Introduction
Developing countries in demographic transition face problems of increasing prevalence of chronic conditions and their complications (Yach et al., Reference Yach, Hawkes, Linn Gould and Hoffmann2004). However, in spite of this growing burden, these low- and middle-income countries (LMIC) are still more acute disease oriented. Such is the case in the Philippines, where the leading causes of mortality for the past 20 years have been chronic conditions (Philippine Department of Health, n.d.), but the public health is generally still oriented to acute and infectious diseases.
The approach to chronic care is very different from the acute disease-oriented approach practiced in most LMIC: in addition to the disease prevention and drug prescription activities usually carried out in acute disease care, chronic care also focusses on disability limitation and rehabilitation (Longino et al., Reference Longino, Pardeck and Murphy1998) and gives particular attention to the psychosocial aspects of the patient (DeRidder et al., Reference De Ridder, Geenen, Kuijer and van Middendoerp2008). Models for chronic care have been introduced, more commonly in high-income countries (HIC), where care for chronic conditions has long been in the forefront and where resources are more readily available.
Published evidence suggests that practices re-designed in accordance with Wagner’s (Reference Wagner1998) Chronic Care Model (CCM) generally improved quality of care and outcomes for patients with various chronic illnesses (Coleman et al., Reference Coleman, Austin, Brach and Wagner2009). Studies conducted on the implementation of the CCM in HIC demonstrated significant correlations between specific CCM elements and better health outcomes (Nutting et al., Reference Nutting, Perry Dickinson, Miriam Dickinson, Nelson, King, Crabtree and Glasgow2007; Coleman et al., Reference Coleman, Austin, Brach and Wagner2009); the number, kind and degree of elements of the CCM implemented may vary depending on many contextual and organizational factors (Cretin et al., Reference Cretin, Shortell and Keeler2008). Taking into consideration numerous economic, socio-political and health problems encountered in LMICs, the World Health Organization (2007) introduced a more flexible model – the Innovative Care for Chronic Conditions Framework (ICCC).
Each country, its people and healthcare system have unique characteristics and possess certain strengths and weaknesses; a single solution in a one-size-fits-all approach would not be most effective and efficient everywhere. Thus, the investigators aimed to adapt a model for chronic care based on the local context and implement selected elements of this context-adapted chronic care model (CACCM) in the hope of improving first-line chronic care making use of diabetes mellitus type 2 (type 2 DM) as the representative condition in the City of Batac and municipality of Pagudpud in Northern Philippines. The possible effects of the implemented CACCM elements on Patients’ Assessment of Chronic Illness Care (PACIC) and glycaemia in people with diabetes were explored in this study.
Background
Public healthcare in the Philippines was devolved in 1992, and the responsibility of providing basic healthcare services for the people was handed down to local governments, specifically municipalities and cities. A decade before this healthcare devolution, the country implemented a primary healthcare policy that created a large cadre of community-based health workers locally called ‘barangay health workers’ (BHW). The barangay (village) is the smallest unit of government; a city or a municipality would be composed of a number of barangays.
Batac [population=53 542 as of 2010 (Philippine National Statistics Office, 2010)] is a non-highly urbanized component city in the island of Luzon ∼470 km to the north of Metro Manila, which is accessible by air and land transportation. It is composed of 43 barangays. The local government health unit (LGHU) operates two healthcare centres with barangay health stations. Other healthcare services available in Batac City are a tertiary-level Department of Health-operated hospital, a primary-level private hospital, a number of private multi-specialty clinics and clinical laboratories, and several private drugstores/pharmacies.
Pagudpud [population=21 877 as of 2010 (Philippine National Statistics Office, 2010)], the northernmost settlement in Luzon, is a rural municipality classified to be very poor in economic development. It is ∼100 km further from Batac City. Composed of 16 barangays, it only has a basic government healthcare centre and barangay health stations for healthcare. There are no laboratory facilities or any private clinics or drugstores/pharmacies.
As in many LMIC, most healthcare expenditures are out-of-pocket.
