Introduction
The level of maternal health-care services coverage is a major determinant of maternal, neonatal and infant mortality and the incidence of childhood morbidities and complications during maternity. Maternal health-care coverage is the outcome of two domains of health service availability and utilization that include antenatal care (ANC), care at delivery and postnatal care. Utilization of the recommended maternal health-care services also improves the overall health and well-being of women and children.
In developing countries, inadequate availability and utilization of maternal health-care services are associated with adverse pregnancy outcomes and complications, as well as high risk of maternal, neonatal and infant mortality. Despite several decades of continuing efforts to promote universal coverage of maternal and child health (MCH) programme, service provision and coverage are still at the bottom end of the scale in the socio-economically poorer northern states of India, and particularly among women and children who are in the poorer strata of social and economic scale.
The maternal mortality ratio at the national level for India is one of the highest in the world, although it is estimated to have declined from 400 maternal deaths per 100 000 live births in 1997–98 to 300 in 2001–03 (Registrar General, 2006). However, estimates indicate that in India over 100 000 women die every year from pregnancy- and childbirth-related causes of the 500 000 maternal deaths worldwide (World Health Organization (WHO), 2000). Although infant and child mortality rates in India have been halved in the last three decades, the pace of decline in infant mortality and neonatal mortality has slowed down since the 1990s. Globally, 10 million children die every year before reaching the age of five, of which 2 million occur in India, the highest number in any country worldwide (Black et al., 2003). More than 50% of these 2 million child deaths occur in the first few months of life every year (WHO, 2005).
All these statistics point to the sluggish pace of progress in recent times in the levels of maternal health-care services coverage, though it is a critical and direct contributor to the unacceptably high levels of maternal and neonatal mortality rates in the country. Maternal and child health programme, despite being at the centre stage in public health policy agenda and even as part of the reproductive and child health (RCH) programme in the aftermath of International Conference on Population and Development conference in 1994, suffers from continued neglect. There are several areas of neglect, particularly in the demographically backward northern states of India in improving the quality of existing and new health services infrastructure development. The neglect covers the areas of health services infrastructure development, adequacy of health professionals in health centres, and improvement of personnel and quality of health-care services provision.
ANC
ANC refers to pregnancy-related health care provided by a health worker either in a medical facility or at home. In theory, ANC should address both the psychosocial and medical needs of women within the context of the health-care delivery system and the surrounding culture (WHO, 1996). ANC has two major functions. First, antenatal health check-ups facilitate early detection of several co-implications such as high blood pressure and malnutrition. Second, antenatal visits play a crucial role in preparing a woman and her family for birth by establishing confidence between the woman and the health-care provider and by individualizing promotional health messages (WHO, 1996).
Thus, the recommended content of ANC service provision has three main components:
1) Assessments – include history-taking, physical examination and laboratory tests to identify problems of risk factors.
2) Health promotion – includes advice on nutrition, planning the birth, information about danger signs and contingency planning, subsequent contraception and breastfeeding.
3) Care provision – includes iron and foliate supplements, tetanus toxoid immunization, psychosocial support and record keeping.
ANC provides an opportunity for a variety of preventive interventions for pregnant women, including immunization, nutrition education and counselling about their plans for delivery and postpartum family planning. It also allows women who meet known risk criteria to be identified and monitored and subsequently referred for delivery care. Ideally, pre-existing and new medical problems such as malaria, anaemia and syphilis can also be detected and managed during ANC visits. It is also during such visits that providers can develop rapport with women, making them more likely to seek assistance during labour and delivery, should an emergency occur.
Delivery care
The aim of global safe motherhood programme in 1987 was to ensure that the outcome of every pregnancy is a healthy mother and a healthy newborn. Attendance by a medically trained person during labour and delivery can facilitate such referral and is one goal of the safe motherhood initiative. An important indicator of health service coverage is the proportion of births where the women delivered in a health facility where obstetric complications can be managed (Koblinsky et al., Reference Koblinsky, McLaurin, Russell-Brown and Gorbach1995; Maine et al., Reference Maine, Ward, Wardlaw, McCarthy and Birnbaum1995).
Indian context
In India, since the 1970s, the MCH programme was implemented as a means of preventing maternal deaths and vaccine-preventable child deaths and associated morbidities. In the 1980s, the MCH programme, especially, was sought to be promoted as a route to achieve successful coverage in family planning. However, this revised approach failed to invigorate in the performance of demographically backward states of India. The safe motherhood programme was introduced as a more effective intervention, and the RCH programme initiative was launched in the mid-1990s. Under the RCH programme, MCH services were expanded to cover reproductive health package as a whole. The RCH package included the earlier components of safe motherhood programmes, child survival including that of diarrhoeal diseases control. The full programme of RCH was launched as a new package in 1996.
Highly pronounced regional variations exist in maternal health-care coverage in India. Aside from such regional variations, inequalities by socio-economic status are also striking, which varied across the regions. The consequence of failing to provide maternal and early postnatal care can be seen in the disturbing statistics of very high levels of maternal and early childhood mortality and morbidity prevalence in the empowered action group (EAG) states of Bihar, Chhattisgarh, Jharkhand, Madhya Pradesh, Orissa, Rajasthan, Uttar Pradesh and Uttaranchal.
