Background
As the numbers of people with dementia increase, it is unlikely that the current specialist care model will be able to meet their needs. This model is not affordable and does not facilitate continuing care, holistic management of or care coordination for complex multi-morbidities; these are core functions of primary healthcare (Prince et al., Reference Prince, Comas-Herrera, Knapp, Guerchet and Karagiannidou2016).
Currently, there is no cure for dementia, and the goals for clinical care depend on the stage of the disease. Early on, they may focus on maximising function in daily activities and promoting social activities. At least this should be so, according to the recent focus on ‘social health’ in dementia (Dröes et al., Reference Dröes, Chattat, Diaz, Gove, Graff, Murphy, Verbeek, Vernooij-Dassen, Clare, Johannessen, Roes, Verhey and Charras2016). However, in later stages of dementia, the goals may shift to addressing behavioural and psychological symptoms and reducing carer burden. As with other chronic diseases, assessing quality of life (QoL) in dementia is a core task. A metasynthesis of qualitative research identified four relevant determinants (relationships, agency in everyday life, a wellness perspective and a sense of place); the experience of connectedness or disconnectedness within each factor influences the QoL of people with dementia (O’Rourke et al., Reference O’rourke, Duggleby, Fraser and Jerke2015).
Worldwide, dementia is under-managed in primary care (Prince et al., Reference Prince, Comas-Herrera, Knapp, Guerchet and Karagiannidou2016). Three systematic reviews highlight the complex and multifactorial barriers to dementia management (Koch & Iliffe, Reference Koch and Iliffe2010; Aminzadeh et al., Reference Aminzadeh, Molnar, Dalziel and Ayotte2012; Mansfield et al., Reference Mansfield, Noble, Sanson-Fisher, Mazza and Bryant2018): people with dementia factors (e.g., non-compliance with care and medication), general practitioner (GP) factors (e.g., lack of knowledge about dementia, unfamiliarity with support services) and system factors (e.g., time constrains; limited availability of support services, and care coordination).
In Portugal, every person has access, in principle, to primary care services within the National Health Service (where GPs control access to secondary care). GPs are considered pivotal health professionals although there is a variable shortage of them, regionally (Gonçalves-Pereira & Leuschner, Reference Gonçalves-Pereira, Leuschner, Burns and Robert2019). In recent years, a new organisation has been introduced in primary care: family health units consisting of multidisciplinary teams (GPs, practice nurses (PNs) and administrative staff) with a variable payment based on capitation and professional performance. The current list of indicators that measure professional performance does not include dementia (Serviços Partilhados Ministério da Saúde, 2021).These units coexist with the traditional health centres, constituting groups of primary care centres, a significant number of them in metropolitan Lisbon (Barros et al., Reference Barros, Machado and Simões2011) (Figure 1). The multidisciplinary teams, considered the core teams, are supported by an extended team (e.g., social workers, psychologists) (Barros et al., Reference Barros, Machado and Simões2011).
