Introduction
There have been considerable efforts by sub-Saharan African (SSA) countries to improve access to primary health care services, partly through the implementation of risk-pooling community or national health insurance schemes (Jowett et al., Reference Jowett, Deolalikar and Martinsson2004; Witter & Garshong, Reference Witter and Garshong2009; Robyn et al., Reference Robyn, Sauerborn and Barnighausen2013). Universal health insurance coverage programmes, such as Ghana’s National Health Insurance Scheme (NHIS), are vital mechanisms for ensuring equity in access to and use of health care services, via the removal of financial barriers associated with seeking treatment in health care facilities (Bennett, Reference Bennett2004; Agyepong & Adjei, Reference Agyepong and Adjei2008; Blanchet et al., Reference Blanchet, Fink and Osei-Akoto2012). Community-based and national health insurance schemes also offer additional funds for health care financing (Jowett et al., Reference Jowett, Deolalikar and Martinsson2004; Gnawali et al., Reference Gnawali, Pokhrel, Sié, Sanon, De Allegri, Souares, Dong and Sauerborn2009). Yet, evidence from existing studies in the sub-region shows payment of health insurance premiums remains a significant challenge and impacts the utilization of health care services (Dixon et al., Reference Dixon, Tenkorang and Luginaah2011; Jehu-Appiah et al., Reference Jehu-Appiah, Aryeetey, Spaan, de Hoop, Agyepong and Baltussen2011; Aryeetey et al., Reference Aryeetey, Jehu-Appiah, Kotoh, Spaan, Arhinful, Baltussen, van der Geest and Agyepong2013). As a consequence, direct out-of-pocket payment for health care services still remains a predominant practice (McIntyre et al., Reference McIntyre, Thiede, Dahlgren and Whitehead2006; Gnawali et al., Reference Gnawali, Pokhrel, Sié, Sanon, De Allegri, Souares, Dong and Sauerborn2009; Saksena et al., Reference Saksena, Antunes, Xu, Musango and Carrin2011; Kusi et al., Reference Kusi, Enemark, Hansen and Asante2015). In Ghana, this expenditure accounts for nearly half of the total expenditure on health care (Akazili et al., Reference Akazili, Garshong, Aikins, Gyapong and McIntyre2012). At the household level, inability to pay for insurance premiums excludes many people, particularly those with low socioeconomic status, from enrolling in insurance schemes (Dixon et al., Reference Dixon, Tenkorang and Luginaah2011; Jehu-Appiah et al., Reference Jehu-Appiah, Aryeetey, Spaan, de Hoop, Agyepong and Baltussen2011; Kusi et al., Reference Kusi, Enemark, Hansen and Asante2015). Thus, access to basic health care services in the formal health care system still remains a significant challenge for many poor and vulnerable populations in Ghana and SSA.
Despite the growing availability of modern or Western health care services, significant sections of populations in Ghana and other SSA countries continue to rely on indigenous healing practices (traditional medicine – TM) for their health care needs (Pouliot, Reference Pouliot2011; Sato, Reference Sato2012a; Thorsen and Pouliot, Reference Thorsen and Pouliot2015). TM refers to healing knowledge, skills and practices based on the traditions, cultural beliefs and experiences indigenous to different communities or cultures (WHO, 2002). It comprises of the use of animal-based, plant-based and mineral-based medicine, as well as, the use of spiritual therapies in the prevention, diagnosis, improvement and treatment of physical and psychosocial illness (World Health Organisation, 2013). Traditional medical practitioners include herbalist, bone setters, faith healers and spiritualist (Amegbor Reference Amegbor2014; World Health Organisation, 2013; Lakshmi et al., Reference Lakshmi, Nambiar, Narayan, Sathyanarayana, Porter and Sheikh2015). Evidence from existing studies show that TM is effective in treating various illness and common health conditions such as malaria, cholera and typhoid, as well as complex health issues such as infertility (O’Brien et al., Reference O’Brien, Soliman, Annan, Lartey, Awuah and Merajver2012; Thorsen and Pouliot, Reference Thorsen and Pouliot2015; Towns and Van Andel, Reference Towns and Van Andel2016). Reports indicate that between 60% and 80% of the population in SSA rely on indigenous medical remedies, including herbal medicine for their primary health care needs (World Health Organisation, 2013; McFarlane, Reference McFarlane2015; Thorsen and Pouliot, Reference Thorsen and Pouliot2015).