Similar to most LGHU, organized care for chronic conditions is non-existent in Batac City and Pagudpud. The chronic condition-related activities are limited to informative posters on stroke, high blood pressure, diabetes, chronic lung diseases, smoking cessation, and the benefits of exercise and a healthy diet. There are also one-day annual campaigns on specific conditions, healthy lifestyle, tobacco control, etc., as programmed by the Philippine Department of Health (2013).
Methods
This study was sequenced in three main phases. The first step was context adaptation of the CCM. Steps 2 and 3 involved implementation of selected elements of the CACCM in the two purposively selected LGHU of Batac City and Pagudpud, Ilocos Norte Province, from October 2010 to February 2013. CACCM elements were selected based on the feasibility of implementing these elements in the context, and acceptability and sustainability of the said measures in the two local government units. Step 2 aimed to introduce the issue of type 2 DM to the community. Step 3 aimed at organizing care for people with type 2 DM, which we termed as the First-Line Diabetes Care (FiLDCare) Project. An evaluation of the effects of the implemented CACCM elements was carried out one year after complete implementation. The indicators for expected improvement used in this study were as follows: improvements in PACIC and glycaemia control as measured through glycosylated haemoglobin (HbA1c) levels.
Step 1: context adaptation of CCM
The investigators adapted existing models and programmes for chronic care delivery to the local context. The main frameworks reviewed for chronic care were the CCM and its offshoots (Wagner, Reference Wagner1998; Cheah, Reference Cheah2001; Bodenheimer et al., Reference Bodenheimer, Wagner and Grumbach2002; Siminerio et al., Reference Siminerio, Piat and Zgibor2005; Campbell et al., Reference Campbell, Murray, Darbyshire, Emery, Farmer, Griffiths, Guthrie, Lester, Wilson and Kinmoth2007; Nutting et al., Reference Nutting, Perry Dickinson, Miriam Dickinson, Nelson, King, Crabtree and Glasgow2007; Cretin et al., Reference Cretin, Shortell and Keeler2008; Greenberg et al., Reference Greenberg, Raymond and Leeder2008; Coleman et al., Reference Coleman, Austin, Brach and Wagner2009; Maher et al., Reference Maher, Harries, Zachariah and Enarson2009) and the ICCC framework (World Health Organization, 2007). The different elements of chronic care, methods by which these were implemented, results of implementation and the feasibility of implementing these elements to the context were considered.
Step 2: CACCM implementation: community sensitization
Community sensitization was conducted through active screening for type 2 DM on a random sample of the population in the villages of the involved local government units from October 2010 to April 2011. Active screening was chosen to introduce the issue of diabetes in the community, augment case finding, establish local prevalence and validate a risk score calculator to identify specific sub-populations on which blood glucose screening strategies could be carried out more systematically in succeeding routine clinical settings. Some of the results of the active screening for type 2 DM carried out in this step are discussed elsewhere (Ku and Kegels, Reference Ku and Kegels2013).
Step 3: CACCM implementation: the FiLDCare Project
The FiLDCare Project was implemented from May 2011 to February 2013. The CACCM elements that were applied were decision support to the healthcare workers, minor re-organization of the healthcare service, and provision for organized diabetes care with emphasis on diabetes self-management education and support (DSME/S) to people with diabetes.
Step 3a: Decision support to healthcare workers and healthcare service re-organization/re-design
The investigators prepared a 32-h training workshop for the Batac City and Pagudpud LGHU staff. The healthcare workers were given lectures and hands-on training on primary diabetes care and development of psychosocial skills, including provision of DSME/S. LGHU staff involvement in this training workshop was excellent and no economic incentives were used.
A basic chronic care team was created making use of pre-existing healthcare staff in both LGHUs. Specific tasks for primary diabetes care and self-management education and support were assigned to different team members.
Step 3b: Provision for organized diabetes care and DSME/S
The trained LGHU staff, organized as chronic care teams, provided primary diabetes care, emphasizing on DSME/S to the cohort with type 2 DM who participated in the FiLDCare Project. Details of the CACCM-based DSME/S activities were discussed elsewhere(Ku & Kegels 2014a, 2014b).