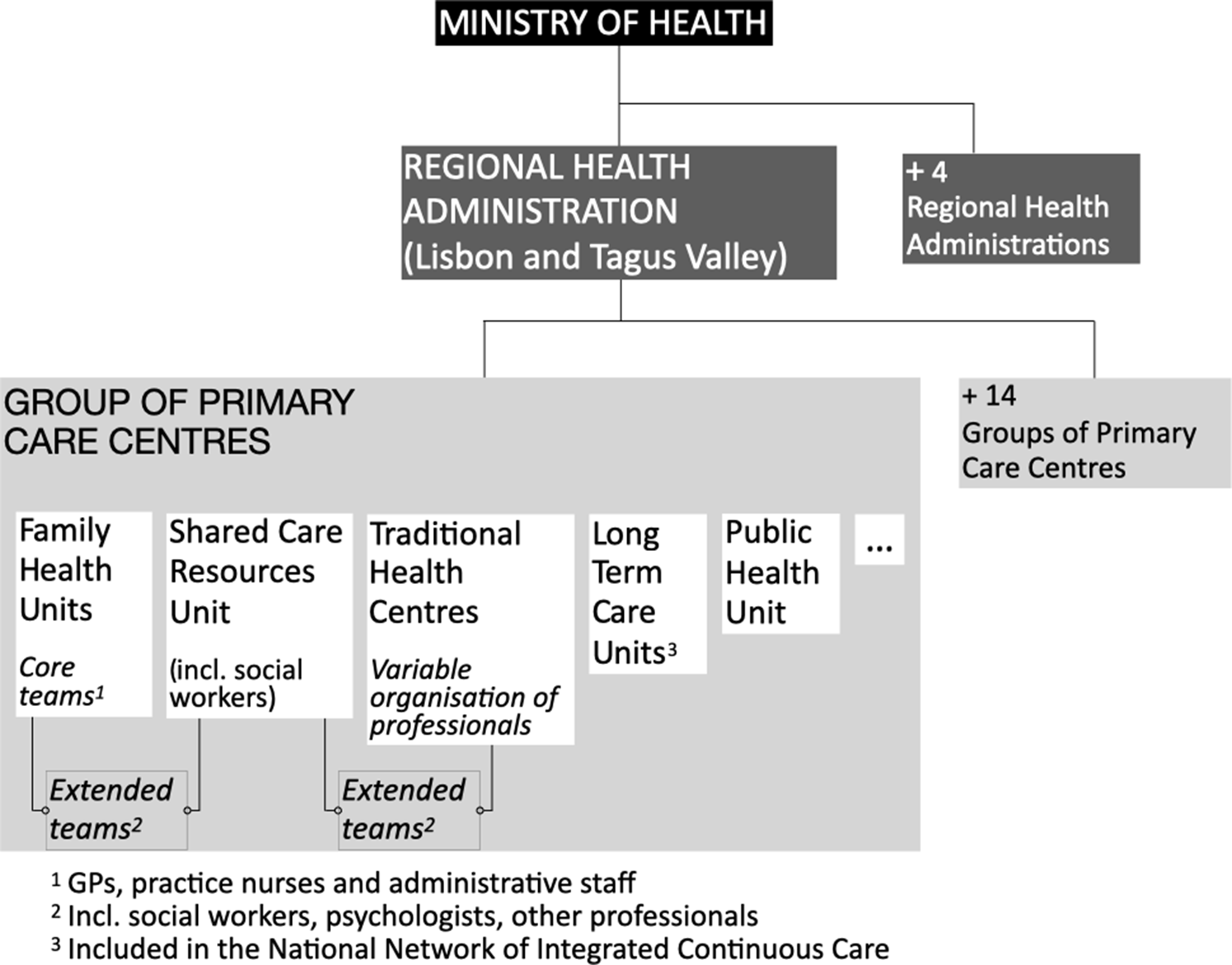
Figure 1. Overview of primary care organisation.
The area of expertise of the elements of extended teams varies geographically and can comprise social work, psychology, occupational therapy and physiotherapy. However, the ratio between these professionals and the population registered is sometimes very low (e.g., occupational therapists 1:74 126 in one group of primary care centres in Lisbon metropolitan area) (Serviços Partilhados Ministério da Saúde, 2021). Although this new model allows for the structural organisation of the teams, it still falls short of their functional organisation [i.e., team members having explicit functions to achieve a common goal (Bower & Sibbald, Reference Bower, Sibbald, Jones, Britten, Culpepper, Gass, Grol, Mant and Silagy2005)]. In fact, the involvement of PNs in chronic disease management was proposed in 2014 and is still not fully implemented, being in place only for diabetes and hypertension. Other constraints on PNs’ involvement in dementia care are related to insufficient dementia training, and their relative scarcity compared with other EU countries (OECD, 2020). On the whole, concerning dementia management in Portuguese primary care, there are important flaws that should be better characterised. On the whole, concerning dementia management in Portuguese primary care, there are important flaws that should be better characterised. Some concern poor liaison with specialised neurology and psychiatry services and insufficient support to primary care (Balsinha et al., Reference Balsinha, Gonçalves-Pereira, Iliffe, Freitas, Grave, Lima and Ivbijaro2019; Gonçalves-Pereira & Leuschner, Reference Gonçalves-Pereira, Leuschner, Burns and Robert2019).
National dementia strategies in Europe emphasise the role of GPs in detecting new cases of dementia and maintaining the general health of the people with dementia; however, their role in diagnosis, initiating anti-dementia drugs and providing social support is more controversial (Koch & Iliffe, Reference Koch and Iliffe2010). The Portuguese Dementia Strategy which was published only in 2018 (Health Strategy in Dementia, 2018) has yet to be implemented, in part due to the present COVID-19 pandemic constraints. Although indicators were to be defined in regional dementia plans, the strategy outlines different areas of intervention for primary care (Box 1). However, current dementia care pathways in primary care still have a long way to go. Social support for people with dementia is limited, being mostly provided at day care centres that are not specific for dementia, and at home by assistance with basic activities of daily living. Respite services are only available by referral (Balsinha et al., Reference Balsinha, Gonçalves-Pereira, Iliffe, Freitas, Grave, Lima and Ivbijaro2019).
