Introduction
An estimated 41 million people worldwide die from noncommunicable diseases (NCDs) each year (World Health Organization, 2018). The pandemic has disrupted millions of lives, with the SARS-CoV-2 virus infecting (at December 15, 2020) more than 71 million people worldwide and causing more than 1.6 million deaths (World Health Organization, 2021a). If infected, people living with NCDs are at higher risk than those without NCDs of developing severe COVID-19-related illness and death (World Health Organization, 2020a). NCD care in healthcare systems, already limited in capacity, has been under further stress, as resources and personnel have been diverted toward control and management of the outbreak.
The burden of NCDs falls disproportionately on people living in LMICs, with more than 85% of premature deaths due to NCDs occurring in low- and middle-income countries (LMICs) (World Health Organization). Effective prevention and management of NCDs may not be possible in LMICs because of the continuing call on resources to prevent and manage infectious diseases and acute conditions (Haque et al., Reference Haque, Islam, Rahman, Mckimm, Abdullah and Dhingra2020). Additionally, broader environmental, political, and social conditions may not be conducive to health promotion activities (Allotey et al., Reference Allotey, Davey and Reidpath2014).
Primary care plays a vital role in the prevention and management of NCDs (World Health Organization, 2021a), for example, in identifying risk factors and providing brief interventions (Beaglehole et al., 2008). Lack of access to primary healthcare services can contribute to and exacerbate the acquisition of NCDs (Haque et al., Reference Haque, Islam, Rahman, Mckimm, Abdullah and Dhingra2020). In LMICs, universal access to affordable quality care of NCDs is achievable only through effective primary care services, such as those provided by frontline health care workers – community health workers, nurses, family physicians/general practitioners, and community pharmacists (Joint Learning Innitiative, 2004).
NCDs during pandemics and natural disasters
During emergencies, routine care provision and on-going management of NCDs may be further disrupted (Ochi et al., Reference Ochi, Hodgson, Landeg, Mayner and Murray2014). Continuity of healthcare may also be impacted by failures in the supply chain of equipment and medications, closure or evacuation of healthcare services (Arrieta et al., Reference Arrieta, Foreman, Crook and Icenogle2008), and reduced attendance and preparedness by frontline healthcare workers (Jaakkimainen et al., Reference Jaakkimainen, Bondy, Parkovnick and Barnsley2014, Balicer et al., Reference Balicer, Omer, Barnett and Everly2006). Infection control measures, such as quarantine and rationing of emergency supplies, may contribute to the disruption of short-term healthcare (Elston et al., Reference Elston, Cartwright, Ndumbi and Wright2017; Jaakimainen et al., 2014). Likewise, emergencies and natural disasters can lead to lower rates of clinic attendance by patients (Kelly et al., Reference Kelly, Squiers, Bann, Stine, Hansen and Lynch2015) and lower levels of medication management and adherence (Ochi et al., Reference Ochi, Hodgson, Landeg, Mayner and Murray2014). Since the start of the COVID-19 pandemic, similar experiences have been reported from a range of healthcare systems (Chang et al., Reference Chang, Cullen, Harrington and Barry2020, Palmer et al., Reference Palmer, Monaco, Kivipelto, Onder, Maggi, Michel, Prieto, Sykara and Donde2020, Prescott et al., Reference Prescott, Baxter, Lynch, Jassal, Bashir and Gray2020). The impact of emergencies and pandemics on NCDs is more severe in LMICs (Slama et al., Reference Slama, Kim, Roglic, Boulle, Hering, Varghese, Rasheed and Tonelli2017). On-going management of the crisis exacerbates preexisting healthcare vulnerabilities in capacity and capability (Kraef et al., Reference Kraef, Juma, Kallestrup, Mucumbitsi, Ramaiya and Yonga2020, Sharma et al., Reference Sharma, Mudgal and Sharma2020, Siedner et al., Reference Siedner, Kraemer, Meyer, Harling, Mngomezulu, Gabela, Dlamini, Gareta, Majozi, Ngwenya, Seeley, Wong, Iwuji, Shahmanesh, Hanekom and Herbst2020). Consequently, people with NCDs, already more susceptible to becoming seriously ill if they become infected with the SARs-CoV-2 virus, may be less able to access adequate treatment to manage their NCD.