Evaluation of the effects of implementation of the CACCM elements: PACIC ratings and glycaemia of the FiLDCare Project participants
People with diabetes from Batac City and Pagudpud were invited to join the FiLDCare project. Inclusion criteria were as follows: diagnosis of type 2 DM, age ⩾20 years, and willingness to participate in the project. The principal investigator and/or trained field researchers provided information about the complete project and obtained written informed consent from each of the study participants. The researchers conducted one-on-one interviews using structured questionnaires and measured HbA1c making use of A1CNow (Bayer HealthCare, Metro Manila, Philippines) before and one year after full implementation. The A1CNow is a point-of-care test that conforms to the National Glycohaemoglobin Standardization Program protocol. For the participants’ assessment of chronic illness care delivery, Glasgow et al.’s (Reference Glasgow, Whitesides, Nelson and King2005) PACIC was used. The PACIC is composed of 20 questions enquiring about patient activation, delivery-system design, goal setting, problem solving, and follow-up activities of a health service providing chronic care. It makes use of a 5-point Likert scale with 1 (‘almost never’) being the lowest and 5 (‘almost always’) being the highest rating.
In the post-implementation phase interviews of the FiLDCare project participants, open-ended questions were also asked regarding their ‘activation’ on their diabetes; the ‘assistance’ provided by the healthcare service in caring for the condition and in setting goals for health and self-care; the provision of advice and support for ‘problem solving’, mainly on care-related decisions that they have to make outside their contacts with a healthcare provider; and any arrangements made for follow-up and/or for consultations with other healthcare professionals, and how these had affected them.
Statistics
Statistical analyses were carried out using the statistical package Stata/IC (2009). Wilcoxon’s signed-rank test was used to compare the pre- and post-implementation ratings of the PACIC and its subsets (patient activation, delivery-system design, goal setting, problem solving, and follow-up) and to compare the pre- and post-implementation HbA1c levels. Test of proportions was used to compare the proportion in good glycaemic control before and one year after full programme implementation. Any differences between post-implementation PACIC ratings based on the level of post-implementation glycaemic control and the post-implementation PACIC ratings based on the changes in HbA1c levels were determined using Wilcoxon–Mann–Whitney test.
Definitions
HbA1c<7% (<53 mmol/mol) was considered as the cut-off for good glycaemic control (American Diabetes Association, 2010).
For the classification of changes in HbA1c before and after implementation, the investigators considered that, without any interventions, the natural history of diabetes is deterioration through time (DeFronzo, Reference DeFronzo2009), and thus classified unchanged HbA1c together with decreased HbA1C as improvement in glycaemic control.
Ethical considerations
The authors assert that all the procedures contributing to this work comply with the ethical standards of the national and institutional guidelines on human experimentation of Belgium and the University of Antwerp and the Institute of Tropical Medicine, Antwerp (Belgian Reg. No. B30020109490) and of the Philippines and the Mariano Marcos Memorial Hospital and Medical Centre, Batac City, The Philippines, as well as with the Helsinki Declaration of 1975, as revised in 2008. This research was conducted with permission from the government of the Province of Ilocos Norte and the Ilocos Norte Provincial Health Office; the government of the City of Batac and its City Health Office; and the government of the Municipality of Pagudpud and its Municipal Health Office.
Results
The CACCM and selected elements
The CACCM framework is presented in Figure 1. Actors/stakeholders rather than activities or elements were used as the backbone in this framework. Compared with the activities and elements of chronic disease care models that are being used in HIC, these actors are more commonly known in the context of a country and a healthcare system used to providing acute disease care. Activities and elements for chronic care were then listed under each of these actors. Concentrating on the actors and identifying chronic care activities and elements revolving around the actors facilitate the ease of understanding in determining gaps and overlaps and identifying areas for improvement. The CACCM can likewise be adaptive: activities and elements may be added or removed under each of these main actors as the healthcare system transforms towards accommodating the provision of chronic care. Eventually, it may be used as the framework in the provision of good quality healthcare – whether for chronic or acute conditions.

Figure 1 The context-adapted chronic care model
Minor re-organization of the healthcare service and service delivery re-design were carried out through the creation of the First-Line Chronic Care Team (FLCCT; Figure 2) based on the local situation and shifting the task of providing DSMS from the physician/nurse to the midwife/BHW. The FLCCT in this context is composed of the primary care physician, the nurse(s), midwives, and the BHW. The person with diabetes may access healthcare services in the health centre where the physician and the nurse deliver clinical diabetes care and DSME. The midwives may provide DSMS in the healthcare centre as well. On certain days, the midwives visit the community and may give DSMS sessions to people with diabetes in their places of residence. The BHW accomplishes DSMS primarily through home visits. The BHW is under the direct supervision of the midwife; the midwives are under the direct supervision of the nurse(s); and the primary care physician supervises the whole FLCCT.