In an earlier publications (Balsinha et al., Reference Balsinha, Iliffe, Dias, Freitas, Grave and Gonçalves-Pereira2021), we explored the role of GPs in dementia care in Portugal and found that GPs contributed little, working alone despite being members of multidisciplinary teams. The provision of dementia care by PNs has been explored in the literature; a recent systematic review identified its potential benefits (e.g., increased patient accessibility to PNs, early recognition and management of cognitive changes, better care management) as well as limitations (e.g., lack of definition of PN roles, inadequate dementia training, time constraints and poor communication with GPs) (Gibson et al., Reference Gibson, Goeman and Pond2020).
Despite team-based care being a feature of high-performing primary care (Bodenheimer et al., Reference Bodenheimer, Ghorob, Willard-Grace and Grumbach2014), previous research on the barriers to dementia management in primary care has focused essentially on GPs’ factors (Aminzadeh et al., Reference Aminzadeh, Molnar, Dalziel and Ayotte2012) and perspectives (Koch & Iliffe, Reference Koch and Iliffe2010; Aminzadeh et al., Reference Aminzadeh, Molnar, Dalziel and Ayotte2012). In our understanding, a comprehensive triangulated view of barriers to dementia management focusing on teamwork is missing. This could inform future strategies in countries with health systems similar to that of Portugal.
The aim of this study is to explore the obstacles and barriers to the implementation of the Portuguese Dementia Strategy by primary care teams, from the perspectives of service users and professionals.
Methods
Design
A qualitative approach was adopted to obtain an in-depth understanding of dementia care (Britten, Reference Britten, Pope and Mays2006). Semi-structured face-to-face interviews were conducted. The interview guides drew on available literature (Fortinsky, Reference Fortinsky2001; Wensing et al., Reference Wensing, Mainz and Grol2009; WHO, 2010, Dreier-Wolfgramm et al., Reference Dreier-Wolfgramm, Michalowsky, Austrom, Van Der Marck, Iliffe, Alder, Vollmar, Thyrian, Wucherer, Zwingmann and Hoffmann2017) and were adapted for the different sets of participants (see Table 1).
Table 1. Interviews’ topic guide
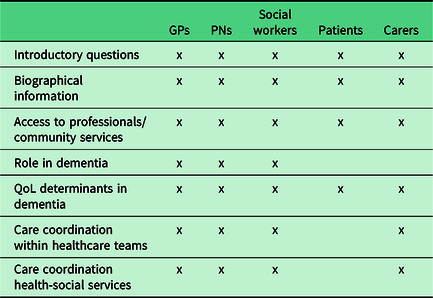
GPs – general practitioners; PNs – practice nurses; QoL – quality of life.
Ten pilot interviews (two with each type of participants) were conducted, resulting in minor adaptations to the interview guide (rephrasing a few questions and adding prompts to clarify the answers). Interviews were informal in style, enabling specific issues to be explored as and when they arose (Creswell, Reference Creswell2014).
Setting
As in our previous studies (Balsinha et al., Reference Balsinha, Iliffe, Dias, Freitas, Grave and Gonçalves-Pereira2021), four groups of primary care centres within the Lisbon metropolitan area were selected to reflect different socio-economic characteristics.
Sampling
A contact person (GP) in each family health unit recruited the GPs. Purposive sampling was used to recruit participants (Ritchie et al., Reference Ritchie, Lewis, Elam, Ritchie and Lewis2003a). The GPs’ inclusion criterion was that they provided regular care to people with dementia. The GP sample comprised both genders and different durations of clinical experience. PNs belonged to the same core team as the GPs. Social workers were recruited without any specific criteria given their reduced number in each group of primary care centres. People with dementia were recruited by their GPs, if they had a dementia diagnosis according to ICD-10 DCR (WHO, 2004) and could give informed consent. A purposive sample of people with dementia included both genders, individuals at different stages of dementia and with different types of kinship with their carers. All carers were family members. The sample size needed was estimated to be 10–12 participants per group, using Guest et al.’s methods (Guest et al., Reference Guest, Bunce and Johnson2006).
Data collection
Data saturation criteria were based on an initial analysis of eight interviews with each group and on a stopping criterion of two interviews where no new ideas would emerge (Francis et al., Reference Francis, Johnston, Robertson, Glidewell, Entwistle, Eccles and Grimshaw2009). These criteria were met at the sixth interview with people with dementia and tenth interview with carers. In the case of GPs and PNs, only in the last interview did new ideas fail to emerge. The criteria were not met in the social workers’ group.
A total of 40 participants were interviewed: 10 GPs, 8 PNs, 4 social workers, 8 people with dementia and 10 carers. Severity of dementia was assessed with the Clinical Dementia Rating (CDR) (Morris, Reference Morris1993). Two of the 10 people with dementia had advanced dementia and were not able to be interviewed. Three participants had difficulty recalling the care received; therefore, we focused the interview on their subjective experiences (Wilkinson, Reference Wilkinson and Wilkinson2005). The interviews with people with dementia and their carers took place in their homes, and with professionals at their practices. Interviewing was completed before the onset of the COVID-19 pandemic, between March 2018 and May 2019.
