Introduction
The idea that people should be more engaged in protecting their health is widely seen as the best way to ensure the sustainability of health systems in a time of technological progress and increasing demand (World Health Organization, 2000; Wanless, Reference Wanless2002). This is particularly important for those with diabetes, because of the progressive nature of the condition and the prediction that, in England, more than 5% of the population will be affected by 2010 (Yorkshire and Humber Public Health Observatory and National Health Service Diabetes Support Team, 2006). But achieving this engagement may require changes in professional behaviour, according to a recent national survey of almost 125 000 people with diabetes (Healthcare Commission, 2007). Although, almost all had regular check-ups, only 47% of respondents said that they ‘almost always’ agreed on a care plan to manage their diabetes, and 30% said they rarely or never did this. A total of 27% reported that they rarely discussed their goals in caring for their diabetes.
Patient-centred medicine has been seen as a means to engage patients more effectively. It represents a move from a traditional doctor–patient relationship (in which the doctor advises and the patient decides whether to comply) to one based on mutualism; a partnership between adults who each bring their particular experience and expertise to the consultation (Stewart, Reference Stewart, Brown, Weston, McWhinney, McWilliam and Freeman1995a; Mead and Bower, Reference Mead and Bower2000; Royal College of Physicians of London, 2005). Roter and Hall emphasize that this should not be mere consumerism, allowing patients whatever they want, regardless of the cost to them or society. Instead, it implies an active sharing of ideas and negotiation (Roter and Hall, Reference Roter and Hall1992). This approach is reflected in the UK National Service Framework for Diabetes, which called for partnership in decision-making and support for self-management, to be reflected in agreed care plans (Standard 3) (Department of Health, 2001). Furthermore, the white paper Our Health, Our Care, Our Say (Department of Health, 2006), established a commitment to personalized care planning for everyone with a long-term condition, which has been reiterated in the NHS review High Quality Care for All (Darzi, Reference Darzi2009).
In order to consider how this might be implemented, in 2005, the Department of Health and Diabetes, UK established a joint working group, drawing together practitioners, academics and people with diabetes (Department of Health and Diabetes UK Care Planning Working Group, 2006). This was asked to define what care planning involved, and by reviewing the evidence base and identifying examples of the approach in practice, to develop guidance for health services. This group held five one-day meetings between July 2005 and August 2006, with additional discussions in between. Although the primary focus was diabetes care, the group took account of UK policy initiatives, such as the Wanless review which emphasized the need to engage patients in self-care (Wanless, Reference Wanless2002), work on explaining risk by the Royal College of Physicians (Armitage et al., Reference Armitage, Goose, Rosser and Barlow2006) and a report on care planning for people with long-term conditions that the NHS Modernisation Agency had commissioned (Matrix Research and Consultancy, 2004).
From these deliberations, the group characterized care planning as a mechanism for the person with diabetes and the practitioner to share their perspectives, and make joint decisions on actions needed to minimize health risk (see Figure 1). It was agreed that implementing this would take into account the social and health service context, and the way that information is communicated and managed. Having sufficient knowledge and understanding about diabetes was seen as a prerequisite for patients to participate effectively in their care.

Figure 1 Model of Care planning (Dept of Health/Diabetes UK Report)
The group prepared a draft report, which was circulated widely for comment. Although most respondents were supportive, several raised questions about the evidence for the approach and how it related to other models of care. In order to investigate this further, four members of the working group met separately to review the theoretical basis and evidence for the model developed by the wider group. The findings of this review are reported here.
Method
We agreed on the following research question: Does a process of care planning for people with diabetes, combining a patient-centred approach by practitioners with measures to promote self-management by patients and encouragement to both to discuss and agree relevant goals, improve health outcomes? Because of the breadth of the topic and the time imperative of publishing the guideline, we decided to integrate the findings of previous systematic reviews, rather than consider the full range of individual studies that might be relevant. Where there were no reviews specific to diabetes, we considered literature relating to other long-term conditions, because we believed that much of the evidence relating to patient–practitioner interactions would still be relevant.