Access and demand
Service availability and demand for services are two critical dimensions of determinants of maternal health-care utilization. The percentage of population utilizing various health-care services among different socio-economic strata of population is indicative of complementary effects of both demand for and access to health-care services. The demand factors comprising the various maternal, demographic and socio-economic factors tend to alter the individual's perception, influence the decision to seek health care and determine the ability of the individual to do so. Overall, demand-side factors tend to increase the propensity of the women to use maternal health-care services.
Accessibility to services comprises several components such as service availability, accessibility to information about services and quality of services. The role of socio-economic demand factors tends to decline with increasing access. Effective health interventions such as the MCH programme are a means to achieve reduction in inequalities by socio-economic status. Upscaling accessibility to maternal health services is an important route of generating higher demand. Reduced demand due to fear of side effects and misconception regarding modern medical care can be overcome by service accessibility and quality. Thus, access and demand factors mediate both independently and complementarily on maternal health-care utilization.
Demand determinants
The demand for maternal health services comprises the ability and willingness of families and women to adopt new health behaviour. The demand force includes a variety of factors such as household resources, socio-economic characteristics, community norm, price, quality and availability of services (Claeson and Waldman, Reference Claeson and Waldman2000). The demand factors have a strong bearing in the utilization of maternal health services especially with severe constraints in access to health care. Consequently, studies in the 1980s and 1990s dealt with the issue of low MCH service utilization in the developing countries by concentrating on demand determinants (Becker et al., Reference Becker, Peters, Gray, Gultiano and Black1993; Goldman and Pebley, Reference Goldman and Pebley1994; Magadi et al., Reference Magadi, Madise and Rodrigues2000).
Demand for maternal health services tends to rise with improvements in social and economic conditions of women and their families. In contrast, low demand is a critical factor where coverage is at the lower end of the scale. The demand for services is lower because of cultural barriers, poor socio-economic status and poor knowledge of the importance of MCH, and above all poor access on the other side of the spectrum. These factors either individually or in combination determine higher or lesser demand. The pathways of demand factors influence are reviewed under categories of maternal and demographic factors, cultural factors and household economic conditions.
Mother's education is a strong predictor of maternal health-care services, with varying degrees and pattern of influence across different social and cultural settings. A study in Bangladesh indicated that women with primary schooling did not differ from women with no schooling in the utilization of MCH services (Raghupathy, Reference Raghupathy1996). In Guatemala, women with primary schooling are more likely to use MCH services (Goldman and Pebley, Reference Goldman and Pebley1994). However, studies have consistently demonstrated across different social contexts an increase of MCH service utilization for women with middle school and higher education. Other researchers have argued that the relationship between women's education and health-care utilization is not necessarily due to the influence of education, but rather due to women's childhood background, for which education may serve as a proxy (Behrman and Wolfe, Reference Behrman and Wolfe1987). Similarly, urban women are more likely to use ANC, controlling for education (Raghupathy, Reference Raghupathy1996).
The link between women's work status and MCH utilization has been widely studied. Working women tend to have greater knowledge about pregnancy and childbirths because of greater freedom of movement outside the household and are likely to seek information on services available for pregnancy care during their work (Desai and Jain, Reference Desai and Jain1994). However, in developing countries such as India, studies have shown a contrasting trend. Women's work participation in rural areas is poverty induced and therefore it tends to have a negative impact on the use of their health-care services, as it involves substantial opportunity and monetary costs to women (Basu and Basu, Reference Basu and Basu1991; Desai and Jain, Reference Desai and Jain1994; Roy et al., Reference Roy, Khumtakar, Berman and Zeitlin1997). In urban areas, however, MCH coverage tends to be higher for working women.
Studies have also documented differences in maternal health-care utilization by demographic determinants of age and parity of women. Younger women are more likely to use maternal health care, but age differences are not consensually established. Parity of the mother has been shown to be negatively correlated with the level of maternal care service utilization. High parities are negatively associated with the likelihood of receiving ANC and giving birth in a medical institution (Elo, Reference Elo1992; Bhatia and Cleland, Reference Bhatia and Cleland1995; Raghupathy, Reference Raghupathy1996). One of the causal links is that high-parity women are generally from poor socio-economic strata.
Religion and caste in broader contexts represent household and community-level cultural norms and behaviours that are likely to mediate in the use of MCH care services. In India, Scheduled Caste/Tribe communities are in general socially discriminated against and economically poor. They have less exposure, poor access in general to primary health care and face acute constraints in terms of access to MCH services (Retherford and Mishra, Reference Retherford and Mishra1997).
Household economic condition is known to have a strong demand effect on health services utilization. In a comparative perspective, although economic status may provide the resources to use the services, women's education may provide a greater ability to use the services. In this way, each may lead to very distinguishable effects against the context of differences in access to health care and cultural factors contributing to the variations. It is also likely that economic status and education have differential effects on maternal than child health-care services utilization. In rural subsistence economy, wealth effects constitute a powerful determinant of health-care use and consequently can cause swings in child mortality. Demand functions contain the economic core of the model in child survival analysis (Schultz, Reference Schultz1984). A closely related phenomenon of economic prosperity is exposure to mass media whose influence on health-care use is seen to be emerging strongly, in recent analyses.