Interviews lasted around 40 min and were digitally recorded. Transcriptions were done before the next interview, allowing for new ideas to be explored and discussed by the interviewers (Creswell, Reference Creswell2014). The accuracy of the transcripts was checked by the primary author.
Data analysis
The framework approach (Ritchie et al., Reference Ritchie, Spencer, O’connor, Ritchie and Lewis2003b) and data triangulation were core components of the data analysis. All transcripts were coded by two researchers. Using NVivo 12®, the content of three transcripts was initially examined and the codes generated were grouped into categories. The initial analytical framework drew on these categories and was used to code 15 interviews (3 per group of participants) by 2 of the authors, independently. An analytical framework with six themes was then developed and applied to each transcript, and differences were resolved by discussion.
Ethics
Ethics approval was granted by the ARSLVT Research Ethics Committee nº 067/CES/INV/2017, and NOVA Medical School Ethics Committee nº 28/2017CEFCM, and written informed consent was obtained from each participant.
Findings
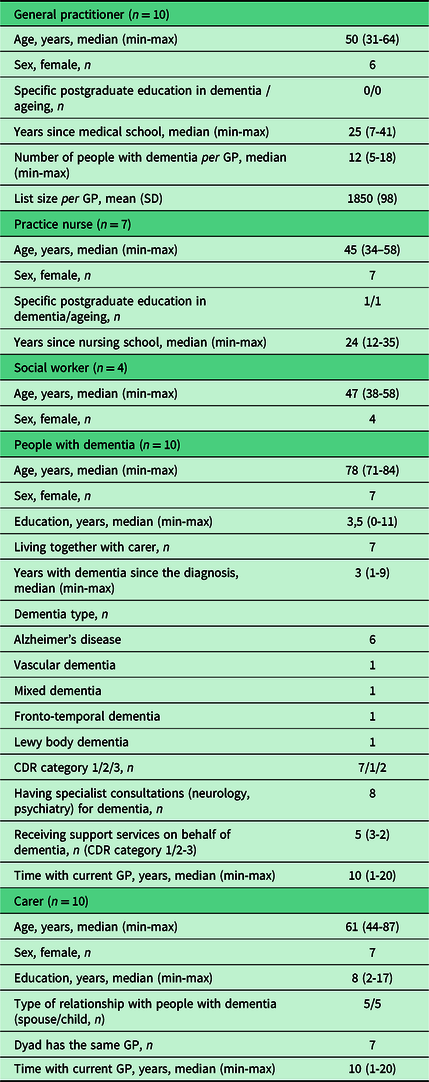
The characteristics of participants are summarised in Table 2.
Table 2. Group characteristics (n = 41)
Four major themes and three subthemes were identified and are summarised in Figure 2.
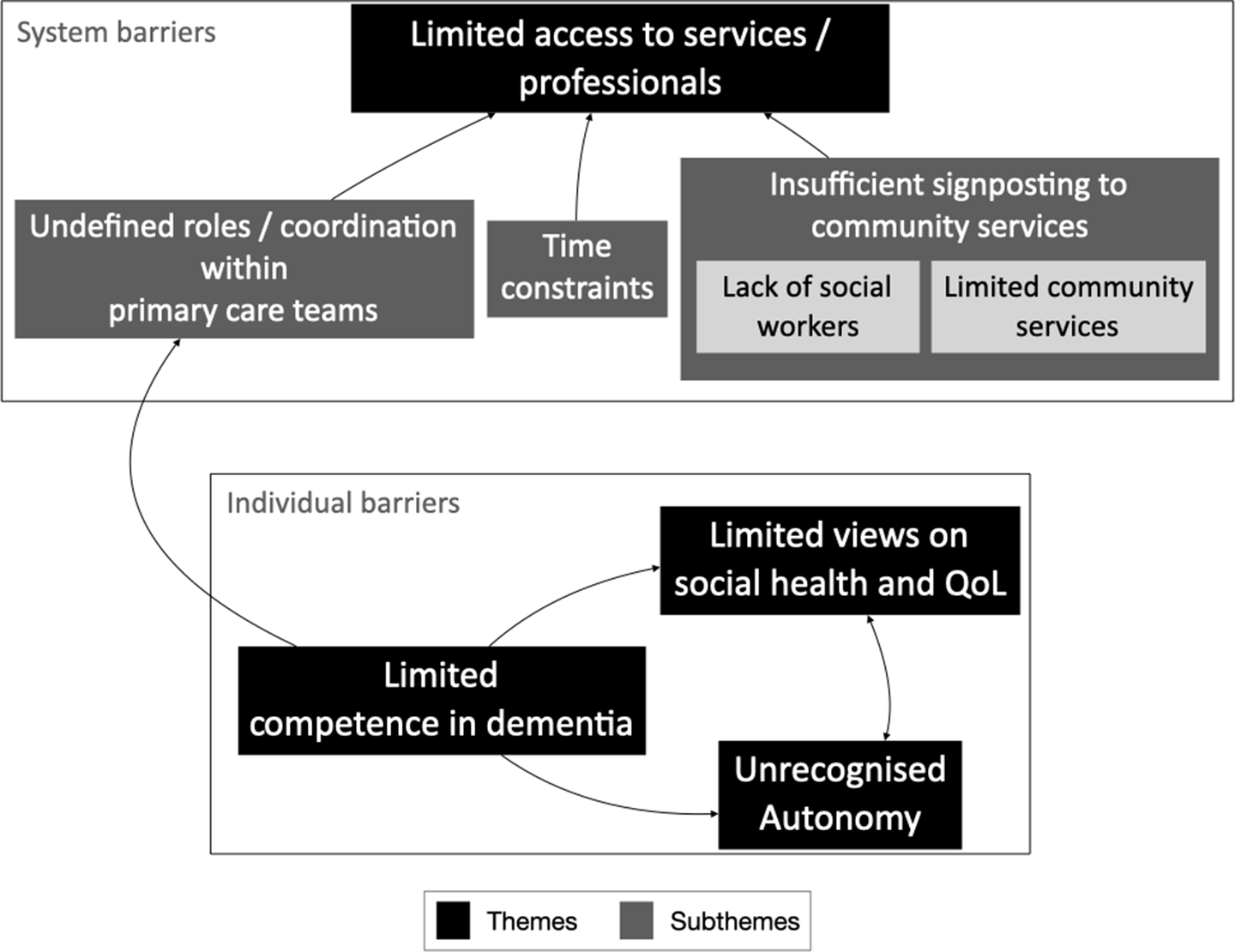
Figure 2. Thematic map.
Limited access to services/professionals
Most participants considered accessibility to be a fundamental feature in primary care; however, they identified several barriers for patients with dementia and their families to accessing primary care and community services (e.g., home care, day centres).
Undefined roles and coordination within primary care teams
All GPs and PNs reported that neither their roles nor coordination within the teams were well defined, which might lead to a dismissive attitude among professionals which could limit access to services, as this GP explained.
We are less involved [in dementia] than in other diseases in which we know our role. It’s difficult to coordinate with the nurse, because it’s not defined as it is for example for diabetes… and altogether this makes us dismissive. (…) Access would be better if there were consultations with nurses. GP5
In fact, most GPs and PNs explained that PNs would only know these patients if they had other chronic conditions.
I’m aware of some patients with dementia, but only those I follow for diabetes or hypertension. PN8
Otherwise, they would provide support for functional dependency only in the advanced stages of dementia.
When they become very dependent, that’s when we visit them. PN7