Search strategy
Two reviewers (JG and SE) independently searched the Cochrane Library and the Database of Reviews of Effectiveness (DARE). We selected the following Medical Subject Heading (MeSH) search terms and keywords following discussion with members of the wider Working Group: *Care planning, *patient education, *self-care, *self-management, *motivation, *self-efficacy, *case management, *problem solving, *decision-making, *decision support techniques, *patient-centred care, *patient participation, *patient activation, *action planning, *goal setting, *behavio(u)r change, *professional-patient relations, *empowerment.
We excluded duplicates and reviews that were solely concerned with education outside the consultation, because this has been extensively reviewed elsewhere (Norris et al., Reference Norris, Nichols, Caspersen, Glasgow, Engelgau, Jack, Snyder, Carande-Kulis, Isham, Garfield, Briss and McCulloch2002b; NICE, 2003; Ellis et al., Reference Ellis, Speroff, Dittus, Brown, Pichert and Elasy2004; Deakin et al., Reference Deakin, McShane, Cade and Williams2005), and our focus was on care planning as an approach to shared decision-making within the consultation. Two reviewers (JG and SE) independently assessed each abstract and rated its relevance. Disagreement on inclusion was referred to the other reviewers (PC and JS) for resolution. A further review was identified from expert opinion, which our searches had not revealed. Following assessment, an agreement was reached to include it.
Assessment of quality and relevance
Working independently in pairs, we assessed the quality of each review, extracted data and presented the findings to the other reviewers for discussion and critique. Data extraction forms were adapted from published guidance (NHS Centre for Reviews and Dissemination, 2001) and a comparable review of integrated care (Ouwens et al., Reference Ouwens, Wollersheim, Hermens, Hulscher and Grol2005). We rated relevance to the three themes: promoting a patient-centred approach by practitioners, promoting self-management by patients and promoting shared decision-making and goal-setting using a 4-point Likert scale. We excluded reviews judged not to be relevant to any of these themes (Box 1). We then considered the interventions, outcomes measured and how reviews related to components of the care-planning model.
Box 1 Assessment of relevance and quality

Results
We identified 86 reviews as potentially relevant; 22 related to diabetes care, 40 to care across several conditions and 24 to another specific long-term condition in searches up to August 2006. After assessing the abstracts, we selected 32 papers for detailed consideration. Of these, 10 were excluded as not relevant, of poor quality, or because the interventions were solely educational (Figure 2). Details of the 22 included reviews are shown in Table 1.
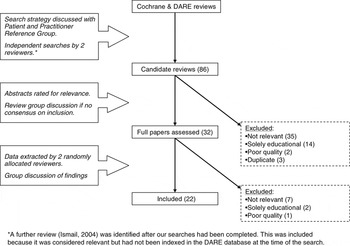
Figure 2 Review flow chart
Table 1 Overview of reviews and relevance to care planning

NHS CRD = NHS Centre for Reviews and Dissemination; RCTs = randomized controlled trials.
a‘Interventions’ refers to any comparative design in which an intervention is delivered, including before and after designs. ‘Varied’ includes intervention studies, observation studies and systematic reviews.
bRelevance was scored using the scale in box 1 (Not at all = 1; Not very well = 2; Very well = 3; Completely = 4). Two reviewers rated each review, and then compared (and sometimes revised) their assessments when they disagreed. The semi-quantitative ratings shown were derived by averaging the two scores: the mid-point, 2.5 is shown as ‘+’; 3 is ‘++’; 3.5 is ‘+++’ and 4 is ‘++++’.
Evidence for components of the model
The reviews incorporated both intervention and observation studies, and although eight employed meta-analysis, mostly the interventions were too heterogeneous to allow more than descriptive synthesis. Interventions to modify clinical interactions were targeted at health care professionals (eg, to improve communication skills), patients (to enhance their role within consultations), the system of care (eg, decision support systems and computerized knowledge management) or a combination of these.
The individual patient’s story
Physician–patient communication, which is necessary if the patients’ story is to be heard, was reviewed by Stewart (Reference Stewart1995b). She included interventions such as communication skills training and observational studies in which communication was evaluated but not altered. In history-taking, techniques such as expressing empathy or asking patients about their concerns were associated with improvements in outcomes such as emotional health, symptom resolution, functional status and blood pressure. Measures to enable patients to play a more active role in discussion of the management plan, such as by asking more questions, were found to reduce anxiety and improve other outcomes. Harrington et al. (Reference Harrington, Noble and Newman2004) reviewed patient focused intervention studies to promote participation and found that these increased patients’ perceptions of control over their health.