The north–south dichotomy of India is also unique, with distinct differences in terms of socio-economic and cultural condition (Dyson and Moore, Reference Dyson and Moore1983). South Indian women typically enjoy greater freedom as an outcome of the Dravidian cultural norm, kinship structure and higher level of literacy, education and employment. North Indian women are strongly subjected to the Aryan cultural tradition of secluding women under purdha and less likely to work outside the home. A comparative analysis of the demand and access factors across the states will provide an important basis to assess the differences arising from cultural context. For example, given that level of access in a state is the same and controlling for other demand factors, lower utilization of maternal care services for women or for girls compared with immunization for male children is likely to indicate differential demand because of prevalent cultural norm in a population.
Access determinants
Strengthening the existing and creating new access (infrastructure) to health-care services is critical for raising utilization. Research on the relative role of access factors was seriously hampered because of lack of data, as very few surveys gathered data on both access and demand-side factors. As a result, a major part of previous research focussed on demand factors, ignoring the role of community access factors on health care utilization.
Access to health-care services is an important requirement to create willingness among the people to use the maternal health services (Navaneetham and Dharmalingam, Reference Navaneetham and Dharmalingam2002). Accessibility to services comprises three components: infrastructure, availability of personnel and quality of services. Some recent studies have focussed on community influence in terms of the effect of village characteristics on health-care use (Tsui, Reference Tsui1985; Entwisle and Sayed, Reference Entwisle and Sayed1989; Tienda, Reference Tienda1991). Access to health care is now viewed in terms of a more comprehensive framework, comprising three dimensions, namely, availability of services, information about health services and accessibility of information to services.
Context and objectives
Previous studies concentrated on studying the impact of individual- and household-level socio-economic factors on health-care use. The potential importance of community access remained less focussed, both because of narrow conceptualization with focus on demand factors and non-availability of data at the community level. Viewed from this context, the national family health survey (NFHS-2) provides useful village-level access data including access to road, health and school facilities. These data representing both access to health services and information on accessibility to health services are effectively used to measure community access.
Therefore, the purpose of this analysis is to compare the role of access vis-à-vis demand determinants of maternal health services utilization. On the basis of the overall framework of access and demand determinants, first, we compare the differentials in the levels of maternal health coverage across the states of India. Second, we estimate the relative influence of access and demand determinants of utilization of maternal health-care services.
The main aim is the examination of the extent to which health-related behaviour is homogeneous within the household and within communities. That is the degree to which observed consistency in behaviour with respect to maternal health-care utilization can be accounted for by social and economic status at individual and household level on the one hand and access to health services in terms of health, road and education facilities, on the other, across selected Indian states.
Data and methods
Data from the three rounds of national family health survey of India (NFHS-1, -2 and -3) conducted in 1992–93, 1998–99 and 2005–06 are used in this analysis. The NFHS sample is nationally representative and covers more than 99% (eg, NFHS-3 sample covers 29 states of India and excluded Union Territories from the sampling framework) of India's population (International Institute for Population Sciences (IIPS), 2007). The urban and rural samples within each state were drawn separately, and the sample within each state was allocated proportionally to the size of the state's urban and rural populations. A uniform sample design was adopted in all states. In each state, the rural sample was selected in two stages, with the selection of Primary Sampling Units (PSUs), which are villages, with probability proportional to population size (PPS) at the first stage, followed by the random selection of households within each PSU in the second stage. In urban areas, a three-stage sampling procedure was followed. In the first stage, wards were selected with PPS sampling. In the next stage, one census enumeration block (CEB) was randomly selected from each sample ward. In the final stage, households were randomly selected within each selected CEB.
NFHS is designed for self-weighting at the domain level. The domains are the urban and rural areas of each state. This means that all households and individuals in the same domain will share a common household weight and individual weight, respectively. The design weight is the inverse of the overall sampling fraction in each domain. The overall sampling fraction is the product of the selection probabilities at each sampling stage (two stages in rural areas and three stages in urban areas). The design weight was adjusted for household non-response in the calculation of the household sampling weight. The household sampling weight was further adjusted for individual non-response to obtain the individual sampling weight. Both adjustments for non-response were done at the domain level in order to preserve the self-weighting nature of the sample within domains. The sampling weights were further normalized at the national level to obtain national standard weights and at the state level to obtain standard state weights for each state. The national standard weights were normalized so that the total number of weighted cases equals the total number of unweighted cases at the national level.
The response rates for all three rounds of NFHS follow the same pattern (IIPS, 1995; 2000; 2007). For example, in NFHS-3, a total of 109 041 households were interviewed. The household response rate, that is, the number of households interviewed per 100 occupied households, was 98% for India as a whole, 97% in urban areas and 99% in rural areas. The household response rate was 96% or higher in all states. The individual response rate, that is, the number of completed interviews per 100 eligible women identified in the households, was 95% for the country as a whole (93% in urban areas and 96% in rural areas).