In a recent survey of Ministries of Health in 163 member states, the World Health Organization (WHO) found that the COVID-19 pandemic had severely interrupted prevention and treatment services for NCDs: 122 countries reported service disruptions due to the pandemic (World Health Organization, 2020b). More than half (53%) of the countries surveyed reported having partly or completely disrupted services for hypertension treatment, 49% for diabetes and diabetes-related complications, and 31% for cardiovascular emergencies. In 94% of countries, the Ministry of Health staff working in NCDs were partly or fully reassigned to support the COVID-19 response. Population health screening programs have also been interrupted, with most significant disruption in countries experiencing high levels of community transmission (World Health Organization, 2020a).
Thus far, research has failed to capture insights into the day-to-day impacts of COVID-19 on FLHCWs (including medical doctors, registered nurses, community pharmacists, and state registered allied staff) providing healthcare for NCDs. In this study, we aimed to gain insights directly from FLHCWs, specifically doctors and pharmacists, working in countries with a high NCD burden, and thereby, identify opportunities to improve the provision of healthcare during the current pandemic and in future healthcare emergencies.
Methods
We designed and conducted an online survey of FLHCWs in nine countries between September–October 2020. We developed the questionnaire in conjunction with a group of expert advisors from Viatris (formerly Upjohn, a Pfizer division), the World Organization of Family Doctors (WONCA), the International Alliance of Patients’ Organizations (IAPO), and the International Pharmaceutical Federation (FIP) with reference to previous surveys conducted during disease outbreaks or natural disasters (Balicer et al., Reference Balicer, Omer, Barnett and Everly2006; Chudasama et al., Reference Chudasama, Gillies, Zaccardi, Coles, Davies, Seidu and Khunti2020; Kaufman et al., Reference Kaufman, Rajataramya, Tanomsingh, Ronis and Potempa2012; World Health Organisation, 2020b). Potential end-users, i.e., physicians and pharmacists provided feedback on the face validity of the survey. The survey and the invitation to participate was made available in English, Thai, Arabic, Portuguese, and Spanish. Surveys were translated by health professionals working for Viatris who were either fluent or native speakers in the respective language. Due to scheduling limitations, we deployed the survey in different countries in rolling recruitment across the study period. We obtained ethical approval from the Auckland Health Research Ethics Committee (Ref: AH3064).
Eligibility criteria
FLHCWs were eligible to participate if they worked as a physician or community pharmacist involved in the healthcare of patients with NCDs and resided in one of the nine selected countries. For the purpose of the questionnaire, we were interested in the following NCDs: diabetes, high cholesterol, cardiovascular disease, depression, and anxiety.
We recruited respondents from the following three regions and nine countries (or collection of states): South East Asia (ASEAN): Malaysia, Thailand, Philippines; Africa and Middle East (AFME): Gulf Cooperation Council, Egypt, South Africa; and Latin America (LATAM): Brazil, Mexico, and Argentina. The countries were pragmatically selected from a group of countries fitting an archetype defined by high NCD burden and varying degrees of readiness to combat NCDs (Ray et al., Reference Ray, Potkar, Salem, Cleveland, Lewis, Subramaniam, Ray, Potkar, Salem, Cleveland, Lewis and Subramaniam2020). Most were LMICs, but we included the Gulf Cooperation Countries, high-income countries, that have a high NCD burden and poor preparedness to combat NCDs, consistent with the LMIC archetype (Ray et al., Reference Ray, Potkar, Salem, Cleveland, Lewis, Subramaniam, Ray, Potkar, Salem, Cleveland, Lewis and Subramaniam2020), recognising that there is diversity within this group of countries in the public health response to COVID-19 (Hale, Reference Hale, Angrist, Goldszmidt, Kira, Petherick, Phillips, Webster, Cameron-Blake, Hallas, Majumdar and Tatlow2021).
We recruited respondents through Upjohn’s and FIP’s databases of FLHCWs and their offices and partner organizations in each country. Potential respondents were emailed an invitation to participate, together with a link to the survey, which was constructed using REDCap (Copyright © 2020 Vanderbilt University, Nash, TN, USA.).
The survey collected demographic information (age group, sex, country, and state) as well as information about the participant’s role as a FLHCW and the nature of their clinic or practice. Survey questions were framed around three domains: the impact of COVID-19 pandemic on clinical practice and NCDs; barriers to clinical care during the COVID-19 pandemic; and innovative responses to the challenges of the pandemic. The survey consisted of multichoice questions, checkboxes, and Likert-scales and took 5–10 min to complete (see Appendix 1).
