Introduction
Health service systems in developing countries are struggling with the weakest and the lowest resourced health systems with underdeveloped primary health care (PHC), while at the same time having the highest burden of noncommunicable diseases (NCDs) within the WHO European Region (Jakab et al., Reference Jakab, Farrington, Borgermans and Mantingh2018). In Kyrgyzstan, a lower-middle income, former-Soviet-Union country in central Asia, NCDs are the leading cause of mortality and cardiovascular diseases (CVDs) alone cause around half of all deaths (WHO Regional Office for Europe, 2017). An estimated 17% of the population aged 40–64 years is at high CVD risk, and the Ministry of Health (MoH) designated 2019 as the year of Hypertension in an effort to increase the focus on control of this major risk factor (Kaliev et al., Reference Kaliev, Meimanaliev, Djumagulova and Habicht2018).
Good health is not only important for individuals, but also for governments being crucial in achieving sustainable development and growth as well as constraining the increment of required resources. Almost 4% of Kyrgyzstan’s gross domestic product is lost due to NCDs. Life expectancy of men is only 67 years of age (women 75 years of age) having major influence on workforce (WHO Regional Office for Europe, 2017). Significant improvements in PHC are thus needed to meet the universal health coverage, one of the principal goals among the Sustainable Development Goals (United Nations Development Programme, 2019; World Health Organization, 2019).
A scoping review by Bitton et al. (Reference Bitton, Fifield, Ratcliffe, Karlage, Wang, Veillard, Schwarz and Hirschhorn2019) assessing the PHC system performance in low- and middle-income countries (LMICs) and related further needs in research addressed the lacking evidence on feasible and effective surveillance approaches across PHC systems in LMICs. Especially, the need for further work to develop better NCD surveillance was highlighted. A systematic review by Kruse et al. (Reference Kruse, Stein, Thomas and Kaur2018) identified that the use of electronic health records (EHRs) facilitated management of population health by improving productivity and efficiency, improved quality, data management, possibilities for surveillance, and support for preventive care. Most of the research related to the use of EHRs has concentrated on effects on processes and outcomes of care in clinical settings. Much less is known about the feasibility of EHRs in providing large-scale and timely data on health situation of population available for health departments (Klompas et al., Reference Klompas, McVetta, Lazarus, Eggleston, Haney, Kruskal, Yih, Daly, Oppedisano, Beagan, Lee, Kirby, Heisey-Grove, DeMaria and Platt2012).
Very little research is available on how to implement and improve the local use of information communication technology and eHealth to improve the outcomes in PHC in LMICs nor what ideal, low-cost, and simple eHealth documentation and data recording systems exist or could be implemented in low-resource settings (Bitton et al., Reference Bitton, Fifield, Ratcliffe, Karlage, Wang, Veillard, Schwarz and Hirschhorn2019). In Kyrgyzstan, it has been found that quality is driven by a top-down approach rather than inherent in the work of clinical teams, and routinely collected data on the management of patients and facilities are not generally shared nor routinely available for performance feedback to managers or clinicians (World Health Organization, 2018).
The aim of this study was to assess the feasibility of the national electronic PHC database administered by the eHealth Center in Kyrgyzstan to obtain valuable information for the national authorities on the disease burden of the patient population and on the potential of routine data systems to support performance management of NCDs in PHC.
Material and methods
The national electronic database for PHC data was established in Kyrgyzstan in 2012. The database is administered by the eHealth Center operating under the MoH. The database includes information collected using a clinical information form (CIF) filled in at all visits to PHC clinics. The CIF is a standard form used throughout the country and includes a limited amount of information, but in structural format. Recently, the form was nationally updated to include some key indicators related to the evaluation needs of WHO Package of Essential NCD Interventions (WHO PEN) framework as the lack of information was observed when piloting the WHO PEN protocols in Kyrgyzstan in 2015–2017 (World Health Organization, 2013; Kontsevaya and Farringtom, Reference Kontsevaya and Farrington2017). In the beginning, the CIF forms were filled in on paper by the health professionals and after the appointment entered to the database by assistants in the clinics. Clinic specific data were then transferred to the national eHealth Center once a month. More recently, the availability of hardware and software has improved and in some clinics the data can be directly entered to the national database by professionals themselves.