The MCH module provides data on the utilization of ANC and delivery care including child immunization. The MCH module provides data on maternal health care for three births in the last four years in NFHS-1, for two births in the last three years in NFHS-2 and for all births in the last five years in NFHS-3. In NFHS-3, the analyses of ANC coverage indicators are restricted for the last birth to ever-married women in the five years preceding the survey. However, information on delivery care is available for all births in the five years preceding the survey in NFHS-3.
The results of this analysis are presented in two sections. First, statewise profiles of maternal health-care utilization from NFHS-1, -2 and -3 are presented to compare the trends. Second, the influence of demand and access factors of health care use estimated from multi-level logistic regression models are presented for selected states of India. Multi-level analyses are limited to rural sample of ANC utilization and safe delivery coverage, as NFHS-2 provides data on community access for rural areas only.
In multi-level regression analyses, we use (a) fully recommended ANC and (b) safe deliveryFootnote 1 coverage as the dependant variables. The full ANC is estimated at the child level, that is, percentage of births whose mothers received recommended maternal health care. Similarly, safe delivery is estimated as the percentage of births delivered in medical facility or assisted by a health professional. The coverage of full ANC is the percentage of the recommended maternal health care that the programme provides: three antenatal visits including first trimester check, two injections of tetanus vaccination and recommended intake of iron and folic acid (IFAC) supplements. We use the composite variable of fully recommended ANC by scoring all the above components except first trimester care. Second, variable ‘safe delivery’ is measured as ‘either hospital delivery or deliveries assisted by health personnel’. The predictor variables comprised two dimensions of community-level access factors and demand factors that represented individual- and household-level variables. The method of multi-level regression model estimation and the predictors used in the models are described in the section on multi-level analyses. The multi-level analysis is restricted to NFHS-2 data. Though, NFHS-3 data set more recent (now in public domain) but it does not permit multi-level analysis involving community factors because village level data were not collected. The main reason why village-level data were not collected in NFHS-3 was that ethical guidelines did not permit collection of data at village/community level, as that would jeopardize anonymity and confidentiality clause of the informed consent protocol relating to HIV prevalence data collection in NFHS-3.
Maternal health-care coverage in states
At the national level for India, full ANC coverage was 34% in NFHS-1 (1992–93), which rose marginally to 35% in NFHS-2 (1998–99), and subsequently the ANC coverage has increased to 41% in NFHS-3. A major concern that strikes is the regional inequalities in the levels and pace of increase in maternal health-care coverage across the states of India. The coverage in three ANC visits varies from a low of 17% in Bihar to a high of 96% in Tamil Nadu (NFHS, 2005–06). This uneven progress is paradoxical in the sense that ANC coverage as a component of reproductive health coverage is in a stagnant phase in states where it is required to increase most.
Table 1 compares the levels of various components of antenatal health-care services coverage among the Indian states over three rounds of NFHS. The coverage disaggregated by ANC components provides useful clues to see which component of ANC is contributing to the change in ANC coverage. Despite the overall trend of marginal increase in the level of full ANC coverage from NFHS-1 to NFHS-2, ANC-3 checks of ANC during pregnancy indicate a reverse (declining) trend in Bihar, Uttar Pradesh and Punjab (Figure 1). Comparatively, the levels of tetanus and IFAC use have increased in most of the states from NFHS-1 to NFHS-2. Tetanus use has increased substantially in most low to medium coverage states. The decline in the coverage of ANC-3 checks in the states where full ANC coverage declined from NFHS-1 to NFHS-2 reveals that the programme has placed emphasis on tetanus vaccination. However, between NFHS-2 and NFHS-3, the ANC coverage (three or more visits) showed increase in all states except Kerala, where it showed a marginal decline from 98% to 94%.
Table 1 Percent distribution of births whose mothers received recommended maternal health care in major states and India, NFHS-1, -2 and -3 (1992–93, 1998–99 and 2005–06)

NFHS = national family health survey; TT2+ = two and more doses tetanus toxoid injection; ANC-FT = antenatal check-first trimester; ANC3+ = three and more antenatal checks; IFAC = iron folic acid tablets.
Full ANC = TT2 + ANC3 + IFAC.
Note: Table is based on last three births to ever-married women in the 4 years preceding the survey in NFHS-1, for last two births in the 3 years preceding the survey in NFHS-2 and last birth to ever-married women in the 5 years preceding the survey in NFHS-3.

Figure 1 Trends in percentage of women receiving ANC (three visits), NFHS-1, -2 and -3, 1992–93, 1998–99, 2005–06. ANC = antenatal care; NFHS = national family health survey.
Delivery in medical institutions or assistance of a professional health worker during delivery is a critical component of maternal health care. Rising trend in these two indicators is very strongly associated with maternal, infant and child mortality reduction. Unlike the mixed increasing and decreasing trend in full ANC coverage, the percentage of deliveries in medical institutions increased in every state during NFHS-1 to NFHS-2 and NFHS-3 (Figure 2). The better-performing south Indian states have recorded very significant increases in the coverage of both institutional and safe deliveries over the three rounds of NFHS (Table 2). However, institutional delivery coverage is still about 20% in Uttar Pradesh and Bihar. Such low coverage of ANC and delivery in medical institutions for these states suggest the long way ahead to achieve universal coverage. This has serious implications for achieving reduction in infant and child mortality in conjunction with national health policy and the UN millennium development goals (MDGs).