Statistical analysis
We used SAS version 9.4 (Copyright © SAS Institute Inc., Cary, NC, USA.) for data analyses, summarizing demographic information as frequencies for categorical variables, by participant type (physician or pharmacist), and region. Variables of interest were compared using chi-squared tests to assess statistical significance, with P = 0.05 used as the cutoff.
Results
Between September 21 and November 2, 2020, 1347 individuals responded to the survey. Of these respondents, 71.1% were physicians, 531 (39.4%) of whom identified as general practitioners, family physicians, or family medicine specialists, while 420 (31.2%) identified as “Other medical specialist”. Three-hundred and eighty-seven survey respondents (28.7%) identified as pharmacists (Table 1). Most respondents came from the LATAM region (70.5%). The majority of respondents from the GCC were from Kuwait (44.3%) and Saudi Arabia (31.2%).
Table 1. Demographic characteristics of physicians and pharmacists summarized by frequency (%)
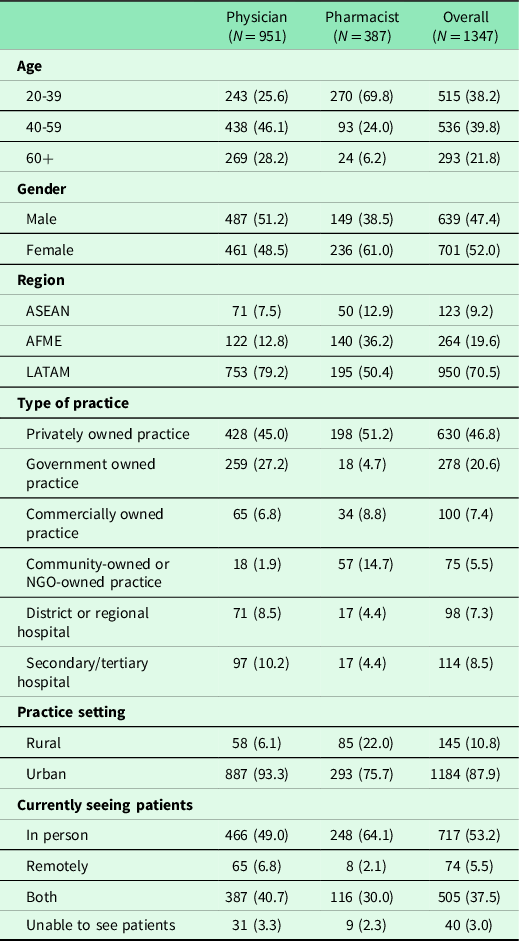
Almost two-thirds of respondents (61.6%) were over the age of 40, with slightly more female (52.0%) than male respondents (see Table 1). Nearly half of respondents worked in a privately owned practice or clinic and 20.6% in a government-owned establishment. Most respondents (87.9%) worked in urban settings. Pharmacists were younger than physicians and comprised a larger proportion of female respondents.
Most respondents reported that they were seeing patients in-person (53.2%) or seeing patients both in-person and remotely (e.g., via a telemedicine connection) (37.5%). Only a small proportion of FLHCWs reported that they only saw patients remotely (5.5%) or were unable to see patients due to public health restrictions (3.0%). Fewer physicians reported currently seeing patients in-person (49.0%) compared to pharmacists (64.1%). The proportion of respondents seeing patients in-person was larger in AFME (58.0%) compared to the ASEAN region (49.6%) and LATAM region (52.3%).
Clinical practice
Most respondents (93.3%) believed that COVID-19 had adversely affected the mental health of most or some of their patients. The proportion of respondents that answered affirmatively was high across all FLHCWs (>88%), and there was no significant difference between the types of FLHCW. Since the pandemic, more than half of the clinicians perceived an increase in the number of patients seeking care for anxiety and/or depression (67.0%), while findings were mixed for hypertension, raised lipids, and diabetes (Figure 1). Of those who reported an increase in patients seeking care, 23.6% reported that the change was an increase in new patients while 18.6% reported that the change was in existing patients seeking more care; the majority reported that it was a combination of both.