To pilot the use of the national data for quality assessment purposes, a data extraction was done by the eHealth Center covering all data until December 2018 covering four PHC clinics in Bishkek. Because the system has not been introduced to all the clinics at the same time, the dates of the first visits varied starting in some clinics already from December 2014. For analyses, we restricted the data to patients over 18 years of age who had visited the clinics during a 1-year period (25 December 2017–25 December 2018) being comparable between the clinics. Every patient has a unique identifier given in the clinic, so we were able to combine the different visits on the patient level inside the clinics, but not between the clinics.
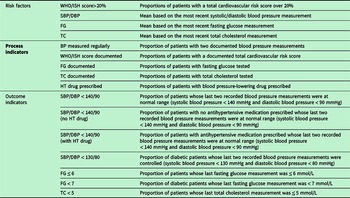
Quality of care indicators were driven from the indicators used in the evaluation of the implementation of the WHO PEN framework which aims at strengthening efficiency and equity of PHC in low-resource settings (Table 1). Similar indicators have been used in various evaluation studies in eastern European and Central Asian countries, where however the data have been collected manually from paper records (Collins et al., Reference Collins, Laatikainen, Shoismatuloeva, Mahmudzoha, Rahimov, Sultonova, Jonova and Farrington2019; Laatikainen et al., Reference Laatikainen, Inglin, Collins, Ciobanu, Corocichin, Salaru, Zatic, Anisei, Chiosa, Munteanu, Alexa and Farrington2020). Both process indicators describing, for example, the measurement activity of risk factors and follow-up of blood pressure, cholesterol, and glucose levels as well as some outcome indicators assessing the achievement of treatment targets were calculated.
Table 1. Definition of indicators

WHO/ISH score = World Health Organization/International Society of Hypertension risk prediction score; SBP = systolic blood pressure; DBP = diastolic blood pressure; FG = fasting glucose; TC = total cholesterol; HT = hypertension; BP = blood pressure.
Regarding these key indicators related to NCDs and their management, the following information was available in the database: age, gender, medical diagnosis recorded during the visit (ICD-10), drug prescriptions, total cardiovascular risk assessed using World Health Organization/International Society of Hypertension (WHO/ISH) risk prediction charts, values of blood pressure measurements, fasting glucose, and total cholesterol. However, it seemed that recording of laboratory values (fasting glucose and total cholesterol) had been implemented in the clinics during spring 2018, and thus data from a few first months were missing. Data were checked for implausible values and logical discrepancies. It was found out that the clear structure of the database and the drop-down menus used, for example, in recording medications supported legibility of the data. Obviously, manual data entry is prone to mistakes and such were found especially in recording measurement values. However, the amount of implausible values was actually very small. Another place for error is diagnostic codes where we were able to observe some differences in practices which codes are preferred.
To identify whether patients had diabetes or CVDs, the recordings of diagnoses were considered also from previous years if available. Patients were regarded as having hypertension if ICD-10 codes I10–I15, diabetes if codes E10–E16, ischemic heart disease if codes I20–I25, and cerebrovascular disease if codes I60–I69 were recorded in CIF forms. Other information was taken into account only based on recordings during the 1-year observation period. The most recent values were used to calculate the mean of blood pressure, cholesterol, and fasting glucose. Hypertension medication was identified from the name of the medication prescribed.
Data were analyzed for all patients over 18 years of age as well as separately for those over 40 years of age, for those with hypertension or with diabetes. Differences between men and women were evaluated by logistic regression models for dichotomous outcomes and multivariate linear regression models for continuous outcomes. All results were age-adjusted and a P-value < 0.05 was considered statistically significant.