Figure 2 Trends in coverage of institutional delivery by states and India, NFHS-1, -2 and -3, 1992–93, 1998–99, 2005–06. ANC = antenatal care; NFHS = national family health survey.
Table 2 Percentage of births delivered in medical facilities and assisted by health professionals in states and India, NFHS-1, -2 and -3 (1992–93, 1998–99 and 2005–06)
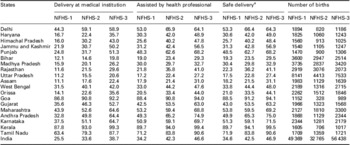
NFHS = national family health survey.
aDelivered in a medical facility or assisted by a health professional.
Note: Table is based on last three births to ever-married women in the 4 years preceding the survey in NFHS-1, for last two births in the 3 years preceding the survey in NFHS-2, and all births to ever-married women in the 5 years preceding the survey in NFHS-3.
Socio-economic and demographic differentials in full ANC and coverage of safe deliveries in selected states of India, NFHS-2, 1998–99
Results further indicate significant differentials in full ANC coverage by several socio-economic demand factors, which tend to vary with the overall ANC coverage among the states and the cultural context in which women may be constrained to seek ANC (Appendix Table A1). In the state of Bihar, the fully recommended maternal care coverage was merely 5% for illiterate women, which rose to about 45% for women who completed high school. In Tamil Nadu, more than 75% of illiterate women have received full ANC; in addition, the proportion of illiterate women is also lower. Similarly, the economic differential in ANC utilization is significantly higher in the states of Bihar, Madhya Pradesh, Orissa and Punjab.
The differentials by socio-economic demand factors are the highest in the low-ANC coverage and in demographically less-advanced states. Correspondingly, the differences in ANC coverage by socio-economic factors are comparatively lower for states such as Tamil Nadu and Andhra Pradesh because overall ANC utilization is very high. Both these trends support the inference that low fertility is linked to rising maternal health-care utilization. Thus, the differentials due to the demand effect of socio-economic conditions tend to narrow down or nearly wipe out where policy intervention has led to the reduction in inequalities in health care accessibility. As a result, health-care utilization has risen to high levels across socio-economic categories.
Analysis of safe delivery coverage shows that considerable levels of socio-economic and demographic differentials exist at the state level (Appendix Table A2). Household economic status explains a major part of the differentials in the coverage of safe delivery. Women who are exposed to any mass media are expected to give birth at the medical institutions or are assisted by health professionals.
Access and demand variables in multi-level analyses
The decision to use health care for mothers during pregnancy and delivery is shaped by both demand for and access to health services. The demand and access factors that operate at different levels are individual, household, village or community access to health services or other contextual factors that cover community norms. In this analysis, we adopt a two-dimensional, demand and supply, and three-level (multi-level) variables framework. On the basis of this two-dimensional framework, influences of hierarchically clustered data at individual, household and community level are examined using multi-level logistic regression models. The multi-level analyses include variables defined at three levels: individual, household and community level (village-level access). The individual and household factors represent demand factors, and the community access variables constitute the supply determinants of maternal health care.
In this framework, maternal health-care-seeking behaviour or use of health care is influenced by the following ways:
a) Demographic factors (individual level) may shape women's desire to use health care (see Stephenson and Tsui, Reference Stephenson and Tsui2002).
b) Socio-economic factors (individual and household) determine ability and resources to use the services availability.
c) Service availability comprises health-care infrastructure and development infrastructure. Community health-care services availability that comprises health-care facility and related development infrastructure (school and road) provides necessary community access to health-care services. It also collectively represents community accessibility and aspiration to use health-care services.
The multi-level logistic regression model includes individual-level predictor variables such as women's age at birth, parity, education and work status. The household-level predictor variables include husband's education, exposure to media, household economic status index, religion and caste.
The NFHS-2 survey provides data on three aspects of community access, that is, availability of health, road and education facility in the villages. The role of community access on health-care use is studied by scoring the above three facilities into a single composite community access variable. The choice of using each of these three factors as separate community access predictor was considered, but was not found suitable. The composite community access variable is scored with three categories viz. villages having no health facilities, villages having at least health facilities and villages having all the three facilities.
Multi-level analyses have been done for selected states of Andhra Pradesh, Tamil Nadu, Bihar, Madhya Pradesh, Orissa, Gujarat, Punjab and northeastern states (combined). The states have been selected to represent regional distribution and variations in demographic and health conditions. Among the four large north Indian states, Bihar and Madhya Pradesh were selected considering their similarities in demographic and health achievements to Uttar Pradesh and Rajasthan, respectively. Among south Indian states, Tamil Nadu was selected instead of Kerala, as sample size was a constraint for Kerala for multi-level analyses.
Multi-level logistic regression models
Multi-level logistic model comprising three-level covariates – individual, household and community – is estimated to determine the comparative influence of individual effect of each of the factors and their collective impact at each level on the utilization of maternal health care and safe delivery in selected states of rural India. The model estimates the coefficients of the effects of community-, household- and individual-level variables separately (a) on the utilization of maternal health care and (b) safe delivery.