The vital role of TM in health and health care delivery is particularly evident among rural residents, the poor and vulnerable populations (Aikins & Marks, Reference Aikins and Marks2007; Powell-Jackson et al., Reference Powell-Jackson, Hanson, Whitty and Ansah2014). Among these populations, barriers to Western health care services include unavailability and inadequate health care facilities and practitioners, cost of care and other sociocultural beliefs (Tabi et al., Reference Tabi, Powell and Hodnicki2006; Pouliot, Reference Pouliot2011; Sato, Reference Sato2012b; Kuuire et al., Reference Kuuire, Bisung, Rishworth, Dixon and Luginaah2015). On the contrary, TM is readily available, accessible and affordable for these segments of the population (Macha et al., Reference Macha, Harris, Garshong, Ataguba, Akazili, Kuwawenaruwa and Borghi2012; Sato, Reference Sato2012b). Though TM use is often associated with basic health problems, studies in Ghana reveals its use is particularly higher among patients with multiple acute and chronic health conditions (Sato, Reference Sato2012b; Aikins et al., Reference Aikins, Kushitor, Koram, Gyamfi and Ogedegbe2014). Likewise, studies report that patients with non-communicable diseases (NCDs), such as hypertension and diabetes, view Western services for their health care needs as expensive and inaccessible, thereby resorting to the use of TMs (Aikins et al., Reference Aikins, Kushitor, Koram, Gyamfi and Ogedegbe2014; Aikins et al., Reference Aikins, Awuah, Pera, Mendez and Ogedegbe2015). The surge in NCDs in SSA coupled with the demand for TM has led to the emergence of quack TM healers whose practices pose a health danger to the poor and vulnerable that patronize their services (Abdullahi, Reference Abdullahi2011; Kigen et al., Reference Kigen, Ronoh, Kipkore and Rotich2013).
The objective of this paper is to examine the effects of wealth and health insurance status on the use of TM among older persons (persons aged 60 years and above) in Ghana. While there is a plethora of literature on the effect of wealth and health insurance on health care-seeking behaviour in Ghana (see Kuuire et al., Reference Kuuire, Tenkorang, Rishworth, Luginaah and Yawson2017; Jehu-Appiah et al., Reference Jehu-Appiah, Aryeetey, Spaan, de Hoop, Agyepong and Baltussen2011; Dixon et al., Reference Dixon, Tenkorang and Luginaah2011), our understanding of how these factors influence the decision around seeking Western or traditional health care remain limited among older people. Existing studies on health care-seeking behaviour among Ghana’s older adult population focus on the effects of socioeconomic factors on NHIS enrolment (Kuuire et al., Reference Kuuire, Tenkorang, Rishworth, Luginaah and Yawson2017) and the impacts of NHIS status on health care utilization (Fenny et al., Reference Fenny, Asante, Arhinful, Kusi, Parmar and Williams2016; Dalinjong et al., Reference Dalinjong, Welaga, Akazili, Kwarteng, Bangha, Oduro, Sankoh and Goudge2017; van der Wielen et al., Reference van der Wielen, Channon and Falkingham2018). Moreover, the discussions in these papers ignore the vital role TM play in health and health care–seeking behaviour of people, especially the poor and vulnerable in society – including the older persons. TM utilization is predominant among Ghanaians with chronic health conditions (Sato, Reference Sato2012b; Aikins et al., Reference Aikins, Awuah, Pera, Mendez and Ogedegbe2015), and research shows that older persons are more susceptible to chronic health conditions compared to younger persons (Aikins et al., Reference Aikins, Kushitor, Koram, Gyamfi and Ogedegbe2014; Prince et al., Reference Prince, Wu, Guo, Gutierrez Robledo, O’Donnell, Sullivan and Yusuf2015). Currently, the NHIS provides limited coverage for chronic conditions (such as hypertension) and does not cover treatment outside the biomedical care setting, including TM (Barimah, Reference Barimah2013; Aikins et al., Reference Aikins, Kushitor, Koram, Gyamfi and Ogedegbe2014).