Only one PN stated that planned coordination within core teams was necessary, similar to other chronic conditions.
We should have definite functions with these patients, as we have with the diabetics. Following them from the beginning of their illness. PN4
Other PNs took a different view; working together with GPs allowed informal coordination on an as-needed basis.
We don’t have a defined role! I’ll go to the GP and say ‘Doctor, I think this lady is becoming forgetful … there’s something wrong with her!’ There is this informality discussing these cases. PN1
None of the social workers questioned their role, but they reported limitations in coordinating with core teams because they were too few to be engaged with each team.
We don’t belong to the core teams (…) it’s difficult to be far from the family health units, but we are very few, so it wouldn’t be possible anyway. SW4
Conversely, all social workers considered the coordination with community services to be good, reporting joint home visits and participation in work groups.
(…) we often do home visits together [with social workers from community services] to assess the situations. SW3
None of the people with dementia referred to professionals other than GPs; some mentioned PNs regarding flu vaccination.
Similarly, carers denied any patient interactions with primary care professionals regarding dementia, other than the GP, with the exception of two carers of patients with advanced dementia whom the nurses assisted regarding functional dependence.
the nurses came here a few times with the GP and told us how we should have our home adapted for this condition (…) C009
Time constraints
Some GPs reported having difficulty scheduling patients in general, and most of them reported that consultation time was insufficient. They explained that people with dementia needed assistance with other chronic conditions, their physical examination was more challenging, and that carers presented their own problems.
(…) time is short because these patients are not alone in the consultation and basically there are almost two consultations in one… although often the patient says little, they still have other conditions to be managed(…) GP10
(…) usually adults are able to report their symptoms, but with these patients, we have to pay attention to the physical examination. GP6
A few GPs believed that PNs played an important role in assessing and supporting the carers; however, most nurses denied having time for those tasks. Most often they only provide essential care to people with dementia and carers in intercurrent illnesses and advanced stages. Some PNs regretted this because they felt they should have a role in carers’ psychoeducation.