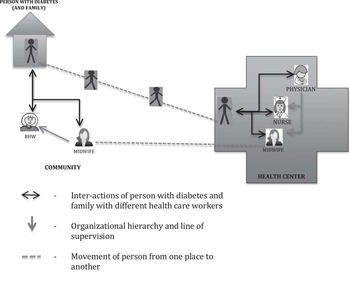
Figure 2 The First-Line Chronic Care Team, set up as adapted to the local situation
Assessment of the implemented CACCM elements: PACIC ratings and glycaemia of the FiLDCare project participants
A total of 203 people with diabetes were enrolled to the FiLDCare project. However, five of them refused any HbA1c testing from the onset, 20 refused any further HbA1c testing, four died, eight migrated, and two refused to take part in the post-implementation interview. These people were excluded from the analysis. Demographics of the participants are listed in Table 1.
Table 1 Demographics of study participants (n=164)
The pre-implementation results showed an overall median PACIC rating of 3.2 out of the highest possible rating of 5. Ratings for the goal setting, problem-solving and follow-up and co-ordination elements of the PACIC were on the centre point of the scale (=3.0). Patient activation was at 3.2 and delivery-system design was at 3.7. Median HbA1c was 7.7% (61 mmol/mol), which is above the cut-off for good glycaemic control.
The post-implementation improvements in PACIC and the HbA1c levels were statistically significant (P=0.009 and <0.001, respectively). All the sub-scales of the PACIC except for delivery-system design likewise demonstrated significant improvements in post-implementation ratings. Median HbA1c decreased to 6.9% (52 mmol/mol), which is the upper limit for good glycaemic control. The results of the PACIC and HbA1c of the FiLDCare project participants are listed in Table 2.
Table 2 Median values of HbA1c, PACIC, and self-assessment of degree of enablement before and after implementation
HbA1c=glycosylated haemoglobin; PACIC=patients’ assessment of chronic illness care.
a Binomial interpolation of confidence intervals.
b Wilcoxon’s signed-rank test.
The proportion of participants with good glycaemic control increased from 37.2% to 50.6% (P=0.014). Regardless of the level of control, HbA1c decreased in 60.5% of the participants, remained the same in 8.0% and increased in 31.5%. Among those with reduced HbA1c, the average change was −1.46 A1C percentage points (−16.0 mmol/mol); when combined with those with unchanged A1C, the average reduction was −1.29 A1C percentage points (−14.1 mmol/mol). Among those with increased A1C, the average change was +1.21 A1C percentage points (+13.2 mmol/mol).
Analysis of the post-implementation findings showed no significant differences in the PACIC ratings between those classified to have ‘good glycaemic control’ and those classified as ‘not in good glycaemic control’ (Table 3). However, significantly higher ratings for the ‘problem solving’ and ‘follow-up and co-ordination’ subsets of the PACIC were noted among those whose HbA1c ‘decreased/remained unchanged’ compared with those whose HbA1c ‘increased’ (Table 4).
Table 3 Median post-implementation PACIC ratings according to post-implementation level of control of diabetes
HbA1c=glycosylated haemoglobin; PACIC=patients’ assessment of chronic illness care.
a Binomial interpolation of confidence intervals.
b Wilcoxon–Mann–Whitney test.
Table 4 Median post-implementation PACIC ratings according to changes in HbA1c
HbA1c=glycosylated haemoglobin; PACIC=patients’ assessment of chronic illness care.
a Binomial interpolation of confidence intervals.
b Wilcoxon–Mann–Whitney test.