Training professionals to focus on the patient as a person, rather than solely on their illness, and to share control of the consultation increased measures of patient-centredness in intervention studies evaluated by Lewin et al. (Reference Lewin, Skea, Entwistle, Zwarenstein and Dick2001). However, few of the studies examined whether this translated into changes in healthcare behaviour or improved health outcomes, and the results from these were mixed.
Whilst a patient-centred approach is widely advocated in diabetes care, evidence to suggest that it leads to improved health outcomes is limited. Mead and Bower (Reference Mead and Bower2002) assessed the methodological rigour of observational studies of patient-centred medicine in primary care. They found that a variety of definitions had been used. They suggest that a lack of agreed definitions is one reason why the relationship between patient-centeredness and improved health outcomes has not yet been established.
The professional’s story
The value of medical management in diabetes is widely accepted (Diabetes Control and Complications Trial Research Group, 1993; UK Prospective Diabetes Study Group, 1998), as is the evidence for systematic approaches to implementing this (Griffin and Kinmonth, Reference Griffin and Kinmonth2000; Renders et al., Reference Renders, Valk, Griffin, Wagner, Eijk and Assendelft2000). While most of the organizational literature is beyond the scope of this review, the review of the effectiveness of disease and case management for diabetes by Norris et al. (Reference Norris, Nichols, Caspersen, Glasgow, Engelgau, Jack, Isham, Snyder, Carande-Kulis, Garfield, Briss and McCulloch2002a) seems relevant. Case management involves identifying and assessing the needs of individuals at particular risk, developing a care plan and monitoring outcomes. The review found that it was often implemented alongside broader disease management and education programmes, and that it was effective at improving glycaemic control and monitoring of glycaemic control.
A further aspect of the ‘professional’s story’ is that recent definitions of ‘patient-centred’ care, derived from a review of observational studies, include the ‘doctor-as-person’ – an awareness of the influence of the personal qualities and subjectivity of the doctor on the practice of medicine (Mead and Bower, Reference Mead and Bower2002).
Learning about and managing diabetes
Helping people understand their condition is vital to ensure their active engagement in their own care. Therefore, a fundamental principle of the care planning process is that it should run in parallel with effective education.
Two reviews identified benefits from a personalized approach to information sharing. Studies of educational interventions for people with hypertension suggest that personalized counselling does more to improve blood pressure control than didactic, curriculum-based approaches (Boulware et al., Reference Boulware, Daumit, Frick, Minkovitz, Lawrence and Powe2001). Similarly, printed information that was tailored to the individual (based on characteristics such as age, risk factors or readiness to change behaviour) enhanced recall and readership, was perceived as more relevant and was more likely to lead to behaviour change than non-tailored leaflets (Skinner et al., Reference Skinner, Campbell, Rimer, Curry and Prochaska1999).
Interactive computerized systems are increasingly used to organize care, support decision-making and provide patients and practitioners with relevant information. Games, web-based education and email communication have been developed for a range of conditions, with reported improvements in knowledge, social support, behaviours such as exercise and medication adherence and clinical outcomes (Murray et al., Reference Murray, Burns, See, Lai and Nazareth2005). For diabetes specifically, computerized patient education programs have been shown to improve diet and metabolic indicators, and computer-assisted insulin dose adjustment was associated with a small improvement in diabetes control (Balas et al., Reference Balas, Krishna, Kretschmer, Cheek, Lobach and Boren2004). Electronic prompts have also been shown to improve health professionals’ compliance with guidelines. Summarizing these findings, Balas et al. (Reference Balas, Krishna, Kretschmer, Cheek, Lobach and Boren2004) concluded that computerized knowledge management is becoming a vital component of quality diabetes care. This has important implications for any strategy to implement care planning.
For asthma, Gibson et al. (Reference Gibson, Powell, Coughlan, Wilson, Abramson, Haywood, Bauman, Hensley and Walters2002) reviewed the effectiveness of self-management education. Optimal self-management, which included written action plans and goals setting, resulted in significant reductions in health care utilization, episodes of nocturnal asthma and days off work. A further asthma review investigated whether written action plans increased medication adherence (Toelle and Ram, Reference Toelle and Ram2004). The studies reported did not appear to involve patients in setting priorities; instead, the plans provided instruction on how to respond to an exacerbation of the condition and the results were inconsistent.