Ghana has an estimated 1.6 million older persons (6.7% of the country’s total population) and this is expected to quadruple to about 4.8 million in 2050 (8.9% of the country’s estimated population in 2050) (Amegbor et al., Reference Amegbor, Kuuire, Robertson and Kuffuora2018; Minicuci et al., Reference Minicuci, Biritwum, Mensah, Yawson, Naidoo, Chatterji and Kowal2014; World Health Organisation, 2014). Understanding the health-seeking behaviour of this rapidly growing section of the population is useful for providing relevant policy direction that contributes to improved health and well-being of older persons. Importantly also, prevalence of NCDs is usually considerably higher among older persons (Aikins et al., Reference Aikins, Boynton and Atanga2010; Amegbor et al., Reference Amegbor, Kuuire, Robertson and Kuffuora2018; Minicuci et al., Reference Minicuci, Biritwum, Mensah, Yawson, Naidoo, Chatterji and Kowal2014), although such conditions are not currently covered under the NHIS and could potentially influence health-seeking behaviours, including the use of TM, due to associated cost of treatment. This context provides the impetus for examining how health insurance and wealth status impact the use of TM among older Ghanaians. Thus, controlling for other factors, the paper assumes that (1) individuals with health insurance coverage and (2) individuals in higher income/wealth categories will be less likely to use traditional healers as their most frequent source of treatment during illness.
Materials and methods
Data
Data for the study comes from the World Health Organisation’s Study of Global Ageing and Adult Health (SAGE). SAGE has a longitudinal design and involves collecting data on the health needs of older persons in five countries including Ghana. Irrespective of the focus on persons who are 50 and older, a small sample of persons aged between 18 and 49 were also included for comparison. We used the first wave of the SAGE data collected in Ghana between January 2007 and December 2008 through face-to-face interviews with respondents who were selected via a stratified multi-stage sampling strategy. While the survey for Wave 2 has been completed, the data are not currently available, hence our decision to use data from Wave 1. The first stage involved stratifying the sample by the 10 administrative regions in Ghana and by rural/urban location. From this, primary sampling units consisting of 235 enumeration areas (EAs) were selected. All EAs that did not have residents who are 50 years or older were excluded. A total of 5269 households were surveyed with some 5573 individuals sampled from these households. An estimated response rate of 86% and 80% were achieved at the household and individual levels respectively. However, this study uses a sub-sample of individuals who are 60 years or older because this is the official retirement age in Ghana and the age from which individuals are categorized as older persons. The final analytical samples used in the study were 2256.
Measures
Dependent variable: The dependent variable (frequently used health care type) for this study was a measure of the type of health care frequently used by older persons during the last three years. We derived this variable from the following question: “Thinking about health care you needed in the last three years, where did you go most often when you felt sick or needed to consult someone about your health?” Response categories were as follows: private doctor’s office, private clinic or health care facility, private hospital, public clinic or health care facility, public hospital, charity or church-run clinic, charity or church-run hospital, traditional healer, pharmacy or dispensary and other. Except respondents who used a traditional healer (recoded “1 = traditional medicine”), all responses were recoded as “0 = modern health facility”.
Focal independent variables: Health insurance coverage, the focal independent variable in the study was obtained from the question ‘do [you] have health insurance coverage?’ with the following response options: ‘Yes, mandatory insurance’, ‘Yes, voluntary insurance’, ‘Yes, both mandatory and voluntary insurance’ and ‘No, none’. The responses were operationalized to indicate whether respondents had health insurance or not (coded 0 = uninsured and 1 = insured). The second focal independent variable in this study, wealth status, was measured by income quintile which is a household asset–based measure of wealth provided in the data. Income quintile was coded as follows: 0 = richest, 1 = richer, 2 = middle, 3 = poorer and 4 = poorest.