The multi-level logistic regression model takes the form of
Where, ln [P ijk/(1 − P ijk)] is the logit in which P ijk is the probability of using maternal health care for the i th children in household j in community k, X ijk, W jk and Z k are the vectors of individual-, household- and community-level characteristics. The β, α and λ are the vectors of estimated parameters coefficients and ujk and εk are unexplained residual terms at the household and community levels, respectively.
The multi-level logistic models provide estimates of random effect at the family and community level and the three-level covariates, controlling for random effects and linkages among the covariates. The desegregation of effects of covariates effects at three levels provides greater clarity in the interpretation of independent causal linkages of the covariates. Statewise logistic regression estimates of coefficients for the covariates on full ANC utilization and safe delivery including random effects are presented in Table 3 and Table 4, respectively.
Table 3 Multilevel logistic regression estimates (coefficients) of full antenatal care useFootnote a in rural areas of selected states, 1998–99

TT2+ = two and more doses tetanus toxoid injection; ANC3+ = three and more antenatal checks; IFAC = iron folic acid tablets.
* <0.1; **<0.05; ***<0.01.
a Full ANC = TT2 + ANC3 + IFAC.
b Includes Arunachal Pradesh, Manipur, Meghalaya, Mizoram, Nagaland, Sikkim and Tripura.
Note: The results are estimated using the second order penalized quasi likelihood (PQL) method to give the least biased estimates. The default estimation procedure is a Restricted Iterative version of Generalized Least Squares (RIGLS), the restricted version leading to unbiased estimates of random parameters.
Table 4 Multilevel logistic regression estimates (coefficients) of safe delivery coverage in rural areas of selected states, 1998–99

*<0.1; **<0.05; ***<0.01.
aIncludes Arunachal Pradesh, Manipur, Meghalaya, Mizoram, Nagaland, Sikkim and Tripura.
Note: The results are estimated using the second order penalized quasi likelihood (PQL) method to give the least biased estimates. The default estimation procedure is a Restricted Iterative version of Generalized Least Squares (RIGLS), the restricted version leading to unbiased estimates of random parameters.
Differentials in full ANC coverage
Individual covariates
Among the four individual covariates, mother's parity and education shows consistent and significant effect on full utilization of ANC care. Parity shows significant negative effect on full ANC utilization for higher parities of women consistently in most states. The parity effect on ANC remains stronger for most states and is greater in states with greater proportion of women with higher parities. Possible explanations for this are women of higher parity drawing on their maternity experiences may not feel the need to receive care during pregnancy and childbirths. It may be suggested that women of lower parity (2 and less) tend to pay more attention to health-care needs of their children (Celik and Hotchkiss, Reference Celik and Hotchkiss2000). Women with high parities also have greater difficulty than others in accessing health-care services because of economic and cultural constraints, as higher parities are often associated with lower socio-economic status (Stephenson and Tsui, Reference Stephenson and Tsui2002).
Coefficients demonstrate a consistently higher impact of mother's education on full antenatal health-care utilization. The education impact is greater in Bihar and Madhya Pradesh, where full ANC coverage is at the bottom end of the scale. There are three broad possible ways, which can explain the higher level of utilization of maternal health services among the educated mothers.
First, educated women are better able to break away from the tradition to utilize modern means of safeguarding their own health and that of their children (Caldwell and Caldwell, Reference Caldwell and Caldwell1988; Cleland, Reference Cleland1990). Second, educated women are better able to utilize what is available in the community to their advantage (Barrera, Reference Barrera1990; Caldwell and Caldwell, Reference Caldwell and Caldwell1990; Goodburn et al., Reference Goodburn, Ebrahim and Senapati1990). Third, educated women may be able to make independent decisions regarding their own and their children's health, leading to greater utilization of health facilities (Caldwell, Reference Caldwell1979; Caldwell, Reference Caldwell1986).
Results show a mixed trend of positive and negative effect of women's age on ANC utilization, but the results are not statistically significant (at 5% level) for most states, and as established in previous studies working women are found to be associated with lower utilization of ANC care compared with women who are not working (Navaneetham and Dharmalingam, Reference Navaneetham and Dharmalingam2002). However, no consistent pattern is indicated in terms of the statistical significance of women employment status effect.
Household covariates
Cross-sectional studies are helpful to separate the effects of household income on maternal health care. Among the household-level covariates, higher household economic status index indicates a strong positive influence on utilization of full ANC in most states. As demonstrated in previous studies, household economic condition shows a tremendous demand effect on maternal health-care utilization in Bihar and Madhya Pradesh, the states with limited access to health-care services. Household wealth enhances the ability of the families to seek health-care services.
Most previous analyses ignored husband's literacy based on the understanding that the mother's education has the strongest influence on maternal health, whereas husband's education has a less dominant impact. Frameworks dealing with the updated reproductive package emphasize the involvement of husband's decision in seeking health-care services for women. Results indicate that the following aspects – household economic status and husband's education – emerge as a significant predictor of full ANC utilization. Given the patriarchal culture of Indian society, the husband's decision turns out to be important in seeking health-care services. Husband's education could be valuable for health-care use from that context.