Living with diabetes
In contrast to managing diabetes, this component of the model focuses on managing life with diabetes. Theoretical literature suggests that self-management improves psychological health, empowers people to make behaviour changes which may be credited with improved clinical outcomes (Bandura, Reference Bandura1977; Funnell et al., Reference Funnell, Anderson, Arnold, Barr, Donnelly, Johnson, Taylor-Moon and White1991) and there is empirical evidence from studies of self-management education outside the consultation to support this (Norris et al., Reference Norris, Nichols, Caspersen, Glasgow, Engelgau, Jack, Snyder, Carande-Kulis, Isham, Garfield, Briss and McCulloch2002b; Loveman et al., Reference Loveman, Cave, Green, Royle, Dunn and Waugh2003; Deakin et al., Reference Deakin, McShane, Cade and Williams2005; Davies et al., Reference Davies, Heller, Skinner, Campbell, Carey, Cradock, Dallosso, Daly, Doherty, Eaton, Fox, Oliver, Rantell, Rayman and Khunti2008).
Steed et al. (Reference Steed, Cooke and Newman2003) reviewed the impact of skills-based self-management information and psychological interventions on psychosocial outcomes in adults with diabetes. The variety of interventions and study designs limit interpretation, but most reported either a modest gain or no change in psychological well-being and quality of life. Taken as a whole, the findings suggest that for those who are also depressed, psychological interventions are helpful and that self-management improves psychological health. Psychological interventions such as cognitive behavioural techniques, motivational interviewing or counselling were found to improve glycated haemoglobin by a clinically significant 1.06% (95%CI −1.61 to −0.51) and also improve psychological well-being (Ismail et al., Reference Ismail, Winkley and Rabe-Hesketh2004).
Other health and social issues
This domain is included in the model to recognize that many people with diabetes have other long-term conditions. If these affect their well-being, this may influence their capacity to self-manage. Holistic diabetes care, therefore, needs to encompass the range of problems that people with diabetes encounter. However, this was beyond the scope of this review, so no specific conclusions can be drawn.
Sharing information and negotiating an action plan
In a review of interventions to enhance the role, or ‘activate’ the patient within the consultation, Griffin et al. (Reference Griffin, Kinmonth, Veltman, Gillard, Grant and Stewart2004) found that these seemed to be effective across a range of conditions, but few of the studies reported the impact on health outcomes. In diabetes, interventions delivered directly to patients (eg, pre-consultation coaching and group consultations) seem more effective at promoting involvement than trying to influence practitioner behaviour (van Dam et al., Reference van Dam, van der Horst, van den Borne, Ryckman and Crebolder2003).
The process of sharing information occurs throughout the care planning process and has been considered in the sections relating to the patient’s story and learning about diabetes. However, we identified a body of work relating largely to other disorders, which focused on discussing risk and aiding decision-making. Risk is a fundamental concept in diabetes care and is central to many decisions about treatments or changes in behaviour. With greater participation in decision-making comes the need to discuss and understand the risks and benefits of different choices.
Bekker et al. (Reference Bekker, Thornton, Airey, Connelly, Hewison, Robinson, Lilleyman, MacIntosh, Maule, Michie and Pearman1999) reviewed the controlled trial evidence for interventions to promote informed decision-making. Studies involving manipulating information to present it in different ways, and those providing individual feedback and training for decision-making appeared more likely to report an effect than those which just provided additional information. Focusing on risk communication about screening (mainly for cancer), Edwards et al. (Reference Edwards, Unigwe, Elwyn and Hood2003) found that personalizing individuals’ risk increased the uptake of screening tests. Categorizing risk in broad groups (high, moderate or low) or listing risk factors was more effective than providing a numerical score, unless the individual was at a particularly high risk.
O’Connor et al. (Reference O’Connor, Stacey, Entwistle, Llewellyn, Rovner, Holmes, Tait, Tetroe, Fiset, Barry and Jones2003) reviewed aids to help people make decisions that were ‘right’ for them (rather than based on necessarily adhering to recommended treatment options), most of which were concerned with cancer treatment or heart disease. They defined a decision aid as including information about the clinical problem, potential options and the possible outcomes. They found that decision aids improved an individual’s understanding of the available options, enhanced participation in decision-making and reduced indecision and decisional conflict.