Other independent variables: We included theoretically relevant demographic and socioeconomic variables in the study based on existing literature on health-seeking behaviours. The demographic variables included in the study were age; sex (coded 1 = male, 2 = female); ethnicity (coded 1 = Akan, 2 = Ewe/Ga-Adangbe, 3 = Gruma/Mole-Dagbani, 4 = other ethnic group); religion (coded 1 = Christian, 2 = Muslim, 3 = Traditional, 4 = Other religion/none); education (coded 0 = no formal education, 1 = primary, 2 = secondary/higher); sector of current or sector of former occupation if currently retired (coded 1 = self-employed, 2 = public/private sector, 3 = informal sector); current employment status (coded 0 = unemployed/retired, 1 = employed); marital status (coded 1 = married, 2 = separated/divorced, 3 = widowed) and location of residence (coded 1 = urban, 2 = rural). We also included respondents’ self-rated health (coded 1 = good, 2 = moderate, 3 = bad), and whether they had ever been diagnosed with at least one NCD (hypertension, stroke, angina, diabetes and asthma) as control variables.
Analytical strategy
We employed descriptive statistics, bivariate and multivariate regression techniques in analysing the data. For the regression models, we adopted the negative loglog link function in estimating the relationship between the outcome and independent variables. The choice of this technique was informed by the skewed nature of the distribution between the categories of our outcome variable (modern health facility = 96.8%; TM = 3.2%). Unlike the logit link function, the negative loglog link function accounts for the specific problem of skewed distributions where lower categories of the binary outcome are more probable. This avoids the possibility of obtaining biased parameter estimates. In all bivariate and multivariate analyses, we imposed respondents’ identification number as a cluster variable due to the hierarchical nature of the data. This strategy prevents the violation of the independence assumption in standard regression models. Missing cases in the data were handled by using the multiple imputation technique. All analyses were undertaken following the completion of the multiple imputations in STATA 14. Analyses also accounted for the sampling weight provided in the data.
Results
Descriptive
From Table 1, most respondents (∼97%) often relied on private or public modern health facilities, while only a small section of respondents (∼3%) used the services of TM practitioners. A little over half (∼55%) of seniors in Ghana do not have health insurance coverage. Most respondents were Akan (∼48%), Christian (∼70%), had no formal education (∼63%), were self-employed (∼80%), married (∼54%) and resided in rural locations (∼60%). Majority of seniors reported they do not have an NCD (∼63%) and close to half reported their health status as moderate (∼45%).
Table 1. Distribution of study variables (n = 2256)
Bivariate
Figure 1 shows only variables that emerged as predictors of the outcome variable at the bivariate level. The results show that there is a statistically significant relationship between the two focal independent variables and the most frequently used type of health care. Seniors who are insured have a 2% decrease in the odds of seeking treatment from TM healers compared to their counterparts who are uninsured. Overall, seniors who belonged to lower income quintiles had higher odds of seeking TM. For example, compared to the richest, the poorest seniors had a 4% increase odds of frequently seeking TM. Similarly, compared to the richest, seniors who belonged to poorer and middle income quintiles had 2% and 5% increased odds of frequently using TM, respectively.
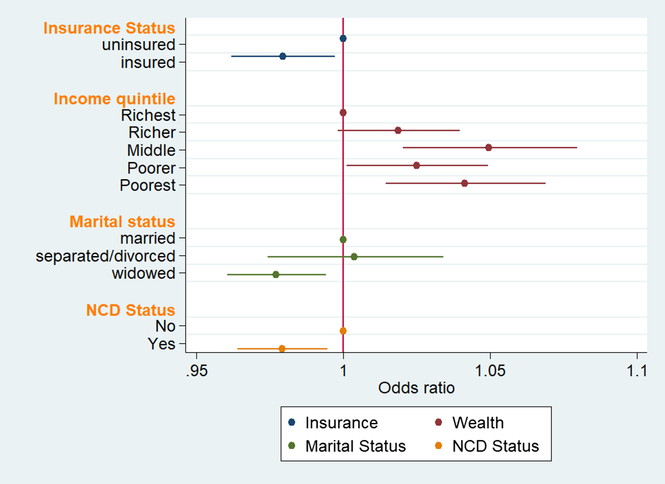
Figure 1. Bivariate negative loglog regression of ‘frequently used health care type’ (n = 2256)
In addition to the two focal independent variables, two other independent variables were significantly associated with the type of health care (see Table 2). Respondents who indicated they were widowed had 2% decreased odds of frequently using TM compared to seniors who are married. Seniors who indicated they had one or more NCD had a 2% decrease in the odds of seeking TM compared to those who had no NCD.