Women's exposure to mass media indicates a positive impact on full ANC utilization among all the states. Although statistically not significant across all the states, exposure to media tends to act as a demand factor, as it provides accessibility to information about health services availability and the need for utilization. The other household-level covariates, religion and caste, which represent cultural and socio-economic status differences, are also consistently related to ANC utilization. In general, the ANC utilization is lower for Muslim compared with Hindu women and Scheduled Caste and Scheduled Tribe women compared with non-SC/ST women, respectively.
Community access factor
The twofold aim of multi-level analyses is to determine the role of community access factors and the extent of unobserved random effects. The community access factor is represented by the composite variable of village facility index. The index comprising health, school and road facility reveals that the availability of health facility in the villages is significantly related to higher utilization of ANC compared with villages with no health facility in most states. The category that considers availability of all three facilities of health, education and road is also significantly related to higher utilization of full ANC in most states. The results demonstrate that community accessibility is critical and has to be comprehensive to impact ANC utilization.
There are three unique outcomes in this multi-level analysis of ANC utilization. First, women's education emerges as the most powerful predictor of ANC utilization, accounting for random effect at three levels in contrast to what ordinary least square (OLS) regression, which does not account for unobserved heterogeneity, could indicate. Second, the random effects at the household level are substantial, as seen from reduction of random effects from individual to household, which are indicated by the household-level factors. Household economic status index indicates a strong demand effect on ANC utilization at the household level. Third, there is substantial reduction of random effects at the community level, implying that the composite village facility index accounts for major influence through community access. However, the remainder random effects at the community level imply that there is still a small portion of unexplained random effects in the model.
ANC utilization by access to health personnel
A related dimension of community access is the presence of various health professionals in rural areas, which may directly impact the level of maternal coverage in developing countries. In the quality of care and health-care section of the women questionnaire, women were asked to report on the availability and access to the following health personnel. These community access-related factors include availability in the village of a regular private doctor, a visiting private doctor, village health guide, availability of traditional attendant and availability of mobile health unit. We present evidence of differentials in full ANC utilization by the above health access-related factors (Appendix Table A3). Availability of private doctor, visiting doctor and village health guide in the villages is seen to be associated with higher utilization of full ANC in Bihar, Madhya Pradesh and Orissa. The availability of mobile health unit in the village is associated with higher utilization of full ANC consistently in all the selected states.
Appendix Table A1 Percentage of full ANCFootnote a coverage by demographic and socio-economic factors in selected states, NFHS (1998–99)

TT2+ = two and more doses tetanus toxoid injection; ANC3+ = three and more antenatal checks; IFAC = iron folic acid tablets.
a Full ANC = TT2 + ANC3 + IFAC.
b Includes Arunachal Pradesh, Manipur, Meghalaya, Mizoram, Nagaland, Sikkim and Tripura.
Table A2 Percentage of safe deliveriesFootnote a by demographic and socio-economic factors in selected states, NFHS (1998–99)

a Delivered in a medical facility or assisted by a health professional.
b Includes Arunachal Pradesh, Manipur, Meghalaya, Mizoram, Nagaland, Sikkim and Tripura.
Table A3 Percentage of mothers who received full antenatal careFootnote a by access-related factors in rural areas of selected states, 1998–99

TT2+ = two and more doses tetanus toxoid injection; ANC3+ = three and more antenatal checks; IFAC = iron folic acid tablets; VHG = Village Health Guide; TBA = Traditional Birth Attendant; MHU = Mobile Health Unit.
a Full ANC = TT2 + ANC3 + IFAC.
Differentials in safe delivery
Safe delivery, which includes deliveries in medical institutions or deliveries assisted by health personnel, is a critical component of maternal health care in terms of its impact on maternal and infant mortality. On the basis of multinomial logistic regression model estimates, we examine the evidence of the effects of demographic, socio-economic characteristics and community-level variables to understand the extent of the influence of demand and access factors on safe deliveries (Table 4).
Coefficients indicate that higher parities are associated with lower coverage of deliveries in medical institutions. Women having less than three parities are much more likely to deliver their children in medical institution or assisted by a health professional compared with women of more than three parities in most of the states.
The level of births delivered in medical institutions or assisted by health professionals increases with the educational level of women and of their husbands as well. Clearly, there is a greater demand effect of both women and their husbands’ education on safe delivery coverage in low-coverage states of Bihar, Madhya Pradesh and northeastern states. The sharp increases in safe delivery coverage with the levels of household economic status suggest a strong demand effect of household economic condition. The likelihood of safe deliveries are higher among mothers who were exposed to any mass media compared with their counterparts particularly in low-coverage states. Overall, the safe delivery is higher for other religions compared with Hindus and Muslims. However, in Tamil Nadu, Gujarat and Punjab, the coverage of safe deliveries is higher for Muslim compared with Hindu mothers.
The community-level access factors emerge as crucial determining factors of safe delivery coverage. The presence of health facility has a significant positive impact on safe delivery coverage in the states of Andhra Pradesh, Bihar, Madhya Pradesh, Orissa, Gujarat and North Eastern states.