If we had more time … we’re supposed to teach the families, but we’re always in a rush, we don’t have enough time….PN4
None of the carers reported that the duration of consultations with GPs was insufficient; on the contrary, most of them perceived consultations to be longer than the standard 15–20 min.
The other day the GP was with us for almost an hour. C9
Insufficient signposting to community services
Most professionals acknowledged the importance of advising carers about community services. However, two factors contributed to insufficient signposting: lack of social workers and inadequacy or limited availability of those services.
Most GPs felt that signposting to community services was not their function but a task for social workers. Some of them did not know which services were available and did not have enough time to get that information. They usually referred carers to social workers or to PNs when social workers were not available.
When social services are needed, it all becomes complicated. We only have one social worker and that’s not enough. I don’t have time to get to know all the services and… honestly, it’s not my job! It turns out to be the nurse who signposts community services…GP5
I often do the social worker’s job! I briefly signpost the services, and carers do the rest… PN6
We have a social worker one afternoon per week, for a population of 17 000, it’s just not enough. GP7
Moreover, most professionals considered that community services were very few or of limited capacity. They focused on day care centres highlighting their inadequacy for many people with dementia, their strict opening hours, and the lack of a transport service.
There should be day centres adapted for dementia. But there are other problems too… In some places there’s no transportation. If the carer is working till late, who will pick them up at 5 pm? SW2
Some professionals also reported respite care to be insufficient, which might lead to abuse or neglect.
In some cases, these services are urgently needed when there is a risk of neglecting the patient (…) carers are often at their limit, cannot endure it any longer. PN7
None of the carers recalled having met any social worker throughout the referral process. All reported having directly addressed the community services, but some felt lost in the process.
We should’ve been instructed at the family health unit, we had to find the services on our own (…) C8
Limited competence in dementia
Some professionals highlighted the need to gain competence in dementia care.
Some GPs attributed their own difficulties regarding dementia treatment to the overall limitations of Medicine in this field. Potential for clinical intervention in dementia was underestimated.
It’s hard not to be able to do much for these patients… this is probably one of the great frustrations of medicine in general, right? GP3
For other GPs, having a colleague with a higher level of expertise in dementia could partly overcome the difficulties of speaking directly to specialists.
It would be very important to have someone in family health units who knew a lot about dementia… it’s difficult to reach the hospital … GP2
Some PNs disclosed the negative impact of their lack of competence in dementia on themselves (even their self-esteem) and on the quality of care delivered.
…families often want answers and we sometimes don’t know what to say (…) and we think ‘what could we have done? We didn’t do anything!’… and we feel a little frustrated. PN4
A few people with dementia were unsure regarding their GP’s ability to help them with cognitive decline.
[the GP] seems to help me, but maybe I needed another help for memory problems, another doctor… I don’t know… P7
In line with the professionals, one carer stated that primary care staff needed to be more competent in supporting them.
There should be someone more knowledgeable in how to help families, at the health centre (…) The things I know, came from internet searches…C2
Unrecognised autonomy
Some GPs acknowledge the impact of the person with dementia’s declining autonomy on care delivery. A few reported being sometimes difficult to have a person-centred attitude in consultations; their uncertainties about patients’ cognitive abilities, associated with a carer’s dominant attitude, might erode the autonomy of people with dementia.
When I see the patient, with the spouse or a child, and it’s difficult to identify the stage of dementia, I end up addressing only the carer … Or when I first address the patient and then the carer immediately contradicts them, I shift my focus to the carer… I feel that the patient is only a bystander and that bothers me …GP10
Conversely, one GP took the view that long-standing relationships with people with dementia and their families made it possible to respect wishes of people with dementia even in advanced stages of disease.
When we accompany these people to the end of their lives, we can work with the families in order to preserve the values and wishes of their relative. GP4
A few professionals and half of the carers attributed some of the people with dementia’s attitudes not to their expression of a will but to mere ‘stubbornness’.
The son worries about her, but she doesn’t want to go to the day centre… she doesn’t want this, she doesn’t want that, she doesn’t want anything! She’s very stubborn! SW1
He’s stubborn, he only does what he wants. If his wife doesn’t stop him, it’s complicated. GP1
The problem is when they don’t want to be helped: when they resist doing the things they should, they’re like children … C5
Conversely, most people with dementia expressed great satisfaction with their ability to make their own decisions. One person explained the importance of having someone who admired their decisiveness.