These reviews (Bekker et al., Reference Bekker, Thornton, Airey, Connelly, Hewison, Robinson, Lilleyman, MacIntosh, Maule, Michie and Pearman1999; NHS Centre for Reviews and Dissemination, 2000; Edwards et al., Reference Edwards, Unigwe, Elwyn and Hood2003) suggest that personalizing risk communication in well designed decision aids could make a useful contribution to diabetes care, if focused around key decisions such as medication changes or the introduction of insulin.
Taking action
Behavioural scientists have identified approaches to the factors which influence people’s intended and actual behaviours (Ajzen and Fishbein, Reference Ajzen and Fishbein1969; Prochaska and DiClemente, Reference Prochaska and DiClemente1983; Backett et al., Reference Backett, Currie, Hunt, McQueen, Martin and Ziglio1989) and these have formed the basis of behaviour-change programs (Marshall and Biddle, Reference Marshall and Biddle2001; Hardeman et al., Reference Hardeman, Johnston, Johnston, Bonetti, Wareham and Kinmonth2002). Although most of this work is beyond the scope of this review, we did include reviews relating to motivational interviewing and medication adherence that appeared relevant.
The meta-analysis of psychological interventions reported before, provides evidence that psychological interventions can help people take action to improve their diabetic control (Ismail et al., Reference Ismail, Winkley and Rabe-Hesketh2004). Most of the interventions tested were, however, delivered outside of routine consultations, often in groups. In contrast, motivational interviewing has been proposed as a personalized approach to individual counselling, that promotes behaviour change by helping clients explore and resolve ambivalence. Although there is some evidence that it may help people overcome substance abuse (Dunn et al., Reference Dunn, Deroo and Rivara2001) and improve their diet (van Wormer and Boucher, Reference van Wormer and Boucher2004), it is unclear how relevant these findings are to diabetes care in the surgery or clinic.
Much of the published research on adherence to medication starts from the premise that the doctor should advise the patient what medication to take and that the patient should comply with the doctor’s recommendation. Evaluating this approach for people with type 2 diabetes, Vermeire et al. (Reference Vermeire, Wens, Van Royen, Biot, Hearnshaw and Lindenmeyer2005) found little evidence that education, reminders, nurse-led telephone interventions or pharmacist reviews significantly improved medication adherence, although one study cited did find that patients who were encouraged to self-manage within a participatory care programme were more successful at controlling their risk factors (Rachmani et al., Reference Rachmani, Levi, Slavachevski, Avin and Ravid2002).
Discussion
Personalized care planning can be seen as integrating a patient-centred approach with efforts to promote self-management through partnership working and shared decision-making. Our review identified a large body of work on patient-centred medicine, both characterizing the components of the approach and describing its impact on the consultation, but less evidence relating to longer term outcomes (Stewart, Reference Stewart1995b; Mead and Bower, Reference Mead and Bower2000; Reference Mead and Bower2002; Michie et al., Reference Michie, Miles and Weinman2003). It was clear that while effective communication was important, it was not enough to focus solely on changing practitioner behaviour, and that interventions also needed to engage patients and provide organizational support to promote shared decision-making.
In conducting this review, we sought to test the evidence for a developing health policy, but we encountered a number of difficulties in doing so. It was striking that the language used in policy discussions differs from that in the academic literature; indeed, the term care planning is not included in the MeSH framework for indexing medical literature. To address this, we consulted lay and professional members of the Department of Health/Diabetes UK Working Group about the meaning of the term care planning, and searched for research findings relating to the underlying principles that we understood it to involve. While the decision to look beyond diabetes might be questioned, we were keen to focus on the processes of care, rather than the condition itself, and did not want to exclude relevant evidence from other long-term conditions. Also, many people with diabetes have multiple co-morbidities.
The wider working group was under pressure to report speedily, so that policy on care planning for diabetes could fit with other initiatives; but this meant that it was not possible to seek research funding for a systematic review of primary literature. Instead, we integrated existing systematic reviews and limited our search to those within Cochrane and DARE, databases established to enable practitioners and policymakers identify high quality reviews more easily. We are aware that as a result we may have missed some relevant work; particularly recent reviews not yet indexed within DARE.
