undergoing screening.
Table 3. Logistic regression of the effect of cancer-related perceptions on physicians’ recommending and women adhering to mammography

*P < .05; ** P < .01
Discussion
This study examined the role of EMs of illness (cancer-related perceptions) in physicians’ and laywomen’s behaviors (decision to recommend undergoing regular mammography, adhering to mammography). As in many previous studies (e.g., Kessels, Reference Kessels2003; van der Meulen et al., Reference van der Meulen, Jansen, van Dulmen, Bensing and van Weert2008; Pianosi et al., Reference Pianosi, Gorodzinsky, Chorney, Cosrten, Johnson and Hong2016), our findings show gaps between physician-women’s reports concerning medical information. We found that the percent of women who recalled being advised by a physician to undergo a mammography was lower than the number of physicians who reported conveying such advice.
Furthermore, our findings might also suggest that women assign less significance to the mammography test than physicians. These findings are not surprising, but they are troubling, given the impact of the early detection of breast cancer on mortality (Gøtzsche and Jørgensen, Reference Croskerry2013). Nevertheless, the majority of women reported undergoing a mammography test. This may be attributed to vigorous national efforts to increase adherence to screening through a population-based invitational breast cancer screening program and to educate women via the mass media. Although the physicians have an imperative role in reminding and encouraging to perform mammography and discussing barriers with patients, these findings may imply that, apart from physicians’ advice, other factors play a role in engaging in breast cancer screening behavior.
We also found evidence that physicians and laywomen hold different perceptions of cancer. This aligns with previous studies which show that physicians and patients/laypersons differ in their EMs or perceptions of illness, even if they share the same culture and language (e.g., Aido and Harpham, Reference Aidoo and Harpham2001; Weller et al., Reference Weller, Baer, Garcia and Rocha2012). In other words, and in accord with other research on EM and illness perception among laypersons (Kleinman et al., Reference Kleinman, Eisenberg and Good2006), in general, and cancer perception among Arabs and Arab women, in particular (Azaiza and Cohen, Reference Azaiza and Cohen2006; Reference Azaiza and Cohen2008; Cohen and Azaiza, Reference Cohen and Azaiza2005; Reference Cohen and Azaiza2008; Reference Cohen and Azaiza2010; Baron-Epel, Reference Baron-Epel2010; Goldblatt et al., Reference Croskerry2013; Cohen, Reference Cohen2014), the women’s perception of illness was shaped by cultural and religious beliefs of cancer (fatalistic beliefs and cultural beliefs).
Women’s perceptions were somewhat reserved concerning early detection outcomes; they tended to view cancer as a death verdict (Azaiza et al., Reference Azaiza, Cohen, Awad and Daoud2010), a punishment inflicted by God, the price for wrongdoing, and/or a trial; and often found comfort in religious texts (Cohen and Azaiza, Reference Cohen and Azaiza2008). We found that laywomen also reported greater social barriers (fear of being pitied, of detachment and resentment from one’s husband, of being disrespected by one’s family, of losing one’s place of work and friends, and of neglecting one’s family) to breast cancer screening than were attributed to women patients by physicians. These barriers attest to the level of cancer-related stigma associated with cancer in the women’s communities, to their fear of being marked as socially inferior, and therefore excluded from mainstream activities and roles, especially the role of the Arab woman, who is first and foremost a spouse and mother (Azaiza and Cohen, Reference Azaiza and Cohen2008; Cohen, Reference Cohen2014).
The results show that physicians mistakenly attributed both access barriers and fear of radiation to their patients. The findings imply that physicians fail to address patients’ and laypeople’s perspectives of cancer in the medical encounter. While physicians put an emphasis on common or typical barriers to health among the general population such as fear (as is the case, e.g., in relation to dental care, see, e.g., Gordon et al., Reference Gordon, Dionne and Snyder1998) and accessibility (which is more prevalent among minority populations; see, e.g., Steinberg et al., Reference Steinberg, Barnett, Meador, Wiggins and Zazove2006), the women reported cultural-related barriers. This might imply that if and when addressing barriers to screening, physicians tend to address the wrong set of barriers.
Our findings concerning the associations between perceptions and reported behavior are of particular importance, especially since they address the role of cultural perceptions among physicians. Fatalistic beliefs played a central role in undergoing mammography among the women. As was mentioned above, such beliefs are part and parcel of the women’s cultural and religious milieu, but it also implies that misunderstanding concerning the nature of cancer (a chronic disease) and novel treatments also play a role. Importantly, we found that physicians’ fatalistic beliefs (and the attribution of accessibility barriers) also affect their behavior. These findings are especially troubling and are in accord with other studies that illustrate how medical decisions may be prone to bias (Croskerry, Reference Croskerry2013).
The study has several limitations, first and foremost is its design – a cross-sectional survey based on two individual samples rather than dyads or clusters of physician–patient/s. Future studies should address this limitation as well as replicate our study in other cultural groups. Future qualitative studies should examine the gaps in illness perceptions among physicians and patients and their implications. Second, the low physicians’ participation rate hampers the representability of the sample. Future studies should attempt to engage a higher response rate among physician samples. Third, the fact that mammography screening is readily offered to Israeli women may positively influence our findings. It is important to note that in less-developed countries where the health system lacks resources, there is an ongoing debate whether to implement mammography programs (Li and Shao, Reference Li and Shao2015). The WHO and others have therefore argued for adopting other screening methods (e.g., clinical examination Li and Shao, Reference Li and Shao2015; Black and Richmond, Reference Black and Richmond2019). While this study as well as most studies (e.g., Cohen and Azaiza, Reference Cohen and Azaiza2008; Baron-Epel, Reference Baron-Epel2010; Azaiza et al., Reference Azaiza, Cohen, Daoud and Awad2011; Keinan-Boker et al., Reference Keinan-Boker, Baron-Epel, Fishler, Liphshitz, Barchana, Dichtiar and Goodman2013; Cohen, Reference Cohen2014; Lavy et al., Reference Lavy, Hershkovitz, Keinan-Boker and Halevy2016) regarding health behaviors of Arab women in Israel and in the Palestinian Authority had not differentiated between subgroups of religions (e.g., Muslims and Christians) due to cultural and lifestyle similarities, it is suggested that further studies will assess patients–physicians’ perceptions and communication patterns in relation to health behaviors, by religion subgroups. Nevertheless, in spite of the limitations, our study is the first to compare physicians’ and layperson’s perceptions of cancer, in general, and among Arab-Israelis, in particular.
Our findings hold implications for practice and policy. The findings concerning the physician–patient–communication-related factors we studied suggest that there is room for improvement. Although today’s curriculum for medical students addresses the role of social, cultural, and behavioral factors in health (Dao, Reference Zoabi and Savaya2017), our findings suggest that further attention to this subject, in general, and to the role of cultural perceptions, in particular, are warranted. In addition to understanding the patient’s perceptions of illness, physicians should also reflect on the social, cultural, and psychological factors that shape his/her decision.
Appendix 1:
the Arab culture-specific barriers (ACSB)