Results
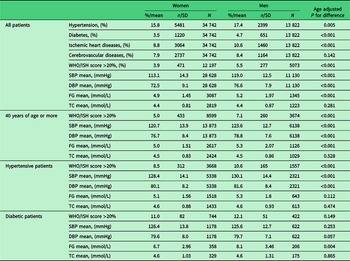
The characteristics of the patient population that had visited the clinics during the designated period are presented in Table 2. There were altogether 48 564 adult patients who had visited these four clinics during the observed year. Over 70% of them were women, but the age distribution of patients was similar for women and men. Out of all patients, diagnosis for hypertension was recorded for 16% of women and 17% of men, diabetes for 4% and 5%, ischemic heart disease for 9% and 11%, respectively (Table 3). Cerebrovascular disease was found from 8% of both women and men.
Table 2. Demographic characteristics of patients

* Medical diagnoses from all available years were taken into account.
Table 3. Documented diseases and risk factors for women and men by patient group

WHO/ISH score = World Health Organization/International Society of Hypertension risk prediction score; SBP = systolic blood pressure; DBP = diastolic blood pressure; FG = fasting glucose; TC = total cholesterol; SD = standard deviation.
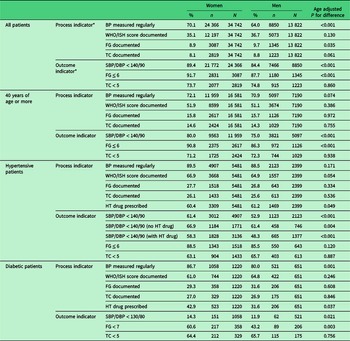
As an example of process indicators among all the patients, the proportion of those having blood pressure measured at least on two occasions was 70% for women and 64% of men and of about 70% of those aged 40 years or more. Of those with hypertension, the blood pressure was measured at least on two occasions of 90% of women and 89% of men (Table 4). Total cholesterol and fasting glucose were documented for less than 10% of the whole patient population, for about 15% of those aged 40 years or older and for 26% of patients with hypertension. About 30% of patients with diabetes had a recorded value of fasting glucose and a little more than 25% of patients with diabetes had total cholesterol documented in patient records. Total cardiovascular risk was assessed among 67% of women and 65% of men having hypertension and of 61% of women and 65% of men having diabetes. About 60% of patients with hypertension had prescription for an antihypertensive drug.
Table 4. Process and outcome indicators for women and men by patient group

BP = blood pressure; WHO/ISH score = World Health Organization/International Society of Hypertension risk prediction score; FG = fasting glucose; TC = total cholesterol; HT = hypertension; SBP = systolic blood pressure; DBP = diastolic blood pressure.
* See definitions in Table 1.
In general, 89% of women and 84% of men in patient population had blood pressure under 140/90 mmHg (Table 4). Fasting glucose was normal among 92% of women and 88% of men of whom it had been measured. Similarly total cholesterol was normal in about three-quarters of patients from whom it had been measured. Blood pressure control was achieved among 61% of women and 53% of men with hypertension. Based on fasting glucose, 61% of women with diabetes and 43% of men achieved the treatment target < 7 mmol/L. As the proportion of patients with measurement of total cholesterol or fasting glucose was reasonably low, the assessment of treatment targets is not fully relevant, but as shown by the data it could be done if the coverage of measurements would be better.
Discussion
In general, the information in the database of the eHealth Center enabled the identification of different patient populations and analyses of various process and outcome indicators on management of NCDs. The database allowed patient-level analyses, the legibility of data was good, and the structured database enabled easy data extraction and variable formation. Regarding the quality of the data, the biggest inaccuracies were the discrepancies in coding practices between physicians which were also reported in a study by Klompas et al. (Reference Klompas, Murphy, Lankiewicz, McVetta, Lazarus, Eggleston, Daly, Oppedisano, Beagan, Kirby and Platt2011) and were observed earlier also in Kyrgyzstan in a quality of care review carried out in 2017 (World Health Organization, 2018). This creates difficulties in determining accurate denominators for the calculation of disease prevalences.