Furthermore, although the reviews identified did not consider this in depth, two individual studies have raised questions about whether adopting a patient-centred approach might distract professionals from addressing clinical problems (Kinmonth et al., Reference Kinmonth, Woodcock, Griffin, Spiegal and Campbell1998; Pill et al., Reference Pill, Rees, Stott and Rollnick1999). More recently, Michie et al. (Reference Michie, Miles and Weinman2003) contrasted studies which adopted different approaches to patient-centredness and suggested that health outcomes were better in studies when health professionals sought to activate the patient as an agent in their own care, than when they sought to adopt the patient’s perspective. These findings lend support to the view that ‘patient-centredness’ alone may not be sufficient to significantly improve on health outcomes, and integration with interventions to promote self-management is required. Our review identified a wide array of such interventions which were associated with improved knowledge, changes in behaviour and better psychological and biomedical outcomes. These included using pre-consultation prompts, coaching to enhance the patient’s role in consultations, tailoring or personalization information, decision aids, risk communication and computerized knowledge management systems.
Over recent years, systematic approaches to diabetes care, recall systems and routine surveillance have been adopted as standard (Griffin and Kinmonth, Reference Griffin and Kinmonth2000; Renders et al., Reference Renders, Valk, Griffin, Wagner, Eijk and Assendelft2000; Norris et al., Reference Norris, Nichols, Caspersen, Glasgow, Engelgau, Jack, Isham, Snyder, Carande-Kulis, Garfield, Briss and McCulloch2002a). Our findings point to ways that diabetes care should now develop further in order to maximize the benefits achievable by engaging patients. This could include mechanisms to share information (such as giving patients test results before consultations), inviting questions in clinic invitation letters and decision support systems that could be used by both patients and practitioners. These interventions will require careful development and testing in adequately powered clinical trials, partly because of the possibility that broadening the agenda to better address patients’ concerns may distract from the traditional biomedical focus on metabolic outcomes. There is also scope for further evaluating the existing evidence-based interventions such as motivational interviewing, to establish the feasibility of incorporating them into routine consultations. In this review, wide-ranging interventions appeared more effective than narrowly targeted ones, which suggests that ideally, measures to promote care planning should be developed as integrated, whole system initiatives, incorporating elements at the level of the individual patient, the practitioner and the healthcare system.
Following the publication of the Working Group’s report in 2006, the UK Department of Health has established pilot projects which will serve to develop and test this approach across three local services (Calderdale and Kirklees, North of Tyne and Tower Hamlets). These Year of Care pilots seek to involve patients in planning their care at an individual level, and to ensure that the services they need are delivered through innovative commissioning arrangements. When complete, the evaluation should provide a clearer idea about some of the practical steps needed if this collaborative approach is to be promoted more widely (National Diabetes Support Team, 2008). Within the NHS context, this is likely to involve educational initiatives, developing and sharing tools for use in everyday practice and using the levers available through commissioning. Specifically, the service specifications for local diabetes services could include a commitment to the process of care planning and in general practice this could be facilitated through Locally Enhanced Service agreements.
These initiatives for diabetes are echoed by wider NHS plans to offer all 15.4 million people with long-term conditions a personalized care plan (Darzi, Reference Darzi2009). While our findings provide pointers as to how this might be achieved, they also suggest that the complexity involved is such that there is a risk of practitioners paying lip-service to an initiative that may not have been adequately thought through.
Adopting personalized care planning may challenge both patients and professionals, so training will be important for both. Some may feel that they already adopt a collaborative approach, but there is evidence that optimal outcomes are not being consistently achieved. Although our review found that the systems and resources needed to support partnership working are reasonably well understood, they are not yet widely available. Despite these concerns, this approach offers a means to share information and responsibility in individual care and pointers as to how services can better engage patients in managing a long-term condition such as diabetes.
Acknowledgements
The present review was funded by the NHS National Coordinating Centre for Research Capacity Development (J Graffy – PD/03/06, J Sturt 02/NandAHP/PD/03/018). We would like to thank the members of the Department of Health/Diabetes UK Care Planning Working Group for contributing to the search strategy for this review. We also thank Clare Goodhart and Sue Roberts for comments on the manuscript. The views expressed in this publication are our own and not necessarily the funders. No ethical approval was required for the review and we have no competing interests to declare.