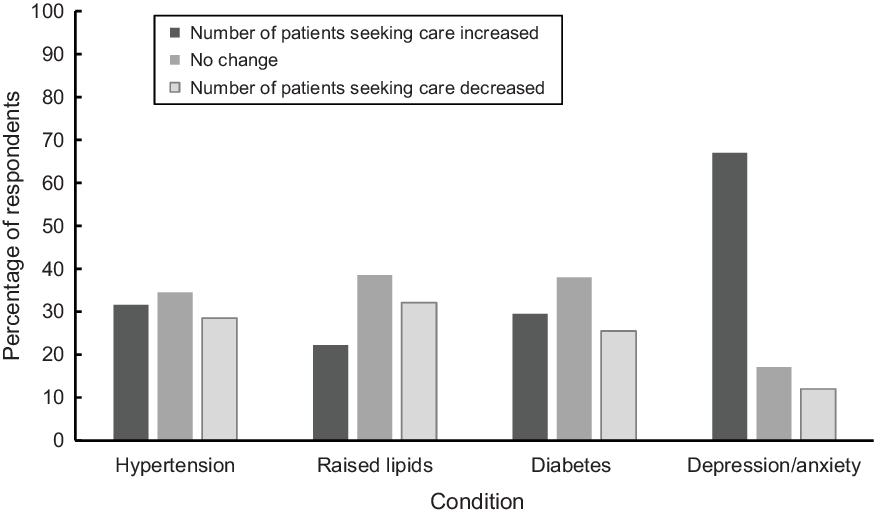
Figure 1. FLHCP perceived change in the number of patients seeking care relating to NCDs or mental health.
Compared to physicians, a higher proportion of pharmacists reported an increase in patient visits for NCDs, especially hypertension (38.5% of pharmacists versus only 29.0% of physicians). Thirty-seven per cent of physicians reported a decline in the number of patient visits for raised lipids, while only 18.6% of pharmacists reported the same. More physicians reported an increase in patient visits for depression and/or anxiety compared to pharmacists (70.7% of physicians versus 58.7% of pharmacists). Depression and/or anxiety was the only condition for both groups where the majority reported an increase in the numbers of patient visits.
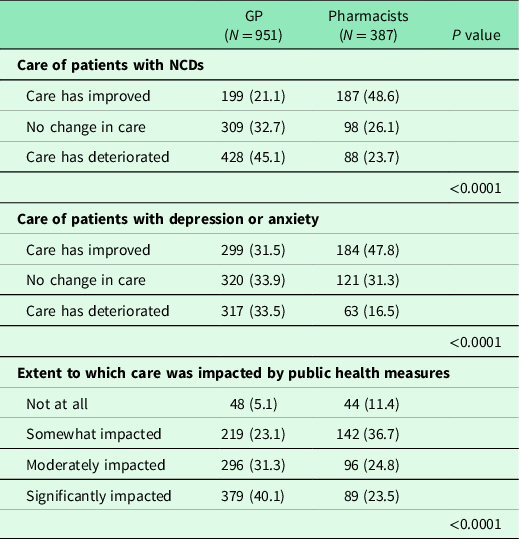
When asked about the effect that COVID-19 had on the ability to provide healthcare for patients with NCDs, nearly one-third (29.0%) reported that healthcare had improved, while 38.6% reported that care had deteriorated for NCDs. When asked about the effect of COVID-19 on the ability to provide care for patients with depression and anxiety, 36.1% reported that care had improved, while 28.6% reported that care had deteriorated. There were significant differences in the findings between healthcare workers for both NCDs and mental health (P < 0.001). As seen in Table 1, a higher proportion of pharmacists than physicians reported improved care for both NCDs and anxiety and depression. Nearly a half of physicians said that their ability to provide care for NCDs had deteriorated, while only a quarter of pharmacists said the same. For care of anxiety or depression, similar proportions of physicians reported that care had deteriorated (33.5%), and that care had improved (31.5%), while 47.8% of pharmacists reported improved care. There was no significant difference in these responses between regions (Figure 2).