Table 2. Bivariate negative loglog regression of ‘frequently used health care type’ (n = 2256)
*** p < 0.001, ** p < 0.01, * p < 0.05
Multivariate
It is important to note that there was a general significant increase in the size of the parameter estimates in the multivariate results (see Table 3). Figure 2 shows the visual comparison in the changes in the coefficient estimates for the focal independent variables between Models 1 and 2. In Model 1, only income quintile was significantly associated with ‘frequently used health care type’ in the last three years. Further investigation revealed that income quintile suppressed the relationship between insurance status and ‘frequently used health care type’. The findings show that seniors who belonged in the middle income quintile had 56% increased odds of seeking TM compared to the richest. Compared to the richest, the odds for the poorest seniors frequently seeking TM were 48% higher.
Table 3. Multivariate negative loglog regression of ‘frequently used health care type’ (n = 2256)
***p < 0.001, ** p < 0.01, * p < 0.05
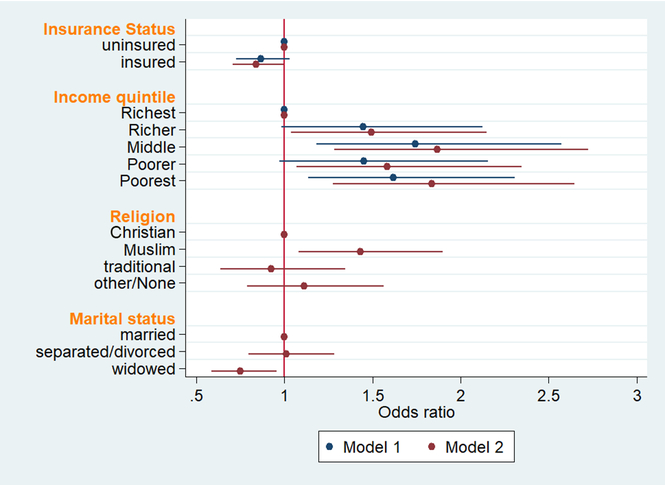
Figure 2. Multivariate negative loglog regression of ‘frequently used health care type’ (n = 2256)
In Model 2, while the relationship between income quintile and ‘frequently used health care type’ remained robust, the relationship between insurance status and ‘frequently used health care type’ also became statistically significant. Further analysis revealed that the relationship between insurance status and ‘frequently used health care type’ was mediated by marital status. Seniors who had health insurance coverage were also 17% less likely to frequently seek treatment from a TM healer relative to the uninsured. The odds of richer seniors seeking treatment from a TM increased by 40% compared to the richest. Seniors in the poorest income quintile observed the highest percentage increase in coefficient estimates between Model 1 and Model 2 (see Figure 2). For this group, the odds of frequently seeking TM increased by 61% when compared to those in the richest quintile.
The results also show that two of the selected socioeconomic variables emerged as significant predictors of ‘frequently used health care type’ in the last three years. While religion had a positive relationship with ‘frequently used health care type’, marital status had a negative relationship. Specifically, seniors who were identified as Muslims had 36% increased odds of frequently seeking TM healers compared to Christians. On the other hand, seniors who indicated they were widowed had 29% decreased odds of frequently seeking TM relative to those who were married.
Discussion and Conclusion
Our study sought to examine the effect of health insurance and wealth status on health care–seeking behaviour of older people in Ghana. It is a widely held believe that TM is a popular form of health care – in terms of access, cost, availability and acceptance – in Ghana and other SSA countries (Pouliot, Reference Pouliot2011; Sato, Reference Sato2012a; Powell-Jackson et al., Reference Powell-Jackson, Hanson, Whitty and Ansah2014). Recent evidence in the literature questions this widely acclaimed popularity of TM in Ghana and SSA, particularly without adequate consideration for the context of utilization (Amegbor, Reference Amegbor2017a, Reference Amegbor2017b; Sato, Reference Sato2012b). The findings of this study show that the majority of Ghanaian older adults (96.8%) reported using modern health care, which is consistent with evidence from other recent studies (Sato, Reference Sato2012b). The popularity of modern care is restricted not only to health care facilities but also in self-care managing of common diseases such as malaria (Fenny et al., Reference Fenny, Asante, Enemark and Hansen2015). In cases of recurring diseases and chronic diseases, the use of TM tends to be relatively higher than biomedicine (Aikins, Reference Aikins2005; Sato, Reference Sato2012b). The literature further indicates that in remote and rural areas where there are deficiencies in modern health facilities, the population are more likely to use TM to address health care needs (Aikins & Marks, Reference Aikins and Marks2007; Powell-Jackson et al., Reference Powell-Jackson, Hanson, Whitty and Ansah2014). Findings in this paper demonstrate the need to contextualize TM utilization with prevailing health care cost and means of payment.