Discussion
The usual healthcare system response to chronic care in many LMIC is still characterized by a public healthcare system focussed on prevention programmes; little consideration for the organization, co-ordination and regulation of healthcare services; routine medical practice without attention for the opportunities and resources for the specific aspects of chronic care; and large out-of-pocket expenses for patients (Ku et al., Reference Ku, Idrissi, Bhojani, Kifle, Chenge, Dimbelolo, Nakiwala, Devadasan, Criel, Maniple, Van Olmen and Kegelsn.d.). A better response could be to strengthen the first line and progressively integrate care for chronic conditions with current primary care activities, taking into consideration the capabilities of the healthcare system. Certain LMICs have successfully made use of specific elements of the CCM or the ICCC framework to design systems of care for chronic conditions. The CCM-based Vera–Cruz Initiative for Diabetes Awareness in Mexico reported improved glycaemia among its study participants 18 months after implementation (Pan American Health Organization, 2013). The Russian Federation utilized the ICCC as its framework in conceptualizing secondary prevention of cerebrovascular disease, whereas Rwanda made use of the ICCC framework as its roadmap in designing a system of care for people with HIV-AIDS (Epping-Jordan et al., Reference Epping-Jordan, Pruitt, Bengoa and Wagner2004). However, context adaptations of CCM with the aim of integrating care for chronic conditions with current healthcare activities in LMIC are still rather exceptional.
The CACCM
In constructing the CACCM, the investigators deemed that the four main actors in first-line chronic care would be the person with the chronic condition, the primary healthcare providers, the healthcare service, and the community, and ideally should involve the following main elements:
-
(1). self-care management skills development and support through education, counselling, and behaviour modification of people with chronic conditions and their families with long-term follow-up and periodic assessment of self-care. These may be accomplished by establishing a good patient–primary healthcare provider relationship, a good patient–healthcare team relationship, and mobilization of community resources to provide, among others, a favourable environment for lifestyle changes at local and national policy levels;
-
(2). decision support to primary healthcare workers, including behaviour modification as needed to ensure development of communication and counselling skills and adherence to clinical practice guidelines; quality assurance and supportive supervision; and community support including incentives if and when applicable;
-
(3). organization of the healthcare service and/or delivery-system design as dictated by the needs of the patients and spearheaded by the primary physician, including creation of a chronic healthcare team and training of team members; support from the healthcare team for appropriate division of labour; assurance of availability of necessary equipment and specialists; and adequate support from the government and the community;
-
(4). clinical information system that follows the person seeking healthcare at all levels: from primary to secondary to tertiary and vice versa; and
-
(5). wider community involvement for proper use and allocation of community resources and development of pertinent policies, as well as national and local government resources and policies, through mobilization of the community by concerted efforts of the primary healthcare provider, the healthcare team, and the patients and their families to ensure the availability of a sustainable chronic disease-care programme, to provide a chronic disease care-friendly environment and to create chronic disease care-oriented policies – that is, inclusion of chronic disease care costs in the national health insurance programme, provision of free or subsidized maintenance medications, assurance of availability of basic healthcare services geared towards chronic disease care, provision of areas for group exercise, etc.
An LMIC such as the Philippines does not have adequate resources to implement state-of-the-art interventions for chronic conditions. However, a number of elements of chronic care may still be addressed through minor adjustments in the healthcare system, public/private partnerships, and introduction of low-cost innovations in order to (a) improve chronic healthcare delivery; (b) guarantee that the persons with chronic conditions are ‘activated’, assisted in setting goals for health and self-care and advised and supported during the ‘in-between’ moments when they have to decide for any issues concerning the condition without the immediate aid of a professional healthcare provider (Van Olmen et al., Reference Van Olmen, Ku, Bermejo, Kegels, Hermann and Van Damme2011); and (c) ensure that arrangements have been made for follow-up and/or for consultations with other healthcare professionals.
Evaluation of the implemented CACCM elements
For this research, the investigators conducted initial sensitization of the communities to diabetes, established the provision of decision support to the healthcare workers and introduced the FiLDCare project where they ‘re-organized’ the LGHU by creating the FLCCT, ‘re-designed’ healthcare service delivery by task-shifting and initiated the provision of DSME/S to people with diabetes. Consequently, significant improvements in the assessment of chronic illness care and in the number of people with good control of diabetes were noted.