I have a friend, at the day centre, who likes me a lot … she is everything to me. She thinks I’m determined and that I know what I like and what I want… P5
Limited views on social health and QoL
The views of most professionals on people with dementia’s QoL were limited to having a family that would keep them safe and support them in their daily activities. Only a few, like GP6, considered it important for people with dementia to have a meaningful occupation and maintain social relationships.
Food and hygiene care must be ensured. (…) Social inclusion is also crucial, as is keeping them occupied with things meaningful to them. GP6
Most of the people with dementia highlighted the importance of social relations but few socialised regularly with friends or neighbours.
(…) and then I have breakfast with a group of friends … knowing that I’m going to meet with them helps me to get out of bed. P7
Discussion
Summary
This study describes the experiences of primary care teams and their users regarding barriers to dementia care, in a country without an operationalised Dementia Strategy but where teamwork in primary care should be normal practice. Our findings suggest that the teams lacked a defined role in dementia care, and the users had limited access to dementia services because of several system and individual barriers.
The roles of GPs and PNs were undefined, and their coordination of care for people with dementia was limited, relying on co-location. As a result, some GPs seemed to be unaware of the PNs’ tasks and most participants suggested that GPs were alone in providing care to people with dementia. Surprisingly, most professionals did not seem to attach importance to formal coordination within teams. The lack of social workers and the inadequate community services for people with dementia explain the limited access to those services.
We have also identified individual barriers to dementia care. Some professionals claimed a lack of knowledge about dementia and few relevant skills. Most professionals and carers have a limited view of the QoL and autonomy of people with dementia.
Strengths and limitations
To the best of our knowledge, this is the first study examining the barriers to dementia management in multidisciplinary primary care teams from the perspectives of team members and service users. The coding and analysis were performed by two authors with experience in consultations with dementia dyads, which could improve their reflexivity. The analytical framework allowed for a combination of inductive and deductive analysis.
There were some limitations. The sample of social workers was limited, but we were able to recruit a social worker in each of the four groups of primary care centres. Our results are not necessarily transferable to other settings; however, primary care teams were drawn from different social settings and at least in Portugal, they could be considered as typical of urban communities and services. Additionally, the Portuguese primary care system is similar to those of other European countries, for example, UK and the Netherlands (Kringos et al., Reference Kringos, Boerma, Hutchinson and Saltman2015). Purposive sampling may have introduced bias (e.g., people with dementia nominated by their GPs may have better doctor–patient relationships).
Comparison with existing literature
Our findings suggest that teamwork concerning the needs of people with dementia and their family carers was restricted, which is consistent with previous research (Hinton et al., Reference Hinton, Franz, Reddy, Flores, Kravitz and Barker2007; Mansfield et al., Reference Mansfield, Noble, Sanson-Fisher, Mazza and Bryant2018). The members of the core teams in our study did not have explicit functions regarding dementia care, a central feature of team-working (Bower & Sibbald, Reference Bower, Sibbald, Jones, Britten, Culpepper, Gass, Grol, Mant and Silagy2005). This was particularly evident in the case of PNs, who mostly delivered opportunistic care, despite previous research suggesting that PNs’ systematic involvement in dementia care can improve assessment, screening, and counselling (Jennings et al., Reference Jennings, Tan, Wenger, Cook, Han, Mccreath, Serrano, Roth and Reuben2016). Previous research suggested that national regulations may affect GPs engagement in dementia care (Petrazzuoli et al., Reference Petrazzuoli, Vinker, Koskela, Frese, Buono, Soler and Thulesius2017). The fact that publication of a Dementia Strategy was late in Portugal, when compared to other European countries, and the current delay in its implementation, can negatively affect the involvement of GPs and PNs in providing specific care in dementia.
This study findings suggest that both GPs and PNs perceive time constraints as a barrier to providing care to their patients with dementia and having a role in carers’ psychoeducation, respectively. Our analysis of the interviews supported and extended previous research that had identified time constraints as a barrier to the management of dementia by GPs (Koch & Iliffe, Reference Koch and Iliffe2010; Aminzadeh et al., Reference Aminzadeh, Molnar, Dalziel and Ayotte2012; Mansfield et al., Reference Mansfield, Noble, Sanson-Fisher, Mazza and Bryant2018).