Health insurance coverage remains a crucial enabling resource for accessing modern health care services (Fenny et al., Reference Fenny, Asante, Arhinful, Kusi, Parmar and Williams2016). It provides a higher degree of financial risk protection against cost associated with seeking treatment. It also reduces health care expenditure significantly for insured persons (Saksena et al., Reference Saksena, Antunes, Xu, Musango and Carrin2011; Kusi et al., Reference Kusi, Enemark, Hansen and Asante2015; Kansanga et al., Reference Kansanga, Asumah Braimah, Antabe, Sano, Kyeremeh and Luginaah2018). However, these risk-pooling and financial protection do not cover TM or other alternative forms of health care. Among the poor and vulnerable, such as older persons in Ghana, inability to pay for modern health care results in delays in seeking treatment or forgoing treatment (Robyn et al., Reference Robyn, Fink, Sié and Sauerborn2012). It is also important to note that a considerable proportion of Ghana’s older adult population is uninsured despite health premium age-exemption criterion for persons 70 years or older (Parmar et al., Reference Parmar, Williams, Dkhimi, Ndiaye, Asante, Arhinful and Mladovsky2014). In view of this, we argue that uninsured older persons do not have the financial cushion associated with seeking modern health care; hence, they may resort to less expensive forms of treatment such as using TM or self-medicating with TM (Amegbor, Reference Amegbor2017a, Reference Amegbor2017b).
Income remains an important determinant of health care–seeking behaviour and health insurance enrolment. A considerable number of persons of lower income status are unenrolled in the NHIS, a situation largely attributable to limited financial capabilities to meet the insurance premium (Dixon et al., Reference Dixon, Tenkorang and Luginaah2011; Jehu-Appiah et al., Reference Jehu-Appiah, Aryeetey, Spaan, de Hoop, Agyepong and Baltussen2011; Aryeetey et al., Reference Aryeetey, Jehu-Appiah, Kotoh, Spaan, Arhinful, Baltussen, van der Geest and Agyepong2013; Kusi et al., Reference Kusi, Enemark, Hansen and Asante2015). In the midst of widespread poverty, individuals often have to make a budgetary trade-off for vital goods such as food, in order to afford the health insurance premiums (Dixon et al., Reference Dixon, Tenkorang and Luginaah2011; Reference Dixon, Luginaah and Mkandawire2014; Fenny et al., Reference Fenny, Asante, Arhinful, Kusi, Parmar and Williams2016). Economic vulnerability of persons of lower income, as well as their inability to afford health insurance premiums, means this section of the Ghanaian population have limited access to and use of modern health care services. As evident in this study, older persons in lower income quintiles were more likely to report using TM for their regular health care needs. This may be due to their inability to afford the cost associated with seeking modern care. TM offers a cheaper alternative form of health care for the poor and vulnerable; and it is also readily available in rural communities where most low income older adults live (Parmar et al., Reference Parmar, Williams, Dkhimi, Ndiaye, Asante, Arhinful and Mladovsky2014). As shown in this paper and others, persons with higher incomes are less reliant on TM for their regular health care needs (Pouliot, Reference Pouliot2011; Sato, Reference Sato2012a; Thorsen & Pouliot, Reference Thorsen and Pouliot2015), partly because they can afford the cost associated with seeking modern health care as well as pay premiums for health insurance coverage to guarantee access to modern care when needed (Jehu-Appiah et al., Reference Jehu-Appiah, Aryeetey, Spaan, de Hoop, Agyepong and Baltussen2011; Sato, Reference Sato2012a; Fenny et al., Reference Fenny, Asante, Arhinful, Kusi, Parmar and Williams2016; Dalinjong et al., Reference Dalinjong, Welaga, Akazili, Kwarteng, Bangha, Oduro, Sankoh and Goudge2017). The rich turn to TM only in cases of chronic health where biomedical care fails to provide a cure (Aikins, Reference Aikins2005; Sato, Reference Sato2012b). Even in such situations, they rely on the services of licensed and commercial TM practitioners compared to the poor and disadvantaged who mostly rely on TM for self-treatment or rely on non-commercial TM healers (Amegbor, Reference Amegbor2017a; Pouliot, Reference Pouliot2011).