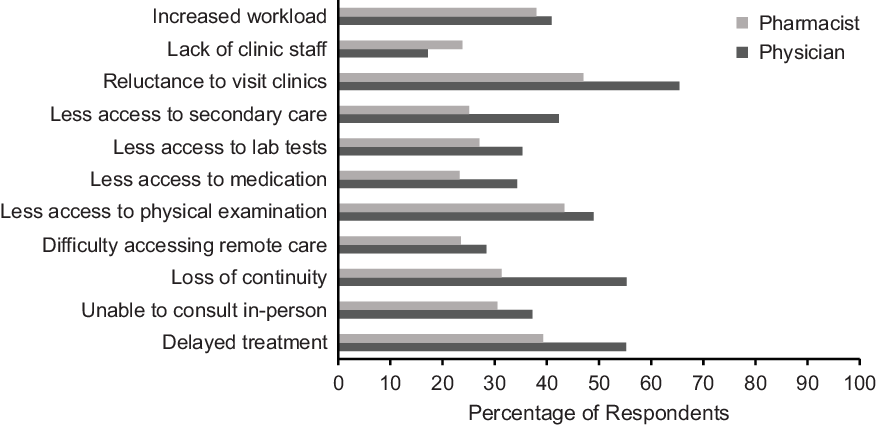
Figure 2. FLHCP perceptions of COVID-19-related factors influencing care of patients.
For most respondents, clinical or patient care activities had been somewhat or moderately adversely impacted by COVID-19 public health measures (56.2%). A third of respondents reported they had been significantly impacted (35.3%). Only a small proportion (6.8%) reported no impact of public health measures. The highest proportion of respondents reporting no impact was from AFME and lowest from ASEAN (8.7% vs 4.1%, respectively), likely reflecting country-to country variation in the intensity and scale of public health measures (Hale, Reference Hale, Angrist, Goldszmidt, Kira, Petherick, Phillips, Webster, Cameron-Blake, Hallas, Majumdar and Tatlow2021).
There was a significant difference in the impact of public health measures on pharmacists and physicians (P < 0.001). Fewer pharmacists reported that they had been impacted by public health measures and were more than twice as likely to note that public health measures had 'not at all’ impacted their ability to provide healthcare, compared to physicians (11.4% vs 5.0% respectively, Table 2). Only 23.5% of pharmacists reported that they had been significantly impacted compared to 40.1% of physicians.
Table 2. Impact of COVID-19 on respondents’ ability to care for patients with NCDs and depression or anxiety
Barriers
Factors influencing the healthcare of patients
When asked which factors relating to COVID-19 were influencing their care of patients, the most common option was the reluctance of patients to visit healthcare settings during the pandemic (59.8%). The next most common responses were delayed treatment for non-COVID-19 conditions (50.5%), loss of continuity of care (48.4%), and less access to physical examination and monitoring (47.2%). Lack of clinical staff was the least frequently selected option (19.2%).
Although the most frequently endorsed barriers were similar across physicians and pharmacists, the level of endorsement was higher across all factors except for lack of clinical staff, which was more widely endorsed by pharmacists. Most physicians selected delayed treatment (55.2%) and loss of continuity of care (55.3%) as factors influencing healthcare. While delayed treatment was selected by nearly 40% of pharmacists, loss of continuity was only endorsed as a factor influencing healthcare by 31.3% of pharmacists. Pharmacists endorsed lower access to physical monitoring to a lesser extent compared to physicians (43.4% vs 49.0%, respectively), although this was still the second most common factor. Both groups reported the importance of increased workload. Lack of staff was endorsed more frequently by pharmacists than physicians (23.8% vs 17.2%, respectively). Compared to physicians, fewer pharmacists reported less access to medication as a factor influencing care. We found significant differences between the proportions of physicians and pharmacists for the following response options: delayed treatment (P < 0.001), inability to have in-person visits (P = 0.0128), loss of continuity of care (P < 0.001), less access to medication (P < 0.001), less access to laboratory tests (P = 0.0035), less access to secondary care (P < 0.001), a reluctance of patients to visit clinics (P < 0.001), and a lack of clinic or pharmacy staff (P = 0.007).
Barriers to accessing routine care
When asked about the barriers they believed patients were experiencing in accessing routine care during the pandemic, fewer than 1% of respondents considered that there were no barriers. The barrier most frequently endorsed was fear of contracting COVID-19 in healthcare settings (76.7%). The barriers most frequently reported, after fear of contracting COVID-19, were restriction of movement (58.4%) and financial hardship or loss of insurance (55.5%). While fear of contracting COVID-19 in healthcare settings was consistently found across both pharmacists and physicians, this barrier was endorsed by less than two-thirds of pharmacists (61.2%) compared to most physicians (82.5%). Similarly, for financial hardship or loss of insurance, this barrier was strongly endorsed by both groups but to a lesser degree by pharmacists (58.5% of physicians vs 48.6% of pharmacists). Restriction of movement and lack of transport were barriers endorsed more frequently by pharmacists compared to physicians.