The increase in the ratings of the PACIC and the improvement in HbA1c levels of the FiLDCare project participants show that, with the implementation of simple but appropriate measures to address chronic disease care, first-line diabetes care may be improved. After implementation of the project, the participants perceived improvements in the patient-activation, goal-setting, problem-solving and follow-up activities of the local government healthcare services. Semi-structured interviews with a number of project participants supported these conclusions.
On ‘patient-activation’ and ‘goal-setting’:
‘I used to resent that I have to do exercises, now I look forward to my early morning brisk walking regimen. There are usually 4 or 5 of us people with diabetes who would walk around (the city square), and we talk and have fun’.
‘(With the self-management education and support that was given)…I felt inspired to control my diabetes’.
Although the intervention involved re-organization and a minor re-design of the healthcare services, the improvement in the subset ‘delivery-system design’ was not statistically significant. The participants expected more than what was done in terms of access to diabetes medicine, laboratory tests, and specialists, where the payments for these are still out-of-pocket:
‘I stayed in (a high-income country) for more than 20 years and when I relocated here I looked for the type of diabetes care that I used to get abroad but I didn’t find it. It is good that there is now this project. …I still pay for my medicine, other laboratory tests and specialist consultations though’.
‘I know I should take all my medicine as prescribed by my doctor but sometimes I do not have enough budget to buy these’.
‘I wish the project would also help us in procuring our medicine’.
Apart from the noted improvements in 4 of the 5 PACIC subsets, this study has shown significantly higher ratings for the ‘problem solving’ and ‘follow-up and co-ordination’ subsets, validated by people whose A1C improved. Some of these people surmised that the FiLDCare project activities have equipped them to deal with their condition and care for their condition:
‘I stopped taking my diabetes medicine because I was afraid. There were times that I would feel weak and sweaty when I take these and I was scared of damaging my kidneys. Now I learned of the side effects of the medicine prescribed me and the effects if I did not do the things I need to do to control my diabetes…’.
‘I was given a prescription good for one month of diabetes medicine. After I consumed all, I thought it was already done and my diabetes was cured. I was not advised otherwise nor were there any arrangements for follow-up. Now I know’.
Study limitations
Although the increase in the PACIC score may connote to a perceived improvement in the first-line diabetes care delivered to people with diabetes, other factors may have contributed to the improvement in the glycaemic control of the FiLDCare project participants beyond the assessed improvement in chronic care as a result of the introduction of a more organized diabetes care in the LGHU and sensitization of the involved communities including local government officials to diabetes and its care. These may include the changes in knowledge, attitude and practises of the project participants, which were discussed separately (Ku and Kegels, Reference Ku and Kegels2014a), and accessibility of HbA1c testing and immediately available results upon consultation at the healthcare unit (Delamater, Reference Delamater2006). The latter effect was not analysed in this study.
Way forward
The project has garnered strong local government support, which has led to the development of local policies on community promotion activities for the prevention of lifestyle-related chronic conditions and complications. The investigators left training and other materials with the local government health officers for future use. The healthcare workers, with the encouragement and support of local government officials, have continued to conduct the self-management education and support activities even after the conclusion of the project. Beyond these, a public–private partnership is being considered to improve access to blood glucose testing by introducing low-cost point-of-care blood glucose monitors to the local government healthcare services, and the Batac City Health Officer has taken initiatives to expand access to diabetes medicine.
Conclusion
This study has shown that first-line diabetes care may be improved through the implementation of certain elements of a CACCM and without causing much strain on an already-burdened healthcare system. The improvements were demonstrated through a significantly higher PACIC rating of the users of the implemented project and a significant reduction in HbA1c of the project participants, as well as an increase in the number of people with good glycaemic control. However, access to medicines, laboratory tests and specialist physicians still needs to be further addressed.
Healthcare systems of LMIC may be able to introduce and improve care for chronic conditions by implementing specific chronic care elements adapted to their context. Such adaptations do not require high level of additional resources to produce positive effects.
Acknowledgements
The authors thank the Belgian Directorate for Development Co-operation through the Institute of Tropical Medicine, Antwerp, for funding this study.
Financial Support
This project was funded by the Belgian Directorate for Development Co-operation through the Institute of Tropical Medicine, Antwerp.
Conflicts of Interest
Neither of the authors have any financial competing interests regarding this research.