The findings of our study have several policy implications. Although numerous studies have examined the effect of income and health insurance status on access to modern care, our understanding of how these two variables influence choice between TM and modern care use remain limited. Findings from this study demonstrate that TM is a vital health care resource for poor and uninsured older persons in Ghana. However, the existence of quack healers, untested or counterfeit TM remedies pose a danger to the uninsured and lower income older adults who depend on TM for primary health care and other health needs. Regulation of TM practices and products in Ghana, like most SSA countries, remains a challenge – providing justification for their current exclusion from public health delivery under the Ministry of Health. TM products and remedies in Ghana are largely untested and do not have approval from state regulatory institutions such as the Centre for Plant Medicine Research (CSRPM), the Food and Drugs Authority and the Ghana Standards Authority. Consequently, some TM products may pose health dangers to users due to their potential toxicities (Pouliot, Reference Pouliot2011; Sato, Reference Sato2012b). Thus, there is the need to fast track the inclusion of TM practitioners, drugs and health centres under the Ministry of Health. Including TM under the Ministry of Health must only be undertaken after ascertaining, on a case-by-case basis, efficacy and establishing best practices. This will help minimize the risk of harm for the public, especially for the uninsured and the poor who frequently rely on TM during times of illness.
The findings of this study ought to be considered in view of some limitations. TM, as used in this study does not incorporates the use of TM in self-care context. While a substantial majority of older adults use modern health care for their regular health care needs, the literature demonstrates a high level of TM use in self-care context (Danso-Appiah et al., Reference Danso-Appiah, Stolk, Bosompem, Otchere, Looman, Habbema and de Vlas2010; Pouliot, Reference Pouliot2011; Chipwaza et al., Reference Chipwaza, Mugasa, Mayumana, Amuri, Makungu and Gwakisa2014). Respondents of the SAGE survey may have limited their response to TM to professional care as the response categories only reference the use of professional TM service. Also, the WHO SAGE wave 1 is a cross-sectional data; hence, we cannot draw causal relationships between health insurance status and the ‘frequently used health care type’ or income status and the ‘frequently used health care type’. Future studies can use subsequent waves of SAGE in addition to Wave 1 to examine the temporal effect of health insurance and wealth status on the use of TM among older Ghanaians. Our study also focused on frequent health care–seeking behaviour which may not be similar to health care–seeking behaviour for specific illnesses or disease episodes (Amegbor, Reference Amegbor2017b).
Concerns around efficacy and dosage of TM remain important discussion points that drive the conversation towards incorporating TM in mainstream health care delivery in Ghana. While such ongoing discussions remain important, it is imperative to understand TM utilization patterns, particularly in the context of Ghana’s NHIS health equity mandate. In this paper, we provided evidence of the factors associated with TM use among older Ghanaians. This understanding is important because it provides useful information that can be incorporated in the broader discussion of strategies to improve primary health care access from the perspective of older people’s health utilization behaviours. The findings from our study demonstrate that TM is a popular source of access to health care among uninsured and older persons with lower incomes. This reiterates the need to improve NHIS coverage for poor older persons and calls for the need to regulate TM and incorporate it into the broader health care system. This will go a long way to protect the poor and uninsured older people from seeking treatment from unlicensed TM practitioners.
Author ORCIDs
Prince M. Amegbor 0000-0001-7701-2585
Acknowledgements
We are grateful for the helpful comments from the editors and anonymous reviewers. We are also grateful to the WHO SAGE programme and the Inter-University Consortium for Political and Social Research (ICPSR) for the data used in this study.
Conflict of Interest
None
Ethical Standards
We used data from the World Health Organisation (WHO)’s Study on Global Ageing and Adult Health (SAGE) Wave 1. Our study used a secondary survey data; hence, ethical approval was not required. We accessed the data through Queen’s University library from the Inter-University Consortium for Political and Social Research (ICPSR) platform.