The information produced could be easily used nationally in following the health service use and monitoring of some key performance indicators in the service system. Up to our knowledge, this is the first study reporting such a work and analyses done in LMIC. Also, possibilities for similar analyses are so far scarce as national electronic databases including patient-level data do not exist in LMICs.
The analyses showed that in general blood pressure was measured quite actively among the whole patient population and very actively among patients with a chronic condition like diagnosed hypertension or diabetes. However, according to the national protocol which is based on the WHO PEN protocol, biological risk factors should be actively screened among population aged 40 years or more, and among them the measurement rates for blood pressure were not higher compared with the total patient population and cholesterol and blood glucose were measured only among about 15% of them (World Health Organization, 2013). This type of information is useful when evaluating the screening and treatment processes in the service system. It is worth noticing that our data included information for only 1 year and for fasting glucose and total cholesterol even for a shorter period and thus does not give a fully right picture on the situation as according to the recommendations yearly screenings are not mandatory for patients with low risk.
There is not much data published earlier from Kyrgyzstan, but according to WHO Global Health Observatory estimates, the prevalence of raised blood pressure (SBP ≥ 140 OR DBP ≥ 90) was in 2015 in men aged 18 years or more 27.4% and in women 25.7% and the prevalence of diabetes 9.9% of men and 10.8% of women both being clearly higher compared with the results based on this study (The Global Health Observatory (WHO), 2020a; The Global Health Observatory (WHO), 2020b). However, it is obvious that the prevalence of diagnosed patients based on clinical records differ from the population estimates, especially if based on elevated risk factor levels.
There are some problems and challenges to overcome in embedding information and communication technology (ICT) and EHR systems in clinical care in developing countries. These include hardware and software compatibility, lack of quality control, and antiquated infrastructure (Williams and Boren, Reference Williams and Boren2008). Also in Kyrgyzstan, these challenges were observed as the process of electronic data entry timely at the appointment and transfer to the central database worked only partly and in some clinics, the initial phase of data entry was still performed separately from paper records. In addition to need of human resources, it disallows the professionals to taking advantage of the EHR as they cannot use it for example to search information from earlier visits.
One of the strengths of the national electronic PHC database in Kyrgyzstan is nationally standardized content allowing comparable data analyses from different clinics. This would allow automated EHR-based surveillance increasing the quantity, coverage, and timeliness of available data to health authorities compared with traditional surveillance methods (Klompas et al., Reference Klompas, McVetta, Lazarus, Eggleston, Haney, Kruskal, Yih, Daly, Oppedisano, Beagan, Lee, Kirby, Heisey-Grove, DeMaria and Platt2012).
One of the key disadvantages of the data collection process in Kyrgyzstan is that unique identifiers for patients are given on the clinic level. Patients moving to another area or visiting different clinics will get a new identification code. This is the main limit of interoperability of the current system and can cause underestimation of actual visits to services, prescription of medications, and procedures or measurements carried out if patients fragment their care between different service providers (Klompas et al., Reference Klompas, McVetta, Lazarus, Eggleston, Haney, Kruskal, Yih, Daly, Oppedisano, Beagan, Lee, Kirby, Heisey-Grove, DeMaria and Platt2012). Assurance of standardization and interoperability of systems are crucial to avoid fragmentation of the information environment (Janett and Yeracaris, Reference Janett and Yeracaris2020; Klompas et al., Reference Klompas, McVetta, Lazarus, Eggleston, Haney, Kruskal, Yih, Daly, Oppedisano, Beagan, Lee, Kirby, Heisey-Grove, DeMaria and Platt2012). Especially, in developing countries due to lack of resources and various needs of different organizations and departments, the development of comprehensive ICT systems and universal, standardized EHRs fulfilling all the needs is extremely complicated. Thus, it is common that every department implements their own technology making the communication of systems impossible (Williams and Boren, Reference Williams and Boren2008). This challenge has been avoided in Kyrgyzstan as the current system is nationwide and directed by the MoH following the national eHealth strategy (Government of the Kyrgyz Republic, 2015). Bitton et al. (Reference Bitton, Fifield, Ratcliffe, Karlage, Wang, Veillard, Schwarz and Hirschhorn2019) addressed in their scoping review the need for research and development of approaches ensuring the interoperability between data sources, scalable and affordable eHealth approaches and innovations strengthening the information systems without significant needs for changes in infrastructure.