Our findings also support others showing that GPs do not signpost to community services (Hinton et al., Reference Hinton, Franz, Reddy, Flores, Kravitz and Barker2007; Pathak & Montgomery, Reference Pathak and Montgomery2015; Foley et al., Reference Foley, Boyle, Jennings and Smithson2017) and are not familiar with them (Pathak & Montgomery, Reference Pathak and Montgomery2015). Despite our finding that PNs would take up the signposting role, they had not received this information from the primary care team. Although it is debatable whether this task belongs to GPs, previous research suggests that people with dementia and their family carers expect to get this information from their family doctor (Foley et al., Reference Foley, Boyle, Jennings and Smithson2017). Finally, the poor signposting of community services may be due to the limited supply of dementia-specific services. Best practice recommendations to improve access to and use of home care services or day care are far from being followed in Portugal, as elsewhere (Stephan et al., Reference Stephan, Bieber, Hopper, Joyce, Irving, Zanetti, Portolani, Kerpershoek, Verhey, de Vugt, Wolfs, Eriksen, Røsvik, Marques, Gonçalves-Pereira, Sjölund, Jelley, Woods and Meyer2018; Røsvik et al., Reference Røsvik, Michelet, Engedal, Bergh, Bieber, Gonçalves-Pereira, Portolani, Hopper, Irving, Jelley, Kerpershoek, Meyer, Marques, Sjølund, Sköldunger, Stephan, Verhey, de Vugt, Woods, Wolfs, Zanetti and Selbaek2020).
The Interdem consensus on social health and dementia advocates helping people with dementia to manage life despite the disease (Dröes et al., Reference Dröes, Chattat, Diaz, Gove, Graff, Murphy, Verbeek, Vernooij-Dassen, Clare, Johannessen, Roes, Verhey and Charras2016); however, our findings suggest that professionals and carers were challenged by the agency of people with dementia. Moreover, most professionals did not recognise the broader QoL and psychosocial needs of their patients, which is also consistent with previous research (Aminzadeh et al., Reference Aminzadeh, Molnar, Dalziel and Ayotte2012). These negative attitudes may stem from deficits in knowledge, from biased observation of people living with dementia (Gerritsen et al., Reference Gerritsen, Oyebode and Gove2018), and from the need to balance safety versus autonomy (Behrman et al., Reference Behrman, Wilkinson, Lloyd and Vincent2017; Stephan et al., Reference Stephan, Bieber, Hopper, Joyce, Irving, Zanetti, Portolani, Kerpershoek, Verhey, de Vugt, Wolfs, Eriksen, Røsvik, Marques, Gonçalves-Pereira, Sjölund, Jelley, Woods and Meyer2018). Importantly, these attitudes contrasted with people with dementia’s appreciation of their agency and relationships, as other studies highlighted (O’Rourke et al., Reference O’rourke, Duggleby, Fraser and Jerke2015). Primary care services could have an important role in the development of social health in dementia, but this would call for profound attitudinal changes (Gonçalves-Pereira et al., Reference Gonçalves-Pereira, Marques and Balsinha2021).
Implications for research, policy and practice
This research has identified obstacles to implementation of Portugal’s Dementia Strategy in primary care. Our results suggest that primary care teams need to extend their functional organisation to dementia care provision, for example, team members having explicit functions to achieve a common goal (Bower & Sibbald, Reference Bower, Sibbald, Jones, Britten, Culpepper, Gass, Grol, Mant and Silagy2005). This could be crucial to improve, for instance, post-diagnostic support (Siva, Reference Siva2021). Additionally, the extended teams must include a workforce from different disciplines (e.g., social workers, neuropsychologists, psychologists, and occupational therapists) in adequate number to deliver person-centred tailored care to people with dementia and their families.
The lack of community support for people with dementia creates another obstacle to policy implementation. In fact, previous research has highlighted the relevance of psychosocial needs among people with dementia in Portugal (Gonçalves-Pereira et al., Reference Gonçalves-Pereira, Marques, Balsinha, Fernandes, Machado, Verdelho, Barahona-Corrêa, Bárrios, Guimarães, Grave, Alves, Almeida, Reis, Orrell, Woods, De Vugt, Verhey and Actifcare2019). Re-designing the primary care teams may not improve per se the QoL of many people with dementia and their carers. This would call for community interventions in the form of social work guidance, home care, and re-location to more supportive environments.
To test our hypothesis, an implementation study is needed, with investment in community resources as the primary intervention, and promotion of dementia pathways in primary care being a supplementary intervention.
Acknowledgements
The authors thank the persons with dementia, their carers, and the general practitioners who participated in this study.
Authors’ Contribution
C.B., S.I. and M.G.P. designed the study, conceived the analysis, and drafted the paper. C.B. collected the data and performed the analysis, with the contribution of A.F. and F.F.B. S.D. supervised data analysis. All authors contributed to the final version of the paper.
Financial support
The present publication was funded by Fundação Ciência e Tecnologia, IP national support through CHRC (UIDP/04923/2020).
Conflicts of interest
The authors declare that they have no competing interests.
Ethical standard
Ethics approval was granted by the ARSLVT Research Ethics Committee nº 067/CES/INV/2017, and NOVA Medical School Ethics Committee nº 28/2017CEFCM, and written informed consent was obtained from each participant.