Technology
Most respondents found technology to be useful in managing routine healthcare of NCDs during the pandemic (76.5%). This finding was consistent across regions and type of FLHCW. Most respondents reported that there had been an increase in the number of patients interested in or purchasing devices related to self-care or self-monitoring of NCDs (67.4%). The proportion of respondents that reported an increase was greater for pharmacists (76.7%) than physicians (63.9%). When asked what healthcare practices they would personally be interested in adopting following the COVID-19 crisis, the most frequently endorsed options were patient counselling (58.9%) and preventative activities (58.1%). We observed significant differences across regions in the degree to which the adoption of different technologies was supported. Respondents from the ASEAN region endorsed technologies to a greater extent than the other regions. For example, a significantly higher proportion (90.1%) of respondents from the ASEAN region considered that there would be increased use of teleconsulting or virtual consulting beyond the pandemic, compared to 77.7% and 70.2% in the LATAM and AFME regions, respectively (P < 0.001). Respondents from the AFME region generally were less likely to endorse the ongoing use of technology than both the ASEAN and LATAM region.
Discussion
Our study has revealed that the COVID-19 pandemic has had a range of impacts on the care of patients with NCDs in LMICs by FLHCWs, from constraints on access to care to health effects, in particular, depression and anxiety as noted in other surveys (Ozawa et al., Reference Ozawa, Shankar, Leopold and Orubu2019). Despite the challenges, most FLHCWs continue to see patients either in person or remotely, the latter mode is especially common for physicians; pharmacists continue to see patients in-person. Physicians’ ability to conduct physical examinations and monitoring is likely to be a factor in this difference, whereas pharmacists can conduct their work while maintaining social distancing (International Pharmaceutical Federation, 2020). The ability of pharmacists to continue to see patients in-person, in some cases even extending their hours (Aruru et al., Reference Aruru, Truong and Clark2020), highlights the potential for pharmacists in closing treatment gaps and maintaining contact between patients and the primary healthcare system during crises and emergencies (Basu, Reference Basu2020, Rasheed et al., Reference Rasheed, Nawaz, Rao and Bukhari2019). Despite continued access, either remotely or face-to-face, most respondents reported that their ability to provide quality healthcare had been compromised by pandemic control measures.
Adaptation and innovation using available technology was common. FLHCWs strongly supported the greater use of teleconsulting after the COVID-19 pandemic has abated. However, most respondents in our survey were in urban settings and therefore more likely than their counterparts in rural areas to be supported by the robust communications infrastructure needed to support telemedicine.
Our findings also suggest that the ability of FLHCWs to provide care for patients with mental health conditions was less adversely impacted than their ability to provide care for NCDs. One reason that may account for this difference is that the care of patients with depression and anxiety does not require a physical examination (Langarizadeh et al., Reference Langarizadeh, Tabatabaei, Tavakol, Naghipour, Rostami and Moghbeli2017), and is, therefore, more amenable to telehealth using readily available technology. The increasing availability of remote monitoring technology (such as blood pressure monitors) will likely facilitate physicians in their adoption of telehealth practices in the treatment of NCDs. This is complemented by a movement which is empowering patients to manage their own health and health data (Devi et al., Reference Devi, Kanitkar, Narendhar, Sehmi and Subramaniam2020).
The findings of the most common barriers and factors influencing care reported by FLHCWs were important to note. Although a fear of contracting COVID-19 is specific to the current circumstances, the other factors identified (such as restricted movement and financial loss) are consistent with research that has identified barriers to accessing routine care during natural disasters (Arrieta et al., Reference Arrieta, Foreman, Crook and Icenogle2008, Balicer et al., Reference Balicer, Omer, Barnett and Everly2006, Jaakkimainen et al., Reference Jaakkimainen, Bondy, Parkovnick and Barnsley2014).
Strengths and limitations
To the best of our knowledge, this is the first study that has elicited perceptions from FLHCWs on the impact of COVID-19 on the care of patients with NCDs in LMICs and countries with high NCD burden fitting the LMIC archetype. Uniquely, our survey included pharmacists as FLHCWs. Pharmacists are an important healthcare provider with varied roles across many LMICs, (Miller and Goodman, Reference Miller and Goodman2016, Yemeke et al., 2020, Ozawa et al., Reference Ozawa, Shankar, Leopold and Orubu2019, Kretchy et al., Reference Kretchy, Asiedu-Danso and Kretchy2021) and should be included in all such surveys.