In Kyrgyzstan, the EHRs are currently mainly used to collect data for centralized purposes. However, EHRs have shown to have structural and process benefits also at service provider level and they have been shown to improve the legibility of clinical notes (Holroyd-Leduc et al., Reference Holroyd-Leduc, Lorenzetti, Straus, Sykes and Quan2011). In Kyrgyzstan, the current system could be much more utilized also at the clinic level to support the work of professionals. The quality of care review in Kyrgyzstan already recommended that the Mandatory Health Insurance Fund (MHIF) should use the patient-based data for feedback, learning, and improvement, and that for the purpose national databases should be required to provide either aggregated analyses of the data to individual health facilities (World Health Organization, 2018). That would, however, also need some infrastructure development. A meta-analysis carried out by Campanella et al. (Reference Campanella, Lovato, Marone, Fallacara, Mancuso, Ricciardi and Specchia2015) suggests that EHRs can increase time efficiency and guideline adherence, reduce medication errors, and adverse drug effects. There is also some evidence that introduction of EHRs support the communication between professionals and patients by e-mail and telephone and thus reduce the demand for primary care office visits (Zhou et al., Reference Zhou, Garrido, Chin, Wiesenthal and Liang2007).
If well established, the EHRs can streamline the measurement and analysis of data on clinical performance metrics. However, that needs properly configured systems, accurately completed data fields, and that the software application supports the measurement and reporting process (Janett and Yeracaris, Reference Janett and Yeracaris2020). This pilot study from Kyrgyzstan also showed that the improvement of data quality would need active use of data, identification of mistakes and discrepancies, and further continuous interaction with professionals and other staff entering the data. Also the contents of data collection and correspondingly the structure of the database should be developed to support both the clinical work and the needs of centralized data collection and monitoring.
Implementation of EHRs in developing countries requires human resources, funds, systematic collection of data, and effective monitoring of the existing system. Governments, health managers, and administrators have to have a strong commitment and make also investments (Williams and Boren, Reference Williams and Boren2008). In addition, health care systems should be advised how to prioritize what kind of data to collect and incorporate to EHRs (Rudin et al., Reference Rudin, Friedberg, Shekelle, Shah and Bates2020). However, this study increased evidence that useful information for national monitoring can be obtained already with reasonably straightforward solutions if the national agreement, commitment, and guidance are on place.
This pilot study on extracting and analyzing national primary care EHR data from Kyrgyzstan showed that even a rather basic system gathering nationally patient-level data to an electronic database can serve as an excellent information source for national authorities. This study was part of a large project commissioned by WHO to support the MoH and MHIF in developing the evaluation of the service system and especially the quality assessment of PHC and the choice of appropriate performance indicators with special focus on hypertension care. Following the aims of the larger project, the results have been thoroughly discussed with the MoH and MHIF. The project included also training and capacity building of eHealth, academic, and MHIF staff enabling similar data extraction and analyses in future and on a larger scale. Local professionals have already been able to replicate this process with some other clinics.
Authors’ contribution
TL, JF, AA and LI designed and concepted the study. IC and BS were responsible in retrieving the raw data and contributed to the preparation of data for analyses. LI carried out the statistical analyses. All the authors participated in the interpretation of the data. TL and LI drafted the manuscript. All the authors critically reviewed and approved the final version of the manuscript.
Financial support
This work was supported by the WHO Regional Office for Europe, with support of grants from the Governments of Denmark and the Russian Federation.
Conflicts of interest
None.
Ethical standards
The study has been carried out using information on electronic health records only. Patients have not been contacted. All the information has been analyzed using pseudonymized data.