Discussion and conclusion
In this research, we assessed the progress and efficacy of maternal health-care utilization among Indian states using the three rounds of NFHS. The results of state-level ANC coverage demonstrate: first, about the regional pattern of differential coverage in maternal health care services and second about differential coverage by different type of maternal health care. Overall, ANC coverage improved from NFHS-1 to NFHS-2 in better-performing south Indian states, but ANC coverage indicated poorly performing northern states of Uttar Pradesh, Bihar and Madhya Pradesh. Data further show a declining trend in coverage of ANC-3 checks in the states where full ANC coverage declined from NFHS-1 to NFHS-2, suggesting that maternal health programme focussed more on tetanus vaccination during this phase; full ANC coverage, however, increased in most states during NFHS-2 to NFHS-3.
Second, coverage of deliveries in medical institutions is still about 20% or <20% in Uttar Pradesh, Bihar, Rajasthan, Madhya Pradesh, Orissa and Assam, which has serious implications for achieving reduction in infant and child mortality in conjunction with national health policy and millennium development goals.
Third, on the basis of the two-dimensional access and demand framework, multi-level analyses based on NFHS-2 data illustrate evidence of the extent of the impact of demand and access determinants on maternal health-care utilization. Maternal education, exposure to mass media, husband's education and household economic status emerge as strong demand determinants of full ANC utilization. Of the demographic factors, women's parity displays substantial impact, but women's age at birth of the child shows much less impact.
Disaggregated demand effects reveal that women's education is a powerful individual-level determinant, whereas household economic status is a strong determinant of full ANC utilization at the household level. The extent of educational differences in ANC utilization further varies significantly with the regional inequalities in overall ANC coverage of the states and the cultural context in which women are constrained to seek ANC. Women's education itself is the result of many different factors at the community, household and individual level, which may interact in influencing maternal health-care utilization. The explanation from several studies for this overwhelming demand effect of women's education is that educated mothers are more likely to have greater awareness, autonomy and decision-making ability to use ANC services.
Among the household-level covariates, household economic condition, husband's education and exposure mass to media have strong demand effects on maternal health-care utilization and safe delivery coverage. Household wealth is known to enhance the ability of the families to seek health-care services. The results confirm the emerging importance of husband's education as a complementing determinant leading to a greater involvement in seeking and using maternal health and delivery care. Mass media exposure is a source of learning on health-care services’ accessibility and availability, and therefore evidence shows significant demand effects of media exposure on maternal health-care utilization.
The pattern of evidence suggests that inequalities in maternal health-care coverage by socio-economic status have narrowed down because of greater access to health care in the south Indian states where ANC coverage is very high. The greater economic progress and social advancement in these states are also part of the reason coupled with access-driven demand across different socio-economic strata. In contrast, in the low-ANC coverage states, individual and household-level socio-economic conditions operate as powerful demand determinants.
Evidence also suggests that maternal health-care utilization is greatly influenced by cultural norms, socio-economic status and awareness about the importance of health care for mothers. For example, in Punjab and Haryana, where patriarchal norms are very strong, the proportion of children covered under child immunization is closer to the levels of utilization in Tamil Nadu, Kerala and Goa (NFHS, 1998–99). Yet, the percentage of women covered by all recommended ANC services is less than half of this. The regional context of cultural differences are likely to mediate, resulting in such regional variation in coverage, because the cultural norms contributed by patriarchal structure of the families in the northern states tend to act as enormous barriers for utilizing modern health care for women during maternity and delivery.
Fourth, as community-level data were collected and available in NFHS-2 data set, we embraced the opportunity to explore the impact of village-level covariates of health-care access on maternal health-care utilization, whereas most previous studies confined themselves by examining the role of household and individual covariates health-care utilization. The finding of the multi-level regression models incorporating village-level covariates will help planners and policymakers to address issues related to demand and supply dimensions of health-care utilization among Indian states. The results of multi-level analysis based on NFHS-2 data provide considerable evidence-based research and policy implications even in the current context, in the absence of community-based data in NFHS-3.
In multi-level analyses of NFHS-2 data, the composite variable of village facility index indicate that compared with villages with no health facility, those with health facility in general and those with all three community access facilities health, education and road are associated with higher utilization of full ANC utilization and safe delivery coverage. The effect of this composite community access variable is especially higher in major states where ANC coverage levels are lower. Significance of village-level clustering effects is, however, not fully accounted for across all the states, leaving out a small remainder of the community effects that the predictors of the model have not been able to explain. This might arise because of several reasons including the shortcoming of NFHS village-level community access. For example, NFHS does not provide data on all dimensions of village-level access factors such as health personnel availability and so on.
Fifth, evidence indicates that better-performing states have achieved progress by creating access in terms of infrastructure, personnel and quality of care and an efficient delivery strategy that includes routine home visits for maternal care. These states also have greater thrust on public health and public health institutions, leading to greater access to the poor and the poorest. Corroborative evidence from NFHS-3 results point to the fact that the proportion using private health care is greater compared with the proportion using public health care (IIPS, 2007). For example, more than a third of deliveries have taken place in private health institutions compared with less than a third in public health institutions with the rest at home.
Finally, the poor availability of health services as a critical constraint is not simply the lack of health facility but access to information on the availability and critical benefits of health care are very important inputs to overcome cultural barriers and the general reluctance in maternal health-care utilization.