Where there were high numbers of participants in particular countries, sufficient statistical power was available to undertake detailed analyses by location and type of FLHCW. However, there were some limitations. First, we used an online survey to collect data, which relied on self-report and perceptions. Second, sampling was nonrandom, convenience, and opportunistic, which limits the generalizability of the findings. We approached existing networks of healthcare providers and may have missed responses from some groups. Third, while we initially aimed to sample 250 respondents from each group (physicians, pharmacists) in each country, we did not meet this target, and we oversampled physicians in Mexico, which may skew findings, particularly given the high number of general practitioners responding in LATAM. The variable number of respondents per country and per occupation meant that individual responses could not be averaged to give country-level responses for cross-country comparisons. Finally, we did not distinguish between the different types of teleconsulting or virtual consulting in the survey questions, limiting our ability to determine which virtual consulting methods (call, video call, text messaging, etc.) were most preferred between the FLHCWs.
Implications
Greater support is needed for FLHCWs in LMICs who care for growing numbers of patients with depression and anxiety (Torales et al., Reference Torales, O’higgins, Castaldelli-Maia and Ventriglio2020). Community pharmacists could play a greater role in NCD and mental health management in pandemic situations because patients were less reluctant to visit their premises than attend medical clinics. One proposed solution to improve healthcare accessibility in LMICs is to train community healthcare workers like pharmacists in testing and screening activities that are traditionally performed by physicians, thereby “task shifting” some of the burden from the physicians (Ganju et al., Reference Ganju, Goulart, Ray, Majumdar, Jeffers, Llamosa, Cañizares, Ramos-Cañizares, Fadhil, Subramaniam, Lim, El Bizri, Ramesh, Guilford, Ali, Devi, Malik, Potkar and Wang2020). A reconfiguration of the healthcare system that maximizes pharmacist involvement in NCD care could also help ease the pressure on physicians in providing care during the COVID-19 pandemic in LMICs. Greater attention should be given to increasing technical support for FLHCWS in LMICs to use readily available communications technologies and tools to enable continuity of preventive care and treatment for their patients and communities, particularly in mental health (Dowrick et al., Reference Dowrick, Kassai, Lam, Lam, Manning, Murphy, Ng and Thuraisingham2020).
Conclusion
Our findings reiterate the need to ensure continuity of care for NCDs as part of pandemic preparedness so that chronic conditions are not exacerbated by public health measures and the direct impacts of the pandemic.
Acknowledgments
We acknowledge the following organizations for their support in conducting this research: International Alliance of Patients’ Organizations, (IAPO), World Organization of Family Doctors (WONCA), and International Pharmaceutical Federation (FIP).
Financial support
This work was funded by Viatris (formerly Upjohn, a Division of Pfizer).
Conflicts of interest
KS, AM, and PH are employees of Viatris.
The remaining authors have no conflicts of interest to declare.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guidelines on human experimentation (Auckland Health Research Ethics Committee) and with the Helsinki Declaration of 1975, as revised in 2008. Data were obtained from an anonymous survey, and submission of the survey was deemed consent.
Appendix 1. Questionnaire
Global Survey: Chronic Illness Care and COVID19
*Branching logic in italics
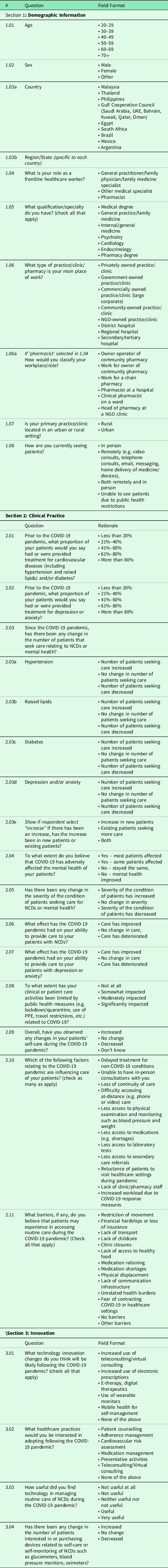
Thank you for participating in this survey.







